1. Introduction
Chronic respiratory diseases, including asthma, affect millions of people worldwide. Asthma symptoms include breathing difficulty, wheezing, coughing, and chest tightness. In severe cases, it can result in hospitalisation or even death. Asthma also impairs the quality of life of patients, their families, and their caregivers. For instance, New Zealand faces a particularly serious asthma challenge, with about one-eighth of its population (or over 597,000 people) suffering from the disease [
1,
2]. The country has a high incidence of asthma among children, who account for the majority of hospitalisations due to asthma [
3]. Furthermore, asthma disproportionately affects native Māori and Pacifica people, who experience higher rates of hospitalisation and mortality from asthma and other respiratory diseases than other ethnic groups. Besides, asthma imposes a significant negative economic impact on the national economy costing about
$7 billion per year in direct and indirect expenses [
3].
Asthma is a chronic condition that demands continuous management and education for patients. In many cases, people with asthma lack adequate knowledge to control the disease symptoms. Often, they also fail to use portable medication application devices (so-called inhalers) properly or consistently [
1]. The main purpose of the inhaler is to deliver aerosol medication to the lungs. The use of a correct application technique is required to make the application effective. Indeed, improper application of the inhaler could lead to aggravating asthma conditions. This ultimately negatively affects the treatment efficiency and leads to higher cost [
4,
5,
6]. Notably, the misuse of inhaler devices in clinical practice was reported to be independent of patients’ clinical or functional characteristics.
Inhaler misuse is often caused by deficiencies of relevant knowledge, incorrect interpretation of printed instructions, and users’ training by healthcare professionals. The correctness of the employed inhaler technique should be regularly verified and reinforced. However, this is frequently impractical in clinical settings. This issue can be addressed by incorporating relevant sensing, evaluation, monitoring, and feedback facilities within inhalers themselves or as add-ons thus making them smart devices (e.g., see
Figure 1). Among other functions,
smart inhalers can gather usage data and indicate whether the inhaler is being used correctly. However, most smart inhalers in the market only record the time and date of medication intake without evaluating the quality of the inhalation in detail [
7,
8]. The inhalation quality largely depends on the inhalation flowrate, which is the volume of air-medication mixture that flows through the inhaler per unit of time (usually measured in
litres per minute or
l/m). Therefore, a consistent inhalation flowrate for a certain duration of time is crucial to the optimal depositing of the medication in the lungs.
Several smart inhalers and add-on devices are available on the market, offering various functionalities such as tracking and logging medication usage, providing reminders for medication intake, etc. There are also literature reviews covering various aspects of smart inhaler research, technology, and implementation, e.g., [
11,
12,
13,
14]. This paper provides an additional contribution to the body of knowledge in the field. To the best of the authors’ knowledge, it offers the first review study focusing specifically on smart inhalers having flowrate sensing and measurement capability. It underlines the significance of inhalation flowrate measurement and control, investigates the current progress in the field, and identifies promising directions for future research and development.
2. Inhalation Flowrate
The right flowrate is crucial for patients with asthma and
Chronic Obstructive Pulmonary Disease (COPD) as it determines the delivery and deposition of inhaled medications [
15,
16,
17]. Insufficient inhalation flowrate leads to lower drug emissions. It is particularly relevant for
Dry Powder Inhalers (DPIs). In [
18], the authors emphasized that different inhalers, such as
Pressurised Metered-Dose Inhalers (pMDIs) and DPIs, need different inhalation flowrates to deliver the drug effectively. Different inhalers were used to examine the
Peak Inspiratory Flowrate (PIFR) at different levels of device resistance. It was found that a significant number of patients could not reach the minimum or optimal PIFR for DPIs. A similar result was observed in the study [
19]. Another study [
20] compared the performance of six different DPIs (3 types each of 2 strength levels) and found that the fine particle dose flowrate dependence was similar for all inhalers. A new metric to measure the flowrate dependence on lung dose was proposed in a detailed review of DPIs [
21]. Among others, the study showed that lung dose depended more on the formulation and device characteristics than on the flowrate. The authors claimed that with changes in formulation and/or device characteristics, passive DPIs could deliver the drug regardless of inhalation technique. The literature review [
6] highlighted the differences in optimal inhalation techniques among inhalation devices. It noticed that healthcare providers should be sure their patients are capable of achieving the required inhalation flowrate, which could vary for device types and models. For instance, it was shown in [
22] that in some cases low-resistance DPIs could achieve higher and more consistent lung deposition than high-resistance DPIs. It suggested that low-resistance DPIs might be more suitable for COPD patients of different severities.
On the other hand, reducing inhalation airflow may also have a positive effect in some cases. As it was noted in [
23], too high aerosol speed from a pMDI or too high inhalation flows from some DPIs may cause excessive droplet deposition in the oropharynx and lower lung regions. In [
24], the authors compared the inhalation dosimetry in the respiratory tract for five breathing depths. They observed significant differences in airflow dynamics and deposition distribution in the oral cavity. The inhalation depth was positively correlated with the mouth deposition and negatively correlated with the small airway deposition. The optimal delivery efficiency to small airways was achieved at quite low flowrate and decreased with higher inhalation depths.
The size, speed, and behaviour of the aerosol droplets or particles that carry the drug are also affected by the inhalation flowrate. This influences how deep particles can penetrate into the lungs and where they can be deposited. In [
25], a computational fluid dynamics model was developed to characterise aerosol flow from a pMDI into a simulated mouth-throat geometry and to analyse the effects of air flowrate and cone angle. The model showed that increasing flowrate had various effects, such as particle deagglomeration and throat particle deposition reduction. The model also indicated that particle deposition depended more on the initial cone angle than on the flowrate and that an 8-degree cone angle was optimal for the lowest mouth–throat deposition. Another study [
26] confirmed in vivo that the total and regional lung depositions were determined by the particle size of the aerosol and the inhalation flowrate, rather than the device resistance.
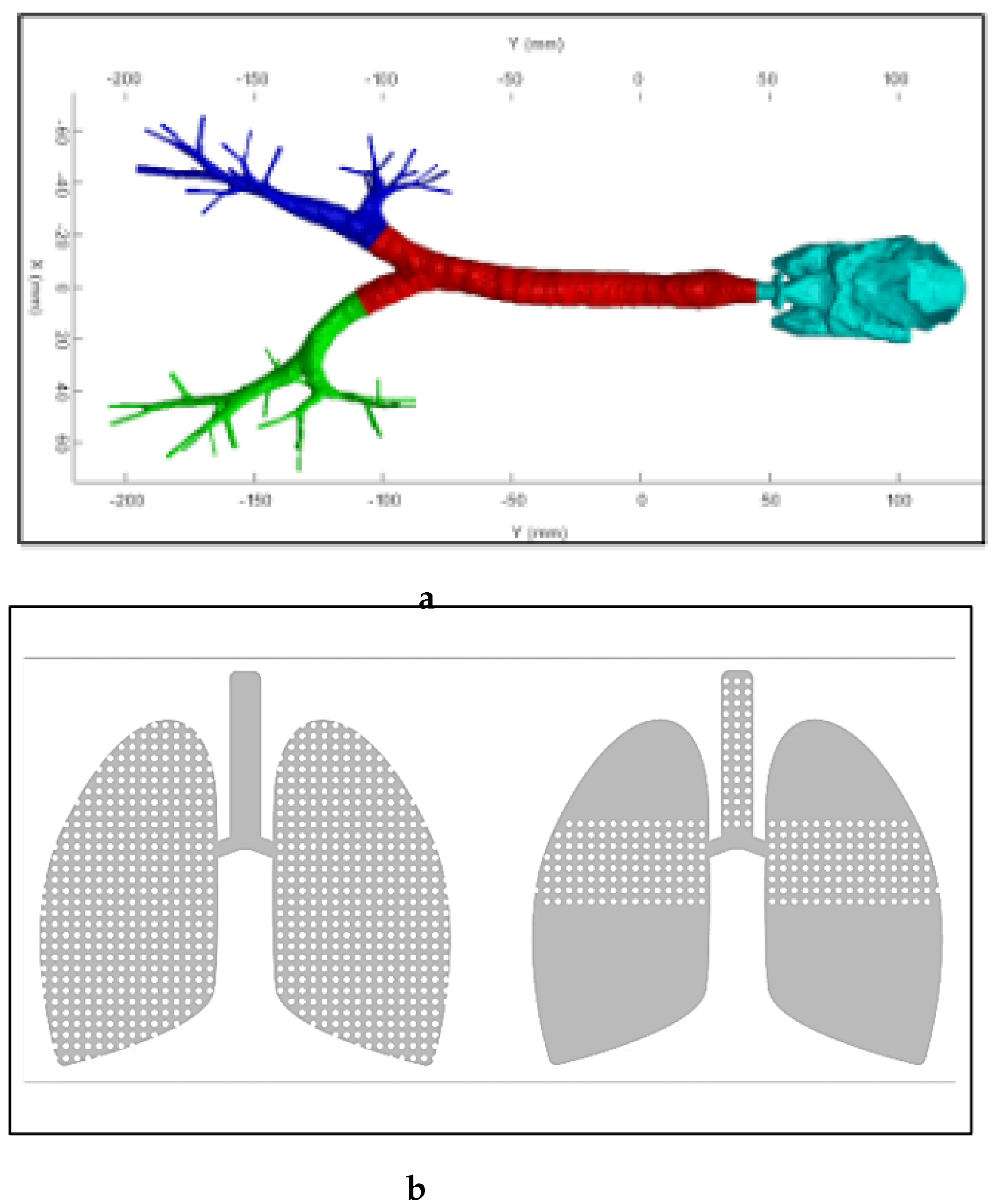
Following the deposition topic, in [
27] the authors used a model based on a realistic geometry of the human airways derived from computed tomography (see
Figure 2, a) to study the effects of various factors on the deposition. They discovered that higher inhalation flowrate increased the turbulence and the particle deposition in the main bronchi, especially for larger particles. It was also observed that impaction was the dominant deposition mechanism for larger particles at higher flowrates, rather than electrostatic deposition.
The timing of drug release is also crucial for optimal lung deposition, as the drug must be dispensed within the best window of the inhalation cycle [
28] (see
Figure 2, b). The article highlighted the importance of determining the inhalation flowrate profile, as it enables the estimation of key inhalation parameters such as inhalation depth and duration, exhalation before inhalation, and lung function.
