Submitted:
20 December 2024
Posted:
23 December 2024
You are already at the latest version
Abstract
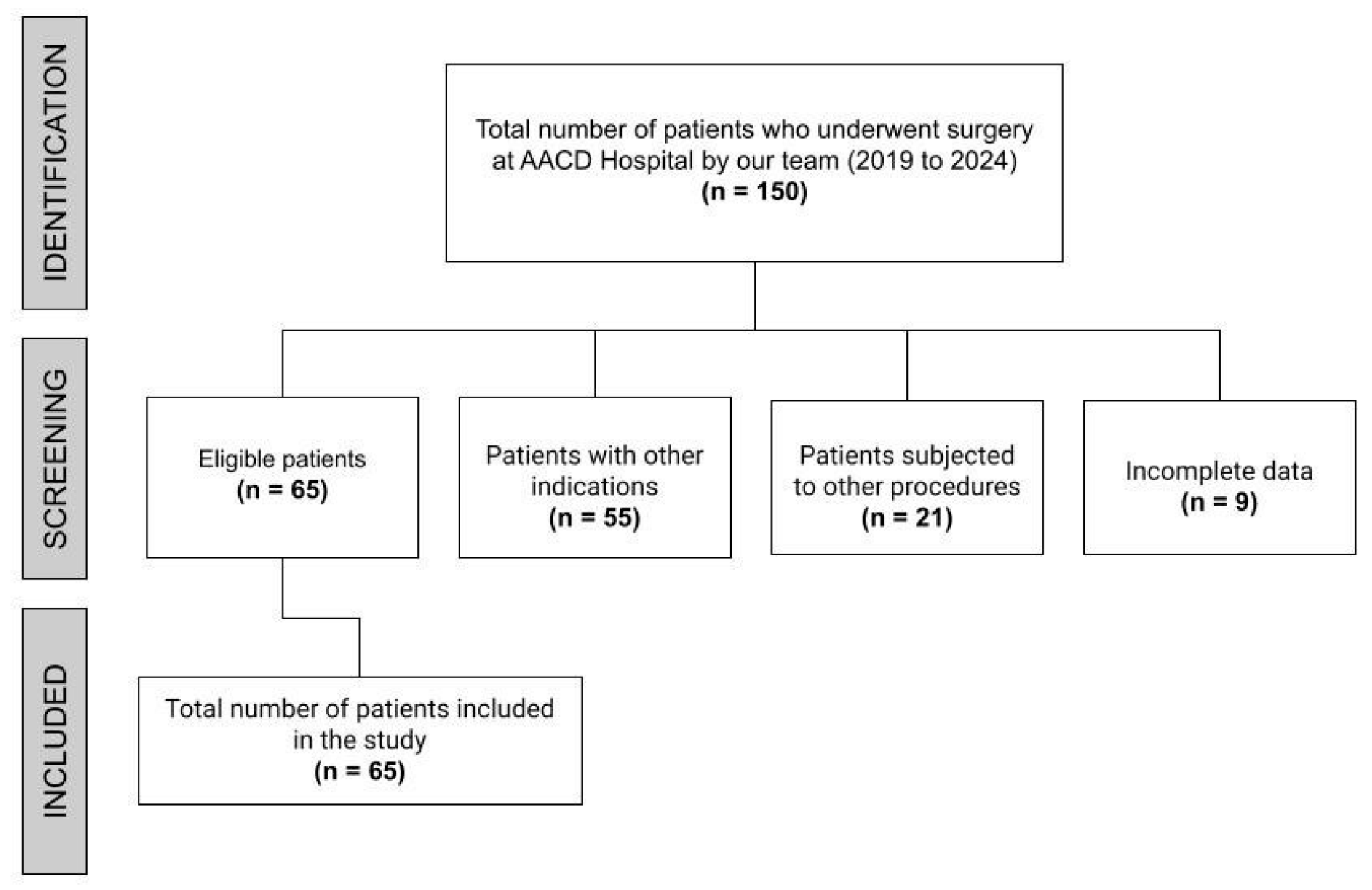
Introduction: To compare intraoperative and short-term postoperative outcomes of patients with recurrent lumbar disc herniation undergoing ALIF Stand-Alone, ALIF 360°, or Arthroplasty. Methods: This retrospective cohort study was conducted at a single center from August 2019 to January 2024. Inclusion criteria included patients over 18 years diagnosed with recurrent lumbar disc herniation undergoing ALIF Stand-Alone, ALIF 360°, or Arthroplasty. Exclusion criteria were incomplete data or other indications. Data collected included demographics, surgical specifics (procedure type, operated levels, graft type, incision type), and clinical outcomes (intraoperative morbidity and short-term postoperative outcomes). Results: Sixty-five patients were evaluated. No intraoperative complications occurred in any group. Average operative times were 165.8 ± 61.72 minutes for ALIF Stand-Alone, 236.25 ± 46.3 minutes for ALIF 360°, and 98.43 ± 45 minutes for Arthroplasty (p < 0.0001). The average postoperative hospital stay was 2.46 ± 1.14 days, with no significant difference between groups (p = 0.515). Postoperative complications were minimal: one surgical site infection in the ALIF Stand-Alone group (p = 0.444) and four instances of sympathetic changes (p = 0.477). Conclusion: There was no significant difference in intraoperative morbidity, short-term postoperative outcomes, or length of stay among the three groups. All techniques demonstrated good results with low morbidity and short hospitalization times post-procedure, suggesting that the choice of technique should be based on the surgeon's experience and the patient's condition and preferences.
Keywords:
Introduction
Material and Methods
Study Design
Ethical Considerations
Study Population
Inclusion and Exclusion Criteria
Data Collection
Subgroup Analysis
Surgical Technique
Statistical Analysis
Results
Demographic Data
Complaint
