1. Introduction
Open wounds can be characterized by the loss of a layer of full-thickness skin, carry a risk of infection due to exposure to a foreign material, and result from traumatic degloving and shear injuries, lacerations, avulsions, envenomation, burns, abscesses, necrotizing vasculitis, incisional dehiscence, and open surgery [
1]. Treating skin defects of the limbs in dogs and cats can be challenging due to limited skin availability [
2]. The advantages of reconstruction with a skin flap is the blood flow supply of the flap and the staged primary closure [
3,
4]. Alternatively, for open wounds of the distal limbs, skin damage can be managed, and the effect of a two-staged treatment approach may be improved [
5]. In wounds involving the extremities, injuries to the nerves, muscles, tendons, blood vessels, and bones can be diagnosed by evaluating the function of the parts distal to the injury site [
6].
The naming of bone transplants is based on their origin and composition. Autograft transplantation is when tissue is taken from a donor site and transplanted to a recipient within the same individual [
7]. A diagnosis of fracture nonunion is based on radiological evidence, such as hypertrophy or atrophy of bone fragments, defects between the fracture ends, sclerosis, and a closed bone marrow cavity [
8]. Among the 582 total fractures in dogs and cats, twenty (3.4%) were reported as nonunion. Implant failure and refracture seemed to occur, and the radius, ulna, and femur seemed to be the most affected [
9]. Cancellous bone grafting has proven to be a very successful method for treating primary fractures showing nonunion and delayed healing, as well as arthritis and chronic myelitis, in dogs. This technique is highly regarded in the field of orthopedics because it promotes bone formation and stimulates the healing of fractures, making it the gold standard among such procedures [
10,
11]. Segmental defects and delayed union for fractures of long bones continue to present significant challenges for orthopedic surgeons. Complex open fractures can create asymmetry in essential anatomical structures, leading to impaired functionality [
12]. Another study suggested that tail vertebral autografts are a new source of long bone defects in dogs [
13]. The aim of this study is to introduce the use of ulnar bone grafting and skin flap reconstruction for radius bone defects and open wounds in a dog.
2. Case Presentation
2.1. History and Clinical Examination
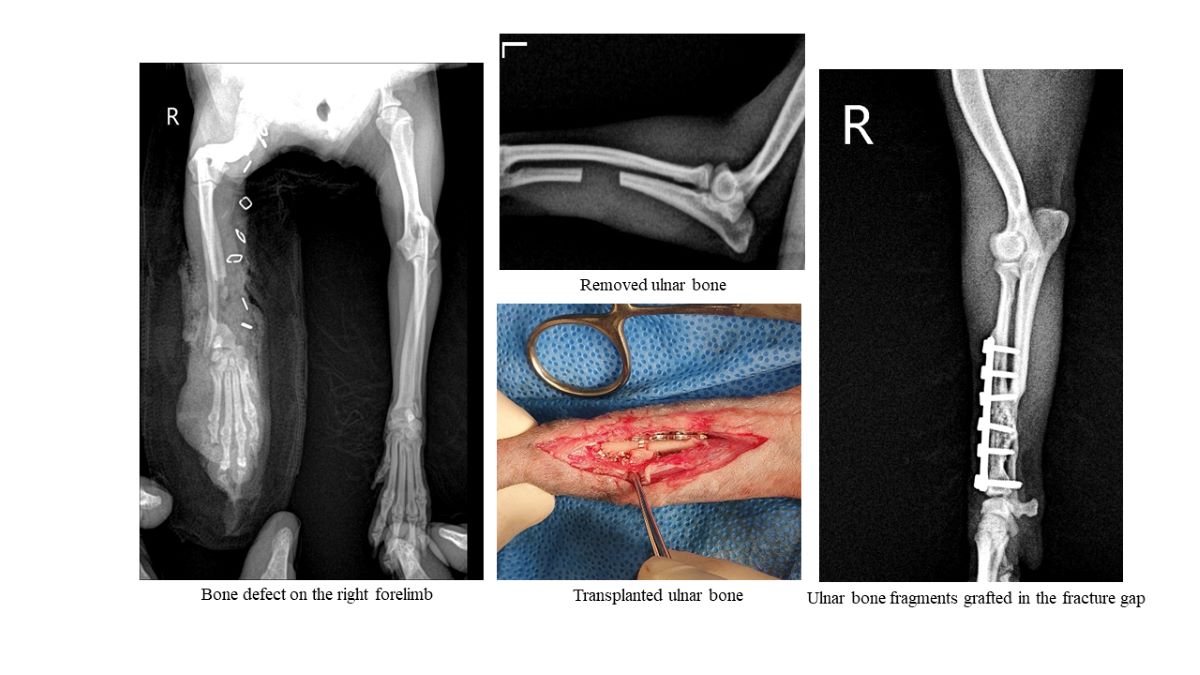
A one-year-old spayed female Poodle dog weighing 1.7 kg was brought in with non-weight-bearing lameness, an open wound, and a fracture in the right forelimb. The dog had fallen off the bicycle being ridden by its owner, causing its right forelimb to be caught in the wheel. As a result, the dog was brought to an animal hospital for treatment. During the visit, it was observed that the right forelimb was unable to bear any weight, and there were visible abrasions and lacerations on the skin. Subcutaneous tissues and muscle were visually exposed due to laceration of the metacarpal pad and the 2nd, 3rd, and 4th digit pads from the shoulder joint to the inside of the distal part of the forelimb (
Figure 1 A, B, and C). Radiography confirmed that the diaphysis of the 5th proximal phalanx was fractured, and the middle and distal phalanx were severely damaged. A bone defect of approximately 1.8 cm was identified in the right radial diaphysis, and there was no specificity for the chest, abdomen, or both hindlimbs except for minor abrasions on the left forelimb (
Figure 1A, B, and C). On ultrasonography, there was no specificity except for the presence of echogenic sludge in the urinary bladder.
