1. Introduction
Diabetic patients not only have high blood glucose, but also tend to have increased triglycerides and low-density lipoprotein-cholesterol (LDL-C), which may contribute to atherosclerosis of the blood vessels, thereby predisposing patients to embolism and lesions, which in turn increase the risk of stroke, hypertension, or myocardial infarction. Angioplasty may also predispose patients to a range of pathologies in the feet. With a reduction in blood flow to the foot, patients may notice a weaker pulse and lowered temperature in the region. Furthermore, injuries occurring in the feet region may not tend to heal as readily and are prone to infection.
Depending on blood glucose concentrations, diabetes can be classified as follows:
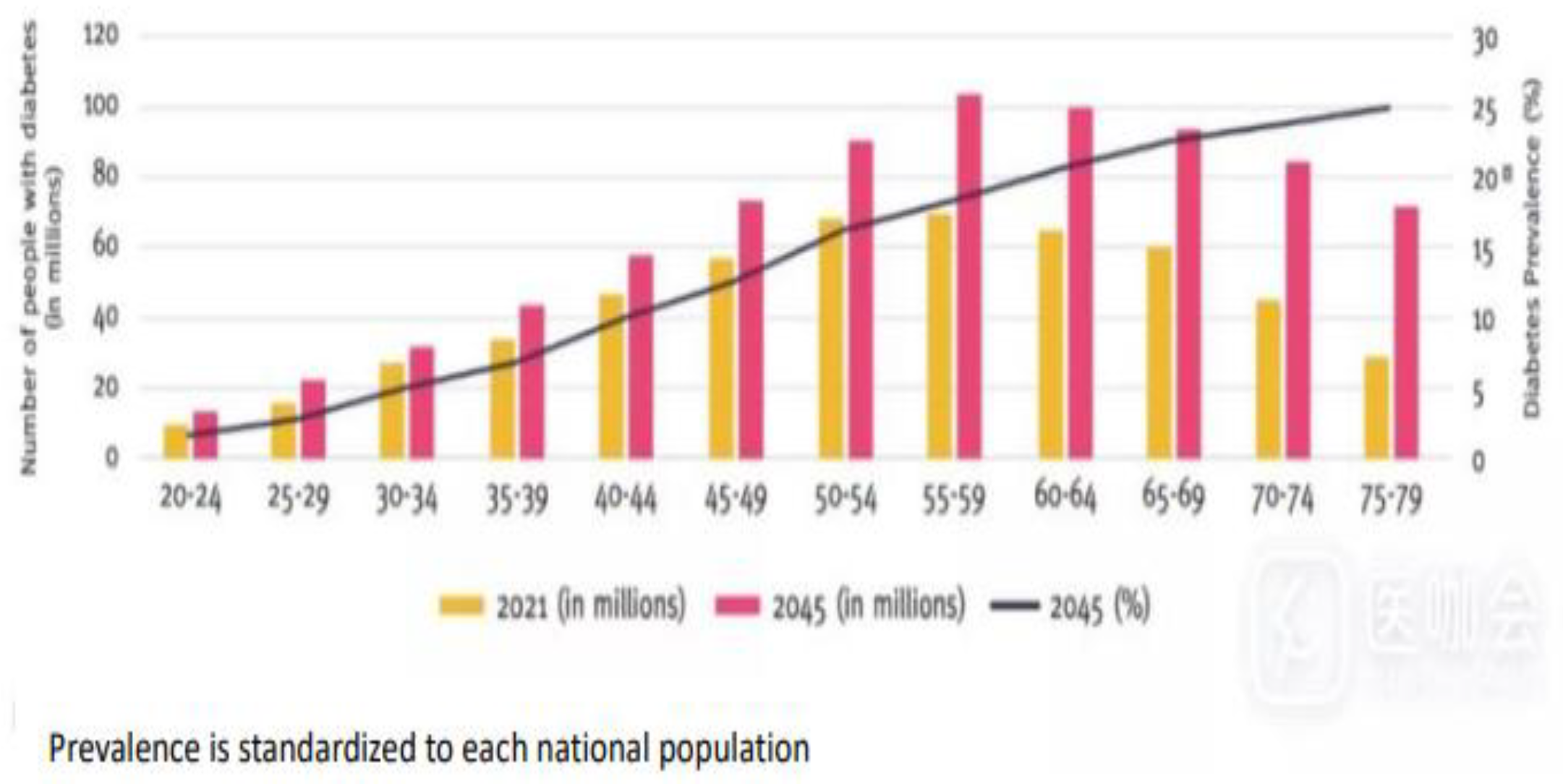
Figure 1.
Number of people with diabetes in adults (20-79 years) by age group in 2021 (columns) and estimated prevalence across age groups in 2045(black line) [
1].
Figure 1.
Number of people with diabetes in adults (20-79 years) by age group in 2021 (columns) and estimated prevalence across age groups in 2045(black line) [
1].
The 2021 diabetes prevalence estimates were applied to population estimates for 2045 to project future prevalence. Results The global diabetes prevalence in 20–79 year olds in 2021 was estimated to be 10.5% (536.6 million people), rising to 12.2% (783.2 million) in 2045. Diabetes prevalence was similar in men and women and was highest in those aged 75–79 year Prevalence (in 2021) was estimated to be higher in urban (12.1%) than rural (8.3%) areas, and in high-income (11.1%) compared to low-income countries (5.5%). The greatest relative increase in the prevalence of diabetes between 2021 and 2045 is expected to occur in middle-income countries (21.1%) compared to high- (12.2%) and low-income (11.9%) countries. Global diabetes-related health expenditures were estimated at 966 billion USD in 2021, and are projected to reach 1,054 billion USD by 2045. Conclusions Just over half a billion people are living with diabetes worldwide which means that over 10.5% of the world’s adult population now have this conditions
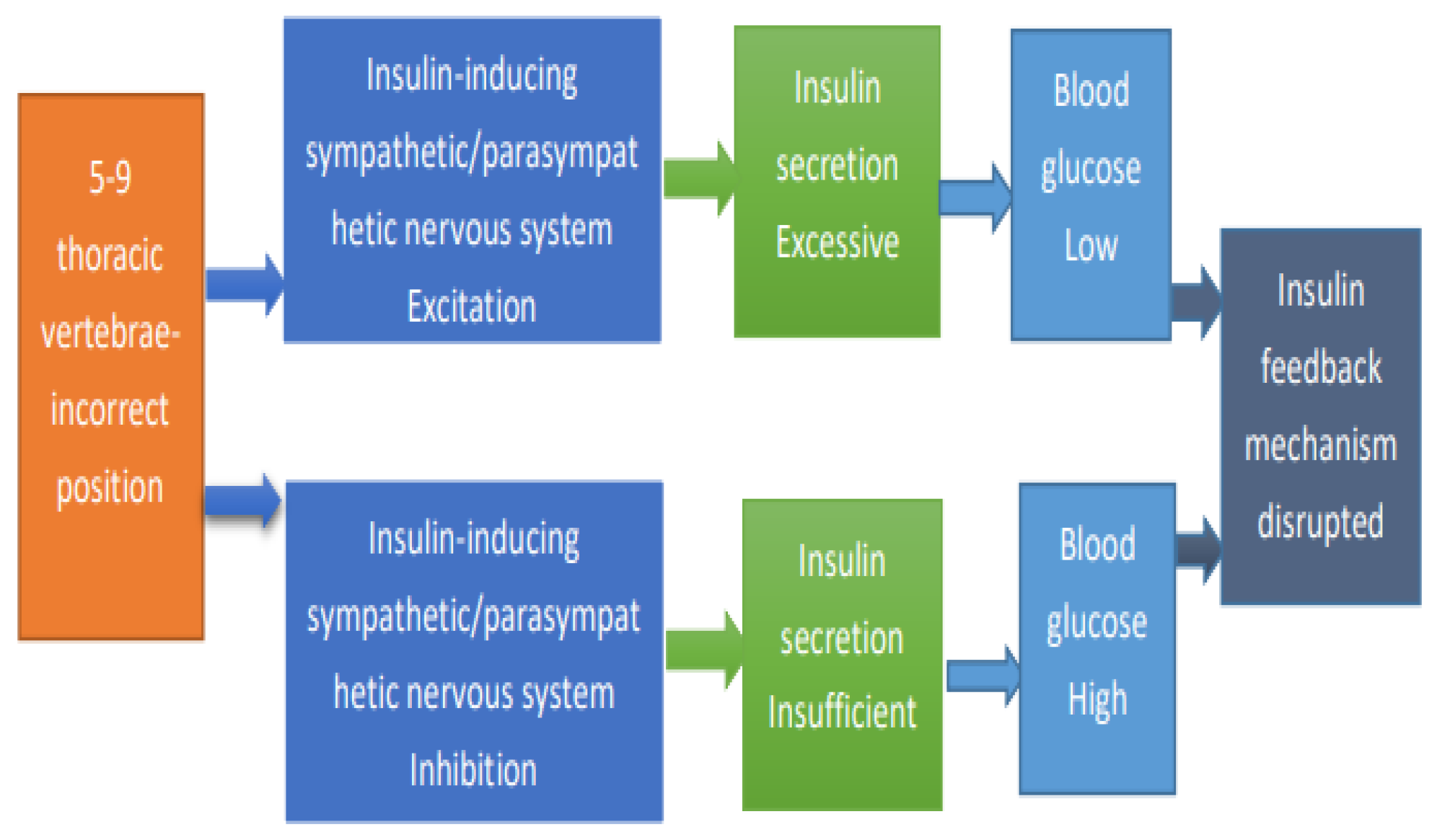
Figure 2.
Diabetes Pathology Diagram.
Figure 2.
Diabetes Pathology Diagram.
- A.
