Submitted:
21 January 2025
Posted:
22 January 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
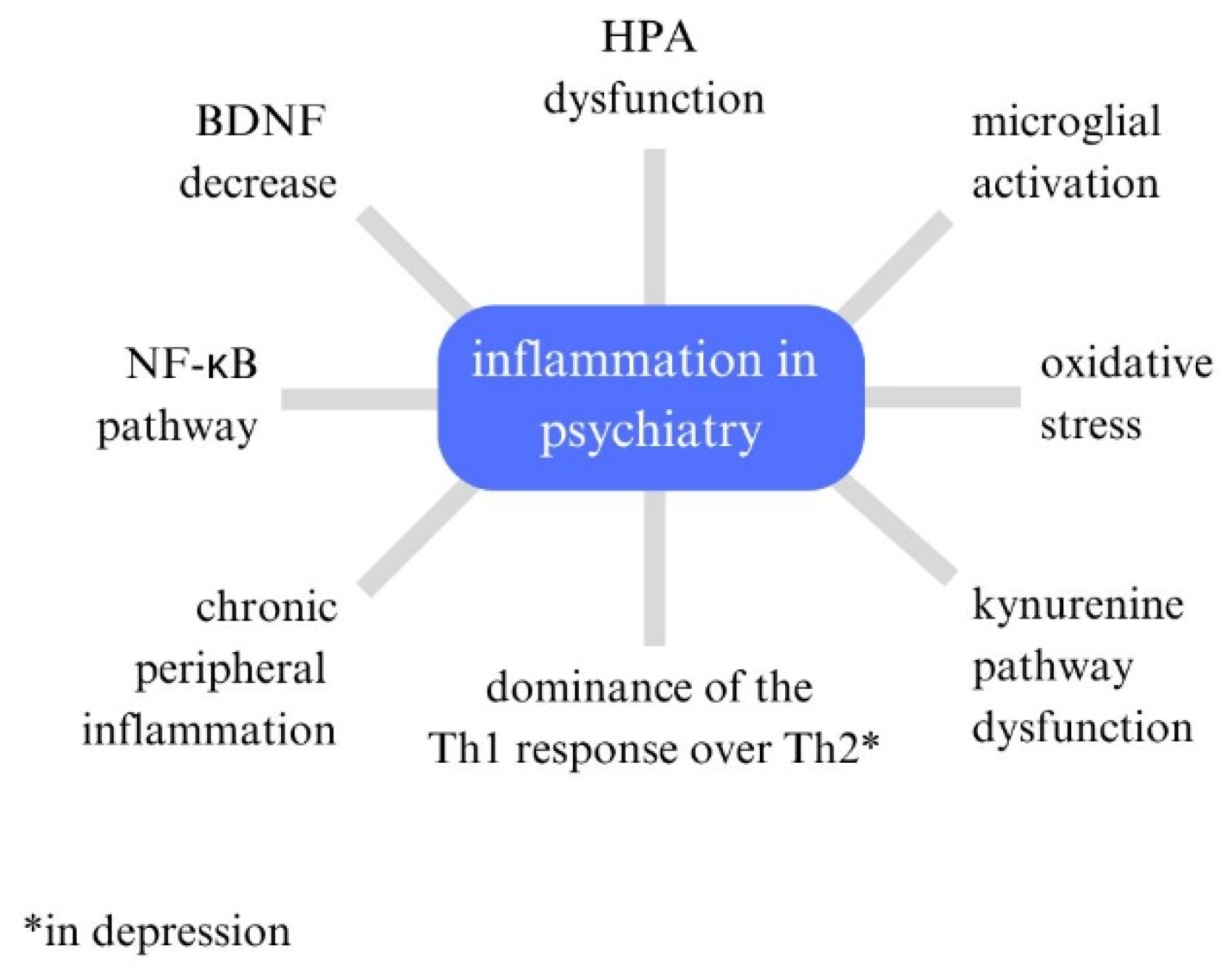
3. Immunological Mechanisms Linked to Seasonality: Inflammatory Markers in Mental Disorders
3.1. Background
3.2. Depression
3.3. Schizophrenia
3.4. Bipolar Disorder
3.5. Generalized Anxiety Disorder (GAD)
3.6. PTSD
3.7. ASD
4. Immunological Mechanisms Linked to Seasonality: A Pathway Between Weather and Immune System
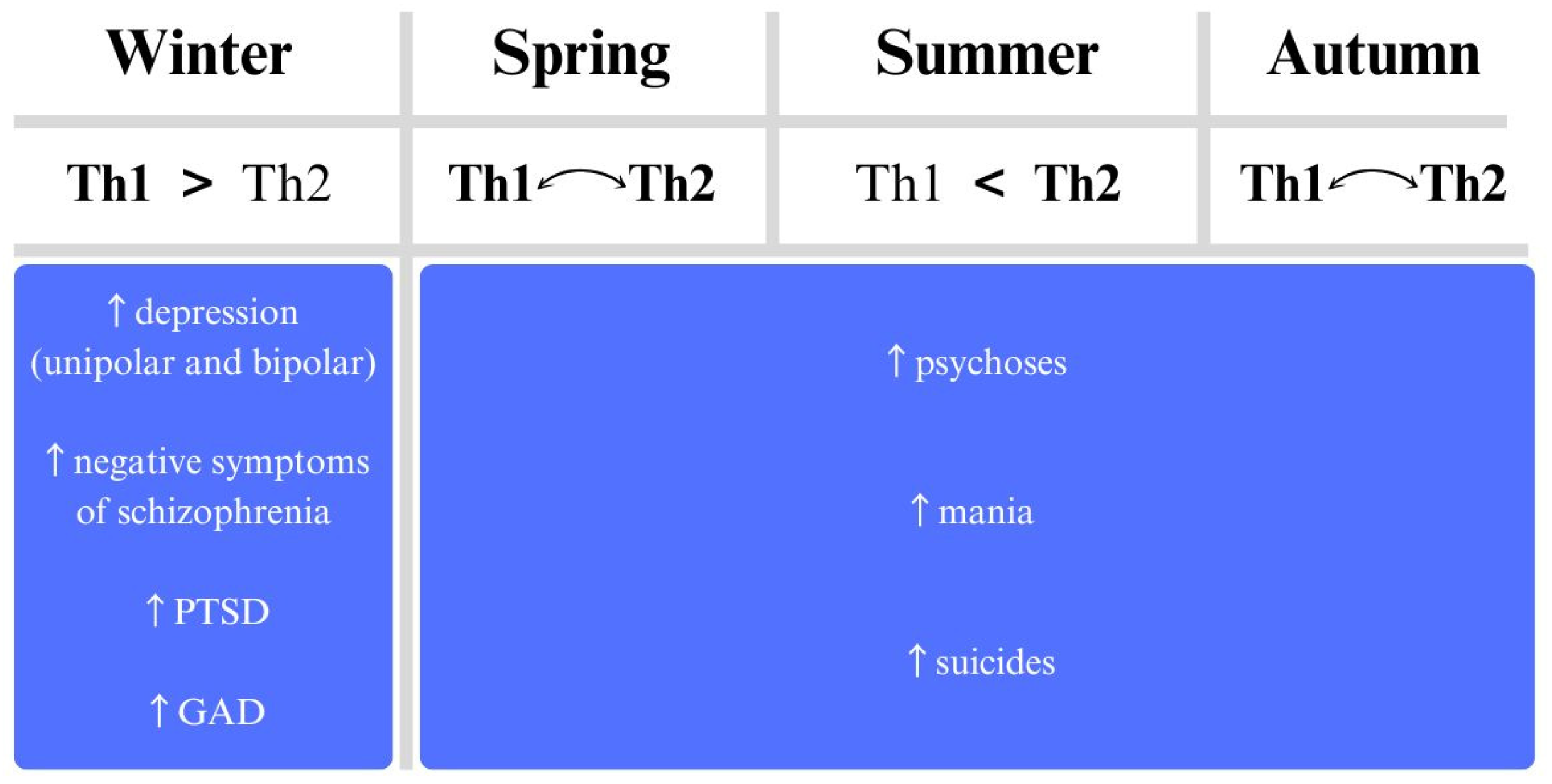
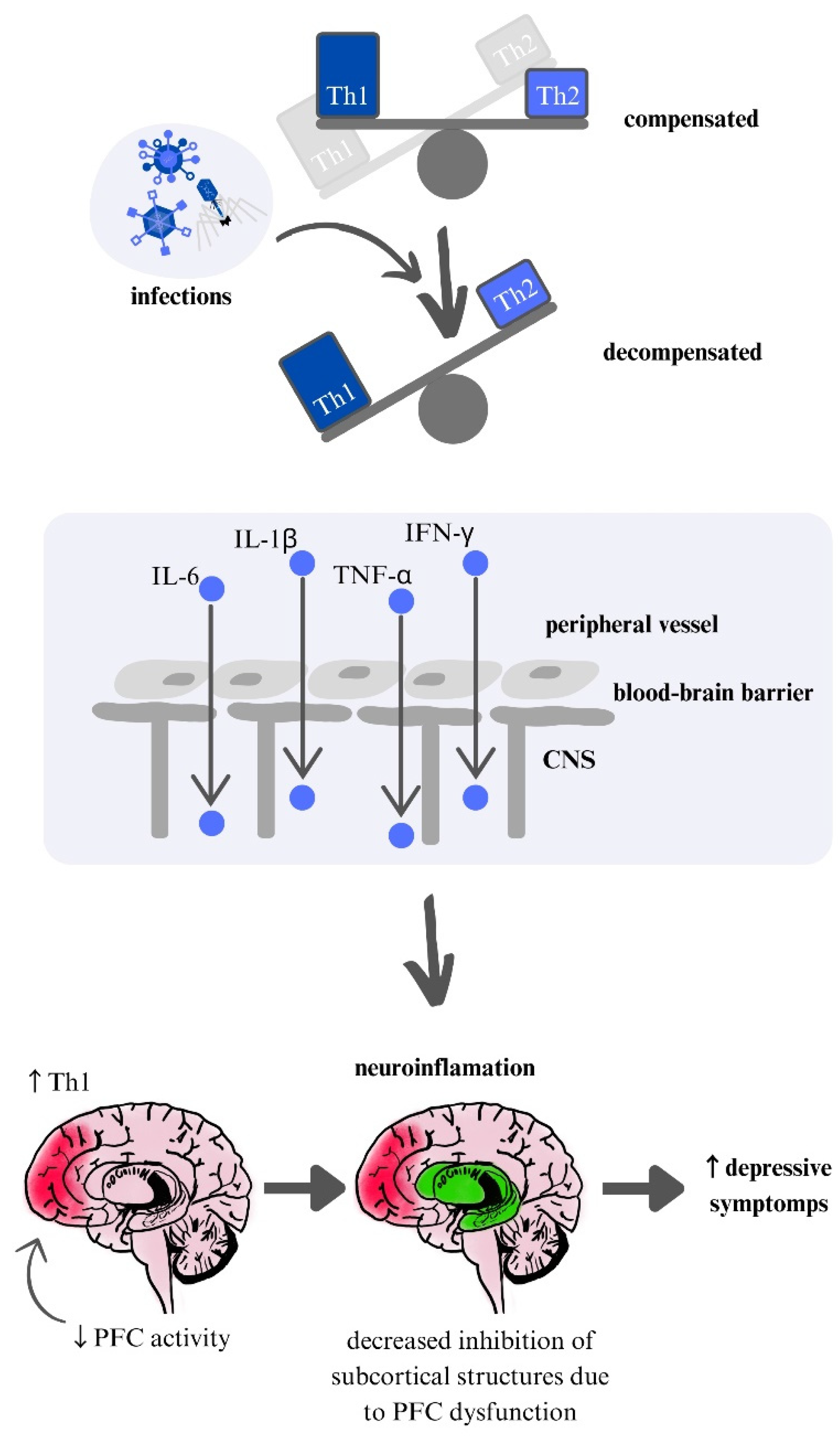
4.1. Outline of the Immunoseasonal Theory
4.2. Extension of the Immunoseasonal Theory
5. Empirical Evidence: Characteristics of Weather Factors
5.1. Humidity
5.2. Temperature
5.3. Atmospheric pressure
5.4. Wind
5.5. Insolation
6. Empirical Evidence: Seasonal Trends
6.1. Depression
6.2. Schizophrenia
6.3. Bipolar Disorder
6.4. Others—ASD, PTSD, GAD
7. Conclusions
7.1. One Mechanism for All Mental Health Issues?
7.2. Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Brandl, E.J.; Lett, T.A.; Bakanidze, G.; Heinz, A.; Bermpohl, F.; Schouler-Ocak, M. Weather conditions influence the number of psychiatric emergency room patients. Int J Biometeorol 2018, 62, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Waszkiewicz, N.; Chlabicz, M.; Paniczko, M.; Jamiołkowski, J.; Sowa, P.; Szpakowicz, M.; Łapińska, M.; Raczkowsk, A.; Kamiński, K. Humidity as the meteorological factor that influences seasonal depression. Neuroscience Applied 2022, 1, 100181. [Google Scholar] [CrossRef]
- Waszkiewicz, N. The Immunoseasonal Theory of Psychiatric Disorders. J Clin Med 2023, 12. [Google Scholar] [CrossRef] [PubMed]
- Brüne, M. Schizophrenia as parasitic behavior manipulation: can we put together the pieces of an evolutionary puzzle? World Psychiatry 2020, 19, 119–120. [Google Scholar] [CrossRef]
- Woodland, L.; Ratwatte, P.; Phalkey, R.; Gillingham, E.L. Investigating the Health Impacts of Climate Change among People with Pre-Existing Mental Health Problems: A Scoping Review. Int J Environ Res Public Health 2023, 20. [Google Scholar] [CrossRef]
- Maes, M. Major depression and activation of the inflammatory response system. Adv Exp Med Biol 1999, 461, 25–46. [Google Scholar] [CrossRef]
- Yirmiya, R. The inflammatory underpinning of depression: An historical perspective. Brain Behav Immun 2024, 122, 433–443. [Google Scholar] [CrossRef]
- Gałecki, P.; Talarowska, M. Inflammatory theory of depression. Psychiatr Pol 2018, 52, 437–447. [Google Scholar] [CrossRef]
- Steiner, J.; Walter, M.; Gos, T.; Guillemin, G.J.; Bernstein, H.G.; Sarnyai, Z.; Mawrin, C.; Brisch, R.; Bielau, H.; Meyer zu Schwabedissen, L.; et al. Severe depression is associated with increased microglial quinolinic acid in subregions of the anterior cingulate gyrus: evidence for an immune-modulated glutamatergic neurotransmission? J Neuroinflammation 2011, 8, 94. [Google Scholar] [CrossRef]
- Liebner, S.; Dijkhuizen, R.M.; Reiss, Y.; Plate, K.H.; Agalliu, D.; Constantin, G. Functional morphology of the blood-brain barrier in health and disease. Acta Neuropathol 2018, 135, 311–336. [Google Scholar] [CrossRef]
- Yang, J.; Ran, M.; Li, H.; Lin, Y.; Ma, K.; Yang, Y.; Fu, X.; Yang, S. New insight into neurological degeneration: Inflammatory cytokines and blood-brain barrier. Front Mol Neurosci 2022, 15, 1013933. [Google Scholar] [CrossRef] [PubMed]
- Slavich, G.M.; Irwin, M.R. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull 2014, 140, 774–815. [Google Scholar] [CrossRef] [PubMed]
- Galińska-Skok, B.; Waszkiewicz, N. Markers of Schizophrenia-A Critical Narrative Update. J Clin Med 2022, 11. [Google Scholar] [CrossRef] [PubMed]
- Orlovska-Waast, S.; Köhler-Forsberg, O.; Brix, S.W.; Nordentoft, M.; Kondziella, D.; Krogh, J.; Benros, M.E. Cerebrospinal fluid markers of inflammation and infections in schizophrenia and affective disorders: a systematic review and meta-analysis. Mol Psychiatry 2019, 24, 869–887. [Google Scholar] [CrossRef]
- Gottesman, I.I.; Gould, T.D. The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry 2003, 160, 636–645. [Google Scholar] [CrossRef]
- Smith, R.S. The macrophage theory of depression. Med Hypotheses 1991, 35, 298–306. [Google Scholar] [CrossRef]
- Levine, J.; Barak, Y.; Chengappa, K.N.; Rapoport, A.; Rebey, M.; Barak, V. Cerebrospinal cytokine levels in patients with acute depression. Neuropsychobiology 1999, 40, 171–176. [Google Scholar] [CrossRef]
- Sluzewska, A.; Rybakowski, J.; Bosmans, E.; Sobieska, M.; Berghmans, R.; Maes, M.; Wiktorowicz, K. Indicators of immune activation in major depression. Psychiatry Res 1996, 64, 161–167. [Google Scholar] [CrossRef]
- Lindqvist, D.; Dhabhar, F.S.; James, S.J.; Hough, C.M.; Jain, F.A.; Bersani, F.S.; Reus, V.I.; Verhoeven, J.E.; Epel, E.S.; Mahan, L.; et al. Oxidative stress, inflammation and treatment response in major depression. Psychoneuroendocrinology 2017, 76, 197–205. [Google Scholar] [CrossRef]
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav Immun 2020, 89, 594–600. [Google Scholar] [CrossRef]
- Lee, C.H.; Giuliani, F. The Role of Inflammation in Depression and Fatigue. Front Immunol 2019, 10, 1696. [Google Scholar] [CrossRef] [PubMed]
- Beurel, E.; Toups, M.; Nemeroff, C.B. The Bidirectional Relationship of Depression and Inflammation: Double Trouble. Neuron 2020, 107, 234–256. [Google Scholar] [CrossRef] [PubMed]