Operated Levels
Incision and Graft Type
Details of the Outcomes
Subgroup Analysis
Discussion
Perioperative Complications
Operative Time
Length of Hospital Stay
Strengths and Limitations
Conclusions
Funding
Conflicts of Interest
References
- Bogduk, N. Functional anatomy of the spine. Handbook of Clinical Neurology. 2016;136:675–88.
- Ruben Ngnitewe Massa, Mesfin FB. Disc Herniation [Internet]. Nih.gov. StatPearls Publishing; 2023.
- Yao M, Xu B, Li Z, Zhu S, Tian Z, Li D, et al. A comparison between the low back pain scales for patients with lumbar disc herniation: validity, reliability, and responsiveness. Health and Quality of Life Outcomes [Internet]. 2020 Jun 10;18.
- Silvinato A, Simões RS, Buzzini RF, Bernardo WM. Lumbar herniated disc treatment with percutaneous hydrodiscectomy. Revista da Associação Médica Brasileira. 2018 Sep;64(9):778–82.
- Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. The Journal of Bone and Joint Surgery American Volume [Internet]. 2003 Jan 1;85(1):102–8.
- Wera GD, Marcus RE, Ghanayem AJ, Bohlman HH. Failure within One Year Following Subtotal Lumbar Discectomy. The Journal of Bone and Joint Surgery-American Volume. 2008 Jan;90(1):10–5.
- Rogers, LA. Experience with limited versus extensive disc removal in patients undergoing microsurgical operations for ruptured lumbar discs. Neurosurgery [Internet]. 1988 Jan 1;22(1 Pt 1):82–5.
- O’Sullivan MG, Connolly AE, Buckley TF. Recurrent lumbar disc protrusion. British Journal of Neurosurgery [Internet]. 1990;4(4):319–25.
- Lebow RL, Adogwa O, Parker SL, Sharma A, Cheng J, McGirt MJ. Asymptomatic Same-Site Recurrent Disc Herniation After Lumbar Discectomy. Spine. 2011 Dec;36(25):2147–51.
- Ebeling U, Kalbarcyk H, Reulen HJ. Microsurgical reoperation following lumbar disc surgery. Journal of Neurosurgery. 1989 Mar;70(3):397–404.
- Pradhan BB, Nassar JA, Delamarter RB, Wang JC. Single-Level Lumbar Spine Fusion: A Comparison of Anterior and Posterior Approaches. Journal of Spinal Disorders & Techniques. 2002 Oct;15(5):355–61.
- Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. Journal of Spine Surgery [Internet]. 2015 Dec 1;1(1):2–18.
- Vadim Goz, Weinreb JC, Schwab FJ, Virginie Lafage, Errico TJ. Comparison of complications, costs, and length of stay of three different lumbar interbody fusion techniques: an analysis of the Nationwide Inpatient Sample database. 2014 Sep 1;14(9):2019–27.
- Ahlquist S, Thommen R, Park HY, Sheppard W, James K, Lord E, et al. Implications of sagittal alignment and complication profile with stand-alone anterior lumbar interbody fusion versus anterior posterior lumbar fusion. Journal of Spine Surgery. 2020 Dec;6(4):659–69.
- Vadim Goz, Weinreb JC, Schwab FJ, Virginie Lafage, Errico TJ. Comparison of complications, costs, and length of stay of three different lumbar interbody fusion techniques: an analysis of the Nationwide Inpatient Sample database. 2014 Sep 1;14(9):2019–27.
- Gamradt SC, Wang JC. Lumbar disc arthroplasty. The Spine Journal. 2005 Jan 1;5(1):95–103.
- Sandhu FA, Dowlati E, Garica R. Lumbar Arthroplasty: Past, Present, and Future. Neurosurgery. 2019 Nov 14.
- Mobbs RJ, Phan K, Daly D, Rao PJ, Lennox A. Approach-Related Complications of Anterior Lumbar Interbody Fusion: Results of a Combined Spine and Vascular Surgical Team. Global Spine Journal. 2015 Jul 16;6(2):147–54.
- Comer GC, Smith MJ, Hurwitz EL, Mitsunaga KA, Kessler R, Carragee EJ. Retrograde ejaculation after anterior lumbar interbody fusion with and without bone morphogenetic protein-2 augmentation: a 10-year cohort controlled study. The Spine Journal. 2012 Oct 1;12(10):881–90.
- Garg J, Woo K, Hirsch J, Bruffey JD, Dilley RB. Vascular complications of exposure for anterior lumbar interbody fusion. Journal of Vascular Surgery. 2010 Apr;51(4):946–50.
- Mahoney JR, Barnes D, Pahl D. Perforated ileus after L5-S1 anterior lumbar interbody fusion: a case report presentation. AME Case Reports. 2019 Jul;3:21–1.
- Phan K, Lackey A, Chang N, Ho YT, Abi-Hanna D, Kerferd J, et al. Anterior lumbar interbody fusion (ALIF) as an option for recurrent disc herniations: a systematic review and meta-analysis. Journal of Spine Surgery. 2017 Dec;3(4):587–95.
- STROBE. STROBE – Strengthening the Reporting of Observational Studies in Epidemiology [Internet]. STROBE. 2023. Available from: https://www.strobe-statement.org/.
- Luo L, Li L, Hu J, Wang X, Hou B, Zhang T, et al. A hybrid solution for extracting structured medical information from unstructured data in medical records via a double-reading/entry system. BMC Medical Informatics and Decision Making. 2016 Aug 30;16(1).
- Mobbs RJ, Loganathan A, Yeung V, Rao PJ. Indications for Anterior Lumbar Interbody Fusion. Orthopaedic Surgery. 2013 Aug;5(3):153–63.
- Sandhu FA, Dowlati E, Garica R. Lumbar Arthroplasty: Past, Present, and Future. Neurosurgery. 2019 Nov 14.
- Li Y, Sun P, Chen D, Tang L, Chen C, Wu A. Artificial total disc replacement versus fusion for lumbar degenerative disc disease: an update systematic review and meta-analysis. Turkish Neurosurgery. 2018.
- Silva GM da, Rodrigues LMR, Lopes FA, Cesar AEM. QUALITY OF LIFE ANALYSIS ON PATIENTS AFTER ARTHROPLASTY OR LUMBAR ARTHRODESIS. Coluna/Columna [Internet]. 2023 Apr 17 [cited 2023 Sep 12];22:e262320.
- Guyer RD, McAfee PC, Banco RJ, Bitan FD, Cappuccino A, Geisler FH, et al. Prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITÉ artificial disc versus lumbar fusion: Five-year follow-up. The Spine Journal. 2009 May;9(5):374–86.