Type 1 Diabetes
Type 1 diabetes is also referred to as insulin-dependent diabetes mellitus (IDDM) or juvenile diabetes mellitus (IDDM) owing to the pathological inability of the body to produce sufficient insulin or to produce insulin at all, a congenital disorder that develops in most cases between infancy and adolescence, the cause of which is currently unknown [
2].
Figure 3.
Type 1 diabetes Symptoms and Causes.
Figure 3.
Type 1 diabetes Symptoms and Causes.
Physician Ratings at Cleveland Clinic [
3]
Some of the symptoms of type 1 diabetes and type 2 diabetes are:
Feeling more thirsty than usual.
Urinating often.
Losing weight without trying.
Presence of ketones in the urine. Ketones are a byproduct of the breakdown of muscle and fat that happens when there's not enough available insulin.
Feeling tired and weak.
Feeling irritable or having other mood changes.
Having blurry vision.
Having slow-healing sores.
Getting a lot of infections, such as gum, skin and vaginal infections.
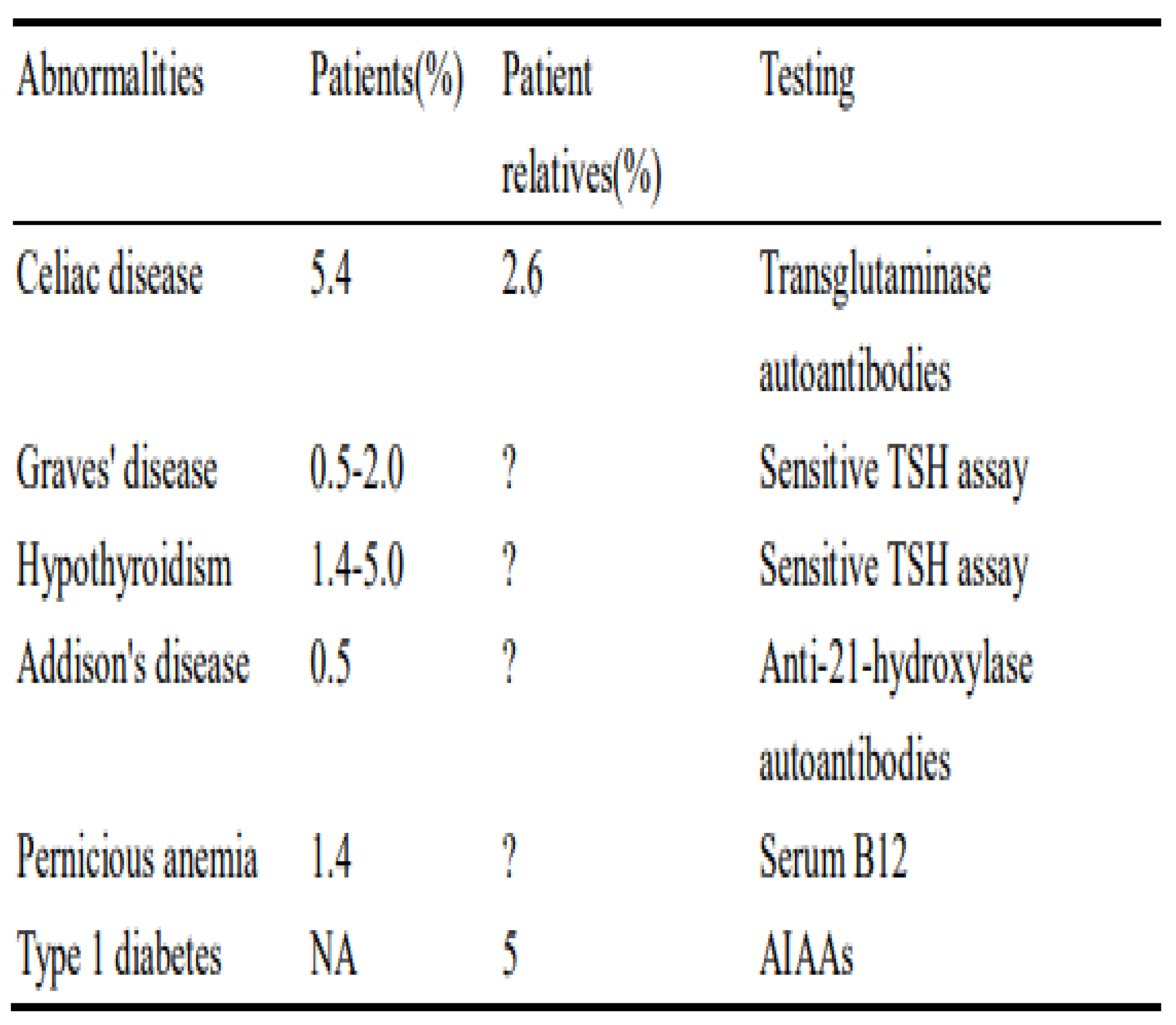
Table 1.
Autoimmune diseases of other organs associated with autoimmune type 1 diabetes [
4].
Table 1.
Autoimmune diseases of other organs associated with autoimmune type 1 diabetes [
4].
Type1 Diabetes Mellitus (T1DM) is an autoimmune disease that results in absolute insulin deficiency due to destruction of the pancreatic beta cells. It is frequently associated with other autoimmune diseases like autoimmune thyroid (AIT) disease, celiac disease (CD), Addison's disease (AD), and vitiligo. These diseases, including T1DM are associated with organ specific autoantibodies.
Adult-onset diabetes is caused by being overweight or a lack of exercise. Studies indicate that obesity is a major contributor to insulin resistance, making it one of the primary risk factors for type 2 diabetes. Research shows that dietary and lifestyle changes can lead to weight loss and reduce the risk of developing type 2 diabetes. Additionally, recent studies suggest that chronic inflammation may be linked to the condition, as 70-80% of patients are not obese. Type 2 diabetes is a metabolic disorder characterized by hyperglycemia, primarily due to insulin resistance and relative insulin deficiency. Unlike type 1 diabetes, where patients completely lose insulin production due to damage to pancreatic islet cells, type 2 diabetes is often caused by the consumption of highly refined diets and trans fats. Diabetes is now one of the chronic diseases in developed countries, with increasing numbers of potential patients, and there is a trend toward younger ages. Typical symptoms of type 2 diabetes include polyuria, polydipsia, and polyphagia. Approximately 90% of diabetes patients have type 2 diabetes, while the remaining 10% mostly consist of type 1 diabetes and gestational diabetes, which may be misdiagnosed. In high-risk populations with genetic predisposition to diabetes, obesity is considered the main cause of type 2 diabetes.
- B.
Type 2 Diabetes
Without a diseased state of the pancreas, type 2 diabetes begins with aberrant insulin resistance (abnormal and unresponsive cellular response to insulin) or cellular unresponsiveness to insulin. As the condition advances, insulin secretion can become increasingly inadequate [
5].
The therapy of diabetes varies according to the severity of the disease. Current treatment for type 1 diabetes consists of long-term insulin delivery to regulate the disease. As with type 2 diabetes and gestational diabetes, oral medicines can be used to treat the disease in addition to insulin. Diabetes has become one of the most prevalent diseases of civilization in industrialized nations, with an increasing number of potential patients and a tendency toward younger people. Typical symptoms of type 2 diabetes include polyuria, polytheist, and polyphagia. Type 2 diabetes accounts for around 90% of the diabetic population, with type 1 diabetes and gestational diabetes, the latter of which is frequently misdiagnosed, accounting for the remaining 10%. Obesity is typically regarded as the primary cause of type 2 diabetes among individuals at high risk of developing diabetes due to genetic factors.
Figure 4.
Cardiovascular Risk Reduction in Adults with Type 2 Diabetes [
6].
Figure 4.
Cardiovascular Risk Reduction in Adults with Type 2 Diabetes [
6].
Cardiovascular disease remains the leading cause of death in patients with diabetes. Cardiovascular disease in diabetes is multifactorial, and control of the cardiovascular risk factors leads to substantial reductions in cardiovascular events.
Objective to determine if the prevalence of cardiovascular risk factors (hypertension, diabetes, hyperlipidemia, obesity, and tobacco use), treatment rates, and control changed among adults aged 20 to 44 years from 2009 through March 2020, overall and by sex and race and ethnicity.