- Dowlati, Y.; Herrmann, N.; Swardfager, W.; Liu, H.; Sham, L.; Reim, E.K.; Lanctôt, K.L. A meta-analysis of cytokines in major depression. Biol Psychiatry 2010, 67, 446–457. [Google Scholar] [CrossRef] [PubMed]
- Haapakoski, R.; Mathieu, J.; Ebmeier, K.P.; Alenius, H.; Kivimäki, M. Cumulative meta-analysis of interleukins 6 and 1β, tumour necrosis factor α and C-reactive protein in patients with major depressive disorder. Brain Behav Immun 2015, 49, 206–215. [Google Scholar] [CrossRef]
- Pillinger, T.; D’Ambrosio, E.; McCutcheon, R.; Howes, O.D. Is psychosis a multisystem disorder? A meta-review of central nervous system, immune, cardiometabolic, and endocrine alterations in first-episode psychosis and perspective on potential models. Mol Psychiatry 2019, 24, 776–794. [Google Scholar] [CrossRef]
- Momtazmanesh, S.; Zare-Shahabadi, A.; Rezaei, N. Cytokine Alterations in Schizophrenia: An Updated Review. Front Psychiatry 2019, 10, 892. [Google Scholar] [CrossRef]
- Halstead, S.; Siskind, D.; Amft, M.; Wagner, E.; Yakimov, V.; Shih-Jung Liu, Z.; Walder, K.; Warren, N. Alteration patterns of peripheral concentrations of cytokines and associated inflammatory proteins in acute and chronic stages of schizophrenia: a systematic review and network meta-analysis. Lancet Psychiatry 2023, 10, 260–271. [Google Scholar] [CrossRef]
- Li, H.; Hong, W.; Zhang, C.; Wu, Z.; Wang, Z.; Yuan, C.; Li, Z.; Huang, J.; Lin, Z.; Fang, Y. IL-23 and TGF-β1 levels as potential predictive biomarkers in treatment of bipolar I disorder with acute manic episode. J Affect Disord 2015, 174, 361–366. [Google Scholar] [CrossRef]
- Brietzke, E.; Stertz, L.; Fernandes, B.S.; Kauer-Sant’anna, M.; Mascarenhas, M.; Escosteguy Vargas, A.; Chies, J.A.; Kapczinski, F. Comparison of cytokine levels in depressed, manic and euthymic patients with bipolar disorder. J Affect Disord 2009, 116, 214–217. [Google Scholar] [CrossRef]
- O’Brien, S.M.; Scully, P.; Scott, L.V.; Dinan, T.G. Cytokine profiles in bipolar affective disorder: focus on acutely ill patients. J Affect Disord 2006, 90, 263–267. [Google Scholar] [CrossRef]
- Kim, Y.K.; Jung, H.G.; Myint, A.M.; Kim, H.; Park, S.H. Imbalance between pro-inflammatory and anti-inflammatory cytokines in bipolar disorder. J Affect Disord 2007, 104, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Becking, K.; Boschloo, L.; Vogelzangs, N.; Haarman, B.C.; Riemersma-van der Lek, R.; Penninx, B.W.; Schoevers, R.A. The association between immune activation and manic symptoms in patients with a depressive disorder. Transl Psychiatry 2013, 3, e314. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Domínguez, A.; Hernández, M.E.; Berlanga, C.; Gutiérrez-Mora, D.; Moreno, J.; Heinze, G.; Pavón, L. Immune variations in bipolar disorder: phasic differences. Bipolar Disord 2007, 9, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Modabbernia, A.; Taslimi, S.; Brietzke, E.; Ashrafi, M. Cytokine alterations in bipolar disorder: a meta-analysis of 30 studies. Biol Psychiatry 2013, 74, 15–25. [Google Scholar] [CrossRef]
- Won, E.; Kim, Y.K. Neuroinflammation-Associated Alterations of the Brain as Potential Neural Biomarkers in Anxiety Disorders. Int J Mol Sci 2020, 21. [Google Scholar] [CrossRef]
- Woodward, E.A.; Prêle, C.M.; Nicholson, S.E.; Kolesnik, T.B.; Hart, P.H. The anti-inflammatory effects of interleukin-4 are not mediated by suppressor of cytokine signalling-1 (SOCS1). Immunology 2010, 131, 118–127. [Google Scholar] [CrossRef]
- Vieira, M.M.; Ferreira, T.B.; Pacheco, P.A.; Barros, P.O.; Almeida, C.R.; Araújo-Lima, C.F.; Silva-Filho, R.G.; Hygino, J.; Andrade, R.M.; Linhares, U.C.; et al. Enhanced Th17 phenotype in individuals with generalized anxiety disorder. J Neuroimmunol 2010, 229, 212–218. [Google Scholar] [CrossRef]
- Copeland, W.E.; Shanahan, L.; Worthman, C.; Angold, A.; Costello, E.J. Generalized anxiety and C-reactive protein levels: a prospective, longitudinal analysis. Psychol Med 2012, 42, 2641–2650. [Google Scholar] [CrossRef]
- Passos, I.C.; Vasconcelos-Moreno, M.P.; Costa, L.G.; Kunz, M.; Brietzke, E.; Quevedo, J.; Salum, G.; Magalhães, P.V.; Kapczinski, F.; Kauer-Sant’Anna, M. Inflammatory markers in post-traumatic stress disorder: a systematic review, meta-analysis, and meta-regression. Lancet Psychiatry 2015, 2, 1002–1012. [Google Scholar] [CrossRef]
- O’Donovan, A.; Ahmadian, A.J.; Neylan, T.C.; Pacult, M.A.; Edmondson, D.; Cohen, B.E. Current posttraumatic stress disorder and exaggerated threat sensitivity associated with elevated inflammation in the Mind Your Heart Study. Brain Behav Immun 2017, 60, 198–205. [Google Scholar] [CrossRef]
- de Oliveira, J.F.; Wiener, C.D.; Jansen, K.; Portela, L.V.; Lara, D.R.; Souza, L.D.M.; da Silva, R.A.; Moreira, F.P.; Oses, J.P. Serum levels of interleukins IL-6 and IL-10 in individuals with posttraumatic stress disorder in a population-based sample. Psychiatry Res 2018, 260, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Modabbernia, A.; Velthorst, E.; Reichenberg, A. Environmental risk factors for autism: an evidence-based review of systematic reviews and meta-analyses. Mol Autism 2017, 8, 13. [Google Scholar] [CrossRef] [PubMed]
- Saghazadeh, A.; Ataeinia, B.; Keynejad, K.; Abdolalizadeh, A.; Hirbod-Mobarakeh, A.; Rezaei, N. A meta-analysis of pro-inflammatory cytokines in autism spectrum disorders: Effects of age, gender, and latitude. J Psychiatr Res 2019, 115, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Zhang, H.; Liu, S.; Luo, W.; Jiang, Y.; Gao, J. Association of Peripheral Blood Levels of Cytokines With Autism Spectrum Disorder: A Meta-Analysis. Front Psychiatry 2021, 12, 670200. [Google Scholar] [CrossRef]