Figure 2.
(
a) Realistic geometry of human upper airways [
27]; (
b) Deposition for medicine release in the optimal window (left) vs late release (right) [
29].
Figure 2.
(
a) Realistic geometry of human upper airways [
27]; (
b) Deposition for medicine release in the optimal window (left) vs late release (right) [
29].
Study [
30] clarified that the main parameter for DPI performance was not PIFR but the negative pressure generated by the patient’s inhalation effort. The authors investigated factors influencing the inspiratory pressures and flowrates along with dispensing and dispersion characteristics of different DPIs. They discovered that inspiratory pressures (not flowrates) constrained and regulated the patient’s ability to generate enough flow for effective DPI use. The article also emphasised that employed inhalers had different operating mechanisms and resistances.
The inhalation flowrate is a significant factor determining the efficacy and safety of inhalation therapy. However, many patients with asthma and COPD cannot achieve a suitable inhalation flowrate for their inhalers, especially during acute exacerbations. This may result in suboptimal therapy and poor clinical outcomes [
18]. As shown in [
31] and [
32], inhaler mishandling is still a major clinical issue. Moreover, it was reported in [
19] that changing the inhaler type was sometimes associated with an increase in the number of errors. Inhalation techniques should be taught and practised to help patients to optimise their inhalation therapy. However, compliance with the correct technique declines over time [
33] implying the high value of regular assessment and monitoring. It is important to mention that clinical practice is not the only way to train patients. For instance, an in-vivo study [
34] showed the effectiveness of using inhaler add-on devices with smartphone applications for adults. Such devices enhance the pMDI inhalation technique through audio-visual feedback thus leading to improved salbutamol delivery to the lungs. Besides, it was shown that slowing the inhalation step was strongly associated with the amount of medicine that reached the lungs and excreted in the urine.
3. Inhalation Technique Training
Various simulators are available on the market and employed in medical practice to train patients to correctly regulate inspiratory flowrate. Such training devices do not require relevant medical authority approvals as they are not intended to be used for medication delivery purposes. Several review studies of different training devices and their efficiency were conducted, e.g., [
23,
35]. This section focuses on the devices that aim to real-time control inhalation flowrate. The goal is to identify potential areas for improvement. The section excludes bulky
spirometers or
Aerosol Inhalation Monitors (AIM) used in hospitals, as they are not pertinent to the current topic of portable inhaler devices for routine use.
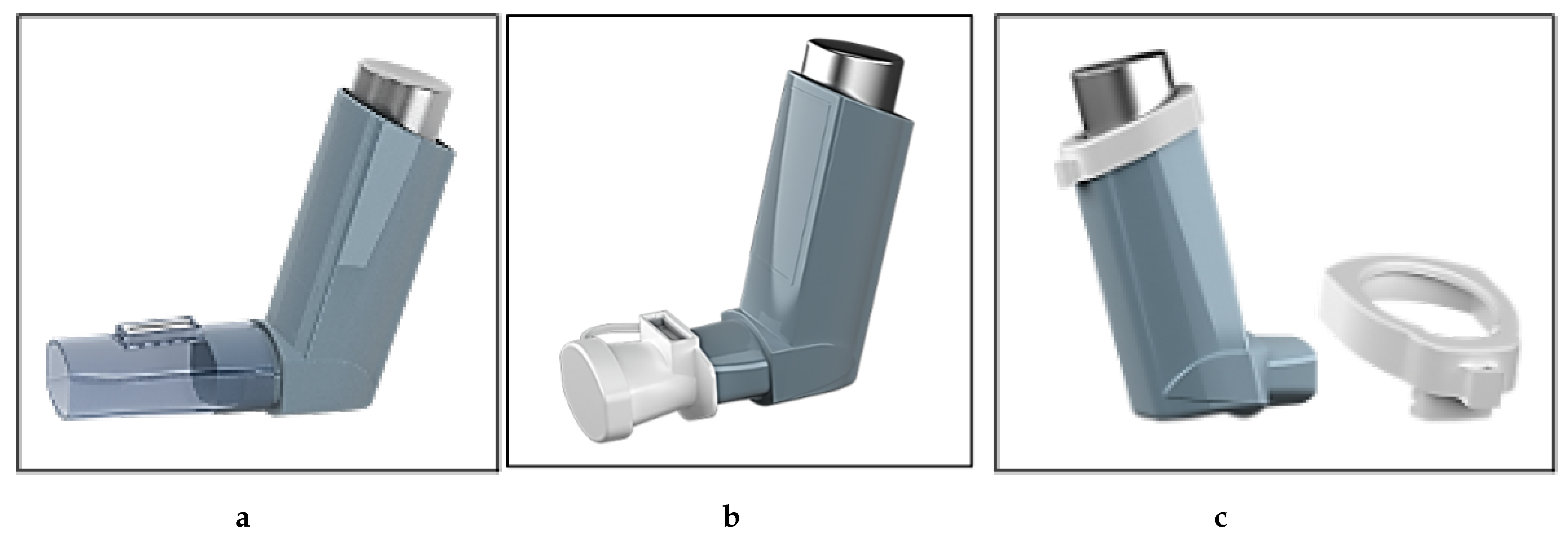
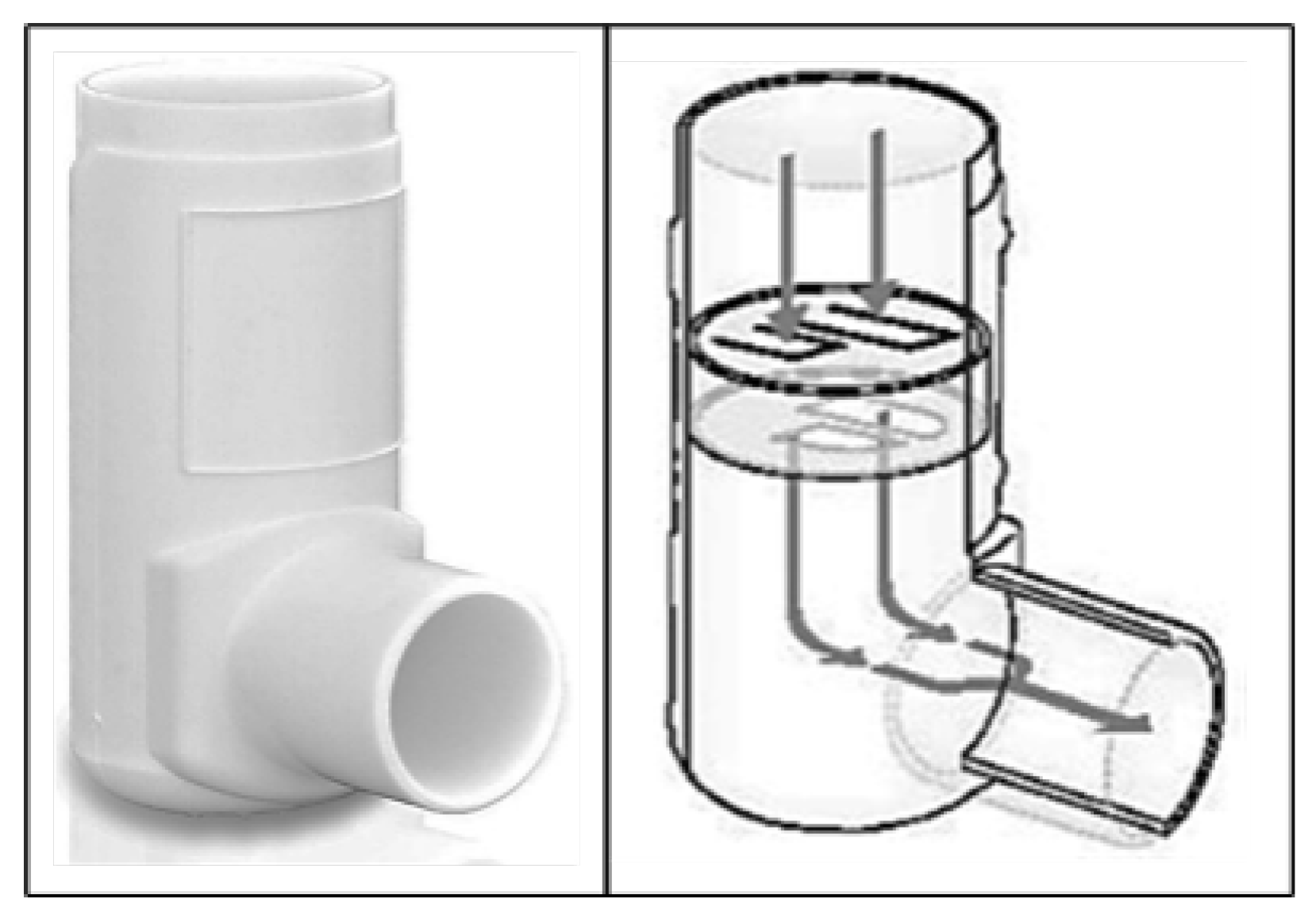
3.1. 2Tone Inhaler Trainer
The
2Tone Inhaler Trainer is a commercially available device that teaches patients how to use their MDIs correctly. The device resembles a real MDI in shape and feel. It does not contain any medication canister (see
Figure 3) as it is employed for training only. The design of the device is simple. It emits sounds (tones) depending on the speed of inhaling. Silence indicates too slow breathing. The presence of two different tones indicates too fast breathing while the advent of just one tone indicates optimal breathing. According to the online brochure, practising with the sound feedback device enables patients to quickly learn to adjust their inhalation speed and improve their inhaler technique [
36]. As a result, patients should get used to breathing through their real inhaler deeply at the right speed.
Just a few studies are available on the effectiveness of the
2Tone Inhaler Trainer, e.g., [
37,
38,
39,
40]. The studies concur that the
2Tone trainer can improve the inhalation technique by helping to maintain a slow inhalation rate when using an MDI. They also report increased asthma patients’ satisfaction and improved confidence with their inhaler use. The study [
41] compared the efficacy of using the
2Tone device with only verbal training for achieving a slow inhalation flow. The study shows that the
2Tone device has an advantage over verbal training and positively impacts the patient inhalation technique. However, it is noteworthy that the device is based on using a sound signal, which could be inconvenient for regular use and unsuitable for deaf or hearing-impaired patients.
