Introduction
The US healthcare system does not adequately address the burden of Chronic Obstructive Pulmonary Disease (COPD), as the challenges in managing COPD patients is growing while resources are diminishing. COPD is the third leading cause of death in the world behind only cardiovascular diseases and cancer [
1]. COPD is also a leading cause of disability and is the third leading cause of healthy life lost to both disability and death, as measured by Disability Adjusted Life Years [
2].
COPD is also extremely expensive, estimated to account for
$50 billion in healthcare spending in 2020, and is one of the leading causes of potentially avoidable hospitalization. Hospitalizations, which account for >70% of all COPD-related medical costs [
3], are often triggered by COPD exacerbations. But those exacerbations are also associated with subsequent cardiovascular complications including acute coronary syndrome, congestive heart failure, and stroke [
4]. 80% of patients with COPD suffer from comorbid conditions, including congestive heart failure, coronary artery disease, peripheral vascular disease, stroke, hypertension, and diabetes.
Caring for patients with COPD requires effectively managing comorbid cardiovascular and related conditions, effectively requiring cardiopulmonary solutions. In recent years, remote care management has gained attention as a potential tool to improve outcomes, reduce hospital admissions and lower the cost of care. Accordingly, CMS has implemented reimbursement models for remote care management, including Remote Physiologic Monitoring (RPM) and Chronic Care Management (CCM). NuvoAir Home Service (NAHS) is a technology-driven, team-based remote care intervention designed to support patients with heart and lung conditions through at-home monitoring and remote chronic care management. The purpose of this study was to evaluate the early outcomes from a pilot program testing NAHS. As hospital admissions are the primary driver of COPD-related costs, this evaluation has a particular focus on early reductions of avoidable hospital admissions as the primary outcome.
Methods
Design
This is a pragmatic evaluation of the NAHS program for patients with COPD living in north-central Wisconsin. Specifically, all participants were members of Security Health Plan of Wisconsin, Inc., an affiliate of the Marshfield Clinic Health System. A cohort evaluation was used, including NAHS enrollees from July 2023 to the end of March 2024 vs. a propensity score matched comparison group of similar individuals not enrolled in NAHS.
Participants
All study participants had evidence of COPD in the health insurer’s database, per medical diagnostic codes. In additions, all participants had reasonable access to usual medical care given their insured status. Those in the NAHS group received their routine clinical care from their healthcare provider with the addition of the NuvoAir Home Service. In contrast, those in the non-NAHS group received routine care from their healthcare provider, and only anonymized claims data collected by their health insurer was subject to analysis. NuvoAir Home and standard care groups were propensity score matched based on sex, days from last inpatient event to enrollment, and disease severity (12 month pre enrollment: number of outpatient visits, ED, number of hospitalizations - all cause and COPD-specific). Both groups were selected from the same geographic areas in north-central Wisconsin. This study was a program evaluation and determined to be exempt by the Marshfield Clinic Health System Institutional Review Board.
NAHS
The NuvoAir Home Service is designed to incorporate the key components of evidence-based care, including remote monitoring and multidisciplinary team-based care to support patient self-management. The NAHS remote monitoring program includes daily heart rate and pulse oximetry testing and weekly home-based spirometry testing, which has been shown to detect COPD exacerbations up to 2 weeks prior to reported symptoms [
5]. Additionally, patients are asked to complete a digital version of the COPD Foundation’s My COPD Action Plan daily based on patient reported symptoms of dyspnea, cough, functional decline and others. The My COPD Action Plan is a key component of supported self-management programs, which are recommended by international guidelines, including GOLD [
6].
The NuvoAir Home Service includes remote interaction with a dedicated NuvoAir care coordinator who provides support and education, including COPD Foundation educational materials, for improved self-management of COPD. A NuvoAir Registered Nurse provides medical advice and triage for patients experiencing new or worsening symptoms. Finally, a NuvoAir physician or nurse practitioner provides consultation and urgent evaluation & treatment for those patients without access to same-day primary or specialty care for COPD exacerbations.
Outcomes
This report focuses on the first six months of participation in the study. The primary end point was the rate of hospitalizations and emergency Department visits. Secondary end points included the rate of hospital readmission in 30 days and the number of hospital days. Secondary analysis was performed to determine avoidable admissions and visits attributable to addressable conditions, including cardiopulmonary conditions and excluding major systemic cancer, musculoskeletal surgeries, and severe psychological conditions.