- Nour-Eldine, W.; Ltaief, S.M.; Abdul Manaph, N.P.; Al-Shammari, A.R. In search of immune cellular sources of abnormal cytokines in the blood in autism spectrum disorder: A systematic review of case-control studies. Front Immunol 2022, 13, 950275. [Google Scholar] [CrossRef]
- Pardo, C.A.; Farmer, C.A.; Thurm, A.; Shebl, F.M.; Ilieva, J.; Kalra, S.; Swedo, S. Serum and cerebrospinal fluid immune mediators in children with autistic disorder: a longitudinal study. Mol Autism 2017, 8, 1. [Google Scholar] [CrossRef]
- Ellul, P.; Rosenzwajg, M.; Peyre, H.; Fourcade, G.; Mariotti-Ferrandiz, E.; Trebossen, V.; Klatzmann, D.; Delorme, R. Regulatory T lymphocytes/Th17 lymphocytes imbalance in autism spectrum disorders: evidence from a meta-analysis. Mol Autism 2021, 12, 68. [Google Scholar] [CrossRef]
- Rossi, C.C.; Van de Water, J.; Rogers, S.J.; Amaral, D.G. Detection of plasma autoantibodies to brain tissue in young children with and without autism spectrum disorders. Brain Behav Immun 2011, 25, 1123–1135. [Google Scholar] [CrossRef]
- Ashwood, P.; Krakowiak, P.; Hertz-Picciotto, I.; Hansen, R.; Pessah, I.; Van de Water, J. Elevated plasma cytokines in autism spectrum disorders provide evidence of immune dysfunction and are associated with impaired behavioral outcome. Brain Behav Immun 2011, 25, 40–45. [Google Scholar] [CrossRef]
- Smith, R.S. A comprehensive macrophage-T-lymphocyte theory of schizophrenia. Med Hypotheses 1992, 39, 248–257. [Google Scholar] [CrossRef]
- Raphael, I.; Nalawade, S.; Eagar, T.N.; Forsthuber, T.G. T cell subsets and their signature cytokines in autoimmune and inflammatory diseases. Cytokine 2015, 74, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Fisman, D. Seasonality of viral infections: mechanisms and unknowns. Clin Microbiol Infect 2012, 18, 946–954. [Google Scholar] [CrossRef] [PubMed]
- Audi, A.; AlIbrahim, M.; Kaddoura, M.; Hijazi, G.; Yassine, H.M.; Zaraket, H. Seasonality of Respiratory Viral Infections: Will COVID-19 Follow Suit? Front Public Health 2020, 8, 567184. [Google Scholar] [CrossRef] [PubMed]
- Lorkiewicz, P.; Waszkiewicz, N. Viral infections in etiology of mental disorders: a broad analysis of cytokine profile similarities - a narrative review. Front Cell Infect Microbiol 2024, 14, 1423739. [Google Scholar] [CrossRef]
- Maes, M.; De Meyer, F. Relationships of climatic data to immune and hematologic variables in normal human. Neuro Endocrinol Lett 2000, 21, 127–136. [Google Scholar]
- Maes, M.; Stevens, W.; Scharpé, S.; Bosmans, E.; De Meyer, F.; D’Hondt, P.; Peeters, D.; Thompson, P.; Cosyns, P.; De Clerck, L. Seasonal variation in peripheral blood leukocyte subsets and in serum interleukin-6, and soluble interleukin-2 and -6 receptor concentrations in normal volunteers. Experientia 1994, 50, 821–829. [Google Scholar] [CrossRef]
- Katila, H.; Cantell, K.; Appelberg, B.; Rimón, R. Is there a seasonal variation in the interferon-producing capacity of healthy subjects? J Interferon Res 1993, 13, 233–234. [Google Scholar] [CrossRef]
- Balashov, K.E.; Olek, M.J.; Smith, D.R.; Khoury, S.J.; Weiner, H.L. Seasonal variation of interferon-gamma production in progressive multiple sclerosis. Ann Neurol 1998, 44, 824–828. [Google Scholar] [CrossRef]
- Więdłocha, M.; Marcinowicz, P.; Krupa, R.; Janoska-Jaździk, M.; Janus, M.; Dębowska, W.; Mosiołek, A.; Waszkiewicz, N.; Szulc, A. Effect of antidepressant treatment on peripheral inflammation markers - A meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry 2018, 80, 217–226. [Google Scholar] [CrossRef]
- Dev, S.I.; Moore, R.C.; Soontornniyomkij, B.; Achim, C.L.; Jeste, D.V.; Eyler, L.T. Peripheral inflammation related to lower fMRI activation during a working memory task and resting functional connectivity among older adults: a preliminary study. Int J Geriatr Psychiatry 2017, 32, 341–349. [Google Scholar] [CrossRef]
- Budu-Aggrey, A.; Joyce, S.; Davies, N.M.; Paternoster, L.; Munafò, M.R.; Brown, S.J.; Evans, J.; Sallis, H.M. Investigating the causal relationship between allergic disease and mental health. Clin Exp Allergy 2021, 51, 1449–1458. [Google Scholar] [CrossRef] [PubMed]
- Najjar, S.; Pearlman, D.M.; Alper, K.; Najjar, A.; Devinsky, O. Neuroinflammation and psychiatric illness. J Neuroinflammation 2013, 10, 43. [Google Scholar] [CrossRef] [PubMed]
- Ruscio, A.M.; Hallion, L.S.; Lim, C.C.W.; Aguilar-Gaxiola, S.; Al-Hamzawi, A.; Alonso, J.; Andrade, L.H.; Borges, G.; Bromet, E.J.; Bunting, B.; et al. Cross-sectional Comparison of the Epidemiology of DSM-5 Generalized Anxiety Disorder Across the Globe. JAMA Psychiatry 2017, 74, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Zorn, J.V.; Schür, R.R.; Boks, M.P.; Kahn, R.S.; Joëls, M.; Vinkers, C.H. Cortisol stress reactivity across psychiatric disorders: A systematic review and meta-analysis. Psychoneuroendocrinology 2017, 77, 25–36. [Google Scholar] [CrossRef]
- Correia, A.S.; Vale, N. Advancements Exploring Major Depressive Disorder: Insights on Oxidative Stress, Serotonin Metabolism, BDNF, HPA Axis Dysfunction, and Pharmacotherapy Advances. International Journal of Translational Medicine 2024, 4, 176–196. [Google Scholar] [CrossRef]