Figure 3.
2Tone Inhaler Trainer [
36,
39].
Figure 3.
2Tone Inhaler Trainer [
36,
39].
3.2. Clement Clarke pMDI Add-Ons
Medical supplier company
Clement Clarke offers several inhaler commercially available add-on devices that help patients improve their inhaler technique for pMDI by optimizing their inhalation flowrate [
42]. All the devices have a similar functionality.
The first device is
Flo-Tone, a trainer that helps patients to achieve the correct flowrate and coordinate actuation. The device can be attached to the mouthpiece of a placebo pMDI (see
Figure 4, a) or
Trainhaler, which is a mock pMDI enclosure with a canister pressing imitation.
Flo-Tone has an integrated whistle that produces a sound when the patient reaches the target inspiratory flowrate. After actuation, the whistle helps to maintain a slow inhalation to deliver the medication to the lungs. For a better experience, the device can be used with the “
Trainhaler Buddy” mobile application. It recognises the whistling sound and provides real-time feedback with graphical visualisation. This helps patients to see if they have achieved the optimal inhalation technique and the duration of inhalation in seconds. It is important to note that the device has low accuracy. The device can be attached to a regular pMDI. However, using it only with a placebo pMDI or
Trainhaler is recommended. This might be because the effect of the whistle by-pass channel might influence inhalation outcomes such as aerosol droplet size and deposition.
The second device is
Flo-Tone CR, which is an upgraded version of the previous device (see
Figure 4, b). It has a built-in
Controlled Resistance (CR) that eliminates the inhaler’s internal resistance variability. This enables the device to fit all pMDIs since the whistle indicates the same flowrate regardless of pMDIs’ resistance. It also has a tethered mouthpiece cap. It is claimed that using the device as a spacer enhances drug delivery and reduces unwanted oropharyngeal deposition.
Another add-on device aiming to improve inhaler technique is
Clip Tone E (see
Figure 4, c). It has a different design, but the same functionality and purpose as the above-described devices. It produces a whistle when the user inhales slowly and steadily. Instead of the mouthpiece, it fits around the pMDI canister at the top of the inhaler enclosure. This design prevents the add-on from affecting medication delivery, as it is away from the medicine injection path. However, the device has a limited use, as it is compatible only with a few specific models of pMDI.
The efficacy of
Trainhaler and
Flo-Tone CR training devices is assessed in [
46]. The study involved 64 asthmatic patients on pMDI therapy for at least a month. They exhibited a poor pMDI technique including too fast inhalation flowrate. The results indicate that
Trainhaler and
Flo-Tone CR enabled enhanced inhalation with effective flowrate control. The devices also allow the patients to practice at their own pace and time.
The broader study [
47] employs
Trainhaler combined with
Flo-Tone to examine the effectiveness of the inhalation technique training. It involved 304 adult asthma patients divided into two groups (intervention and base). The patients of the intervention group utilized the inhalation technique three times with a one-month gap between each performance. At each visit, their pulmonary function and inhalation technique were assessed. This is then followed with feedback and guidance on the correct technique application. The intervention group showed a significant reduction in the frequency of the crucial errors one visit earlier compared to the base group subjected to just verbal counselling.
The effect of advanced patient consulting supported by two similar devices and a smartphone application is examined in [
48]. The study engaged 100 children - asthma patients. The pMDI was used together with a whistling device and inhalation spacer - a transparent chamber fit between the inhaler and the mouthpiece. The spacer allows monitoring of the intake and see if all the medication is inhaled. The whistling devices included the
Flo-Tone and a facemask with a built-in whistle tone that could be detected by the
Trainhaler smartphone application (see
Figure 5). The patients were assigned into two groups based on the type of training device they used. The study evaluated the inhalation technique three times having one-month intervals. After each evaluation, the patients received a training session. The results showed a significant reduction in the number of mistakes for both groups. However, the
Flo-Tone-associated group achieved the desired increase in inhalation duration earlier. The facemask-associated group experienced difficulties in developing the proper technique, especially among the younger patients.
The study [
49] provides a comparison of traditional verbal consulting and the advanced method employing the
Flo-Tone with the mobile application. In total, 201 asthmatic children were randomly assigned to two groups (control and advanced). They demonstrated their inhalation technique three times at one-month intervals and received a training session after each demonstration. The advanced group exhibited a faster and greater decrease in the number of mistakes and an increase in inhalation duration than the control group. Moreover, the advanced group also displayed a higher and quicker improvement in lung function than the control group. The authors noted that the combination of traditional (verbal) and advanced consulting methods led to significant enhancements in inhalation technique and duration compared to using only traditional verbal consulting. The study is replicated in [
50] with a smaller number of subjects while yielding similar findings.
The effectiveness of advanced consulting of adult subjects is discussed in [
51].
Flo-Tone CR and
Clip-Tone E were used with a smartphone application. The outcome was compared with the results of the regular inhaler training. Twelve healthy adult volunteers participated in a cross-over study. They were trained to use: 1) pMDI alone, 2) pMDI with the
Clip-Tone E add-on, and 3) pMDI with the
Flo-Tone CR add-on. They received guiding materials and personal training for each device. The participants used each device twice during a session. The amounts of medicine delivered during inhalation were estimated by urine samples taken 30 minutes past inhalation. The results revealed that the use of the add-on devices led to a significant increase in the concentration of the medicine in the urine samples compared to using the pMDI alone. At the same time, no significant differences were registered 24 hours after the inhalation. Overall, the study concluded that the advanced methods significantly enhanced the inhalation technique for adults.
The above-presented findings are confirmed in [
34]. The study followed the same pattern but with a larger number of subjects (316 asthma patients). The patients were split into three groups. Two of them used the add-on devices while the last one - the pMDI alone. Each group had three sessions of technique demonstration and training. The results showed that the add-on devices, with their visual and auditory feedback, allowed better engagement of the patients while improving their inhalation technique and lung function. The Flo-Tone CR and Clip-Tone E user groups outperformed the control group significantly in terms of the lower number of mistakes in the technique. However, the authors did not find any significant difference between the efficiency of the two add-on devices.
3.3. DPI Whistling Trainers
Some of the DPIs have mock copies available, such as
Turbuhaler (Turbuhaler Training Device),
Accuhaler (Accuhaler Inhalation Training Device – the same as for
Diskus inhaler),
Ellipta (Ellipta Inhalation Trainer), and others. These trainers have a whistling capability. The whistling is triggered when reaching the target inhalation flowrate. However, the whistle sound is usually quite loud. Thus, it is intended only for training purposes. Unlike the research activity for pMDI, no research on the effectiveness of training devices for DPI was reported in recent years. The results of pMDI-focused studies cannot be generalized to DPI, as they have completely different inhalation flowrates and technique characteristics. This can be attributed to the different flowrate values since DPIs require fast and deep inhalation. A different metric, such as pressure drop [
30], should be used instead of maintaining slow and long inhalation typical for pMDI.
The devices reviewed in this section can improve the inhaler technique and overall treatment outcomes for patients having respiratory diseases. Unfortunately, they have drawbacks requiring attention, such as inconvenience in private use and compatibility with different medications. The choice and use of inhalers still depend on consultation with healthcare providers. This indicates that further research is necessary to design and test new generations of smart devices offering more precise inhalation flowrate measurement and providing personalized feedback to the users.
4. Inhalation Flowrate Measurement
Various products have been developed and implemented to measure and control the inhalation flowrate. This section outlines the most notable of them that utilise acoustic and pressure sensors to enhance inhaler technique and adherence. The state of development, benefits, drawbacks, and commercialisation potential of these devices are discussed.
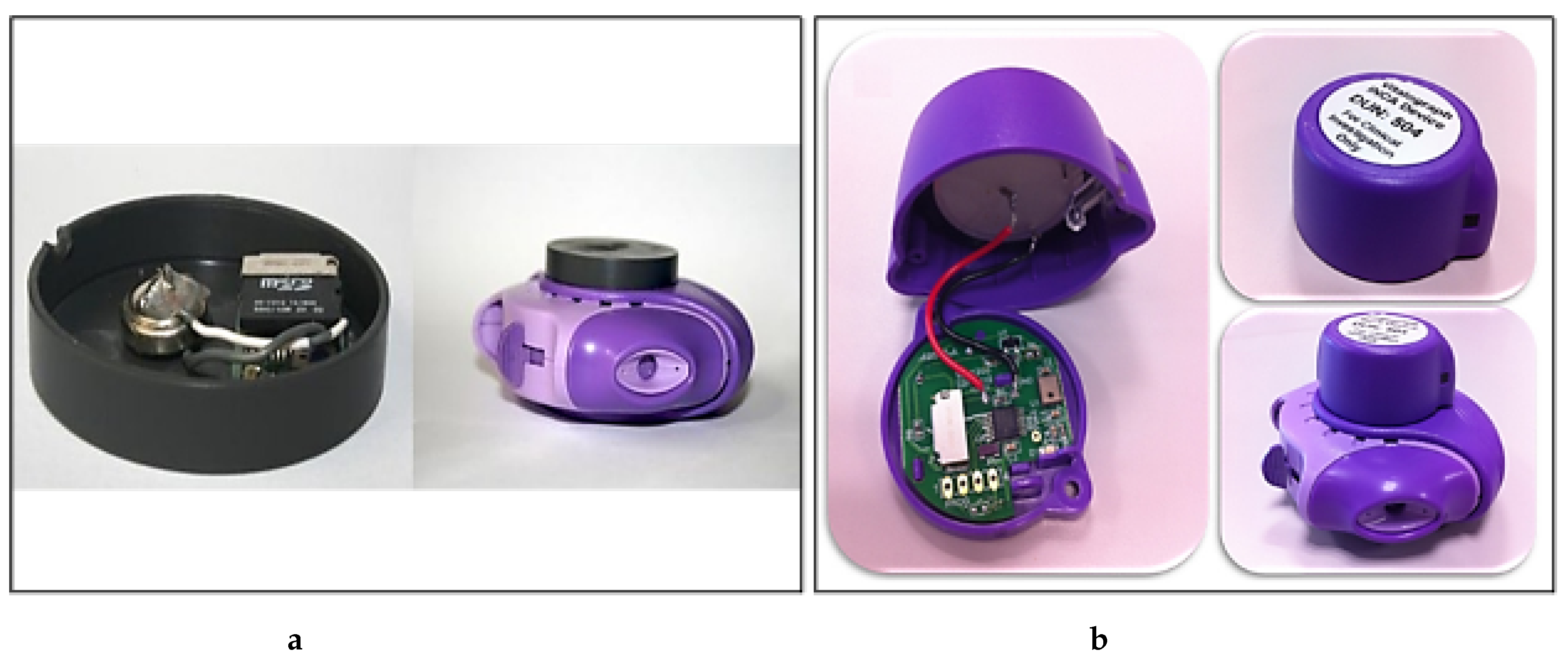
4.1. Inhaler Compliance Assessment Device
A group of Irish researchers conducted a series of studies on the acoustic analysis of DPI use. They developed a device and a method to record and evaluate the sounds produced by DPIs to assess patients’ adherence to the correct inhalation technique. The initial investigation, published in [
52], involved 12 asthma patients who attended a respiratory clinic for three months. An acoustic pickup device (see
Figure 6 (a)) combined with acoustic signal analysis was used to achieve inhalation detection with 89% accuracy. However, the solution faced challenges such as artifact interference and offset time determination due to the flowrate variations at the end of inhalation.