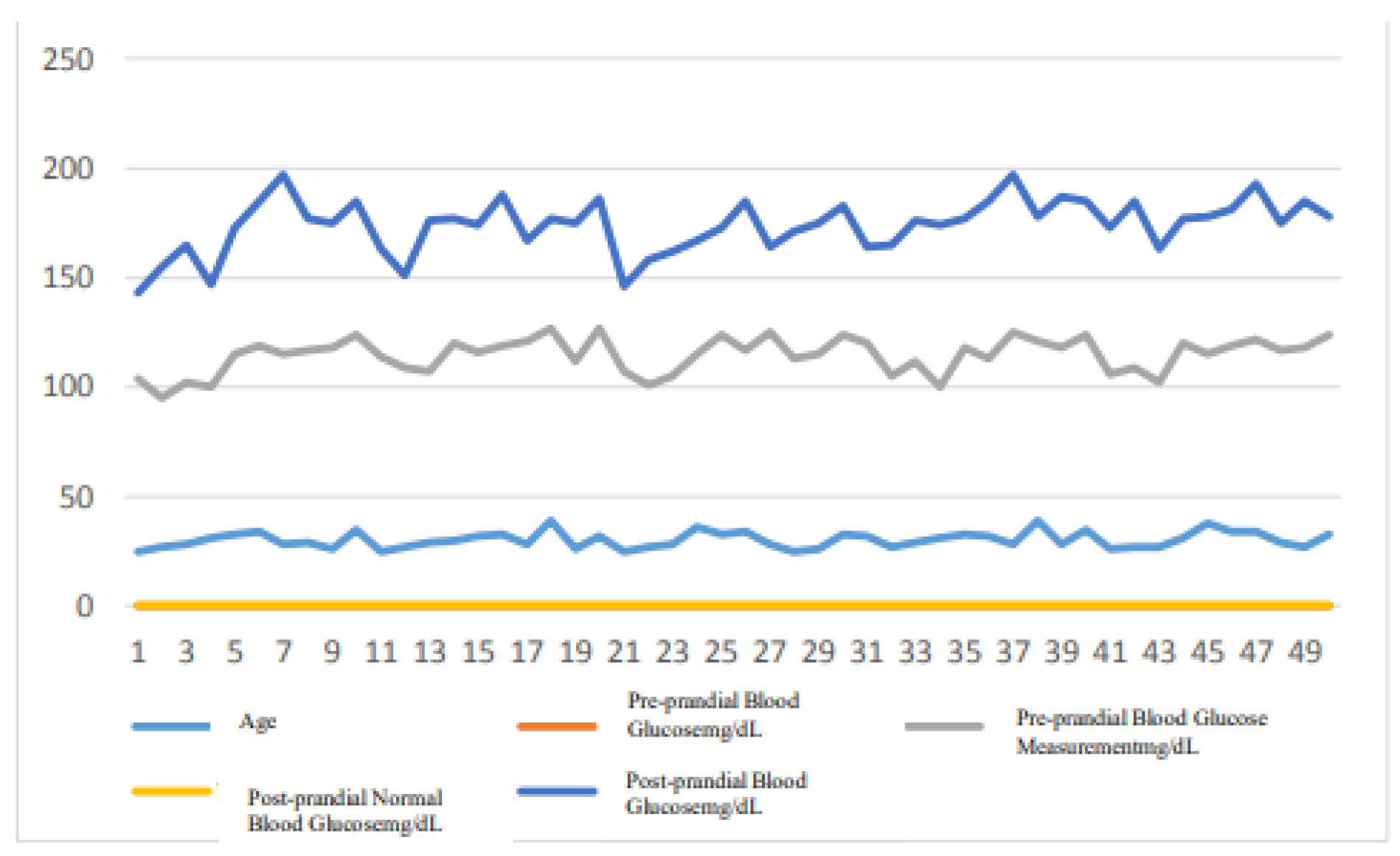
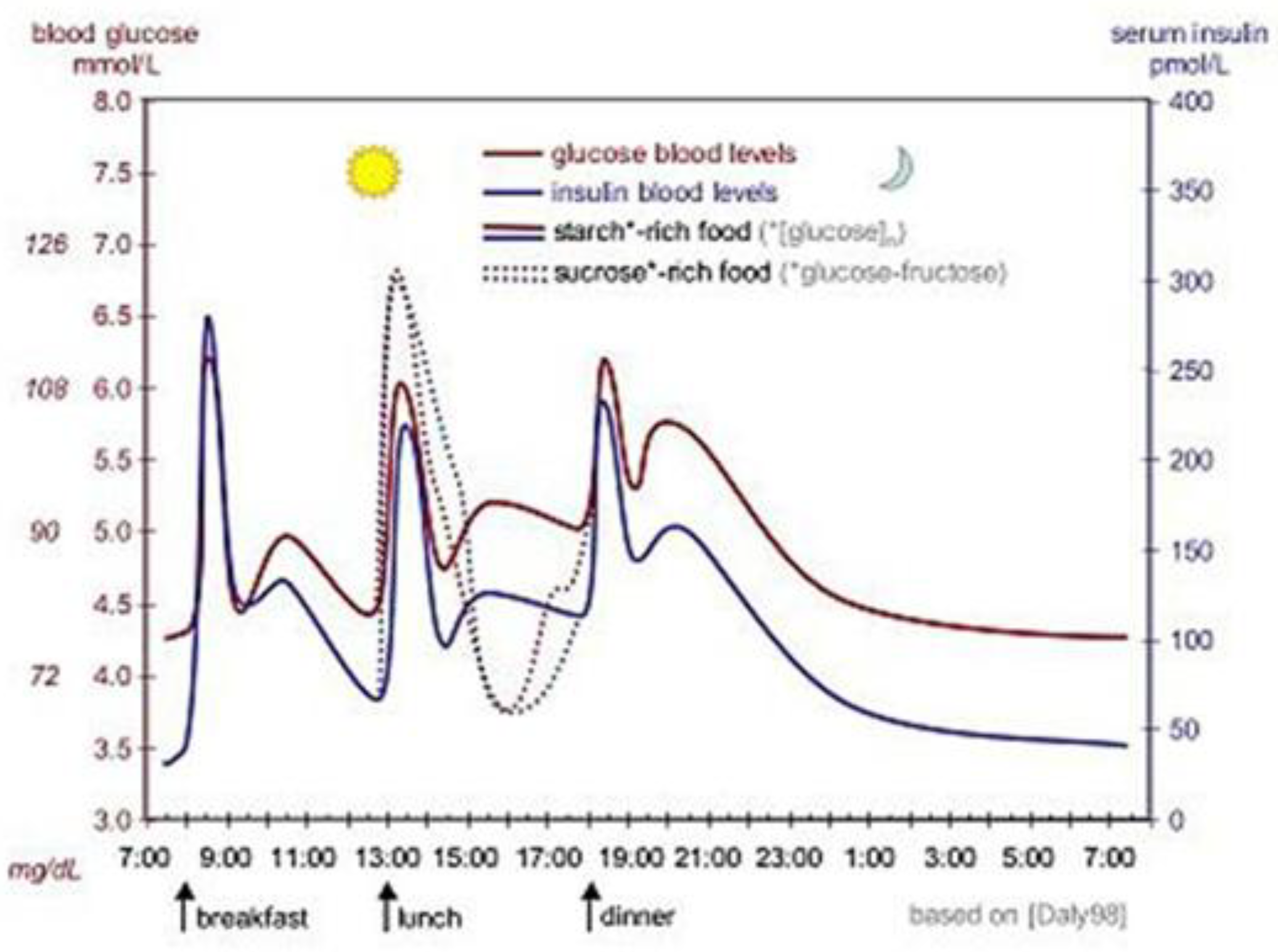
As shown in
Figure 5, the ideal curve of the fluctuations of blood glucose (red) and insulin (blue) concentration in the human body during a day (three meals). The solid line indicates the consumption of starch-rich foods, whereas the dotted line indicates the consumption of sucrose-rich foods. In the human body, glycemic concentrations are rigorously regulated and are commonly maintained at approximately 90 mg/dL (5 mmol/L). In the normal range of 4-7 mmol/L, which is the constant range of blood glucose [8]. Circulating glucose levels in blood are normatively in the range of 3.3-7.05 g (assuming that a human body contains 5 liters of blood, equivalent to the average blood volume of a human male). Blood glucose levels are elevated after one to two hours following consumption of food and fall to a minimum at the termination of sleeping periods.
Dysregulated blood glucose levels may result in a multitude of disorders, including persistent hyperglycemia with high blood glucose levels and hypoglycemia with low blood glucose levels. Continuous hyperglycemia resulting from a variety of causes may result in diabetes, the most prominent disease associated with blood glucose levels, while hypoglycemia may result in symptoms such as dizziness, inability to concentrate, and even shock. Apart from glucose, fructose, and galactose are also available in the blood, however, only the level of glucose concentration may be regulated metabolically through insulin. Under conditions of intense stress, fear and fatigue, adrenal hormones may surge and prevent insulin production, thus affecting blood glucose levels.
When the body's insulin supply is insufficient, glucose cannot be transported to cells via insulin and accumulates in the circulation, resulting in elevated blood glucose levels, while the immune system attacks the pancreatic cells, resulting in insufficient insulin production which in turn causes type 1 diabetes.
Insulin resistance is the aberrant capacity of cells to utilize insulin, whereby insulin cannot efficiently metabolize glucose, resulting in glucose retention in the circulation and in the urine while the kidneys are unable to recover it adequately. Since the cells do not receive enough energy, the body believes it should produce more insulin to transport glucose, so it produces insulin day and night. However, the cells are already resistant to insulin, so they do not receive enough energy, and the body finally loses weight rapidly. Ninety percent of the causes of diabetes are attributable to insulin resistance. Possible causes include obesity, heredity, and old age.
Prevention and treatment of diabetes include maintaining a balanced diet, exercising regularly, quitting smoking, and maintaining an ideal body weight. Blood pressure control and foot care are also very important for people with diabetes. Type 1 diabetes requires insulin injections to control blood glucose, while type 2 diabetes can be controlled with oral medications and, if needed, with insulin injections [9]. Some of the oral medications used for diabetes and insulin may cause hypoglycemia [10]. For patients with type 2 diabetes who also have obesity, bariatric surgery is an effective treatment [11]. In patients with gestational diabetes, blood glucose usually returns to normal after delivery [12].
Figure 6.
Type 2 diabetes Symptoms and Causes [13].
Figure 6.
Type 2 diabetes Symptoms and Causes [13].
Type 2 diabetes can cause various health problems, like heart disease, kidney disease and stroke. You can manage this disease by making lifestyle changes, taking medications and seeing your healthcare provider for regular check-ins.
Symptoms of Type 2 diabetes
Increased thirst (polydipsia).
Peeing more frequently.
Feeling hungrier than usual.
Fatigue.
Slow healing of cuts or sores.
Tingling or numbness in your hands or feet.
Blurred vision.
Dry skin.
Type 3 diabetes: Recent research indicates that Alzheimer’s disease is essentially the brain’s inability to respond to insulin, leading to hyperglycemia in the brain and cognitive decline, referred to as type 3 diabetes. Gestational diabetes mellitus (GDM) refers to the onset of hyperglycemia during pregnancy in individuals with no prior history of diabetes. Symptoms of diabetes: Type 1 diabetes often develops rapidly and is easily detected, while most patients with type 2 diabetes show no early symptoms until blood tests reveal the condition or symptoms such as blurred vision and cardiovascular issues manifest.