Analyses
Patients in the standard care group were selected using propensity score matching (PSM) with a ratio of 1:3. Matching was conducted based on sex, geographic location, disease severity (including number of hospitalizations, number of ED visits, number of outpatient visits related to all causes that may be impacted by the service, and also those related specifically to COPD in the 12 months prior to the start of intervention), the 12-month period included in the analyses (to avoid seasonal effect), and the number of days from the last day of any hospitalization to the start of intervention. For our primary outcome, the difference in the averaged rate of total and avoidable hospitalizations between the NuvoAir Home group and the standard care group was assessed using a generalized linear mixed effects model (GLMM) with a negative binomial link function. The matching strata was included as the random effect, and covariates such as age, disease severity, number of days from the last day of hospitalization to the start of intervention were included as fixed effects. A two-sided significance level of 0.05 was applied to all tests. The data manipulation and analyses were conducted using Python and R.
Results
Baseline characteristics
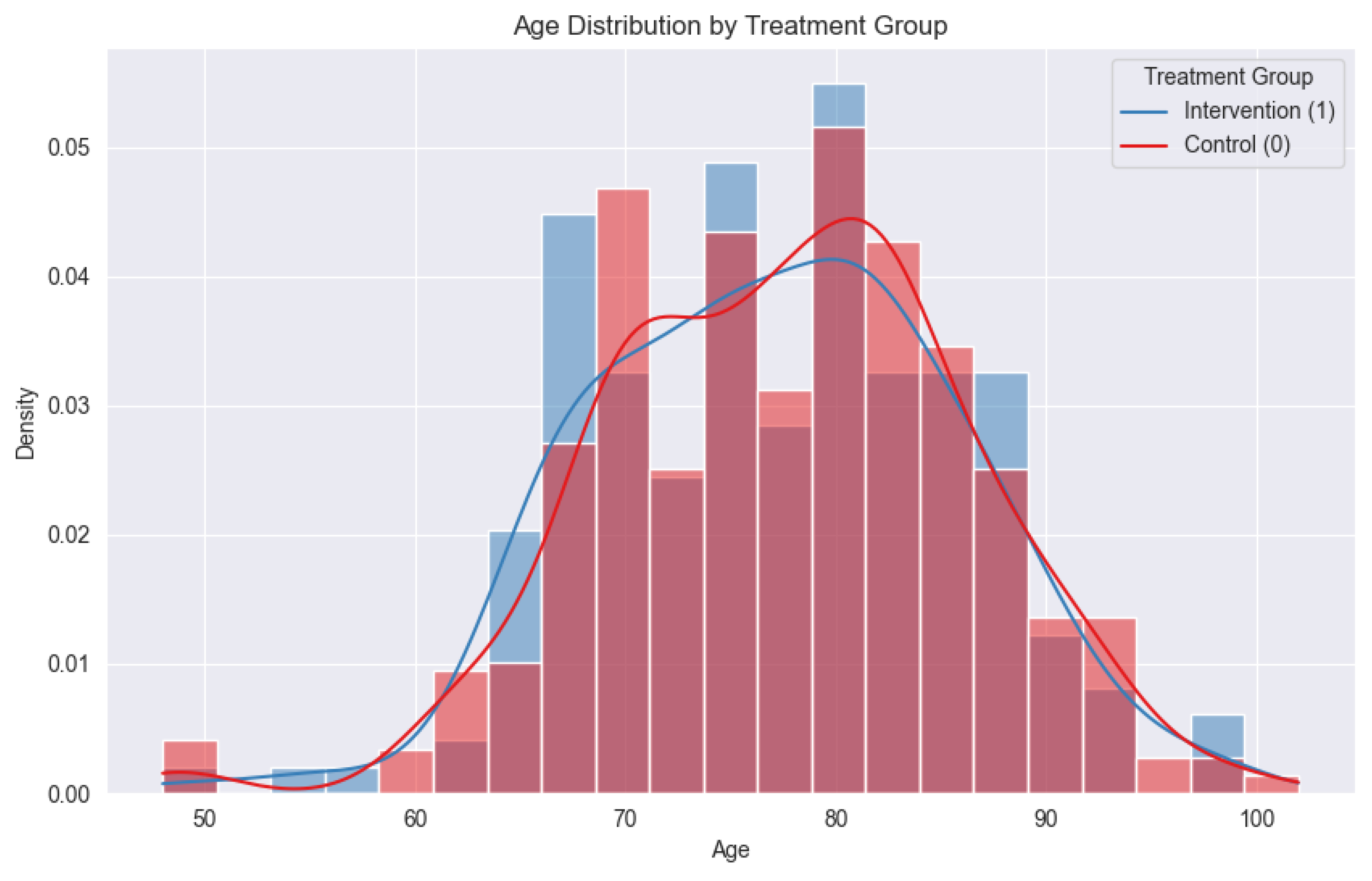
A total of 190 patients participated in NAHS for at least 6 months and were compared to 570 propensity-matched patients in the comparison group. At the time of this report preparation, the mean age of the intervention group was 77.2, while the mean age of the control group was 78.2 (
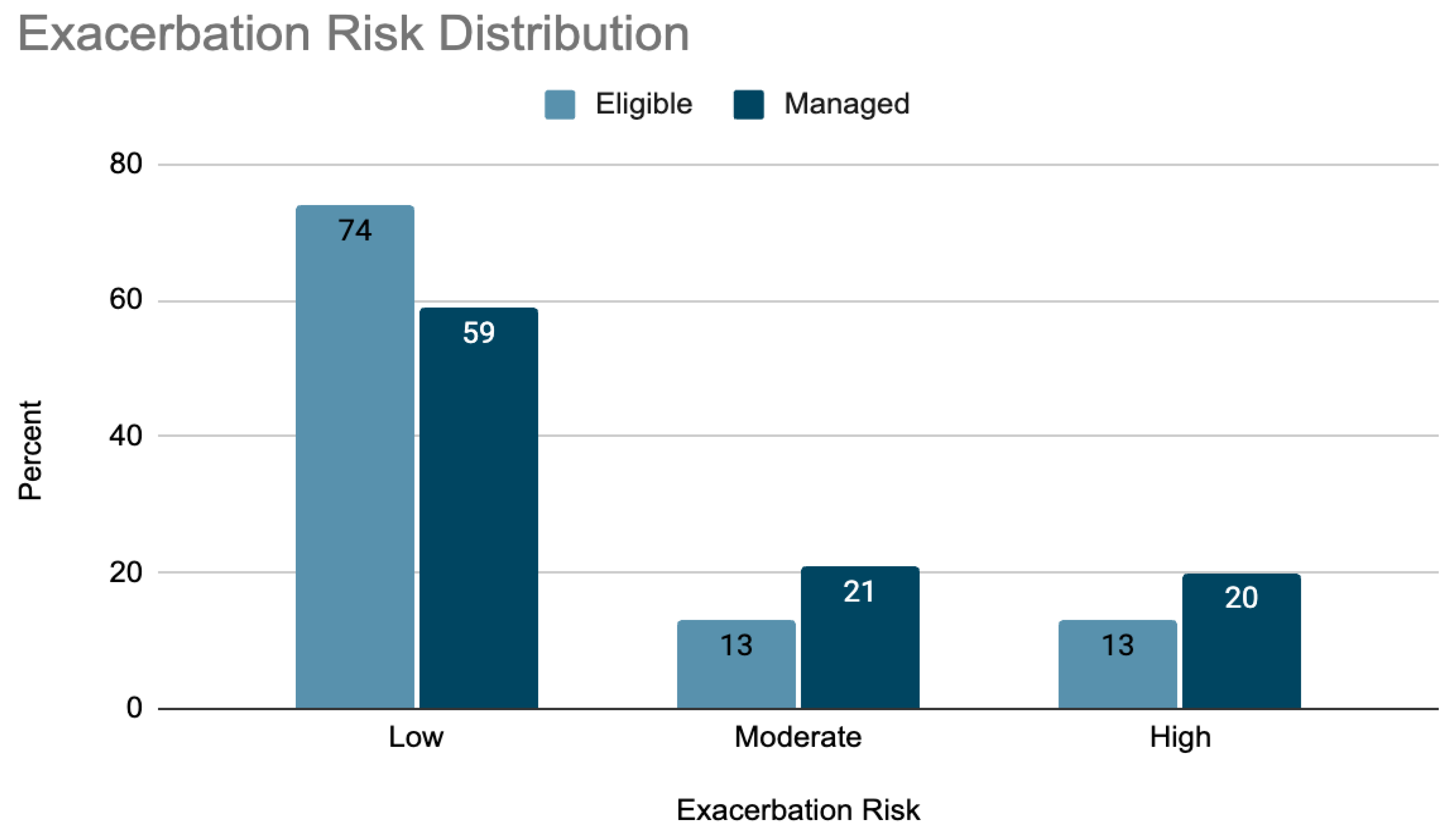
Figure 1). The percentages of females in the intervention group and the control group were 54.2% and 57.2% respectively. Most participants were between the ages of 70 and 90, with significant numbers above 90. Moderate and high-risk members (those with multiple outpatient claims for COPD, and those with one or more ED visits or hospital admission in the past 12 months, respectively) were somewhat more likely to participate in the NuvoAir Home Service than low risk members (
Figure 2).