- Berg S, Tullberg T, Branth B, Olerud C, Tropp H. Total disc replacement compared to lumbar fusion: a randomised controlled trial with 2-year follow-up. European Spine Journal. 2009 Jun 9;18(10):1512–9.
- Holt RT, Majd ME, Isaza JE, Blumenthal SL, McAfee PC, Guyer RD, et al. Complications of Lumbar Artificial Disc Replacement Compared to Fusion: Results From the Prospective, Randomized, Multicenter US Food and Drug Administration Investigational Device Exemption Study of the Charité Artificial Disc. International Journal of Spine Surgery. 2007;1(1):20–7.
- Christensen, FB. Lumbar spinal fusion. Outcome in relation to surgical methods, choice of implant and postoperative rehabilitation. Acta Orthopaedica Scandinavica Supplementum [Internet]. 2004 Oct 1;75(313):2–43.
- Amato V, Giannachi L, Irace C, Corona C. Accuracy of pedicle screw placement in the lumbosacral spine using conventional technique: computed tomography postoperative assessment in 102 consecutive patients. Journal of Neurosurgery: Spine. 2010 Mar;12(3):306–13.
- Fan S, Hu Z, Zhao F, Zhao X, Huang Y, Fang X. Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus conventional open approach. European Spine Journal. 2009 Oct 30;19(2):316–24.
- Strube P, Hoff E, Hartwig T, Perka CF, Gross C, Putzier M. Stand-alone Anterior Versus Anteroposterior Lumbar Interbody Single-level Fusion After a Mean Follow-up of 41 Months. Journal of Spinal Disorders & Techniques. 2012 Oct;25(7):362–9.
- Wei J, Song Y, Sun L, Lv C. Comparison of artificial total disc replacement versus fusion for lumbar degenerative disc disease: a meta-analysis of randomized controlled trials. International Orthopaedics. 2013 May 4;37(7):1315–25.
- Zigler JE, Delamarter RB. Five-year results of the prospective, randomized, multicenter, Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential arthrodesis for the treatment of single-level degenerative disc disease. Journal of Neurosurgery: Spine. 2012 Dec;17(6):493–501.
- Udby PM, Bech-Azeddine R. Clinical outcome of stand-alone ALIF compared to posterior instrumentation for degenerative disc disease: A pilot study and a literature review. Clinical Neurology and Neurosurgery. 2015 Jun;133:64–9.
- Ho VT, Martinez-Singh K, Colvard B, Lee JT, Chandra V. Increased vertebral exposure in anterior lumbar interbody fusion associated with venous injury and deep venous thrombosis. Journal of Vascular Surgery: Venous and Lymphatic Disorders. 2020 Aug.
- Shultz BN, Wilson AT, Ondeck NT, Bovonratwet P, McLynn RP, Cui JJ, et al. Total Disc Arthroplasty Versus Anterior Interbody Fusion in the Lumbar Spine Have Relatively a Few Differences in Readmission and Short-term Adverse Events. Spine [Internet]. 2018 Jan 1;43(1):E52–9.
- Kim JS, Kim DH, Lee SH, Park CK, Jang Yeon Hwang, Cheh G, et al. Comparison Study of the Instrumented Circumferential Fusion with Instrumented Anterior Lumbar Interbody Fusion as a Surgical Procedure for Adult Low-Grade Isthmic Spondylolisthesis. 2010 May 1;73(5):565–71.
- Kobayashi K, Ando K, Kato F, Kanemura T, Sato K, Hachiya Y, et al. Predictors of Prolonged Length of Stay After Lumbar Interbody Fusion: A Multicenter Study. Global Spine Journal. 2018 Sep 13;9(5):466–72.
- McGirt MJ, Parker SL, Chotai S, Pfortmiller D, Sorenson JM, Foley K, et al. Predictors of extended length of stay, discharge to inpatient rehab, and hospital readmission following elective lumbar spine surgery: introduction of the Carolina-Semmes Grading Scale. Journal of Neurosurgery Spine [Internet]. 2017 Oct 1 [cited 2020 Dec 13];27(4):382–90.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