Diabetes risk: Type 1 diabetes is related to autoimmune disorders, with higher prevalence among children and young individuals with a family history of type 1 diabetes. Additionally, those with a family history of latent autoimmune diabetes in adults (LADA) have an increased risk after age 30.
In contrast, type 2 diabetes, which is not autoimmune-related, is primarily influenced by lifestyle factors. Risk factors include prediabetes, obesity, age 45 or older, a family history of type 2 diabetes, engaging in less than three weekly exercise sessions, a history of gestational diabetes, or birth weight exceeding 4,000 grams. Furthermore, recent studies show a clear link between Alzheimer’s disease and diabetes, with prediabetics and type 2 diabetics having a higher risk of Alzheimer’s in later life. As a result, Alzheimer’s is sometimes referred to as type 3 diabetes.[14]
Other types of diabetes: Certain diabetes types are distinct from type 1, type 2, and gestational diabetes. These include:
β-cell genetic defects (β-cell insulin secretion),
Genetic insulin resistance,
Pancreatic diseases,
Hormonal disorders,
or diabetes caused by chemicals or drugs.
Complications: Diabetic complications primarily manifest as microcirculatory disorders affecting the cardiovascular system, cerebrovascular system, retina, peripheral vessels, and kidneys, and can also lead to neuropathy. Diabetic retinopathy results from prolonged hyperglycemia, damaging the endothelial cells of the retinal blood vessels, causing a series of retinal conditions, such as micro aneurysms, hard exudates, cotton wool spots, neovascularization, vitreous proliferation, and even retinal detachment. Retinal changes usually appear after ten or more years in diabetes patients, although those with poor glycemic control or type 1 diabetes may experience these changes earlier, necessitating regular ophthalmologic check-ups. Diabetic nephropathy can progress through five stages, ultimately leading to kidney failure. Diabetic patients have a significantly higher risk of developing nephropathy compared to non-diabetics, with approximately half of type 2 diabetes patients affected. In advanced stages, nephropathy can cause kidney failure, requiring dialysis or kidney transplantation. Reduced renal function also increases the risk of other diabetes-related complications, such as hypoglycemia and cardiovascular disease. Diabetic peripheral neuropathy (DPN), a common long-term complication, is caused by chronic metabolic imbalances affecting the vascular system and leading to nerve damage. Symptoms include severe pain, tingling, burning, numbness, and persistent dysesthesia in the lower limbs, arms, and fingers, affecting quality of life, sleep, and emotional well-being. Advanced complications include foot ulcers, Charcot neuropathic osteoarthropathy, and even amputation. Comorbidities include depression, autonomic neuropathy, cognitive dysfunction, peripheral artery disease, and cardiovascular disease. Insulin plays a crucial role in regulating glucose absorption in most tissues, particularly muscle and adipose cells, excluding neurons in the central nervous system. Insulin deficiency and cellular insensitivity to insulin are central to all types of diabetes. Most carbohydrates in food are converted into glucose monosaccharaides within hours, which is the primary carbohydrate in the bloodstream. Some carbohydrates, like fructose, are not converted into glucose but still provide cellular energy. Additionally, cellulose, despite being composed of glucose molecules in long chains, cannot be digested and converted into glucose because the human digestive system lacks the necessary enzymes. When blood glucose levels rise after meals, β-cells release insulin into the bloodstream. Insulin facilitates glucose absorption by most cells, especially muscle and fat cells, either for immediate energy use or storage. Insulin also regulates the conversion of glucose and glycogen in the liver and muscle cells. When blood glucose levels decrease, β-cells reduce insulin secretion, lowering glucose conversion into glycogen.
2. Measurement Accuracy
Pre-diabetes is a disorder characterized by blood sugar levels that fluctuate between normal and diabetic levels. Pre-diabetes is typically asymptomatic, but if it is not carefully managed, it can rapidly progress into diabetes. However, the early stages of diabetes are typically asymptomatic, and approximately one-third of individuals are unaware they have the condition; hence, routine health screenings are necessary to diagnose diabetes early.
Blood glucose testing is a type of blood test that measures the concentration of glucose in whole blood, serum or plasma samples. It is mainly conducted via chemical and enzymatic methods. Chemical methods utilize the non-specific reductive properties of glucose in reactions in which a chromogenic indicator is added to identify its concentration through color changes. However, other reductive substances such as urea (in particular blood from uremic patients) may also be present in the blood, resulting in an error of 50-150 mg/L in chemical methods. Enzymatic methods are free of such issues due to the high specificity of glucose binding. Commonly utilized enzymes include glucose oxidase and hexokinase. [15]
Fasting blood glucose concentration serves as a universal indicator of glucose homeostasis, with standard values of 700-1100 mg/: (70-110 mg/dl). Both excessive and insufficient values may indicate disease-related conditions.
For definitions and coding of serum/plasma fasting glucose items in the LOINC terminology standards, please refer to this page.
For most individuals, 80 to 99 milligrams of glucose per deciliter prior to a single meal and 80 to 140 milligrams per deciliter postprandial is considered normal. The American Diabetes Association states that most non-pregnant adults with diabetes are expected to have between 80 and 130 mg/dL prior to meals and under 180 mg/dL in the first 1-2 hours after meals. This variation in blood glucose levels before and after a meal reflects the way in which the body absorbs and stores glucose. Following a meal, your body breaks down the carbohydrates in your food into smaller portions, which include glucose, which can be absorbed by the small intestine. [16]
3. Experimental Module
This study adopts a quantitative module approach utilizing statistics data as follows:
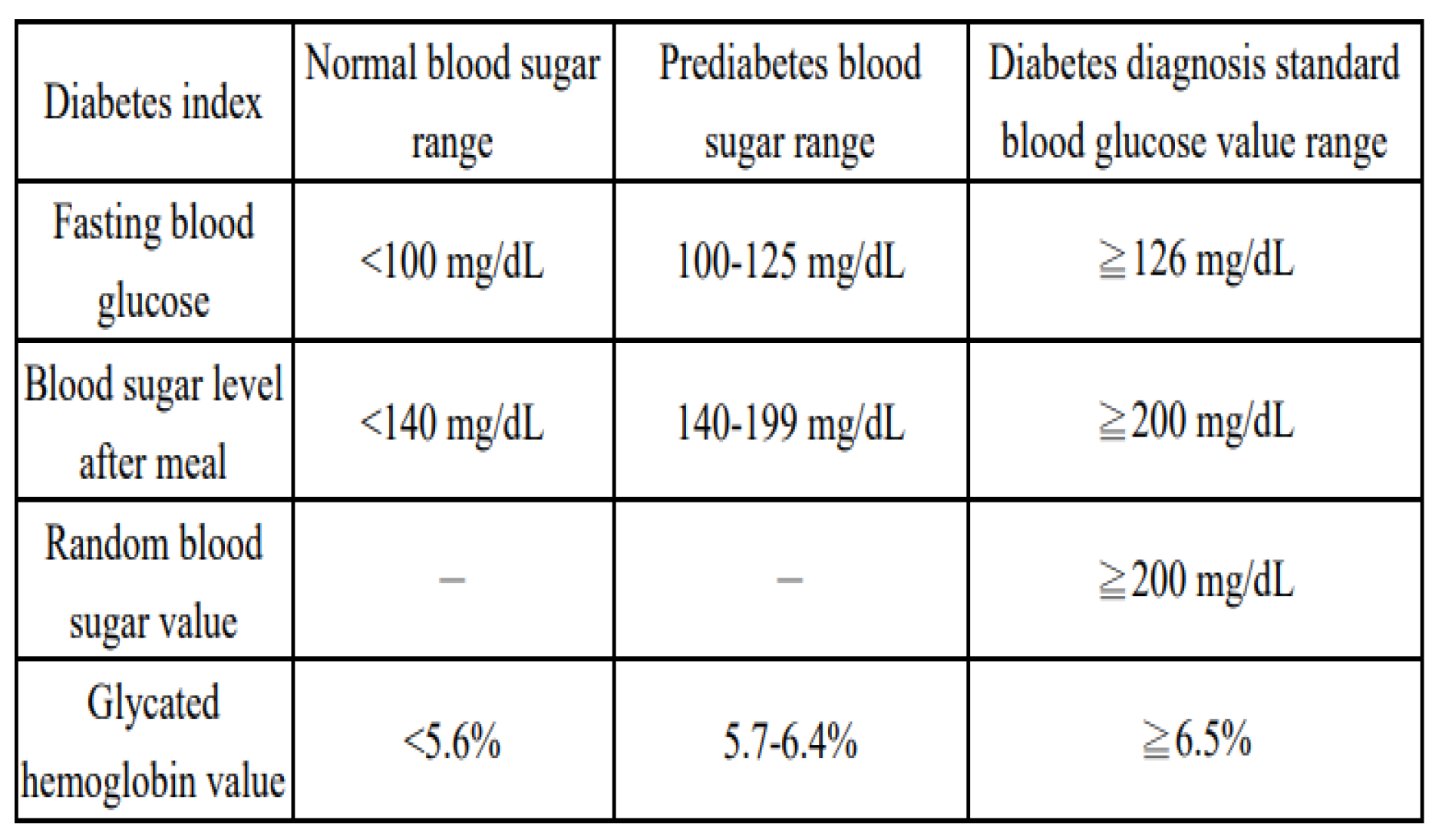
Table 2.
Diabetes diagnostic criteria [17].
Table 2.
Diabetes diagnostic criteria [17].