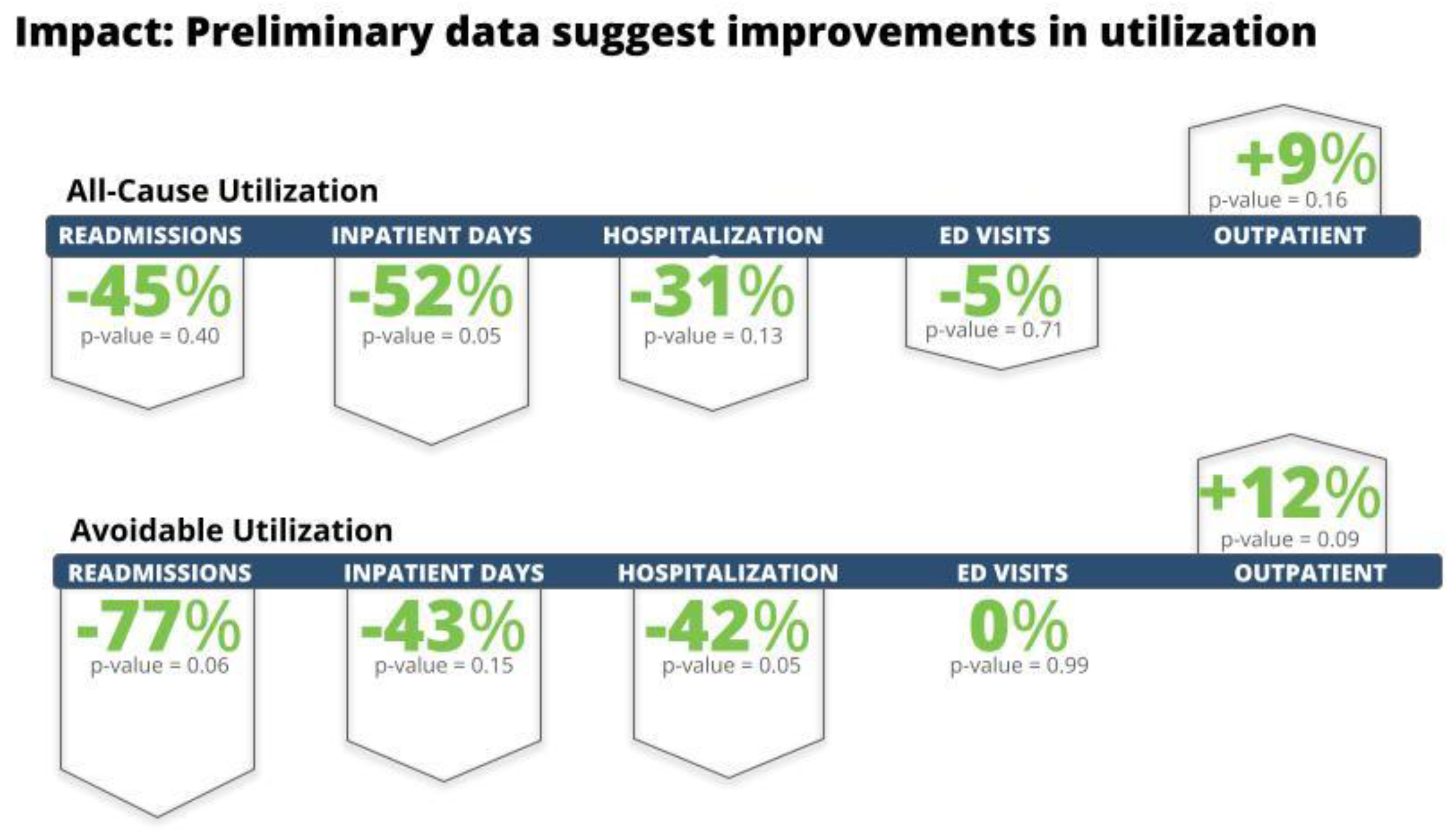
Interim study results after six months indicated that the NAHS group experienced several clinically significant positive impacts. As outlined in
Figure 3. Rates of avoidable readmissions, inpatient days, and hospitalizations were 77%, 43%, and 42% lower, respectively, in the NAHS groups vs. the non-NAHS group. All cause readmissions, inpatient days, and hospitalizations were 45%, 52%, and 32% lower, respectively. All cause and avoidable outpatient visits were increased modestly, as expected, and there was no significant change in ED visit rates. Further details are outlined in
Table 2. These results were in the expected direction, shifting utilization from the inpatient to outpatient setting, though not statistically significant. No patient safety events were detected during the program to date.