Based on these promising results, the study was extended by taking into account the correlations between flow/volume parameters and the acoustic measurements. The device was named
Inhaler Compliance Assessment (INCA). It is shown in
Figure 6 (b). The main objective of the extended study was to explore the possibility of using acoustic signals to measure the inspiratory flowrate and drug delivery from the DPI. An in-vitro study [
54] was performed using a vacuum pump to simulate different inspiratory efforts. Two more studies [
55,
56] were carried out using volunteers to collect acoustic and flowrate records. It was found that several acoustic parameters had strong correlations with PIFR. Also, an algorithm was proposed for identifying the inhalation and exhalation events with up to 92.8% accuracy. Unlike the earlier research focused only on respiratory sound signals, the reported studies analyzed both the respiratory and inhaler device sounds.
The paper [
53] reports the extension of the study where the PIFR and the
Inspiratory Capacity (IC) were quantitively estimated using the acoustic features of inhalations. Acoustic signals were captured and analysed by the
INCA device. The PIFR was found to correlate with the average power in certain frequency bands and with the amplitude parameters of the inhalation signal, such as median, mean absolute deviation, and root mean square. The results show that the average power in the 300–600 Hz frequency band is strongly correlated with PIFR and IC for the
INCA device with
Diskus. Therefore, the study proved the possibility of employing acoustics to monitor inhaling objectively.
The research was further extended and reported in [
57] and [
58]. The main goal was to discover an objective method to evaluate the inhalation technique without relying on subjective judgments. An algorithm was developed and deployed to automatically detect inhalation from audio signals while providing feedback on patient adherence to the expected technique. It achieved an 83% accuracy rate in evaluating the inhaler technique. The algorithm could identify major critical errors such as exhaling into the mouthpiece, insufficient inhalation force, and multiple inhalations. Also, it enabled the continuous monitoring of patient competency in a home environment, not just in the clinical setting. The extension study is reported in [
59]. A larger group of patients was engaged to examine how the inhalation flowrate and duration affect the aerosol delivery.
The proposed method can be applied to other DPIs (e.g.,
Turbuhaler and
Evohaler) [
60]. The mean acoustic power was found to be the most reliable predictor of PIFR for all inhalers tested. However, some studies note the limitation of recording acoustic signals in a noise-free environment (e.g., [
57,
60]) as not representing realistic acoustic conditions. To address the limitation, it was suggested to concentrate on the orientation and number of microphones along with the use of adaptive noise cancellation.
The INCA Sun Research Study [
61,
62,
63] was an in-vivo clinical trial that examined the INCA device’s effect on managing severe asthma. It involved 200 adult patients suffering from poor asthma control [
64]. The trial was conducted from Oct 2015 to Jan 2020. The study aimed to enhance inhaler therapy adherence and asthma control by comparing treatment decisions based on digitally acquired data with those based on conventional methods. Patients were randomly assigned to either the active or control group. Both groups attended three education visits over 8 weeks. It was followed by three treatment adjustment visits over 24 weeks. Digital inhaler adherence data guided treatment adjustment of the active group, while the control group used traditional methods. A third of the active group had dose reductions without increased airway inflammation, symptoms, or exacerbations, thus lowering side effect risks. This reduction did not compromise asthma control. The digital clinical decision support tool helped clinicians adhere to treatment recommendations. Medication adherence was improved by about 10% with a significant reduction in the treatment volume. This illustrates that digitally aided asthma care can be cost-effective and clinically beneficial.
Another similar two-stage study [
65] shows that the INCA device improves adherence and inhaler technique when used during consultations. Besides, the patients were satisfied with the device and the consultations. Despite the smaller sample size (18 adult COPD and asthma patients), the study demonstrates that embedding an objective measure of adherence and inhaler technique during community pharmacists’ consultations enhances the patients’ adherence and inhaler technique.
4.2. Sagentia Innovation VeriHaler
The
VeriHaler is an acoustic device by
Sagentia Innovation that aims to improve patient adherence to inhaler therapy [
62]. It features a built-in microphone that records the acoustic signals of inhalation and delivers feedback via a mobile application. The device is compatible with pMDIs and DPIs. It has a non-intrusive electronic design that does not affect the medication delivery.
VeriHaler eliminates background noise and accurately measures flowrate and inhaler usage. It promises to detect key inhalation parameters such as PIFR, inhalation timing, and formulation delivery. The mobile application enhances the user experience by enabling communication with the healthcare provider and alerting the patient in case of any signs of deterioration in their condition or employed technique. The device is still in the development stage.
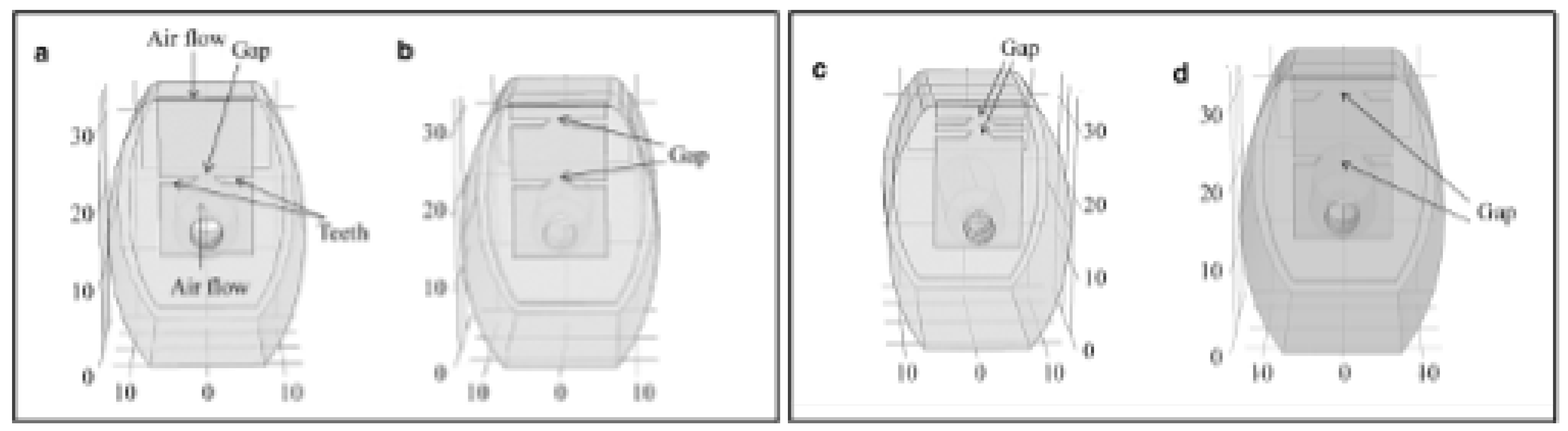
4.3. Tone Elements
An acoustic dry powder inhaler that could measure inhalation flow and medication dose was developed by the
University of Copenhagen and presented in [
66]. The device employs a passive acoustic component with comb-shaped teeth to produce sound signals changing with the air flowrate. The flow parameters associated with the inhalation technique are obtained by examining the features of the sound signals (e.g., amplitude, frequency, etc.). It is noteworthy that the device has a two-inlet design. Only one of them employs a passive acoustic component. This lowers the breathing resistance. It is particularly important for patients with severe airflow obstruction. The study investigated the effects of different geometries of acoustic elements. The results show that the proposed design with a single-tone gap (see
Figure 7, a) does not produce clear and distinct spectral peaks indicating tone components. On the other hand, increasing the number of gaps (see
Figure 7, b) improves the resolution of the spectra and the correlation with the airflow rate. At the same time, increasing the distance between the gaps (see
Figure 7, c) reduce the distinctness of the spectral peaks at lower frequencies. Moreover, the combination of two larger gaps and increasing gap distance (see
Figure 7, d) result in less pronounced and distinct spectral peaks.
Unfortunately, the design of the tone element was not justified or compared with any existing topologies. Moreover, the analysis was limited to the human audible range (20-20000 Hz), without explaining why this was done. The tone elements could have more pronounced peaks outside this range, which could be beneficial for several reasons. First, the natural frequency of the designed acoustic element could be above 20 kHz. Second, there could be less interference from other sources at higher frequencies. Third, higher frequencies could be more attenuated by distance, which could reduce the background noise. Furthermore, it would be preferable to have an inaudible acoustic element for the final product, as the device should not disturb other people with its noise. Despite the potential of the device for medication tracking for asthma and COPD patients (aiming to enhance their disease management and improve inhaler techniques), the project was not followed up or commercialized.