A questionnaire survey was conducted on 250 employees of an enterprise, aged from 25 to 65 years old, following analysis and screening, 50 men aged 40 to 55 years old and 50 women of the same age stratum were enrolled in a 60-day normal blood glucose measurement, with the following statistics:
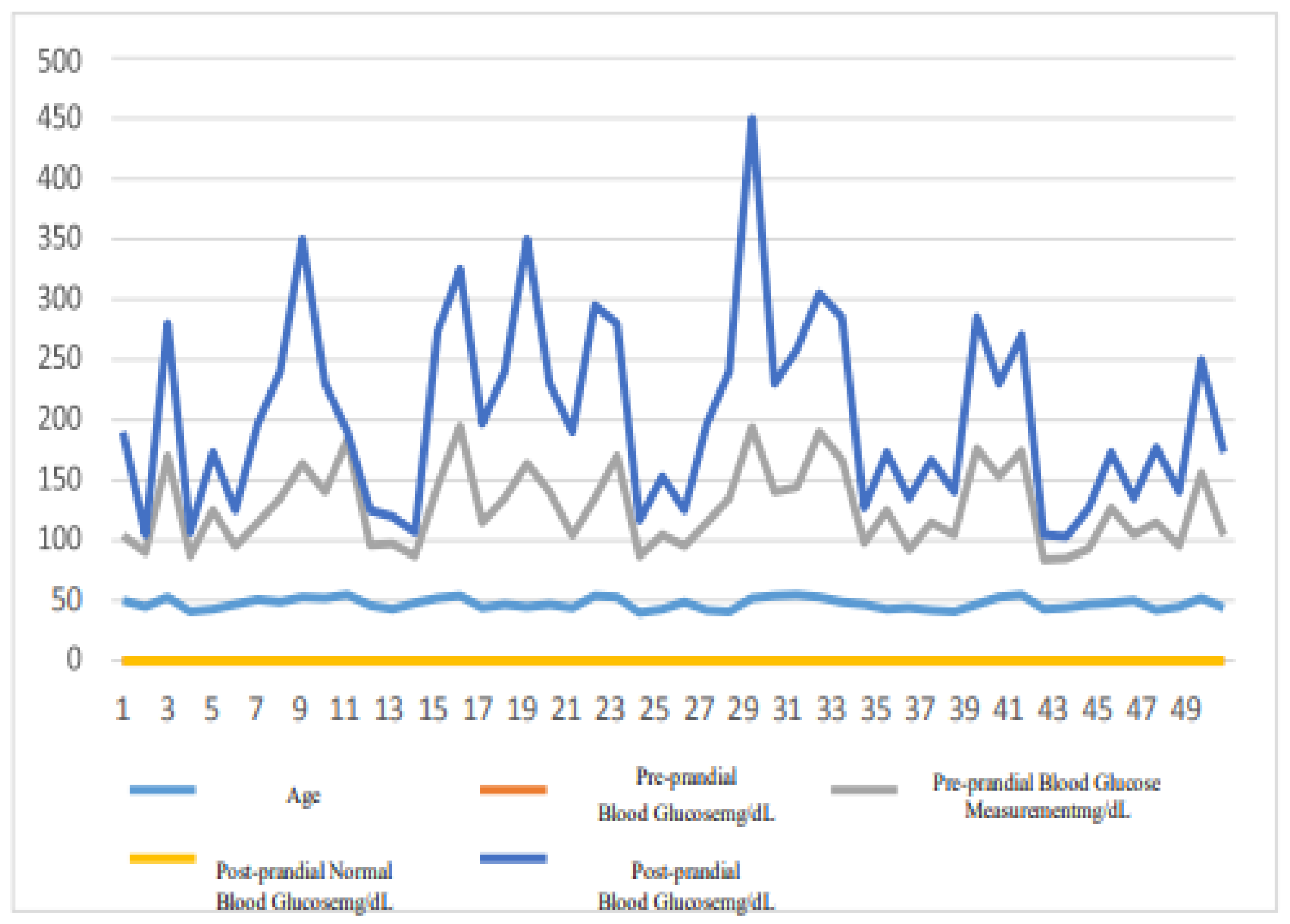
Figure 7.
Cumulative records of normal blood glucose measurements in males over a 60-day period.
Figure 7.
Cumulative records of normal blood glucose measurements in males over a 60-day period.
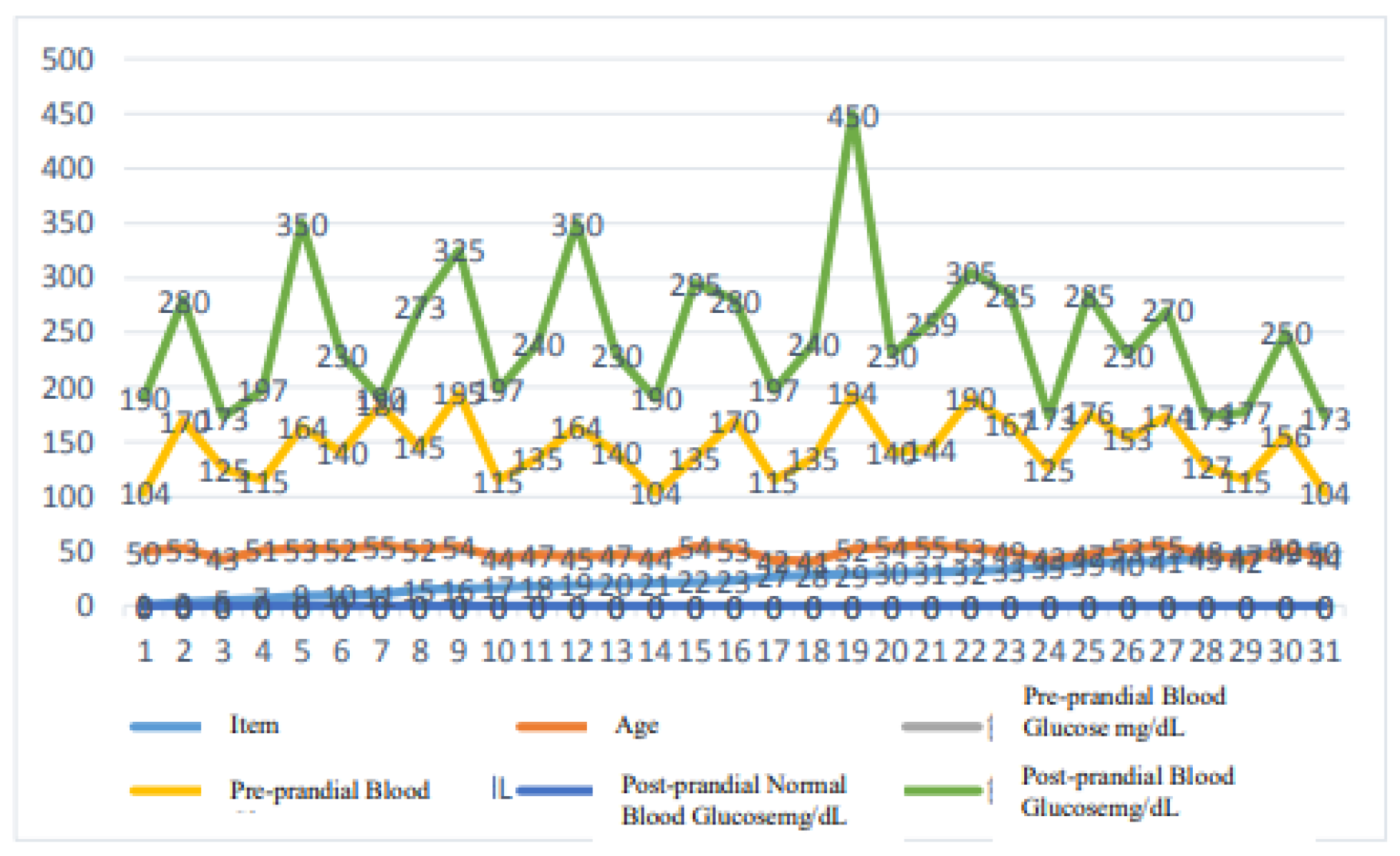
Figure 8.
Cumulative records of male diabetic patients with interfering factors in blood glucose measurements over a 60-day period.
Figure 8.
Cumulative records of male diabetic patients with interfering factors in blood glucose measurements over a 60-day period.