- Pizzagalli, D.A.; Roberts, A.C. Prefrontal cortex and depression. Neuropsychopharmacology 2022, 47, 225–246. [Google Scholar] [CrossRef]
- Albert, P.R.; Vahid-Ansari, F.; Luckhart, C. Serotonin-prefrontal cortical circuitry in anxiety and depression phenotypes: pivotal role of pre- and post-synaptic 5-HT1A receptor expression. Front Behav Neurosci 2014, 8, 199. [Google Scholar] [CrossRef]
- Nixon, N.L.; Liddle, P.F.; Worwood, G.; Liotti, M.; Nixon, E. Prefrontal cortex function in remitted major depressive disorder. Psychol Med 2013, 43, 1219–1230. [Google Scholar] [CrossRef]
- Etkin, A.; Prater, K.E.; Schatzberg, A.F.; Menon, V.; Greicius, M.D. Disrupted amygdalar subregion functional connectivity and evidence of a compensatory network in generalized anxiety disorder. Arch Gen Psychiatry 2009, 66, 1361–1372. [Google Scholar] [CrossRef]
- Ramasubbu, R.; Konduru, N.; Cortese, F.; Bray, S.; Gaxiola-Valdez, I.; Goodyear, B. Reduced intrinsic connectivity of amygdala in adults with major depressive disorder. Front Psychiatry 2014, 5, 17. [Google Scholar] [CrossRef]
- Dantzer, R.; O’Connor, J.C.; Freund, G.G.; Johnson, R.W.; Kelley, K.W. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci 2008, 9, 46–56. [Google Scholar] [CrossRef]
- Zimmerman, G.; Shaltiel, G.; Barbash, S.; Cohen, J.; Gasho, C.J.; Shenhar-Tsarfaty, S.; Shalev, H.; Berliner, S.A.; Shelef, I.; Shoham, S.; et al. Post-traumatic anxiety associates with failure of the innate immune receptor TLR9 to evade the pro-inflammatory NFκB pathway. Transl Psychiatry 2012, 2, e78. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.K.; Amidfar, M.; Won, E. A review on inflammatory cytokine-induced alterations of the brain as potential neural biomarkers in post-traumatic stress disorder. Prog Neuropsychopharmacol Biol Psychiatry 2019, 91, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Sarapultsev, A.; Sarapultsev, P.; Dremencov, E.; Komelkova, M.; Tseilikman, O.; Tseilikman, V. Low glucocorticoids in stress-related disorders: the role of inflammation. Stress 2020, 23, 651–661. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Neylan, T.C.; Mueller, S.G.; Lenoci, M.; Truran, D.; Marmar, C.R.; Weiner, M.W.; Schuff, N. Magnetic resonance imaging of hippocampal subfields in posttraumatic stress disorder. Arch Gen Psychiatry 2010, 67, 296–303. [Google Scholar] [CrossRef]
- Campbell, S.; Marriott, M.; Nahmias, C.; MacQueen, G.M. Lower hippocampal volume in patients suffering from depression: a meta-analysis. Am J Psychiatry 2004, 161, 598–607. [Google Scholar] [CrossRef]
- Ploski, J.E.; Vaidya, V.A. The Neurocircuitry of Posttraumatic Stress Disorder and Major Depression: Insights Into Overlapping and Distinct Circuit Dysfunction-A Tribute to Ron Duman. Biol Psychiatry 2021, 90, 109–117. [Google Scholar] [CrossRef]
- Johnstone, T.; van Reekum, C.M.; Urry, H.L.; Kalin, N.H.; Davidson, R.J. Failure to regulate: counterproductive recruitment of top-down prefrontal-subcortical circuitry in major depression. J Neurosci 2007, 27, 8877–8884. [Google Scholar] [CrossRef]
- Etkin, A.; Wager, T.D. Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry 2007, 164, 1476–1488. [Google Scholar] [CrossRef]
- Rauch, S.L.; Shin, L.M.; Phelps, E.A. Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research--past, present, and future. Biol Psychiatry 2006, 60, 376–382. [Google Scholar] [CrossRef]
- Shin, L.M.; Rauch, S.L.; Pitman, R.K. Amygdala, medial prefrontal cortex, and hippocampal function in PTSD. Ann N Y Acad Sci 2006, 1071, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Chauhan, A.; Sheikh, A.M.; Patil, S.; Chauhan, V.; Li, X.M.; Ji, L.; Brown, T.; Malik, M. Elevated immune response in the brain of autistic patients. J Neuroimmunol 2009, 207, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Keown, C.L.; Shih, P.; Nair, A.; Peterson, N.; Mulvey, M.E.; Müller, R.A. Local functional overconnectivity in posterior brain regions is associated with symptom severity in autism spectrum disorders. Cell Rep 2013, 5, 567–572. [Google Scholar] [CrossRef] [PubMed]
- Donovan, A.P.; Basson, M.A. The neuroanatomy of autism - a developmental perspective. J Anat 2017, 230, 4–15. [Google Scholar] [CrossRef]
- Florido Ngu, F.; Kelman, I.; Chambers, J.; Ayeb-Karlsson, S. Correlating heatwaves and relative humidity with suicide (fatal intentional self-harm). Sci Rep 2021, 11, 22175. [Google Scholar] [CrossRef]
- Ding, N.; Berry, H.L.; Bennett, C.M. The Importance of Humidity in the Relationship between Heat and Population Mental Health: Evidence from Australia. PLoS One 2016, 11, e0164190. [Google Scholar] [CrossRef]
- Vida, S.; Durocher, M.; Ouarda, T.B.; Gosselin, P. Relationship between ambient temperature and humidity and visits to mental health emergency departments in Québec. Psychiatr Serv 2012, 63, 1150–1153. [Google Scholar] [CrossRef]
- D’Hondt, P.; Maes, M.; Leysen, J.E.; Gommeren, W.; Heylen, L.; DeMeyer, F.; Scharpe, S.; Peeters, D.; Desnyder, R. Seasonal variation in platelet [3H]paroxetine binding in healthy volunteers. Relationship to climatic variables. Neuropsychopharmacology 1996, 15, 187–198. [Google Scholar] [CrossRef]
- Maes, M.; Scharpé, S.; Verkerk, R.; D’Hondt, P.; Peeters, D.; Cosyns, P.; Thompson, P.; De Meyer, F.; Wauters, A.; Neels, H. Seasonal variation in plasma L-tryptophan availability in healthy volunteers. Relationships to violent suicide occurrence. Arch Gen Psychiatry 1995, 52, 937–946. [Google Scholar] [CrossRef]