4.4. Amiko Respiro
Respiro is a digital platform created by
Amiko provider. It offers electronic solutions to track and record inhaler usage. The platform is compatible with various inhalers. The only currently commercially available model is
RS01X (see
Figure 8). It incorporates built-in sensors and digital features [
63]. The platform uses machine learning and sensing to measure and analyze the inhalation techniques, including inspiratory effort and inhalation flowrate. These metrics are assessed using pressure drop measurements ( [
67,
68]) enabling the real-time estimation of the inhalation technique. The data can be synchronized with a mobile application, which acts as a companion to the inhaler. It reminds a patient when to take a dose. It also provides personalized feedback and suggestions based on acquired data while using artificial intelligence to help a patient self-manage the use of the tool more effectively. Besides, it allows data sharing with healthcare providers. Unfortunately, no information was found in the literature presenting the in-vivo tests of the
RS01X device and its comparison with conventional methods of sustaining inhaler technique adherence. Nonetheless, the successful use of the platform with the
Ellipta inhaler was reported in [
69]. The patients showed high adherence to inhaled medication. They also completed daily diaries as part of the self-management intervention.
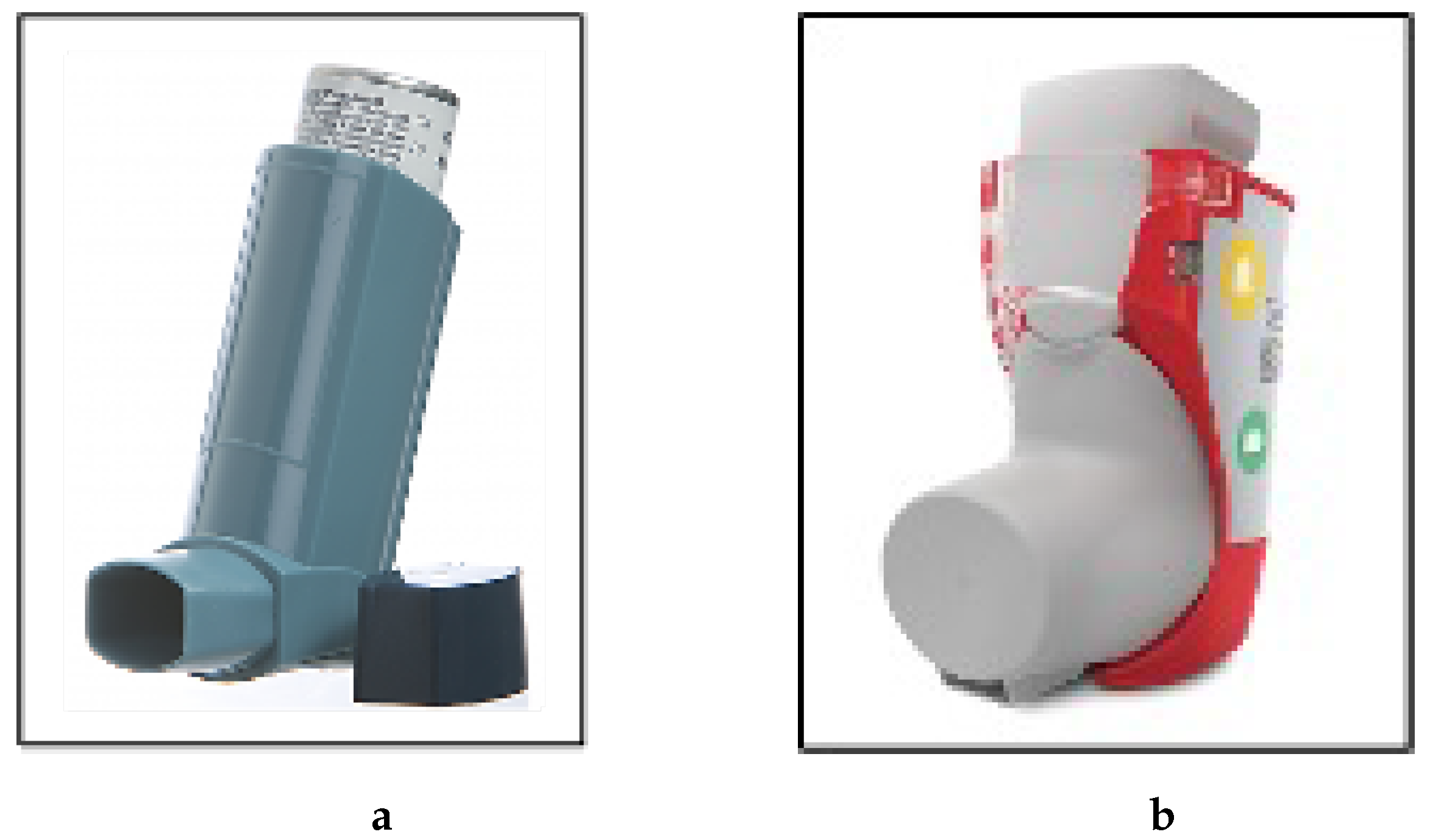
4.5. Intelligent Control Inhaler
The
Intelligent Control Inhaler (ICI) is a smart device developed by the
3M Drug Delivery Systems to enhance the treatment of respiratory diseases (see
Figure 9). The device was introduced in 2016 [
71]. It received the top award in a new category at the CPhI Pharma Awards that year [
72]. The device evaluates the inhalation technique and monitors drug delivery. Besides, it can regulate the inhalation flowrate. It is equipped with an integrated screen providing user instructions and feedback. The device offers a mobile application allowing users to share data with their healthcare providers via an inhalation data management platform. It employs a combination of breath actuation and innovative technology to control inhalation flowrate, and automatically improve the consistency of drug delivery. It is assumed that the device achieves this control function by varying its inhalation resistance characteristics [
73]. The latest update [
74] states that the device is still under development by
Kindeva, formerly
3M Drug Delivery Systems.
4.6. Teva Digihaler
Another option for the inhalation profile evaluation is the use of the
Digihaler family of smart inhalers developed by
Teva Respiratory [
76]. These devices were approved by the
Food and Drug Administration (FDA). Three models of
Digihaler devices having the same shape and electronic platform but differing in their medication were developed (see
Figure 10). The first model is the
ProAir Digihaler. It is a rescue inhaler that contains a short-acting medication to relieve or prevent bronchospasms associated with asthma and COPD as well as exercise-induced bronchospasms. The
ArmonAir Digihaler is a maintenance inhaler for long-term treatment that reduces inflammation and swelling of the airways. The
AirDuo Digihaler is also a maintenance device that contains a long-acting medication for the control of symptoms such as wheezing and airway narrowing. The
Digihaler devices are equipped with a pressure sensor, wireless transmitter, and processor. The pressure sensor is connected to a mouthpiece. It senses all inhaler activities. The device estimates the inhalation flow rate in real time using the pressure measurement. The device can be paired with a smartphone app to track inhaler usage data, such as peak inspiratory flow rate, inhalation volume, and events. The data can be shared with healthcare providers. Additionally, it offers feedback to help users improve their inhalation technique, potentially preventing symptom worsening.
A predictive model for
Clinical Asthma Exacerbation (CAE) based on data collected from the
ProAir Digihaler was developed and validated in a pilot study involving 360 poorly controlled asthma patients [
77]. The model used metrics such as PIFR, volume, duration, and time-to-peak flow as predictors. The results show that the average number of daily inhalations over five days is a reliable indicator of CAE risk. The same data were later used in another study [
78] to build a machine-learning model for CAE prediction. The machine learning model also confirms that increased medication consumption is a predictor of CAE events and can forecast their occurrence within the next five days.
The efficacy of the
ProAir Digihaler was demonstrated in a randomized controlled trial [
79]. The main objective of the trial was to compare the
ProAir Digihaler application with standard asthma care. A total of 333 participants were randomly assigned to either the
Digihaler enhanced or the standard care group. Their inhalation data were monitored weekly for 12 weeks. The trial found that participants using the
Digihaler device had an 85.3% higher probability of improving their asthma control than those using standard care.
However, there is also a downside to the Digihaler devices. All the devices have a dose counter attached to the actuator. It shows the number of remaining doses. Since these devices are all-in-one, they are to be discarded once they run out of doses. Moreover, they are relatively expensive.
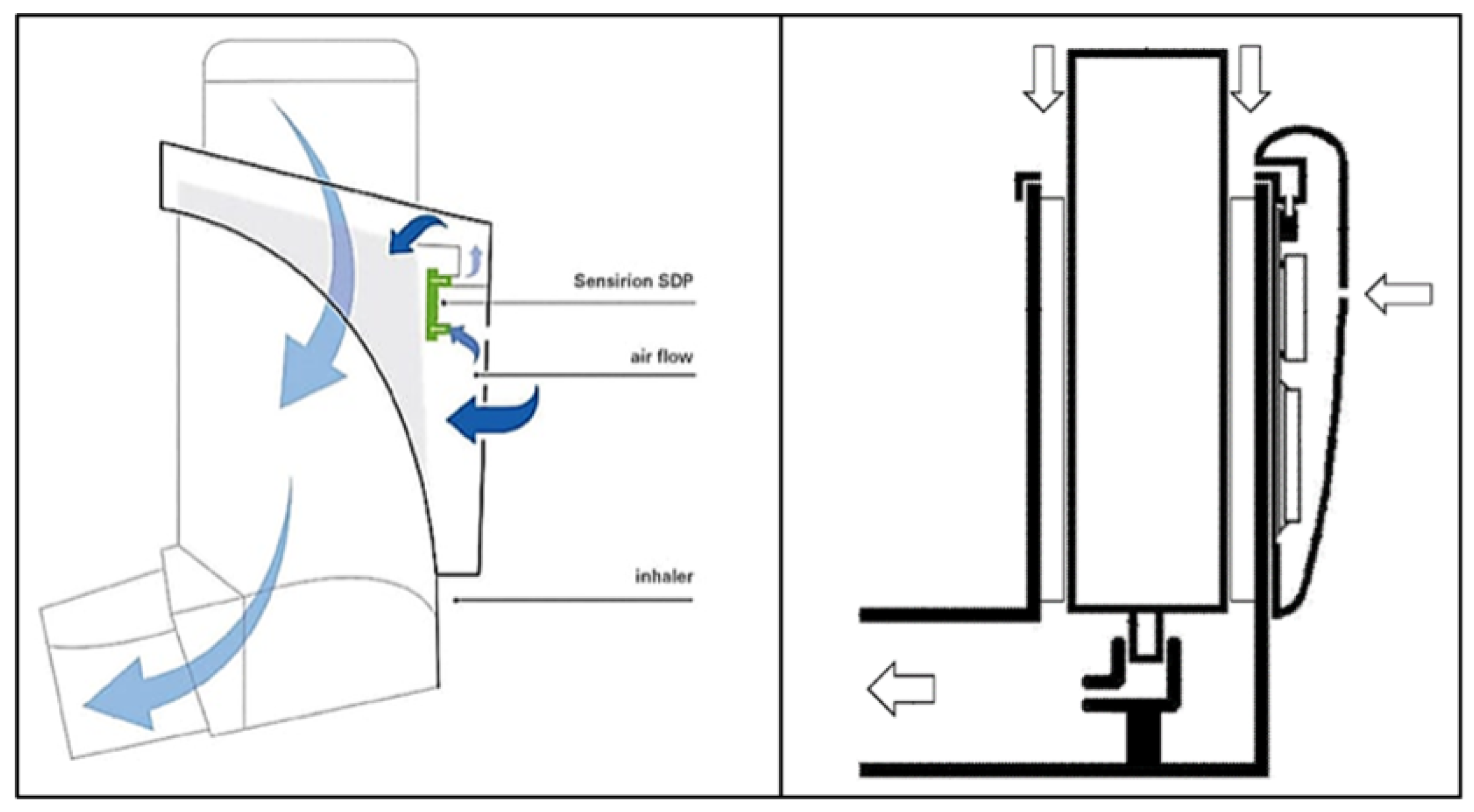
4.7. Sensirion Inhaler Clip-on
A prototype of a clip-on device with a pressure sensor was designed and patented by
Sensirion [
28,
80]. It is attached to the inhaler and measures the patient’s inhalation airflow and timing of the inhaler actuation. The device employs a differential pressure sensor enabling the measurement of mass flow in a bypass configuration. The bypass configuration (see
Figure 11) preserves the flow path of the inhaler and ensures no interference with the existing inhaler device function. This feature offers a significant benefit as it eliminates the need for revalidation of the inhaler with the FDA.