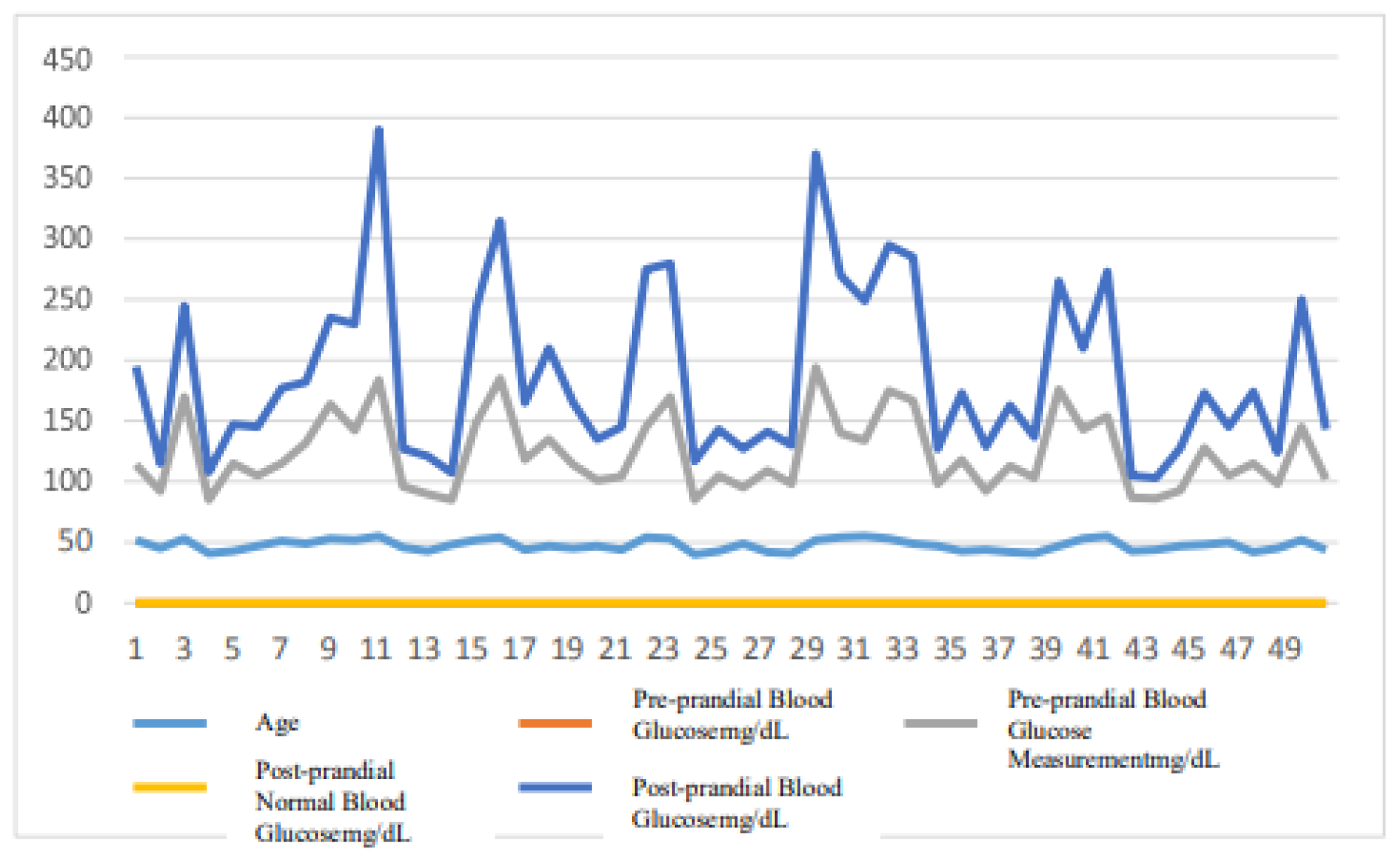
Figure 9.
Cumulative records of normal blood glucose measurements in females over a 60-day period.
Figure 9.
Cumulative records of normal blood glucose measurements in females over a 60-day period.
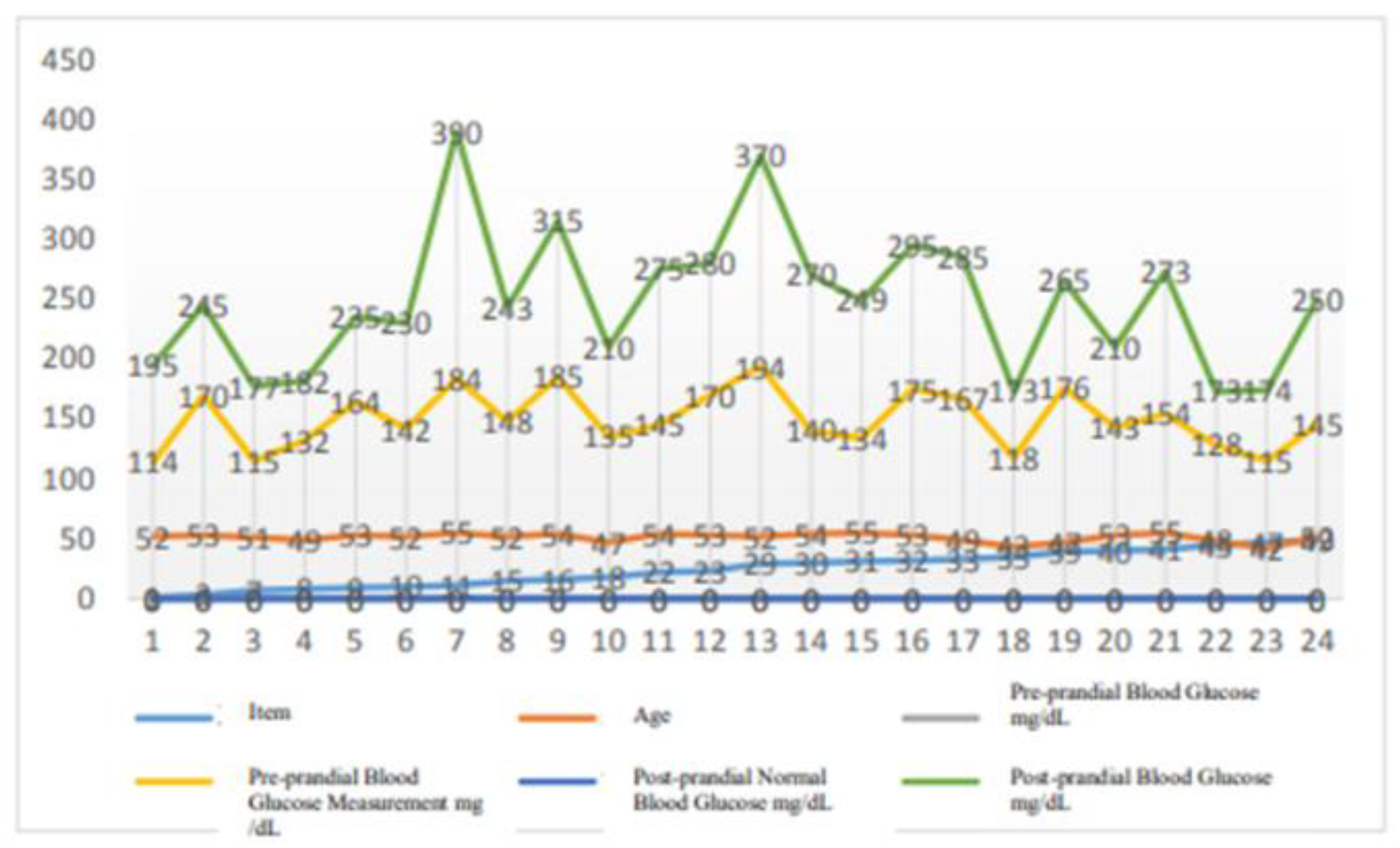
Figure 10.
Cumulative records of female diabetic patients with interfering factors in blood glucose measurements over a 60-day period.
Figure 10.
Cumulative records of female diabetic patients with interfering factors in blood glucose measurements over a 60-day period.
A. in
Figure 8 and
Figure 10, 50 males aged from 40 to 55 and 50 females in the same age range had varying blood glucose indices before and after meals for 60 days of normal blood glucose measurements, dependent on age and physical conditions.
B. in
Figure 7 and
Figure 9, men and women with diabetes had interfering factors before and after meals during the 60-day period, while their blood glucose indices were abnormally high. The results of this examination demonstrate that environmental, physiological, and dietary factors contribute to the cause of diabetes.
What is the origin of diabetes? Insulin transports glucose from the blood into cells to provide cellular energy for operation. With insufficient supply of insulin in the body, body tissues are unable to uptake energy where glucose remains in the blood instead of entering the cells, resulting in abnormally high blood glucose levels.
Figure 11.
Composite standard and normal blood glucose measurements among 50 males d females aged from 25 to 39 years.
Figure 11.
Composite standard and normal blood glucose measurements among 50 males d females aged from 25 to 39 years.
C.
Figure 8 is a composite of pre and postprandial normal blood glucose measurements for 50 subjects, both male and female, aged 25 to 39 years, compared with the standard pre and postprandial blood glucose ranges published by the International Diabetes Federation (IDF). [16]
Diabetes is a disorder that prevents normal blood sugar management! The diabetes index is the key to understanding the condition.
The blood glucose value refers to the glucose concentration in the blood. "mg/dL" represents the number of milligrams (mg) of glucose per 100 milliliters (dL) of plasma. When food is digested and absorbed into the circulation, blood glucose level rises, prompting the release of substantial quantities of insulin in an effort to lower the blood glucose level.
The progression of diabetes will result in several complications, which may have a negative impact on patients' health and quality of life. The frequency of periodic blood glucose testing is dictated by the primary care physician's prescriptions.
Significant diabetes indicators that can identify prediabetes and diabetes include fasting blood glucose, postprandial blood glucose, random blood glucose, and glycated hematocrit, each of which has a distinct significance.
Fasting blood glucose values:
The pre-meal glucose value, measured in milligrams per deciliter (mg/dL), and fasting glucose value are glucose values taken after 8 hours of fasting, and are often tested in the morning before breakfast. The fasting blood glucose level can indicate whether or not the pancreas is able to release insulin to keep the blood glucose level within the normal range when the individual is fasting.
Postprandial blood glucose values:
The post-meal glucose value, measured in milligrams per deciliter (mg/dL), is the glucose value tested two hours after the first bite of a meal; for instance, if the first bite of lunch is had at 12:00 p.m., the post-meal glucose value should be evaluated at 2:00 p.m. The post-meal glucose level can indicate if insulin is effective after a meal, allowing the fast increasing blood glucose level to return to the normal range within a particular amount of time.
Random blood glucose values:
Measured in milligrams per deciliter, the random blood glucose value is the blood glucose level taken at any random time of the day, regardless of whether the individual is fasting or eating.
