Submitted:
24 February 2025
Posted:
25 February 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
3. Results
3.1. Four LB Studies on Stroke Patients
3.2. Other LB Studies on Neurological Diseases—4 Articles
4. Discussion
5. Conclusion
Abbreviations
| LB | Lee Silverman Voice Treatment-BIG |
| LSVT | Lee Silverman Voice Treatment |
| TBI | Traumatic Brain Injury |
| VR | Virtual Reality |
| ADL | Activities of Daily Living |
| QOL | Quality Of Life |
| POQ | Performance Of Quality |
| OT | Occupational Therapist |
| MAS | Modified Ashworth Scale |
| WMFT | Wolf Motor Function Test |
| COPM | Canadian Occupational Performance Measure |
| PASS | Performance Assessment of Self-Care Skills |
| SS-QOL | Stroke-Specific Quality of Life scale |
| CAHAI-13 | Chedoke Arm and Hand Activity Inventory-13 |
| REACH | Rating of Everyday Arm-use in the Community and Home |
| PQRS-OD | Performance Quality Rating Scale-Operational Definition |
| MFT | Manual Function Test |
| BBS | Berg Balance Scale |
| FRT | Functional Reaching Test |
| TUG | Time Up and GO |
| PROMIS-43 | Patient-Reported Outcomes Measurement Information System-43 |
| DE | Daily Exercise |
| FCM | Functional Component Movements |
| HT | Hierarchy Tasks |
| BW | BIG Walking |
| HP | Homework Practice |
| PTP | Person to Person |
| PT | Physical Therapist |
| PSP | Progressive Supranuclear Palsy |
| INPH | Idiopathic Normal Pressure Hydrocephalus |
| FGA | Functional Gait Assessment |
| 6MWT | 6 Minute Walk Test |
| 5TSTS | 5 Time Sit to Stand |
| ABC | Activities-Specific Balance and Confidence |
| PSPRS | Progressive Supranuclear Palsy Rating Scale |
| UPDRS: | Unified Parkinson’s Disease Rating Scale |
| 10MWT | 10 Meter Walk Test |
References
- Borsook, D. Neurological diseases and pain. Brain 2012, 135, 320–344. [Google Scholar] [CrossRef] [PubMed]
- Collaborators, G.U.N.D. Burden of Neurological Disorders Across the US From 1990-2017: A Global Burden of Disease Study. JAMA Neurology 2021, 78, 165–176. [Google Scholar] [CrossRef]
- Jensen M, C.A. , Chaudhry N, Ng M, Sule D, Duncan W, Ray P, Weinstock-Guttman B, Smith B, Ruttenberg A, Szigeti K, Diehl AD. The neurological disease ontology. The neurological disease ontology. J Biomed Semantics 2013, 4, 1–10. [Google Scholar] [CrossRef]
- Gooch, C.L.; Pracht, E.; Borenstein, A.R. The burden of neurological disease in the United States: A summary report and call to action. Annals of neurology 2017, 81, 479–484. [Google Scholar] [CrossRef]
- Kossi, O.; Raats, J.; Wellens, J.; Duckaert, M.; De Baets, S.; Van de Velde, D.; Feys, P. Efficacy of rehabilitation interventions evaluated in common neurological conditions in improving participation outcomes: A systematic review. Clinical Rehabilitation 2024, 38, 47–59. [Google Scholar] [CrossRef]
- Chan, D.Y.; Chan, C.C.; Au, D.K. Motor relearning programme for stroke patients: a randomized controlled trial. Clinical rehabilitation 2006, 20, 191–200. [Google Scholar] [CrossRef]
- Hornby, T.G.; Campbell, D.D.; Kahn, J.H.; Demott, T.; Moore, J.L.; Roth, H.R. Enhanced gait-related improvements after therapist-versus robotic-assisted locomotor training in subjects with chronic stroke: a randomized controlled study. Stroke 2008, 39, 1786–1792. [Google Scholar] [CrossRef]