The inventors refer to the Bernoulli/Venturi effect to describe how the patient’s inhalation causes the air flow entering the inhaler to accelerate and create a negative pressure at the inhaler top opening (around the canister) and the opening of the clip-on device. The negative pressure magnitude is directly proportional to the flowrate magnitude of the airflow through the inhaler to the patient and is detected by the flow sensor. By measuring the bypass airflow and knowing the bypass-to-main-pass ratio (which is determined by the clip-on/inhaler geometries), the total airflow to the patient can be calculated. The device uses the world’s smallest differential pressure sensor from the Sensirion SDP3x family. This solution is optimal for measuring mass flow in a bypass configuration. Unfortunately, it is relatively costly thus affecting the device’s accessibility. However, it has the advantage of being reusable (unlike the Digihaler devices discussed earlier). Currently, the device has no data on experimental testing or research on its efficacy. It is also not yet available on the market while having a trademark.
4.8. Adherium Hailie
Hailie sensors were developed by
Adherium Limited. They can be attached to different inhalers (see
Figure 12). The sensors are linked to a phone and record medication actuation events. Initially, they did not measure the inspiratory flow. However, the next generation of the devices was capable of measuring flowrate, detecting inspiratory flow, inhaler shakes, and inhaler orientation. Inhalers such as
Trava ProAir, Advair, Ventolin, and
Symbicort are supported by the
Hailie devices. The FDA approval for these next-generation sensors was obtained in late 2021 [
81] and received FDA clearance later [
81]. Unfortunately, no results of clinical studies of the devices and their benefits were found in the literature.
4.9. CapMedic
CapMedic is a digital add-on device designed by
Cognita Labs to assist patients with asthma and COPD to use pMDIs correctly (see
Figure 13). It provides real-time feedback by audio-visual cues throughout the steps of the device application. Spirometry and measurement of lung exhalation parameters such as
Forced Expiratory Volume and
Peak Expiratory Flow are among the declared features [
83]. These measurements are performed using built-in sensors. They provide users with information on their actual inhalation technique.
CapMedic can be beneficial in improving the inhaler application technique and medication delivery as indicated by the publications [
84] and [
82]. However, significantly more substantial independent studies are needed to fully validate the efficiency of the device. Furthermore, the technical details of the sensors are not well-documented in the literature. Besides, the
CapMedic device operates while employing a subscription-based model, which may pose a kind of barrier for some users.
5. Conclusion
The significance of the inhalation flowrate measurements and the current state of the related technologies are reviewed in this paper. The review demonstrates that proper inhaler technique and consistent adherence are crucial for managing respiratory conditions effectively. Monitoring inhalation flowrates emerges as a promising approach to assess the progress. However, the widespread mishandling of inhaler application techniques poses a significant clinical challenge. This is particularly true in ensuring the accurate dose delivery, which depends on the optimal flowrate. Unfortunately, it is specific to an inhaler model.
Results in the relevant recent literature support special training device engagement to guide and improve inhalation techniques. However, despite the demonstrated positive impact, training inhalation devices have limitations such as inconvenience in private usage and incompatibility with different medications and inhaler models. The ongoing reliance on healthcare professionals for inhaler selection and utilization highlights the need for research to develop smart inhaler devices capable of flowrate measurements and providing personalized feedback. The development and application of smart inhaler technologies and products (particularly those facilitating flowrate control) become a critically important task.
The presented review on existing and forthcoming new perspective solutions in the field of inhalation flowrate measurement aims to contribute towards addressing the task.
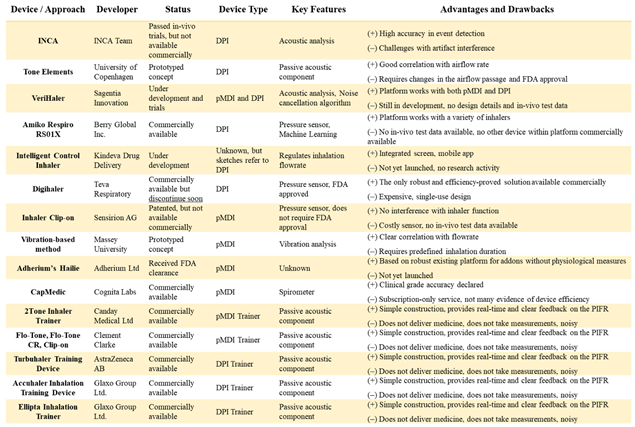
Table 1 summarises information on the smart inhaler devices referred to in this review. Several of them are capable of measuring the flowrate during inhalation and providing feedback to the users. However, most of them are not commercially available as yet.
Approaches based on the acoustic analysis of the inhalation process have been introduced, using cost-effective acoustic sensors over traditional small-sized pressure sensors for airflow measurements. Despite the strong potential, none of such devices have reached the commercial availability stage, with only one passing through some trials after extensive development. This highlights the need for further research and trials to overcome the challenges and limitations of such a novel approach.
References
- Asthma and Respiratory Foundation NZ (ARFNZ). Asthma. https://www.asthmafoundation.org.nz/your-health/living-with-asthma. Accessed: 14 01 2024.
- Environmental Health Intelligence New Zealand (EHINZ). Environmental health indicators - indoor environment - asthma. https://www.ehinz.ac.nz/indicators/indoor-environment/asthma/. Accessed: 14 01 2024.
- Asthma and Respiratory Foundation NZ (ARFNZ). Key statistics | Asthma Foundation NZ. https://www.asthmafoundation.org.nz/research/key-statistics. Accessed: 14 01 2024.
- Kocks, J.; Chrystyn, H.; van der Palen, J.; Thomas, M.; Yates, L.; Landis, S.; Driessen, M.; Gokhale, M.; Sharma, R.; Molimard, M. Systematic review of association between critical errors in inhalation and health outcomes in asthma and COPD. npj Primary Care Respiratory Medicine 2018, 28, 43. [Google Scholar] [CrossRef] [PubMed]
- Usmani, O.; Lavorini, F.; Marshall, J.; Dunlop, W.; Heron, L.; Farrington, E.; Dekhuijzen, R. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respiratory Research 2018, 19, 1–20. [Google Scholar] [CrossRef]
- Haidl, P.; Heindl, S.; Siemon, K.; Bernacka, M.; Cloes, R. Inhalation device requirements for patients’ inhalation maneuvers. Respiratory Medicine 2016, 118, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, D. Smart inhalers: will they help to improve asthma care? The Pharmaceutical Journal https://pharmaceutical-journal.com/article/feature/smart-inhalers-will-they-help-to-improve-asthma-care. Accessed: 2024 01 15.
- GoodRx. Smart inhalers: A review of smart inhalers. https://www.goodrx.com/conditions/asthma/smart-inhalers-review. Accessed: 14 01 2024.
- CareFirst Community Partners, Inc. Asthma | CareFirst Community Health Plan Maryland. https://www.carefirstchpmd.com/health-wellness/asthma. Accessed: 05 03 2024.
- Adherium Limited. Hailie® for Symbicort® HFA. https://www.hailie.com/collections/hailie-sensors/products/hailie-for-symbicort-hfa. Accessed: 05 03 2024.
- Eikholt, A.; Wiertz, M.; Hew, M. Electronic monitoring devices to support inhalation technique in patients with asthma: a narrative review. Current Treatment Options in Allergy 2023, 10, 28–52. [Google Scholar] [CrossRef]
- Xiroudaki, S.; Schoubben, A.; Giovagnoli, S.; Rekkas, D. Dry powder inhalers in the digitalization era: current status and future perspectives. Pharmaceutics 2021, 13, 1455. [Google Scholar] [CrossRef] [PubMed]
- Häußermann, S.; Arendsen, L.; Pritchard, J. Smart dry powder inhalers and intelligent adherence management. Advanced Drug Delivery Reviews 2022, 12. [Google Scholar] [CrossRef]
- Chrystyn, H.; Audibert, R.; Keller, M.; Quaglia, B.; Vecellio, L.; Roche, N. Real-life inhaler adherence and technique: Time to get smarter! Respiratory Medicine 2019, 158, 24–32. [Google Scholar] [CrossRef]
- Hancox, R.; Jones, S.; Baggott, C.; Chen, D.; Corna, N.; Davies, C.; Fingleton, J.; Hardy, J.; Hussain, S.; Poot, B.; Reid, J.; Travers, J.; Turner, J.; Young, R. New Zealand COPD guidelines: quick reference guide. https://www.asthmafoundation.org.nz/health-professionals/management-guidelines/nz-copd-guidelines. Accessed: 2024 01 24.