- Salib, E.; Sharp, N. Relative humidity and affective disorders. Int J Psychiatry Clin Pract 2002, 6, 147–153. [Google Scholar] [CrossRef]
- Rizavas, I.; Gournellis, R.; Pantazis, N.; Chatzinikolaou, F.; Douzenis, P.; Efstathiou, V.; Lagouvardos, K.; Douzenis, A. The impact of meteorological factors on involuntary admission in Attica, Greece. Psychiatriki 2023, 34, 289–300. [Google Scholar] [CrossRef] [PubMed]
- Dixon, P.G.; Sinyor, M.; Schaffer, A.; Levitt, A.; Haney, C.R.; Ellis, K.N.; Sheridan, S.C. Association of weekly suicide rates with temperature anomalies in two different climate types. Int J Environ Res Public Health 2014, 11, 11627–11644. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Lavigne, E.; Ouellette-kuntz, H.; Chen, B.E. Acute impacts of extreme temperature exposure on emergency room admissions related to mental and behavior disorders in Toronto, Canada. J Affect Disord 2014, 155, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Bundo, M.; de Schrijver, E.; Federspiel, A.; Toreti, A.; Xoplaki, E.; Luterbacher, J.; Franco, O.H.; Müller, T.; Vicedo-Cabrera, A.M. Ambient temperature and mental health hospitalizations in Bern, Switzerland: A 45-year time-series study. PLoS One 2021, 16, e0258302. [Google Scholar] [CrossRef]
- Talaei, A.; Hedjazi, A.; Rezaei Ardani, A.; Fayyazi Bordbar, M.R. The relationship between meteorological conditions and homicide, suicide, rage, and psychiatric hospitalization. J Forensic Sci 2014, 59, 1397–1402. [Google Scholar] [CrossRef]
- Carney, P.A.; Fitzgerald, C.T.; Monaghan, C.E. Influence of climate on the prevalence of mania. Br J Psychiatry 1988, 152, 820–823. [Google Scholar] [CrossRef]
- Abdul-Rahim, F.A.; Al-Sabai, A.; Al-Hamad, A.R.; Bamgboye, E. The seasonality of mania: Preliminary findings. Ann Saudi Med 1992, 12, 472–475. [Google Scholar] [CrossRef]
- Maes, M.; De Meyer, F.; Thompson, P.; Peeters, D.; Cosyns, P. Synchronized annual rhythms in violent suicide rate, ambient temperature and the light-dark span. Acta Psychiatr Scand 1994, 90, 391–396. [Google Scholar] [CrossRef]
- Müller, H.; Biermann, T.; Renk, S.; Reulbach, U.; Ströbel, A.; Kornhuber, J.; Sperling, W. Higher environmental temperature and global radiation are correlated with increasing suicidality--a localized data analysis. Chronobiol Int 2011, 28, 949–957. [Google Scholar] [CrossRef]
- Aguglia, A.; Giacomini, G.; Montagna, E.; Amerio, A.; Escelsior, A.; Capello, M.; Cutroneo, L.; Ferretti, G.; Scafidi, D.; Costanza, A.; et al. Meteorological Variables and Suicidal Behavior: Air Pollution and Apparent Temperature Are Associated With High-Lethality Suicide Attempts and Male Gender. Front Psychiatry 2021, 12, 653390. [Google Scholar] [CrossRef]
- Hiltunen, L.; Ruuhela, R.; Ostamo, A.; Lönnqvist, J.; Suominen, K.; Partonen, T. Atmospheric pressure and suicide attempts in Helsinki, Finland. Int J Biometeorol 2012, 56, 1045–1053. [Google Scholar] [CrossRef] [PubMed]
- Schory, T.J.; Piecznski, N.; Nair, S.; el-Mallakh, R.S. Barometric pressure, emergency psychiatric visits, and violent acts. Can J Psychiatry 2003, 48, 624–627. [Google Scholar] [CrossRef] [PubMed]
- El-Mallakh, R.S.; Brar, K.; Watkins, C.; Nuss, S.; O’Connor, S.S.; Gao, Y.; Wright, J.H. Association Between Low Barometric Pressure and Completed Suicides. Am J Psychiatry 2017, 174, 905. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.Y. Geophysical variables and behavior: LXXXXIX. The influence of weather on suicide in Hong Kong. Percept Mot Skills 2000, 91, 571–577. [Google Scholar] [CrossRef]
- Wu, Y.W.; Chen, C.K.; Wang, L.J. Is suicide mortality associated with meteorological and socio-economic factors? An ecological study in a city in Taiwan with a high suicide rate. Psychiatr Danub 2014, 26, 152–158. [Google Scholar]
- Tapak, L.; Maryanaji, Z.; Hamidi, O.; Abbasi, H.; Najafi-Vosough, R. Investigating the effect of climatic parameters on mental disorder admissions. Int J Biometeorol 2018, 62, 2109–2118. [Google Scholar] [CrossRef]
- Li, D.; Zhang, Y.; Li, X.; Zhang, K.; Lu, Y.; Brown, R.D. Climatic and meteorological exposure and mental and behavioral health: A systematic review and meta-analysis. Sci Total Environ 2023, 892, 164435. [Google Scholar] [CrossRef]
- Mawson, D.; Smith, A. Relative humidity and manic admissions in the London area. Br J Psychiatry 1981, 138, 134–138. [Google Scholar] [CrossRef]
- Boker, S.M.; Leibenluft, E.; Deboeck, P.R.; Virk, G.; Postolache, T.T. Mood Oscillations and Coupling Between Mood and Weather in Patients with Rapid Cycling Bipolar Disorder. Int J Child Health Hum Dev 2008, 1, 181–203. [Google Scholar]
- Mizoguchi, H.; Fukaya, K.; Mori, R.; Itoh, M.; Funakubo, M.; Sato, J. Lowering barometric pressure aggravates depression-like behavior in rats. Behav Brain Res 2011, 218, 190–193. [Google Scholar] [CrossRef]
- McWilliams, S.; Kinsella, A.; O’Callaghan, E. Daily weather variables and affective disorder admissions to psychiatric hospitals. Int J Biometeorol 2014, 58, 2045–2057. [Google Scholar] [CrossRef] [PubMed]
- Falagas, M.E.; Theocharis, G.; Spanos, A.; Vlara, L.A.; Issaris, E.A.; Panos, G.; Peppas, G. Effect of meteorological variables on the incidence of respiratory tract infections. Respir Med 2008, 102, 733–737. [Google Scholar] [CrossRef] [PubMed]