- Hassett, L.M.; Moseley, A.M.; Tate, R.L.; Harmer, A.R.; Fairbairn, T.J.; Leung, J. Efficacy of a fitness centre-based exercise programme compared with a home-based exercise programme in traumatic brain injury: a randomized controlled trial. Journal of rehabilitation medicine 2009, 41, 247–255. [Google Scholar] [CrossRef]
- Combs-Miller, S.A.; Kalpathi Parameswaran, A.; Colburn, D.; Ertel, T.; Harmeyer, A.; Tucker, L.; Schmid, A.A. Body weight-supported treadmill training vs. overground walking training for persons with chronic stroke: a pilot randomized controlled trial. Clinical rehabilitation 2014, 28, 873–884. [Google Scholar] [CrossRef]
- Heine, M.; Verschuren, O.; Hoogervorst, E.L.; van Munster, E.; Hacking, H.G.; Visser-Meily, A.; Twisk, J.W.; Beckerman, H.; de Groot, V.; Kwakkel, G. Does aerobic training alleviate fatigue and improve societal participation in patients with multiple sclerosis? A randomized controlled trial. Multiple Sclerosis Journal 2017, 23, 1517–1526. [Google Scholar] [CrossRef]
- Lewthwaite, R.; Winstein, C.J.; Lane, C.J.; Blanton, S.; Wagenheim, B.R.; Nelsen, M.A.; Dromerick, A.W.; Wolf, S.L. Accelerating stroke recovery: body structures and functions, activities, participation, and quality of life outcomes from a large rehabilitation trial. Neurorehabilitation and Neural Repair 2018, 32, 150–165. [Google Scholar] [CrossRef] [PubMed]
- de Rooij, I.J.; van de Port, I.G.; Punt, M.; Abbink-van Moorsel, P.J.; Kortsmit, M.; van Eijk, R.P.; Visser-Meily, J.M.; Meijer, J.-W.G. Effect of virtual reality gait training on participation in survivors of subacute stroke: a randomized controlled trial. Physical therapy 2021, 101, pzab051. [Google Scholar] [CrossRef] [PubMed]
- Flood, M.W.; O’Callaghan, B.P.; Diamond, P.; Liegey, J.; Hughes, G.; Lowery, M.M. Quantitative clinical assessment of motor function during and following LSVT-BIG® therapy. Journal of NeuroEngineering and Rehabilitation 2020, 17, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Sapir, S.; Ramig, L.O.; Fox, C.M. Intensive voice treatment in Parkinson’s disease: Lee Silverman voice treatment. Expert Review of Neurotherapeutics 2011, 11, 815–830. [Google Scholar] [CrossRef]
- Fox, C.; Ebersbach, G.; Ramig, L.; Sapir, S. LSVT LOUD and LSVT BIG: behavioral treatment programs for speech and body movement in Parkinson disease. Parkinson’s disease 2012, 2012, 391946. [Google Scholar] [CrossRef]
- Iwai, M.; Koyama, S.; Takeda, K.; Hirakawa, Y.; Motoya, I.; Kumazawa, N.; Sakurai, H.; Kanada, Y.; Kawamura, N.; Kawamura, M. Effect of LSVT® BIG on standing balance in a Parkinson's patient: A case report. Physiotherapy Research International 2021, 26, e1921. [Google Scholar] [CrossRef]
- Millage, B.; Vesey, E.; Finkelstein, M.; Anheluk, M. Effect on gait speed, balance, motor symptom rating, and quality of life in those with stage I Parkinson’s disease utilizing LSVT BIG®. Rehabilitation research and practice 2017, 2017, 9871070. [Google Scholar] [CrossRef]
- Isaacson, S.; O’Brien, A.; Lazaro, J.D.; Ray, A.; Fluet, G. The JFK BIG study: the impact of LSVT BIG® on dual task walking and mobility in persons with Parkinson’s disease. Journal of physical therapy science 2018, 30, 636–641. [Google Scholar] [CrossRef]
- Choi, Y.; Kim, D. Effects of Task-Based LSVT-BIG Intervention on Hand Function, Activity of Daily Living, Psychological Function, and Quality of Life in Parkinson’s Disease: A Randomized Control Trial. Occupational therapy international 2022, 2022, 1700306. [Google Scholar] [CrossRef]