- Yang, I.; George, J.; McDonald, C.; McDonald, V.; Ordman, R.; Goodwin, A.; Smith, B.; McNamara, R. andZwar, N.; Dabscheck, E. The COPD-X plan Australian and New Zealand guidelines for the management of chronic obstructive pulmonary disease 2023. https://copdx.org.au/copd-x-plan/. Accessed: 24 01 2024.
- Usmani, O. Choosing the right inhaler for your asthma or COPD patient. Therapeutics and Clinical Risk Management 2019, 15, 461–472. [Google Scholar] [CrossRef]
- Hua, J.; Ye, X.; Du, C.; Xie, N.; Zhang, J.; Li, M.; Zhang, J. Optimizing inhalation therapy in the aspect of peak inhalation flow rate in patients with chronic obstructive pulmonary disease or asthma. BMC Pulmonary Medicine 2021, 21, 302. [Google Scholar] [CrossRef]
- Bosnic-Anticevich, S.; Chrystyn, H.; Costello, R.; Dolovich, M.; Fletcher, M.; Lavorini, F.; Rodríguez-Roisin, R.; Ryan, D.; Wan Yau Ming, S.; Price, D. The use of multiple respiratory inhalers requiring different inhalation techniques has an adverse effect on COPD outcomes. International Journal of Chronic Obstructive Pulmonary Disease 2016, 21, 59–71. [Google Scholar] [CrossRef]
- Janson, C.; Loof, T.; Telg, G.; Stratelis, G. Impact of inhalation flow, inhalation volume and critical handling errors on delivered Budesonide/Formoterol dose in different inhalers: An in vitro study. Pulmonary Therapy 2017, 3, 243–253. [Google Scholar] [CrossRef]
- Weers, J.; Clark, A. The Impact of inspiratory flow rate on drug delivery to the lungs with dry powder inhalers. Pharmaceutical Research 2017, 34, 507–528. [Google Scholar] [CrossRef]
- Colthorpe, P.; Voshaar, T.; Kieckbusch, T.; Cuoghi, E.; Jauernig, J. Delivery characteristics of a low-resistance dry-powder inhaler used to deliver the long-acting muscarinic antagonist glycopyrronium. Journal of Drug Assessment 2013, 2. [Google Scholar] [CrossRef] [PubMed]
- Lavorini, F.; Pistolesi, M.; Usmani, O. Recent advances in capsule-based dry powder inhaler technology. Multidisciplinary Respiratory Medicine 2017, 12. [Google Scholar] [CrossRef]
- Talaat, M.; Si, X.; Xi, J. Lower inspiratory breathing depth enhances pulmonary delivery efficiency of ProAir sprays. Pharmaceuticals 2022, 15. [Google Scholar] [CrossRef] [PubMed]
- Dastoorian, F.; Pakzad, L.; Kozinski, J.; Behzadfar, E. A CFD investigation on the aerosol drug delivery in the mouth–throat airway using a pressurized metered-dose inhaler device. Processes 2022, 10, 11–16. [Google Scholar] [CrossRef]
- Yang, M.; Verschuer, J.; Shi, Y.; Song, Y.; Katsifis, A.; Eberl, S.; Wong, K.; Brannan, J.; Cai, W.; Finlay, W.; Chan, H. The effect of device resistance and inhalation flow rate on the lung deposition of orally inhaled mannitol dry powder. International Journal of Pharmaceutics 2016, 513, 294–301. [Google Scholar] [CrossRef]
- Koullapis, P.; Kassinos, S.; Bivolarova, M.; Melikov, A. Particle deposition in a realistic geometry of the human conducting airways: Effects of inlet velocity profile, inhalation flowrate and electrostatic charge. Journal of Biomechanics 2016, 49, 2201–2212. [Google Scholar] [CrossRef]
- Sensirion, AG. Flow measurement in smart medical inhalers. https://www.techbriefs.com/component/content/article/45965-flow-measurement-in-smart-medical-inhalers. Accessed: 15 01 2024.
- Sensirion, AG. Flow measurement in smart inhalers. https://www.sensirion.com/products/product-insights/specialist-articles/flow-measurement-in-smart-inhalers-for-connected-drug-delivery/. Accessed: 05 03 2024.
- Clark, A.; Weers, J.; Dhand, R. The confusing world of dry powder inhalers: It is all about inspiratory pressures, not inspiratory flow rates. Journal of Aerosol Medicine and Pulmonary Drug Delivery 2020, 33, 1–11. [Google Scholar] [CrossRef]
- Duarte-de Araújo, A.; Teixeira, P.; Hespanhol, V.; Correia-de Sousa, J. COPD: misuse of inhaler devices in clinical practice. International Journal of Chronic Obstructive Pulmonary Disease 2019, 14, 1209–1217. [Google Scholar] [CrossRef]
- Al-Woraf, Y. Evaluation of inhaler technique among patients with asthma and COPD in Yemen. Journal of Taibah University Medical Sciences 2018, 13, 488–490. [Google Scholar] [CrossRef] [PubMed]
- DeWeerdt, S. Environmental concerns and the perennial problem of poor inhaler technique are driving change in the devices used to deliver respiratory drugs. Nature 2020, 581. [Google Scholar]
- Sobh, A.; Rabea, H.; Hamouda, M.; Shawky, F.; Abdelrahim, M. Impact of repeated patient counseling using different pressurized metered-dose inhalers training devices on inhalation technique, lung function, and asthma control in adult asthmatics. Beni-Suef University Journal of Basic and Applied Sciences 2022, 88. [Google Scholar] [CrossRef]
- Fortescue, R.; Kew, K.; Mathioudakis, A. Interventions to improve inhaler technique for people with asthma. Cochrane Database of Systematic Reviews 2017, 3, CD012286. [Google Scholar]
- Canday Medical Ltd. 2Tone Trainer - The metered dose inhaler (MDI) training device. http://2tonetrainer.net/index.html. Accessed: 30 01 2024.
- Al-Showair, R.; Pearson, S.; Chrystyn, H. Two-tone trainer maintains a slow inhalation rate when using a metered dose inhaler (MDI). European Respiratory Journal 2005, 26. [Google Scholar]
- Al-Showair, R.; Pearson, S.; Chrystyn, H. Maintenance of good inhalation technique for metered dose inhalers (MDIs) by using a two-tone trainer; American Thoracic Society 2005 International Conference: San Diego, California, 2005. [Google Scholar]
- Al-Showair, R.; Pearson, S.; Chrystyn, H. The potential of a 2Tone trainer to help patients use their metered-dose inhalers. Chest 2007, 131, 1776–1782. [Google Scholar] [CrossRef] [PubMed]
- Tarsin, W.; Hshad, N.; Elshamli, I.; Soussi, M.; Chrystyn, H. Training patients on how to use metered dose inhaler (MDI) by using the 2Tone will improve asthma quality of life (AQOL); European Respiratory Society Annual Congress: Berlin, Germany, 2008. [Google Scholar]
- Ammari, W.; Chrystyn, H. Optimizing the inhalation flow and technique through metered dose inhalers of asthmatic adults and children attending a community pharmacy. Journal of Asthma 2013, 50, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Flexicare. Inhaler Trainers • Clement Clarke • Flexicare. https://flexicare.com/en-us/product-category/inhaler-technique/train/. Accessed: 30 01 2024.
- Clement Clarke International Limited. Flo-Tone Trainer Regular. https://shop.clement-clarke.com/ProductDetails/tabid/122/ProductID/18/Default.aspx. Accessed: 05 03 2024.
- Clement Clarke International Limited. Flo-Tone CR. https://shop.clement-clarke.com/ProductDetails/tabid/122/ProductID/82/Default.aspx. Accessed: 05 03 2024.
- Clement Clarke International Limited. Clip-Tone E. https://shop.clement-clarke.com/ProductDetails/tabid/122/ProductID/95/Default.aspx. Accessed: 05 03 2024.
- Ammari, W.; Obeidat, N.; Anani, A.; AlKalbani, R.; Sanders, M. Evaluation of Trainhaler and Flo-Tone Cr training devices to help adults with asthma optimize their pressurized metered dose inhaler technique and inhalation flow; The American Thoracic Society (ATS) Annual Conference: Washington DC, USA, 2017. [Google Scholar]
- Nicola, M.; Elberry, A.; Sayed, O.; Hussein, R.; Saeed, H.; Abdelrahim, M. The impact of adding a training device to familiar counselling on inhalation technique and pulmonary function of asthmatics. Advances in Therapy 2018, 35, 1049–1058. [Google Scholar] [CrossRef] [PubMed]
- Tony, S.; Abdelrahman, M.; Osama, H.; Abdelrahim, M. Advanced counselling using training device and smartphone application on inhalation technique from metered-dose inhaler with spacer equipped with different interfaces in asthmatic children. International Journal of Clinical Practice 2021, 75. [Google Scholar] [CrossRef]
- Tony, S.; Abdelrahman, M.; Osama, H.; Elgendy, M.; Abdelrahim, M. The effect of adding a training device and smartphone application to traditional verbal counseling in asthmatic children. Pulmonary Therapy 2021, 7, 549–562. [Google Scholar] [CrossRef]
- Tony, S.; Abdelrahman, M.; Elsalam, M.; Shafik, M.; Abdelrahim, M. Effect of using acoustic flo-tone training device and its smartphone application on enhancing inhalation technique from metered-dose inhaler with spacer in asthmatic children. Experimental Lung Research 2022, 48, 224–238. [Google Scholar] [CrossRef] [PubMed]
- Sobh, A.; Rabea, H.; Hamouda, M.; Shawky, F.; Saeed, H.; Abdelrahim, M. The impact of using different add-on devices to pressurized metered-dose-inhalers containing salbutamol in healthy adult volunteers: An in-vivo study. Journal of Drug Delivery Science and Technology 2022, 74, 103539. [Google Scholar] [CrossRef]
- Holmes, M.; Menn, M.; D’Arcy, S.; Rapcan, V.; MacHale, E.; Costello, R.; Reilly, R. Automatic identification and accurate temporal detection of inhalations in asthma inhaler recordings; San Diego, California USA: Annual International Conference of the IEEE EMBS, 2012. [Google Scholar]
- Holmes, M.; Seheult, J.; Geraghty, C.; D’Arcy, S.; O’Brien, U.; O’Connell, G.; Costello, R.; Reilly, R. A method of estimating inspiratory flow rate and volume from an inhaler using acoustic measurements. Physiological Measurement 2013, 34, 903–914. [Google Scholar] [CrossRef] [PubMed]
- Holmes, M.; Seheult, J.; Geraghty, C.; D’Arcy, S.; Costello, R.; Reilly, R. Using acoustics to estimate inspiratory flow rate and drug removed from a dry powder inhaler; Annual International Conference of the IEEE EMBS: Osaka, Japan, 2013. [Google Scholar]
- Seheult, J.; Holmes, M.; Geraghty, C.; Costello, R.; Hughes, C.; Keane, F.; Reilly, R. Validation of an acoustic device for the real-time monitoring of inhalational technique and correlation with drug delivery from a Diskus inhaler 2013.