- Yackerson, N.S.; Zilberman, A.; Todder, D.; Kaplan, Z. The influence of air-suspended particulate concentration on the incidence of suicide attempts and exacerbation of schizophrenia. Int J Biometeorol 2014, 58, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Haid, M.; Gohm, A.; Umek, L.; Ward, H.C.; Rotach, M.W. Cold-Air Pool Processes in the Inn Valley During Föhn: A Comparison of Four Cases During the PIANO Campaign. Boundary Layer Meteorol 2022, 182, 335–362. [Google Scholar] [CrossRef]
- Mikutta, C.A.; Pervilhac, C.; Znoj, H.; Federspiel, A.; Müller, T.J. The Impact of Foehn Wind on Mental Distress among Patients in a Swiss Psychiatric Hospital. Int J Environ Res Public Health 2022, 19. [Google Scholar] [CrossRef]
- Delyukov, A.; Didyk, L. The effects of extra-low-frequency atmospheric pressure oscillations on human mental activity. Int J Biometeorol 1999, 43, 31–37. [Google Scholar] [CrossRef]
- Saulnier, K.G.; Bagge, C.L. Changes in meteorological conditions as near-term risk factors for suicide attempts. Int J Biometeorol 2024. [Google Scholar] [CrossRef]
- Hu, T.; Xu, Z.Y.; Wang, J.; Su, Y.; Guo, B.B. Meteorological factors, ambient air pollution, and daily hospital admissions for depressive disorder in Harbin: A time-series study. World J Psychiatry 2023, 13, 1061–1078. [Google Scholar] [CrossRef]
- Vencloviene, J.; Beresnevaite, M.; Cerkauskaite, S.; Lopatiene, K.; Grizas, V.; Benetis, R. The effects of weather on depressive symptoms in patients after cardiac surgery. Psychol Health Med 2023, 28, 682–692. [Google Scholar] [CrossRef]
- Brazienė, A.; Venclovienė, J.; Vaičiulis, V.; Lukšienė, D.; Tamošiūnas, A.; Milvidaitė, I.; Radišauskas, R.; Bobak, M. Relationship between Depressive Symptoms and Weather Conditions. Int J Environ Res Public Health 2022, 19. [Google Scholar] [CrossRef]
- Seregi, B.; Kapitány, B.; Maróti-Agóts, Á.; Rihmer, Z.; Gonda, X.; Döme, P. Weak associations between the daily number of suicide cases and amount of daily sunlight. Prog Neuropsychopharmacol Biol Psychiatry 2017, 73, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Jee, H.J.; Cho, C.H.; Lee, Y.J.; Choi, N.; An, H.; Lee, H.J. Solar radiation increases suicide rate after adjusting for other climate factors in South Korea. Acta Psychiatr Scand 2017, 135, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Bang, M.; Wee, J.H.; Min, C.; Yoo, D.M.; Han, S.M.; Kim, S.; Choi, H.G. Short- and long-term exposure to air pollution and lack of sunlight are associated with an increased risk of depression: A nested case-control study using meteorological data and national sample cohort data. Sci Total Environ 2021, 757, 143960. [Google Scholar] [CrossRef] [PubMed]
- Tietjen, G.H.; Kripke, D.F. Suicides in California (1968-1977): absence of seasonality in Los Angeles and Sacramento counties. Psychiatry Res 1994, 53, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, F.C.; Frangakis, C.E.; Skalkidou, A.; Petridou, E.; Stevens, R.G.; Trichopoulos, D. Exploring lag and duration effect of sunshine in triggering suicide. J Affect Disord 2005, 88, 287–297. [Google Scholar] [CrossRef]
- Gbyl, K.; Østergaard Madsen, H.; Dunker Svendsen, S.; Petersen, P.M.; Hageman, I.; Volf, C.; Martiny, K. Depressed Patients Hospitalized in Southeast-Facing Rooms Are Discharged Earlier than Patients in Northwest-Facing Rooms. Neuropsychobiology 2016, 74, 193–201. [Google Scholar] [CrossRef]
- Bauer, M.; Glenn, T.; Alda, M.; Andreassen, O.A.; Angelopoulos, E.; Ardau, R.; Baethge, C.; Bauer, R.; Bellivier, F.; Belmaker, R.H.; et al. Relationship between sunlight and the age of onset of bipolar disorder: an international multisite study. J Affect Disord 2014, 167, 104–111. [Google Scholar] [CrossRef]
- Lee, H.J.; Kim, L.; Joe, S.H.; Suh, K.Y. Effects of season and climate on the first manic episode of bipolar affective disorder in Korea. Psychiatry Res 2002, 113, 151–159. [Google Scholar] [CrossRef]
- Aguglia, A.; Serafini, G.; Escelsior, A.; Canepa, G.; Amore, M.; Maina, G. Maximum Temperature and Solar Radiation as Predictors of Bipolar Patient Admission in an Emergency Psychiatric Ward. Int J Environ Res Public Health 2019, 16. [Google Scholar] [CrossRef]
- Bauer, M.; Glenn, T.; Alda, M.; Andreassen, O.A.; Angelopoulos, E.; Ardau, R.; Ayhan, Y.; Baethge, C.; Bauer, R.; Baune, B.T.; et al. Association between solar insolation and a history of suicide attempts in bipolar I disorder. J Psychiatr Res 2019, 113, 1–9. [Google Scholar] [CrossRef]
- Dominiak, M.; Swiecicki, L.; Rybakowski, J. Psychiatric hospitalizations for affective disorders in Warsaw, Poland: Effect of season and intensity of sunlight. Psychiatry Res 2015, 229, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Morken, G.; Lilleeng, S.; Linaker, O.M. Seasonal variation in suicides and in admissions to hospital for mania and depression. J Affect Disord 2002, 69, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Gardarsdottir, H.; Egberts, T.C.; van Dijk, L.; Heerdink, E.R. Seasonal patterns of initiating antidepressant therapy in general practice in the Netherlands during 2002-2007. J Affect Disord 2010, 122, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Patten, S.B.; Williams, J.V.; Lavorato, D.H.; Bulloch, A.G.; Fiest, K.M.; Wang, J.L.; Sajobi, T.T. Seasonal variation in major depressive episode prevalence in Canada. Epidemiol Psychiatr Sci 2017, 26, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Näyhä, S. Autumn incidence of suicides re-examined: data from Finland by sex, age and occupation. Br J Psychiatry 1982, 141, 512–517. [Google Scholar] [CrossRef]