- McDonnell, M.N.; Rischbieth, B.; Schammer, T.T.; Seaforth, C.; Shaw, A.J.; Phillips, A.C. Lee Silverman Voice Treatment (LSVT)-BIG to improve motor function in people with Parkinson’s disease: a systematic review and meta-analysis. Clinical rehabilitation 2018, 32, 607–618. [Google Scholar] [CrossRef]
- Hochstedler, R. The Application of Lee Silverman Voice Treatment (LSVT)–BIG with a Patient Diagnosed with Parkinson’s Disease: A Case Study and Literature Review. 2019. [Google Scholar]
- Jeong, S.-A.; Hong, D.-G. Research Trends of LSVT-BIG Interventions for Patients with Parkinson’s Disease : Scoping Review. The Journal of Korean Society of Community-Based Occupational Therapy 2022, 12, 59–73. [Google Scholar] [CrossRef]
- Proffitt, R.M.; Henderson, W.; Scholl, S.; Nettleton, M. Lee silverman voice treatment BIG® for a person with stroke. The American Journal of Occupational Therapy 2018, 72, 7205210010p7205210011–7205210010p7205210016. [Google Scholar] [CrossRef] [PubMed]
- Metcalfe, V.; Egan, M.; Sauvé-Schenk, K. LSVT BIG in late stroke rehabilitation: A single-case experimental design study. Canadian Journal of Occupational Therapy 2019, 86, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.-A.; Hong, D.-G. A case study on the clinical application of lee silverman voice treatment-big (LSVT-BIG) program for occupational performance and motor functions of stroke patients. Therapeutic Science for Rehabilitation 2020, 9, 63–75. [Google Scholar] [CrossRef]
- Proffitt, R.; Henderson, W.; Stupps, M.; Binder, L.; Irlmeier, B.; Knapp, E. Feasibility of the Lee Silverman voice treatment-BIG intervention in stroke. OTJR: Occupation, Participation and Health 2021, 41, 40–46. [Google Scholar] [CrossRef]
- Brown, E. Modified LSVT BIG Treatment for a Patient with Progressive Supranuclear Palsy: A Case Report. University of Iowa, 2019.
- Fillmore, S.; Cavalier, G.; Franke, H.; Hajec, M.; Thomas, A.; Moriello, G. Outcomes following LSVT BIG in a person with idiopathic normal pressure hydrocephalus: A case report. Journal of Neurologic Physical Therapy 2020, 44, 220–227. [Google Scholar] [CrossRef]
- Hoyman, J. LSVT BIG Exercises as Treatment for a Patient with Huntington’s Disease: A Case Report. University of Iowa, 2022.
- Hirakawa, Y.; Takeda, K.; Koyama, S.; Iwai, M.; Motoya, I.; Sakurai, H.; Kanada, Y.; Kawamura, N.; Kawamura, M.; Tanabe, S. Effect of the Lee Silverman Voice Treatment BIG® on motor symptoms in a participant with progressive supranuclear palsy: A case report. Physiotherapy Theory and Practice 2024, 40, 2171–2178. [Google Scholar] [CrossRef]
- Henderson, W.; Boone, A.E.; Heady, J.; Nettleton, M.; Wilhelm, T.; Bliss, J. Use of occupation-based measures in LSVT BIG research: A case study. OTJR: Occupation, Participation and Health 2020, 40, 131–137. [Google Scholar] [CrossRef]
- Sosner, J.; Wall, G.C.; Sznajder, J. Progressive supranuclear palsy: clinical presentation and rehabilitation of two patients. Archives of physical medicine and rehabilitation 1993, 74, 537–539. [Google Scholar] [CrossRef]
- Tilley, E. The effectiveness of allied health therapy in the symptomatic management of progressive supranuclear palsy: a systematic review protocol. 2014. [Google Scholar] [CrossRef]
- Quinn, L.; Kegelmeyer, D.; Kloos, A.; Rao, A.K.; Busse, M.; Fritz, N.E. Clinical recommendations to guide physical therapy practice for Huntington disease. Neurology 2020, 94, 217–228. [Google Scholar] [CrossRef]