Glycosylated hematocrit values:
Measured as a percentage. Glycated hemoglobin is the result of the interaction of hemoglobin and glucose in red blood cells; the higher the normal blood glucose level, the higher the level of glycated hemoglobin. What is the blood glucose level at which pre-diabetes or diabetes will be diagnosed? [18]
Diabetes Index Summary
Normal blood glucose value range:
Normal value of fasting blood sugar: <100 mg/dL
Normal value of blood glucose after meals: <140 mg/dL
Normal value of glycosylated hematocrit: < < 5.6%
Pre-diabetes blood glucose value range:[19]
Fasting blood glucose value: 100-125 mg/dL
Blood glucose value after meals: 140-199 mg/dL
Glycosylated hematocrit value: 5.7-6.4%
Diabetes diagnosis standard blood glucose value range:
Blood glucose value:≧126 mg/dL
Blood glucose value after meals:≧ 200 mg/dL
Glycosylated hematocrit value:≧ 6.5%
Total diabetes index summary
Blood glucose machine usage procedures for accurate testing of blood glucose
Insert a clean blood collection needle into the pen so that the depth and placement of the needle into the skin may be controlled. Please remove the test strips from the bottle of test strips. Please put the cap back on promptly after using the test strips to avoid moisture entering the bottle and harming the remaining test strips. Follow the device's instructions to operate and activate the blood glucose machine for measurement. It is advised to draw blood from the side of the fingertip rather than directly pricking the fingertip when using a blood collection pen to collect blood. This can lessen discomfort and prevent inadequate blood collection, which can alter test findings.
4. Blood Glucose Machine Operation Procedures and Notes Pertaining to Processes Prior to and Post Testing
Blood glucose testing involves measuring the concentration of glucose in the blood. To test your blood glucose at home or somewhere else, you need simply prepare a compact, portable electronic gadget - a blood glucose machine.
A: Who needs at-home blood glucose testing?
Hypoglycemia and pregnant women may require blood glucose testing; however, diabetes patients are the primary target population. In general, the frequency of blood glucose testing is determined by the kind of diabetes you have and your specific treatment plan; thus, please adhere to your doctor's instructions for the frequency of blood glucose tests based on the type of diabetes you have and your specific treatment plan.
1. Type 1 Diabetes: Physicians may prescribe that type 1 diabetics check their blood glucose four to eight times a day, possibly before meals/snacks, before and after exercise, before bedtime, or at night. If the person becomes ill, has a change of daily habit or is consuming new medication, one must also perform blood glucose testing often.
2. Type 2 Diabetes: If insulin is used to manage Type 2 Diabetes, your doctor may prescribe more than two blood glucose tests each day, often before meals and occasionally before night, depending on the type of diabetes you have and the amount of insulin you require.
3. Regular prenatal examinations and home blood glucose monitoring are essential for pregnant women with diabetes, not only to assist in maintaining stable blood glucose levels that may impair fetal development but also lower the risk of diabetes-related complications.
B. Blood glucose machine operation procedure
1. Operate the blood glucose machine according to the instrument's instructions and turn it on for measurement.
2. When using the blood collection pen to collect blood, it is advised to draw blood from the side of the fingertip rather than directly stabbing the fingertip, which reduces discomfort and prevents inadequate blood collection, which can alter test results.
3. Since the findings of the blood glucose machine are typically only maintained for a few days or weeks, it is advised that users record the time and results of the test after the test in order to determine if their blood glucose is within the required range.
C. Three essential indicators for identifying diabetes mellitus
Normal conditions dictate that the diagnosis of diabetes should be verified by measuring fasting blood glucose and glycated hemoglobin, followed by a glucose tolerance test.
1. Glycosylated hematocrit (HbA1c, A1C)
Whether it is a fasting blood glucose value or an oral glucose tolerance test, only the blood glucose level at the moment of blood collection is represented. For this reason, it is required to do further glycated hematocrit testing in order to determine the long-term average blood glucose level.
The mixture of glucose and hemoglobin in the blood is glycated hemoglobin. Therefore, the fraction of glycated hemoglobin collected in the body will increase according to the glucose concentration and duration of high blood glucose.
2. Fasting blood glucose value
The fasting blood glucose level is the blood glucose level without eating for eight hours. It is also known as the "intravenous fasting plasma glucose level," which is the glucose concentration per 100 grams of plasma in the body.
A typical individual's fasting blood glucose level is below 100 mg/dL; when it surpasses 126 mg/dL, the person is deemed to have diabetes. If the blood glucose level is between 100 and 125 mg/dL, it is regarded to be "Impaired fasting glucose" (IFG), and an oral glucose tolerance test is advised.
Diabetes can be verified if the test result exceeds 200 mg/dL.
3. two-hour postprandial glucose value
Normal two-hour postprandial blood glucose levels are 140 mg/dL or below; however, values above 200 mg/dL indicate diabetes. Between 140 and 200 mg/dL indicates impaired glucose tolerance (IGT).
4. Each year, one out of ten individuals with high postprandial glucose readings will develop diabetes. The risk is much greater for those who are obese, have high blood cholesterol, high blood pressure, or are smokers.
In general, the frequency and periodicity of blood glucose testing depend on a person's diabetes progression, blood glucose status, overall health, and other factors. In addition, blood glucose testing aids in determining how the body reacts to diet, disease, stress, exercise, medicine, and other stimuli. For example, a person can determine the effects of one meal on blood glucose level by perform a pre-meal blood glucose testing and a post-meal blood glucose testing, thereby adjusting one’s dietary habits.
In addition to obtaining an annual blood glucose test, "pre-diabetic" individuals should alter their lifestyle by decreasing 5 to 10 percent of their body weight and exercising at least 150 minutes weekly.[20]
5. Conclusions
The World Health Organization reported in 2016 that 422 million people worldwide have diabetes and that an estimated 1.5 million people died from the consequences of hyperglycemia in 2012 [21], In 2012, more than 80% of deaths from diabetes occurred in low- and middle-income countries [22] In 2013, there were 382 million people with diabetes worldwide, 90% of whom had type 2 diabetes. [23] The proportion of the adult population with diabetes has reached 8.5%, with approximately equal gender representation [24] and is expected to increase to 592 million worldwide by 2035 [25]. During 2012-2013, diabetes was responsible for 15 to 51 million deaths per year, ranking eighth among causes of death [26] In general, having diabetes doubles the risk of death [27]. In 2013, the global cost of diabetes was estimated at US$548 billion [28], with US$245 billion spent in the United States alone in 2012 [29] Other studies have found that Asians (especially East Asians) are more likely to develop diabetes and are highly associated with rice as a staple food. [30]
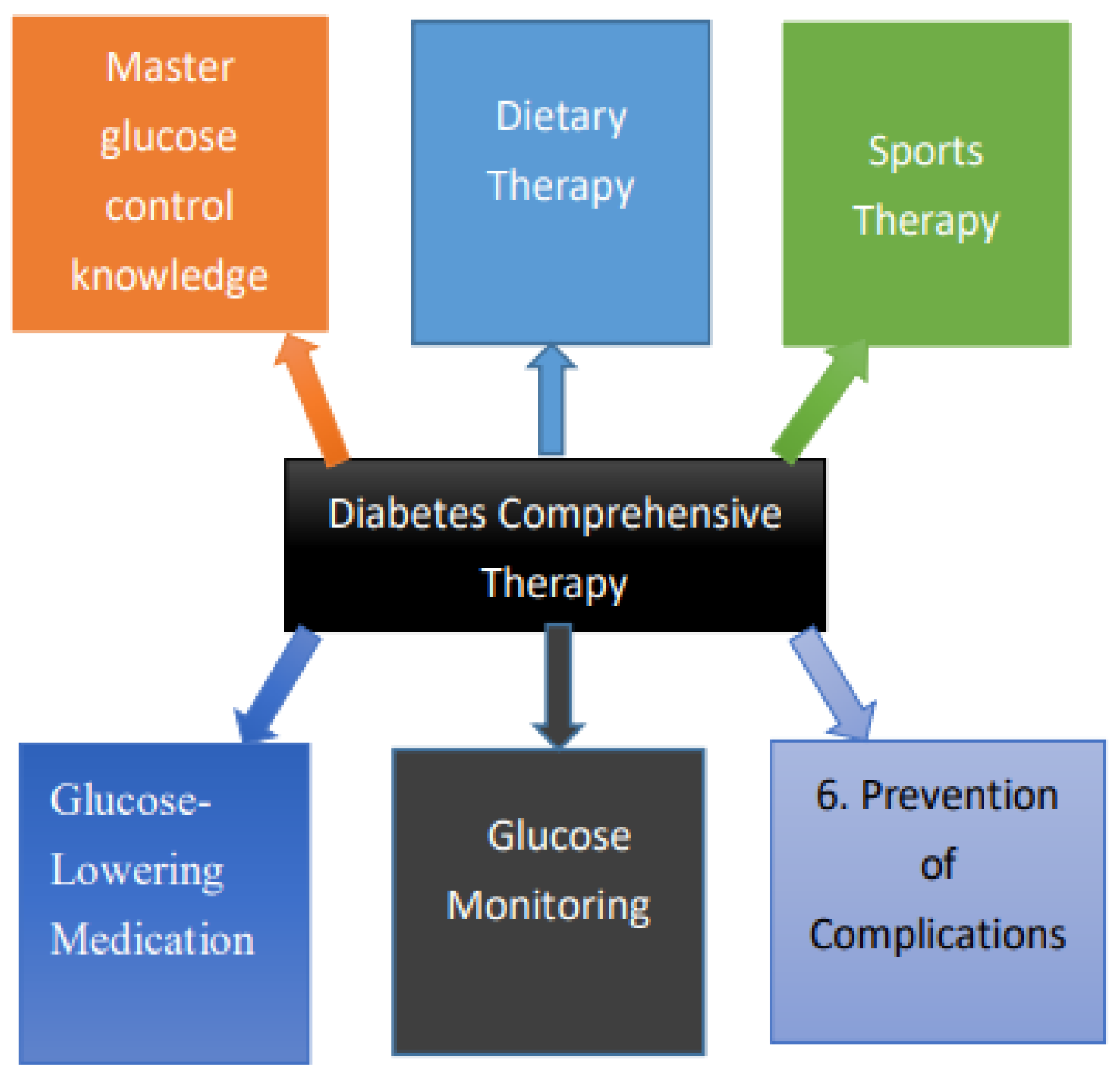
Figure 12.