- Araki, S.; Murata, K. Suicide in Japan: socioeconomic effects on its secular and seasonal trends. Suicide Life Threat Behav 1987, 17, 64–71. [Google Scholar] [CrossRef]
- Sarran, C.; Albers, C.; Sachon, P.; Meesters, Y. Meteorological analysis of symptom data for people with seasonal affective disorder. Psychiatry Res 2017, 257, 501–505. [Google Scholar] [CrossRef]
- O’Hare, C.; O’Sullivan, V.; Flood, S.; Kenny, R.A. Seasonal and meteorological associations with depressive symptoms in older adults: A geo-epidemiological study. J Affect Disord 2016, 191, 172–179. [Google Scholar] [CrossRef]
- Christodoulou, C.; Douzenis, A.; Papadopoulos, F.C.; Papadopoulou, A.; Bouras, G.; Gournellis, R.; Lykouras, L. Suicide and seasonality. Acta Psychiatr Scand 2012, 125, 127–146. [Google Scholar] [CrossRef]
- Deisenhammer, E.A.; Kemmler, G.; Parson, P. Association of meteorological factors with suicide. Acta Psychiatr Scand 2003, 108, 455–459. [Google Scholar] [CrossRef]
- Sit, D.; Seltman, H.; Wisner, K.L. Seasonal effects on depression risk and suicidal symptoms in postpartum women. Depress Anxiety 2011, 28, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Sylvén, S.M.; Papadopoulos, F.C.; Olovsson, M.; Ekselius, L.; Poromaa, I.S.; Skalkidou, A. Seasonality patterns in postpartum depression. Am J Obstet Gynecol 2011, 204, 413.e411–416. [Google Scholar] [CrossRef] [PubMed]
- Kerr, D.C.; Shaman, J.; Washburn, I.J.; Vuchinich, S.; Neppl, T.K.; Capaldi, D.M.; Conger, R.D. Two longterm studies of seasonal variation in depressive symptoms among community participants. J Affect Disord 2013, 151, 837–842. [Google Scholar] [CrossRef] [PubMed]
- Øverland, S.; Woicik, W.; Sikora, L.; Whittaker, K.; Heli, H.; Skjelkvåle, F.S.; Sivertsen, B.; Colman, I. Seasonality and symptoms of depression: A systematic review of the literature. Epidemiol Psychiatr Sci 2019, 29, e31. [Google Scholar] [CrossRef] [PubMed]
- Rizavas, I.; Gournellis, R.; Douzenis, P.; Efstathiou, V.; Bali, P.; Lagouvardos, K.; Douzenis, A. A Systematic Review on the Impact of Seasonality on Severe Mental Illness Admissions: Does Seasonal Variation Affect Coercion? Healthcare (Basel) 2023, 11. [Google Scholar] [CrossRef]
- Hinterbuchinger, B.; König, D.; Gmeiner, A.; Listabarth, S.; Fellinger, M.; Thenius, C.; Baumgartner, J.S.; Vyssoki, S.; Waldhoer, T.; Vyssoki, B.; et al. Seasonality in schizophrenia-An analysis of a nationwide registry with 110,735 hospital admissions. Eur Psychiatry 2020, 63, e55. [Google Scholar] [CrossRef]
- Force, R.W.; Hansen, L.; Bedell, M. Psychotic episode after melatonin. Ann Pharmacother 1997, 31, 1408. [Google Scholar] [CrossRef]
- Touitou, Y.; Fèvre, M.; Bogdan, A.; Reinberg, A.; De Prins, J.; Beck, H.; Touitou, C. Patterns of plasma melatonin with ageing and mental condition: stability of nyctohemeral rhythms and differences in seasonal variations. Acta Endocrinol (Copenh) 1984, 106, 145–151. [Google Scholar] [CrossRef]
- Gu, S.; Huang, R.; Yang, J.; Sun, S.; Xu, Y.; Zhang, R.; Wang, Y.; Lu, B.; He, T.; Wang, A.; et al. Exposure-lag-response association between sunlight and schizophrenia in Ningbo, China. Environ Pollut 2019, 247, 285–292. [Google Scholar] [CrossRef]
- Carrillo-Vico, A.; Lardone, P.J.; Alvarez-Sánchez, N.; Rodríguez-Rodríguez, A.; Guerrero, J.M. Melatonin: buffering the immune system. Int J Mol Sci 2013, 14, 8638–8683. [Google Scholar] [CrossRef]
- Maestroni, G.J.; Conti, A.; Pierpaoli, W. Role of the pineal gland in immunity. III. Melatonin antagonizes the immunosuppressive effect of acute stress via an opiatergic mechanism. Immunology 1988, 63, 465–469. [Google Scholar] [PubMed]
- Ben-Nathan, D.; Maestroni, G.J.; Lustig, S.; Conti, A. Protective effects of melatonin in mice infected with encephalitis viruses. Arch Virol 1995, 140, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Davies, G.; Ahmad, F.; Chant, D.; Welham, J.; McGrath, J. Seasonality of first admissions for schizophrenia in the Southern Hemisphere. Schizophr Res 2000, 41, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Owens, N.; McGorry, P.D. Seasonality of symptom onset in first-episode schizophrenia. Psychol Med 2003, 33, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Dawidowski, B.; Górniak, A.; Podwalski, P.; Lebiecka, Z.; Misiak, B.; Samochowiec, J. The Role of Cytokines in the Pathogenesis of Schizophrenia. J Clin Med 2021, 10. [Google Scholar] [CrossRef]
- Yao, Y.; Shi, S.; Li, W.; Luo, B.; Yang, Y.; Li, M.; Zhang, L.; Yuan, X.; Zhou, X.; Liu, H.; et al. Seasonality of hospitalization for schizophrenia and mood disorders: A single-center cross-sectional study in China. J Affect Disord 2023, 323, 40–45. [Google Scholar] [CrossRef]
- McWilliams, S.; Kinsella, A.; O’Callaghan, E. The effects of daily weather variables on psychosis admissions to psychiatric hospitals. Int J Biometeorol 2013, 57, 497–508. [Google Scholar] [CrossRef]
- Jahan, S.; Wraith, D.; Dunne, M.P.; Naish, S.; McLean, D. Seasonality and schizophrenia: a comprehensive overview of the seasonal pattern of hospital admissions and potential drivers. Int J Biometeorol 2020, 64, 1423–1432. [Google Scholar] [CrossRef]
- Amr, M.; Volpe, F.M. Seasonal influences on admissions for mood disorders and schizophrenia in a teaching psychiatric hospital in Egypt. J Affect Disord 2012, 137, 56–60. [Google Scholar] [CrossRef]