- Stolze, H.; Kuhtz-Buschbeck, J.P.; Drücke, H.; Jöhnk, K.; Illert, M.; Deuschl, G. Comparative analysis of the gait disorder of normal pressure hydrocephalus and Parkinson's disease. Journal of Neurology, Neurosurgery & Psychiatry 2001, 70, 289–297. [Google Scholar] [CrossRef]
- Fishel, S.C.; Hotchkiss, M.E.; Brown, S.A. The impact of LSVT BIG therapy on postural control for individuals with Parkinson disease: A case series. Physiotherapy Theory and Practice 2020, 36, 834–843. [Google Scholar] [CrossRef] [PubMed]
| Session (time) |
Session contents | Details |
|---|---|---|
| 1st half (30 min or more) |
Daily Exercise | 1. Floor to ceiling(seated)- 8 repetitions (10 second hold) |
| 2. Side to side(seated)- 8 repetitions (10 second hold) | ||
| 3. Forward step and reach(standing)-8 repetitions each leg | ||
| 4. Sideways step and reach(standing)-8 repetitions each side | ||
| 5. Backward step and reach(standing)-8 repetitions each leg | ||
| 6. Forward rock and reach(standing)-10 repetitions each leg | ||
| 7. Sideways rock and reach(standing)-10 repetitions each side | ||
| Functional Component movements | 5 everyday tasks that the subject wants to perform more successfully – 5 repetition each |
|
| 2nd half (30min. or less) |
Hierarchy Tasks | Activities that are divided into stages for more difficult movements targeting the movements that have been resolved among daily life or functional component movements |
| BIG Walking | Walking during various distances and time limits with large strides | |
| Homework practice | Treatment day: one time for 5-10 minutes Nontreatment day: two time for 10-15 minutes |
|
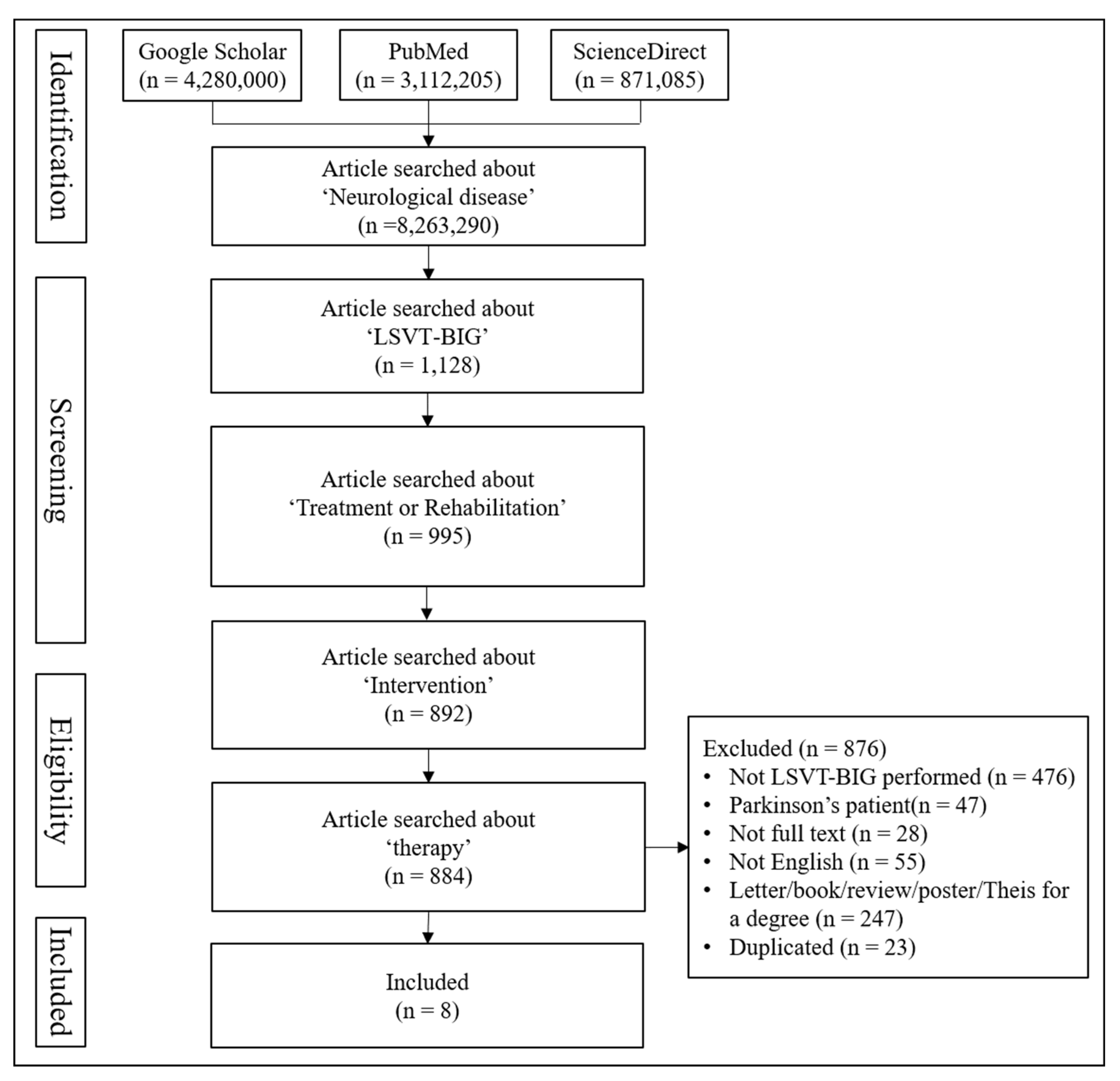
| Electronic databases | Google Scholar, PubMed, ScienceDirect |
|---|---|
| Search keyword | Neurological disease, LSVT-BIG, Treatment or Rehabilitation, Intervention, Therapy |
| Criteria for inclusion | Written in English; Performed LSVT-BIG; Available in Full text; Published in journals |
| Authors (year) |
Licenses of Trainer | Design/Subject (in/out patient) |
Diagnosis | Evaluation | |||||||||
| Spasticity | Upper function | Upper-extremity use rate | Occupational function | Balance | Gait | ADL | QOL | POQ | Health condition | ||||
| Proffitt et al (2018) | OT | Case study/N=1(out) | Ischemic stroke | MAS | WMFT | COPM | PASS | SS-QOL | |||||
| Metcalfe et al (2019) | OT | single subject design/N=2(out) | A: Rt. Side ischemic stroke B: Stroke |
CAHAI-13 | REACH | COPM | PQRS-OD | ||||||
| Jung& Hong (2020) | OT | Case study/N=2(in) | A: Infarction B: Hemorrhage |
MFT | COPM, | BBS, FRT | TUG | ||||||
| Proffitt et al (2021) | OT | Waitlist cross-over design/N=5(out) | Stroke | WMFT | COPM | PASS | PROMISE-43 | ||||||
| Authors (year) |
Intervention | Result | Limitation | ||||
| DE | FCM | HT | BW | HP | |||
| Proffitt et al (2018) | O | O | O | O | O | Improvement in all tests | 1. Small sample size 2. Only 50% of the planned homework practice was performed. 3. The items of the 5 tasks in the PASS results are not mentioned. 4. The intensity of the LB intervention is not mentioned. 5. It is impossible to identify which component of the LB contributed most to the functional improvement. |
| PTP type, 1-hr session/day, consecutive 4 days/week for 4 weeks | 1-hr session/day (treatment on days), 2-hr session/day (nontreatment on days) for 4 weeks |
||||||
| Metcalfe et al (2019) | O | O | O | X | O | REACH: Maintained PQRS-OD: Improvement in some items COPM: Improvement CAHAI-13: No significant difference |