Table 1.
Baseline clinical characteristics in the intervention and control groups in the 12 months prior to engagement date.
Table 1.
Baseline clinical characteristics in the intervention and control groups in the 12 months prior to engagement date.
| Variable |
Control Group |
Intervention Group |
P- value |
| all-cause hospitalizations |
0.27 |
0.23 |
0.41 |
| all-cause days hospitalized |
1.30 |
0.87 |
0.11 |
| all-cause readmissions |
0.01 |
0.01 |
0.84 |
| all-cause ED visits |
0.79 |
0.83 |
0.68 |
| all-cause outpatient office visits |
8.89 |
9.46 |
0.08 |
| Avoidable Hospitalizations |
0.28 |
0.25 |
0.45 |
| Avoidable Days hospitalized |
1.15 |
0.75 |
0.12 |
| Avoidable Readmissions |
0.04 |
0.04 |
0.83 |
| Avoidable ED visits |
0.62 |
0.67 |
0.44 |
| Avoidable outpatient office visits |
5.70 |
6.16 |
0.10 |
Conclusion
COPD is an important driver of potentially avoidable death, disability, hospitalization, and health care spending. While participation in this evaluation was uncompensated, conditions were met for RPM and CCM reimbursement, meaning that this program could be implemented in a commercial setting. To our knowledge, this is the first large-scale evaluation of a commercially available clinical service to demonstrate that remote physiological monitoring combined with integrated chronic care management can improve clinical outcomes for patients with COPD.
This interim report suggests that the NuvoAir Home Service is effective in reducing all-cause hospital admissions, readmissions, and hospital days. While not statistically significant, the findings are yet preliminary and could change as further follow-up time accrues. Further analyses, including total cost of care, will be analyzed and reported at the end of the 12-month evaluation.
Author Contributions
Eric Harker, Jeffrey Van Wormer, and Dandi Qiao participated in the conception and design of the study, the acquisition of the data, data analysis and/or interpretation, writing and editing of the article.
Data Sharing
The data supporting this evaluation will not be publicly available.
Author Affiliations
Eric Harker: Chief Medical Officer, NuvoAir Medical Inc, Boston MA. Dandi Qiao: Data Scientist, NuvoAir Medical Inc, Boston MA. Jeffrey VanWormer PhD, Director of the Center for Clinical Epidemiology and Population Health, Marshfield Clinic Research Institute. Marshfield WI
Declaration of Interest
Both Eric Harker and Dandi Qiao are employees of NuvoAir Medical Inc, Boston MA. Jeffrey Van Wormer is an employee of Marshfield Clinic Health System, Marshfield WI.
Statement of Funding Support
This evaluation and all related work were funded by the sponsor, NuvoAir Medical Inc. ClinicalTrials.gov ID NCT05955482.
Abbreviations
PROMISE, NAHS, COPD, CMS, RPM, CCM, ICD10, IRB, GOLD, PSM, GLMM
References
- Saloni Dattani, Fiona Spooner, Hannah Ritchie and Max Roser (2023) - “Causes of Death” Published online at OurWorldinData.org. Accessed Nov 3, 2024. https://ourworldindata.org/causes-of-death.
- Global health estimates: Leading causes of DALYs Disease burden, 2000–2021. Published 2024. Accessed Oct 29, 2024. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/global-health-estimates-leading-causes-of-dalys.
- Torabipour A, et al. Cost Analysis of Hospitalized Patients with Chronic Obstructive Pulmonary Disease: A State-Level Cross-Sectional Study. Tanaffos. 2016;15(2):75-82.
- Müllerová H, et al. Association of COPD exacerbations and acute cardiovascular events: a systematic review and meta-analysis. Ther Adv Respir Dis. 2022 Jan-Dec;16:17534666221113647. [CrossRef]
- Watz, H., et al. Spirometric changes during exacerbations of COPD: a post hoc analysis of the WISDOM trial. Respir Res 19, 251 (2018). [CrossRef]
- GLOBAL STRATEGY FOR PREVENTION, DIAGNOSIS AND MANAGEMENT OF COPD: 2024 GOLD Report. Published 2024. Accessed Oct 29, 2024. https://goldcopd.org/2024-gold-report/.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).