- Holmes, M.; D’Arcy, S.; Costello, R.; Reilly, R. An acoustic method of automatically evaluating patient inhaler technique; Annual International Conference of the IEEE EMBS: Osaka, Japan, 2013. [Google Scholar]
- Holmes, M.; D’arcy, S.; Costello, R.; Reilly, R. Acoustic analysis of inhaler sounds from community-dwelling asthmatic patients for automatic assessment of adherence. IEEE Journal of Translational Engineering in Health and Medicine 2014, 11, 2700210. [Google Scholar] [CrossRef] [PubMed]
- D’Arcy, S.; MacHale, E.; Seheult, J.; Holmes, M.; Hughes, C.; Sulaiman, I.; Hyland, D.; O’Reilly, C.; Glynn, S.; Al-Zaabi, T.; McCourt, J.; Taylor, T.; Keane, F.; Killane, I.; Reilly, R.; Costello, R. A method to assess adherence in inhaler use through analysis of acoustic recordings of inhaler events. PLOS ONE 2014, 9, e98701. [Google Scholar] [CrossRef] [PubMed]
- Seheult, J.; O’Connell, P.; Chun Tee, K.; Bholah, T.; Bannai, H.; Sulaiman, I.; MacHale, E.; D’Arcy, S.; Holmes, M.; Bergin, D.; Reeves, E.; Reilly, R.; Crispino-O’Connell, G.; Ehrhardt, C.; Healy, A.; Costello, R. The acoustic features of inhalation can be used to quantify aerosol delivery from a Diskus™ dry powder inhaler. Pharmaceutical Research 2014, 31, 2735–2747. [Google Scholar] [CrossRef] [PubMed]
- Taylor, T.; Holmes, M.; Sulaiman, I.; Costello, R.; Reilly, R. Monitoring inhaler inhalations using an acoustic sensor proximal to inhaler devices. Journal of Aerosol Medicine and Pulmonary Drug Delivery 2016, 29, 439–446. [Google Scholar] [CrossRef] [PubMed]
- INCA. INhaler Compliance Assessment (INCA). https://www.incadevice.com/#research. Accessed: 03 02 2024.
- Sulaiman, I.; Hale, E.; Holmes, M.; Hughes, C.; D’Arcy, S.; Taylor, T.; Rapcan, V.; Doyle, F.; Breathnach, A.; Seheult, J.; Murphy, D.; Hunt, E.; Lane, S.; Sahadevan, A.; Crispino, G.; Diette, G.; Killane, I.; Reilly, R.; Costello, R. A protocol for a randomised clinical trial of the effect of providing feedback on inhaler technique and adherence from an electronic device in patients with poorly controlled severe asthma. BMJ Open 2016, 6, e009350. [Google Scholar] [CrossRef] [PubMed]
- O’Dwyer, S.; MacHale, E.; Sulaiman, I.; Holmes, M.; Hughes, C.; D’Arcy, S.; Rapcan, V.; Taylor, T.; Boland, F.; Bosnic-Anticevich, S.; Reilly, R.; Ryder, S.; Costello, R. The effect of providing feedback on inhaler technique and adherence from an electronic audio recording device, INCA®, in a community pharmacy setting: study protocol for a randomised controlled trial. Trials 2016, 17, 1–9. [Google Scholar] [CrossRef]
- Hale, E.; Greene, G.; Mulvey, C.; Mokoka, M.; van Boven, J.; Cushen, B.; Sulaiman, I.; Brennan, V.; Kerr, P.; Reilly, R. Use of digital measurement of medication adherence and lung function to guide the management of uncontrolled asthma (INCA Sun): a multicentre, single-blinded, randomised clinical trial. The Lancet. Respiratory Medicine 2023, 11, 591–601. [Google Scholar] [CrossRef]
- Hesso, I.; Nabhani-Gebara, S.; Kayyali, R. Objective assessment of adherence and inhaler technique among asthma and COPD patients in London: A study in community pharmacies using an electronic monitoring device. Pharmacy 2023, 11, 94. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Bohr, A.; Jensen, H.; Rantanen, J.; Cornett, C.; Beck-Broichsitter, M.; Bøtker, J. Medication tracking: design and fabrication of a dry powder inhaler with integrated acoustic element by 3D printing. Springer Science+Business Media 2020, 37, 2755–2758. [Google Scholar] [CrossRef] [PubMed]
- Braido, F.; Paa, F.; Ponti, L.; Canonica, G. A new tool for inhalers’ use and adherence monitoring: the Amiko® validation trial. International Journal of Engineering Research & Science 2016, 2, 2395–6992. [Google Scholar]
- Rogueda, P.; Grinovero, M.; Ponti, L.; Purkins, G.; Croad, O. Telehealth ready: Performance of the Amiko Respiro Sense connected technology with Merxin DPIs. Drug Delivery to the Lungs 2018, DDL2018. [Google Scholar]
- Sloots, J.; Bakker, M.; van der Palen, J.; Eijsvogel, M.; van der Valk, P.; Linssen, G.; van Ommeren, C.; Grinovero, M.; Tabak, M.; Effing, T.; Lenferink, A. Adherence to an eHealth self-management intervention for patients with both COPD and heart failure: Results of a pilot study. International Journal of Chronic Obstructive Pulmonary Disease 2021, 15, 2089–2103. [Google Scholar] [CrossRef] [PubMed]
- Berry Global Inc.. RS01X | Connected and intelligent single-dose dry powder inhaler. https://rs01x.com/. Accessed: 05 03 2024.
- 3M drug delivery systems. 3M News Center - Press Releases. https://news.3m.com/2016-04-19-3M-Unveils-Intelligent-Inhaler-Designed-to-Help-Control-Spiraling-Costs-of-Respiratory-Disease#assets_all, 2016. Accessed: 05 02 2024.
- 3M drug delivery systems. Industry recognition for 3M’s smart inhaler. https://www.3m.co.uk/3M/en_GB/health-care-uk/stories/full-story/?storyid=0435d96d-8c27-4c9a-b6cd-d5ac72b80ac7, 2016. Accessed: 05 02 2024.
- 3M. (23) 3M’s Intelligent Control Inhaler wins Excellence in Drug Delivery Devices Award at CPhI | LinkedIn. https://www.linkedin.com/pulse/3ms-intelligent-control-inhaler-wins-excellence-drug-delivery-harris/, 2016. Accessed: 05 02 2024.
- Needham, M.; Cocks, P.; Righton, L. Next-generation pressurised metered dose inhalers: a holistic, patient-centred approach to sustainability. ONdrugDelivery.
- Beesley, R. A seismic shift for inhalation is just the beginning. Pharmaceutical Processing 2018. https://www.pharmaceuticalprocessingworld.com/a-seismic-shift-for-inhalation-is-just-the-beginning/, 2018. Accessed: 25 07 24.
- Teva Respiratory, LLC. Digihaler Support Site Home. https://www.digihaler.com/support. Accessed: 04 02 2024.
- Safioti, G.; Granovsky, L.; Li, T.; Reich, M.; Cohen, S.; Hadar, Y.; Pleasants, R.; Chrystyn, H.; Hill, T.; DePietro, M. A predictive model for clinical asthma exacerbations using Albuterol eMDPI (ProAir Digihaler): A twelve-Week, open-label study. iproc 2019, 5, e15173. [Google Scholar] [CrossRef]
- Lugogo, N.; DePietro, M.; Reich, M.; Merchant, R.; Chrystyn, H.; Pleasants, R.; Granovsky, L.; Li, T.; Hill, T.; Brown, R.; Safioti, G. A predictive machine learning tool for asthma exacerbations: Results from a 12-week, open-label study using an electronic multi-dose dry powder inhaler with integrated sensors. Journal of Asthma and Allergy 2022, 11, 1623–1637. [Google Scholar] [CrossRef] [PubMed]
- Hoyte, F.; Mosnaim, G.; Rogers, L.; Safioti, G.; Brown, R.; Li, T.; DePietro, M.; Reich, M.; Hill, T.; Wechsler, M. Effectiveness of a digital inhaler system for patients with asthma: A 12-week, open-label, randomized study (CONNECT1). The Journal of Allergy and Clinical Immunology: In Practice 2022, 11, 1334. [Google Scholar] [CrossRef]
- Zipkes, C.; Alt, A. Determination of air flow rate through an. inhaler. Patent Number 20200155773, 2019. [Google Scholar]
- Adherium Limited. Adherium - Adherium unveils new FDA-cleared Smartinhaler® compatible with Airsupra® and Breztri® inhalation devices. https://www.adherium.com/news/adherium-unveils-new-fda-cleared-smartinhaler-compatible-with-airsupra-and-breztri-inhalation-devices/, 2021. Accessed: 2024 07 25.
- Paronyan, E.; Landon, C.; Biswas, R.; Wicklund, H.; Wallace, K.; Thompson, A. Utilizing Capmedic electronic device to measure and improve inhaler technique in clinic; American Thoracic Society International Conference: Philadelphia, PA, 2020. [Google Scholar]
- Cognita Labs. CapMedic - simplifying respiratory care by correct and regular inhaler use. https://capmedicinhaler.com/. Accessed: 2024 07 25.
- Biswas, R.; Patel, G.; Mohsin, A.; Hanania, N.; Sabharwal, A. Measuring competence in metered dose inhaler use using Capmedic electronic inhaler monitoring tool. Chest 2016, 150, 14A. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).