1. Small sample size and no mention of premorbid dominant hand 2. It is impossible to identify which component of the intervention contributed to the improvement of occupational performance. 3. For the LB protocol, BIG Walking, only 4 times a week is mentioned, and there is no mention of consecutive 4 times a week as mentioned in the protocol. 4. No clear description on homework practice and intervention intensity 5. Occupational performance evaluation was conducted only through the subjective assessment COPM |
| PTP type, 1-hr session/day, 4 days/week for 4 weeks | Not mentioned in detail | ||||||
| Jung& Hong (2020) | O | O | O | O | X | Improvement in MFT, FRT, BBS, TUG, COPM | 1. Small sample size 2. No mention of the subjects’ premorbid dominant hand 3. Lack of prior mention of the degree of recovery of stroke patients to whom LB can be applied, resulting in differences in functional recovery for each subject 4. In performing LB, only 4 times a week was mentioned, making it unclear whether it would be implemented consecutive 4 times a week as mentioned in the protocol 5. No homework practice 6. It is difficult to determine the effect of LB alone since other rehabilitation therapies were performed simultaneously with LB application. 7. It is impossible to identify which component of the LB contributed most to the functional improvement. 8. There is a difference in the number of stroke occurrences and the frequency of rehabilitation therapy other than LB in only two subjects. |
| PTP type, 1-hr session/day, 4 days/week for 4 weeks The intensity of the intervention was 80% of the maximum exercise volume for each subject. |
|||||||
| Proffitt et al (2021) | O | O | O | X | O | Improvement in all tests | 1. Small sample size 2. There is no pre/post comparison of MAS, and BIG Walking is excluded from the basic structure. 3. No left-right distinction of improved results of the subject in WMFT 4. It is impossible to identify which component of the LB contributed most to the functional improvement. 5. Not all 16 sessions could be performed due to accessibility issues of the intervention site. |
| PTP type, 1-hr session/day, consecutive 4days/week for 4weeks The intensity of the intervention was a score of 7 or higher on a 10-point self-report scale. |
20-40 min session/day for 4 weeks (once on treatment days and twice on nontreatment days | ||||||
|
Authors (year) |
Licenses of Trainer |
Design/Subject (in/out patient) |
Diagnosis | Evaluation | |||||
| Muscle strength | Balance | motor | Gait | coordination | Follow-Up Questions | ||||
| Brown (2019) |
PT | Case report/N=1(out) | PSP | 5TSTS | BBS | FGA 6MWT |
|||
| Fillmore (2020) |
PT | Case report/N=1(out) | INPH | 5TSTS | BBS ABC |
Getting off the floor | TUG TUG- cognition TUG- manual |
Follow-Up Questions | |
| Hoyman (2022) |
PT | Case report/N=1(out) | Huntington’s Disease | TUG gait assessment karaoke stepping |
coordination | ||||
| Hirakawa (2023) |
PT | Case report/N=1(out) | PSP | BBS | PSPRS-limb PSPRS-gait UPDRS Part3 |
10MWT | Follow-Up Questions | ||
| Authors (year) |
Intervention | Result | Limitation | ||||
| DE | FCM | HT | BW | HP | |||
| Brown (2019) |
O | O | O | O | O | FGA: Improvement BBS, 6MWT, 5TSTS: Deterioration |