- Bakstein, E.; Mladá, K.; Fárková, E.; Kolenič, M.; Španiel, F.; Manková, D.; Korčáková, J.; Winkler, P.; Hajek, T. Cross-sectional and within-subject seasonality and regularity of hospitalizations: A population study in mood disorders and schizophrenia. Bipolar Disord 2020, 22, 508–516. [Google Scholar] [CrossRef]
- Takei, N.; O’Callaghan, E.; Sham, P.; Glover, G.; Tamura, A.; Murray, R. Seasonality of admissions in the psychoses: effect of diagnosis, sex, and age at onset. Br J Psychiatry 1992, 161, 506–511. [Google Scholar] [CrossRef] [PubMed]
- Volpe, F.M.; Del Porto, J.A. Seasonality of admissions for mania in a psychiatric hospital of Belo Horizonte, Brazil. J Affect Disord 2006, 94, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Geoffroy, P.A.; Bellivier, F.; Scott, J.; Etain, B. Seasonality and bipolar disorder: a systematic review, from admission rates to seasonality of symptoms. J Affect Disord 2014, 168, 210–223. [Google Scholar] [CrossRef] [PubMed]
- Bullock, B.; Murray, G.; Meyer, D. Highs and lows, ups and downs: Meteorology and mood in bipolar disorder. PLoS One 2017, 12, e0173431. [Google Scholar] [CrossRef]
- Partonen, T.; Lönnqvist, J. Seasonal variation in bipolar disorder. Br J Psychiatry 1996, 169, 641–646. [Google Scholar] [CrossRef]
- Fellinger, M.; Waldhoer, T.; König, D.; Hinterbuchinger, B.; Pruckner, N.; Baumgartner, J.; Vyssoki, S.; Vyssoki, B. Seasonality in bipolar disorder: Effect of sex and age. J Affect Disord 2019, 243, 322–326. [Google Scholar] [CrossRef]
- Medici, C.R.; Vestergaard, C.H.; Hadzi-Pavlovic, D.; Munk-Jørgensen, P.; Parker, G. Seasonal variations in hospital admissions for mania: Examining for associations with weather variables over time. J Affect Disord 2016, 205, 81–86. [Google Scholar] [CrossRef]
- Liu, L.; Zhang, D.; Rodzinka-Pasko, J.K.; Li, Y.M. Environmental risk factors for autism spectrum disorders. Nervenarzt 2016, 87, 55–61. [Google Scholar] [CrossRef]
- Frye, R.E.; Cakir, J.; McCarty, P.J.; Rose, S.; Delhey, L.M.; Palmer, R.F.; Austin, C.; Curtin, P.; Yitshak-Sade, M.; Arora, M. Air Pollution and Maximum Temperature Are Associated with Neurodevelopmental Regressive Events in Autism Spectrum Disorder. J Pers Med 2022, 12. [Google Scholar] [CrossRef]
- Botsas, G.; Koidou, E.; Chatzinikolaou, K.; Grouios, G. Environmental Influences on Individuals with Autistic Spectrum Disorders with Special Emphasis on Seasonality: An Overview. Children (Basel) 2023, 10. [Google Scholar] [CrossRef]
- Upthegrove, R.; Marwaha, S.; Birchwood, M. Depression and Schizophrenia: Cause, Consequence, or Trans-diagnostic Issue? Schizophr Bull 2017, 43, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Della, D.F.; Allison, S.; Bidargaddi, N.; Wa, S.K.; Bastiampillai, T. An Umbrella Systematic Review of Seasonality in Mood Disorders and Suicide Risk: The Impact on Demand for Primary Behavioral Health Care and Acute Psychiatric Services. Prim Care Companion CNS Disord 2023, 25. [Google Scholar] [CrossRef]
- Zhang, R.; Volkow, N.D. Seasonality of brain function: role in psychiatric disorders. Transl Psychiatry 2023, 13, 65. [Google Scholar] [CrossRef] [PubMed]
- Kidd, P. Th1/Th2 balance: the hypothesis, its limitations, and implications for health and disease. Altern Med Rev 2003, 8, 223–246. [Google Scholar] [PubMed]
| General Information | Preliminary Questions | Masking Seasonality | Symptom characteristics considering seasonality and individual weather factors |
|---|---|---|---|
| Age | Is the course of the illness fluctuating so far? | Recent events, typically observed in a given season and associated with social impact | General characteristics of the exacerbation and course of the illness: Intensification, symptom alleviation, treatment attempts |
| Gender | How many previous hospitalizations were there and in which season or time of year? | Since when and what medications or substances are being taken? | What is the patient’s daily rhythm? |
| Reason for hospitalization | Has a difference in clinical presentation been observed in different seasons? | Is the patient’s schedule regular, e.g., 8-hour workdays, or variable? | Does the patient take vitamin D? |
| Diagnosed Condition | Is there a specific season that seems particularly difficult for the patient? | Does the patient actively use other forms of treatment? | How does the patient assess their sleep? How many hours do they sleep? Do they work remotely or outdoors? |
| Are there any global events (e.g., war) that might have been overlooked but significantly impact the patient? | Recent Endocrine Problems: menopause, PMS, thyroid issues, and others. Other chronic illnesses. | Has the patient used fototherapy, and with what result? | |
| What conditions does the patient experience at home and work? (cold, humidity, wind, light exposure) | How does the patient assess the air quality where they live? | ||
| Has the patient recently returned from traveling to another country or climate zone? Have they recently spent time near water? | How does the patient assess their immunity? | ||
| What is the patient’s level of physical activity? | Does the patient suffer from allergies or allergic diseases | ||
| Does the patient have parasites? | |||
| What is the patient’s residence (considering distance to water bodies, pollution, presence of allergens, etc.) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