Diabetes Comprehensive Therapy.
Figure 12.
Diabetes Comprehensive Therapy.
To prevent hypoglycemic symptoms from occurring due to insufficient blood sugar, routine physical exercise is necessary.[31] For diabetic patients, glycosylated hematocrit should be controlled at less than 7%, while maintaining ideal body weight and body fat percentage, which for males aged 18 to 30 years, a normal value ranges from 14% to 20%, and for males aged 30 years or older, a normal value ranges from 17% to 25%, while for females aged 18 to 30, a normal value ranges from 17% to 25%, and for women aged 30 and above, a normal value ranges from 20% to 30%. As for waist circumference, for males, a normal value of less than 90 cm should be maintained, while for females, a normal value of less than 80 cm should be maintained. In addition, stress may result in abnormal secretion of hormones, resulting in the breakdown of liver sugar into blood sugar and increasing the risk of developing diabetes. Therefore, it is essential to alleviate stress in a balanced and timely manner. Starting with lifestyle adjustments, a good option is physical activity, which enables more accurate blood glucose measurements.
For diabetic patients, steady blood sugar management is the primary health care objective. To prevent excessive variations in blood sugar, it is required to limit the incidence of abrupt changes in blood sugar and hypoglycemia after meals; hence, monitoring blood sugar after meals is even more crucial for diabetes patients than monitoring fasting blood sugar. To avoid the progression of diabetes, it is essential to comprehend the numerous diabetes indices that may help us determine the level of diabetes control within our family. During the procedure, we are able to witness the fluctuations and long-term changes in blood glucose levels, and we cannot help but worry about the status of diabetic patients. In addition to worrying and nagging, we should spend more time and care for the patient's health, remind the patient in a timely manner, record the blood glucose level and the information of each meal on a regular basis, accompany the patient to exercise together to control the blood glucose level, prepare appropriate diets and nutritional supplements for the patient's family, and provide practical assistance to the patio
Diabetes prevention and treatment involve maintaining a balanced diet, regular exercise, quitting smoking, and maintaining an ideal weight. Blood pressure control and foot care are also crucial for diabetes patients. Type 1 diabetes requires insulin injections to manage blood glucose, while type 2 diabetes can be managed with oral medications, sometimes combined with insulin if necessary. Some oral diabetes medications and insulin may cause hypoglycemia. For obese type 2 diabetes patients, bariatric surgery is an effective treatment. In cases of gestational diabetes, blood glucose usually returns to normal after childbirth.
World Health Organization diagnostic criteria for diabetes:
Postprandial glucose (2h), fasting plasma glucose,[32]
HbA1c, mmol/l (mg/dl), mmol/l (mg/dl) %
Normal <7.8 (<140) <6.1 (<110) <6.0
Impaired fasting glucose <7.8 (<140) ≥6.1 (≥110) & <7.0 (<126) 6.0–6.4
Impaired glucose tolerance ≥7.8 (≥140) <7.0 (<126) 6.0–6.4
Diabetes ≥11.1 (≥200) ≥7.0 (≥126) ≥6.5
Glucose metabolism classification (WHO 1999):
Classification Venous plasma glucose (mmol/L)
Fasting glucose (FPG) Post-glucose load (2hPPG)
Normal glucose regulation <6.1 <7.8
Impaired fasting glucose 6.1–<7.0 <7.8
Impaired glucose tolerance <7.0 7.8–<11.1
Diabetes ≥7.0 ≥11.1
Comprehensive treatment principles include lifestyle modifications, such as dietary control, physical exercise, weight reduction, smoking cessation, and avoiding secondhand smoke, along with medication management to control blood glucose and prevent complications. Currently, there is no cure for diabetes. According to data released by the International Diabetes Federation (IDF) in 2009, there are approximately 30 million type 1 diabetes patients worldwide. While type 1 diabetes cannot be cured, scientific and rational management can enable most patients to lead normal lives with the same quality of life and life expectancy as others. Comprehensive diabetes prevention and management require patient education, lifestyle changes, and mental health adjustments, with dietary, exercise, and pharmacological treatments as the main therapeutic strategies. The cooperation of patients and their families is essential to achieving satisfactory outcomes. Latent autoimmune diabetes in adults (LADA) is diagnosed as type 1 diabetes in adulthood. [33]
References
- Diabetes Blue Circle Symbol. International Diabetes Federation. April 2016.
- Diabetes Blue Circle Symbol. International Diabetes Federation. 17 March 2006.
- IDF Diabetes Atlas(29-79Years 2021). Available online: https://diabetesatlas.org/living-with-diabetes/.
- 2024 ICD-10-CM Diagnosis Code E10.9 Type 1 diabetes mellitus without complications.
- E10.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. -type 1 diabetes estimates In children and adults. Available online: https://diabetesatlas.org/atlas-reports/.
- Cardiovascular risk reduction in type 2 diabetes. Available online: https://www.ahajournals.org/doi/10.1161/CIR.0000000000001040.
- The fluctuation of blood sugar (red) and the sugar-lowering hormone insulin (blue) in humans during the course of a day with three meals. One of the effects of a sugar-rich vs a starch-rich meal is highlighted. Available online: https://en.wikipedia.org/wiki/Blood_sugar_level.
- 2017 Journal of Clinical and Scientific Research | Published by Wolters Kluwer – Medknow. Available online: https://journals.lww.com/jcsr/abstract/2017.
- Diabetes Fact sheet N°312. WHO. October 2013 [25 March 2014].
- Triparty, B.B.; Chanda, H.B. RSSDI Textbook of Diabetes Mellitus; Medical Ltd.: JP, 2012. [Google Scholar]
- Ripsin, C.M.; Kang, H.; Urban, R.J. Management of blood glucose in type 2 diabetes mellitus. American Family Physician 2021. [Google Scholar] [PubMed]
- About diabetes. World Health Organization. [4 April 2014].
- Type 2 diabetes Symptoms and Causes. Available online: https://my.clevelandclinic.org/health/diseases/21501-type-2-diabetes.
- Alzheimer’s is sometimes referred to as type 3 diabetes. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC7246646/.
- Irwin, R.S.; Ripple, J.M. Manual of Intensive Care Medicine; Lippincott Williams & Wilkins, 2010; ISBN 978-0-7817-9992-8. [Google Scholar]
- Picot, J.; Jones, J.; Colquitt, J.L.; Gospodarevskaya, E.; Loveman, E.; Baxter, L.; Clegg, A.J. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health technology assessment 2009, 13, 1–190. [Google Scholar] [CrossRef] [PubMed]
- Cash, J. Family Practice Guidelines 3; Springer Publishing Company, 2014; ISBN 9780826168757. [Google Scholar]
- What is the blood glucose level at which pre-diabetes or diabetes will be diagnosed? Available online: https://www.cdc.gov/diabetes/diabetes-testing/prediabetes-a1c-test.html.
- Pre-diabetes blood glucose value range. Available online: https://www.mayoclinic.org/zh-hans/diseases-conditions/prediabetes/diagnosis-treatment/drc-20355284.
- In people with normal glucose tolerance, testing should be repeated once every 3 years... weight loss in a pre-diabetic population. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC6125024/.
- The World Health Organization reported in 2016. Available online: https://www.who.int/docs/default-source/gho-documents/world-health-statistic-reports/world-heatlth-statistics-2016.pdf.
- In 2012, diabetes was the direct cause of 1.5 million deaths, with more than 80% of these deaths occurring in low- and middle-income countries. WHO projects that diabetes will be the 7th leading cause of death by 2030. Available online: https://www.emro.who.int/right-teasers/diabetes-info/what-are-the-consequences-of-diabetes.html.
- In 2013, there were 382 million people with diabetes worldwide, 90% of whom had type 2 diabetes. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC8369920/.
- The proportion of the adult population with diabetes has reached 8.5%, with approximately equal gender representation. Available online: https://iris.who.int/bitstream/handle/10665/204871/9789241565257_eng.pdf;jsessionid=5D780F85E193607683D29C605195BF7C?sequence=1.
- Worldwide, there is a projected increase in the prevalence of diabetes from 382 million (8.3%) in 2013 to 592 million (10.1%) in 2035. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC4282306/.
- During 2012-2013, diabetes was responsible for 15 to 51 million deaths per year, ranking eighth among causes of death. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC6768526/.
- In general, having diabetes doubles the risk of death. Available online: https://pubmed.ncbi.nlm.nih.gov/31722562/.
- In 2013, the global cost of diabetes was estimated at US$548 billion. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC5321382/.
- In 2013, the global cost of diabetes was estimated at US$548 billion, with US$245 billion spent in the United States alone in 2012. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC5321382/.
- Other studies have found that Asians (especially East Asians) are more likely to develop diabetes and are highly associated with rice as a staple food. Available online: https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/rice-and-noodle-consumption-is-associated-with-insulin-resistance-and-hyperglycaemia-in-an-asian-population/93A2A632C36844841ECF1511F1353421.
- To prevent hypoglycemic symptoms from occurring due to insufficient blood sugar, routine physical exercise is necessary. Available online: https://www.medicalnewstoday.com/articles/exercise-induced-hypoglycemia-what-to-know.
- World Health Organization diagnostic criteria Postprandial glucose (2h), fasting plasma glucose. Available online: https://www.ncbi.nlm.nih.gov/books/NBK532915/.
- The cooperation of patients and their families is essential to achieving satisfactory outcomes. Latent autoimmune diabetes in adults (LADA) is diagnosed as type 1 diabetes in adulthood. Available online: https://www.tsim.org.tw/ehc-tsim/s/viewFile?documentId=306c5aa22a894abb82e8268f6dc37981.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).