1. Small sample size 2. It is clinically difficult to provide effective interventions to patients with progressive diseases such as PSP and improve the scores 3. It is difficult to judge the intervention effect when the patient’s function is deteriorating to the extent that it is impossible to respond to treatment intervention due to the progression of the disease. 4. The treatment was only performed three times a week, and it is impossible to know whether it was performed consecutively. |
| PTP type, 1-hr session/day, 3days/week for 3weeks The intensity of the intervention was 75~85% of the subject’s maximum exercise volume. |
1-hr session/day, 3~4days/week for 3weeks | ||||||
| Fillmore (2020) |
O | O | O | O | ABC, BBS: Improvement TUG, TUG cognitive & manual, 5TSTS test, Getting off the floor: No difference Subjective assessment: Improvement |
1. There is a limitation in generalizing the observation results since it was conducted for only one participant. 2. It is difficult to directly link the improvement in the result to the LB intervention and its effect since there is no previous physical therapy experience. 3. There is a limitation in interpreting the intervention results only with the MDC results. 4. The program could not be performed for a sufficiently long period due to the subject’s cognitive impairment. 5. The LB program needs to be operated according to the cognitive status and learning ability of each patient. 6. The intervention was only performed on consecutive 3 days a week, and no participation was made twice during the entire schedule. 7. There is no objective mention of the intensity of the intervention (standardized maximum daily exercise volume) |
|
| PTP type, 1.5-hr session/day, consecutive 3days/week for 4weeks | 1.5-hr 2sessions/day 3days/week for 4weeks | ||||||
| Hoyman (2022) |
O | O | O | O | O | TUG: Improvement Gait assessment, karaoke stepping: Improvement in some items Coordination: Improvement |
1. Small sample size 2. A home exercise program was implemented from the third week. 3. Initially, treatment was performed 3 times a week, but the number of treatments was reduced to 1 time a week after symptom improvement. 4. Since most physical therapy interventions were performed together with LB exercise, it is difficult to compare LB exercise with other physical therapy interventions performed for Huntington’s disease. 5. LB intervention was performed on the subject in the intermediate stage of Huntington’s disease symptoms. 6. No specific mention of intervention intensity 7. After administering antipsychotic medication at the third week, all outcome measures showed functional improvement but stagnated thereafter, so the contribution of the medication can be considered. |
| PTP type, 45-min session/day, 1~3days/week for 8weeks | Home exercise from the third week 5 days/week for 6weeks |
||||||
| Hirakawa (2023) |
O | O | O | O | O | Improvement in all tests | 1. The results cannot be generalized due to the small sample size. 2. Since PSP gait abnormalities vary from patient to patient, additional research is needed to examine the generalizability of LB to various PSP patients. 3. It is difficult to identify what made the effect as medications were administered before implementation of LB. |
| PTP type, 1-hr session/day, consecutive 4days/week for 4weeks The intensity of the intervention was 70-80% of the subject’s maximum exercise volume. |
(1-hr session/day, 5days/week for 4 weeks | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