The owner was told to watch for other clinical symptoms while the dog was hospitalized for 3 days, and butorphanol (0.1 mg/kg, Myungmoon Pharm Co., Korea) was injected into the dog as first aid. In addition, Hartman-D (Hartman-D Solution 500 mL, HK inno. N Corp, Korea) was infused at a rate of 5 ml/kg/hr intravenously to maintain adequate perfusion and circulation. The TLK complex [tramadol (tramadol loading dose (2 mg/kg) and infusion of tramadol (1.3 mg/kg/hour), lidocaine (3 mg/kg/hour, 2% Lidocaine Inj, Jeil Pharmaceutical Co., Korea), and ketamine (0.6 mg/kg/hour, Ketamine HCl Injection Huons, HUONS Co., Korea)] (1 ml/hr IV by constant rate infusion) was administered for pain control; cefotaxime IV (20 mg/kg TID) and metronidazole (10 mg/kg IV, q12h) were administered for secondary infection; and famotidine (0.5 mg/kg, q12h, IV, Gaster, Donga ST, Korea) was administered for gastrointestinal protection for three days during hospitalization. The open wound was managed by applying sugar twice a day. Three days after injury, a surgical procedure was carried out to remove the necrotic tissue in the right forelimb, which had lacerations, and to reconstruct the skin. In addition, Hartman-D (Hartman-D Solution 500 mL, HK inno. N Corp, Korea) was administered at an infusion rate of 5 ml/kg/hr intravenously to maintain adequate perfusion and circulation during surgery.
2.2. Preoperative Management and Anesthesia for Skin Reconstruction
Cefazolin (25 mg/kg, q12h, Cefazolin Inj. Chong Kun Dang Pharm, Korea), and meloxicam (0.1 mg/kg, q24h, Meloxicam inj., Boehringer Ingelheim Vetmedica GmbH, Germany) was injected intravenously and subcutaneously for premedication. Propofol (10 mg/kg, Provive, Myungmoon Pharm, Korea) was injected intravenously for anesthesia induction. Prior to surgery, betadine (povidone iodine, Sungkwang Pharm., Korea) was applied to the surgical site, and after 20 minutes, the beta band was removed with 70% alcohol, and the affected area was thoroughly disinfected. Next, a sterile surgical cloth was used to widely cover the affected area to prevent contamination. Cefazolin was injected intravenously. Butorphanol (0.1 mg/kg, Myungmoon Pharm Co., Korea) was administered as a premedication for anesthesia. Propofol (10 mg/kg, Provive, Myungmoon Pharm, Korea) was injected intravenously as a preanaesthetic for tracheal intubation, and the dog was placed in the dorsal recumbency position for surgery.
After intubation using an endotracheal tube (Rushelit, size ID 3.5 mm, OD 5.3 mm, Teleflex, Malaysia), general anesthesia was induced with isoflurane (Ifran, Hana Pharm, Korea) by forced breathing circulation using a respiratory anesthetic machine (Drager primus, Dragerwerk AG & Co. KGaA, Germany) with a volume of 20 to 30 cc. In addition, normal saline (a 100 ml bag of saline, Sejung Korea, Korea) was administered intravenously to maintain adequate perfusion and circulation during surgery. In addition, normal saline (a 100 ml bag of saline, Sejung, Korea) was administered intravenously at an infusion rate of 5 ml/kg/hr to maintain adequate perfusion and circulation during surgery.
2.3. Surgical Procedures and Postoperative Management
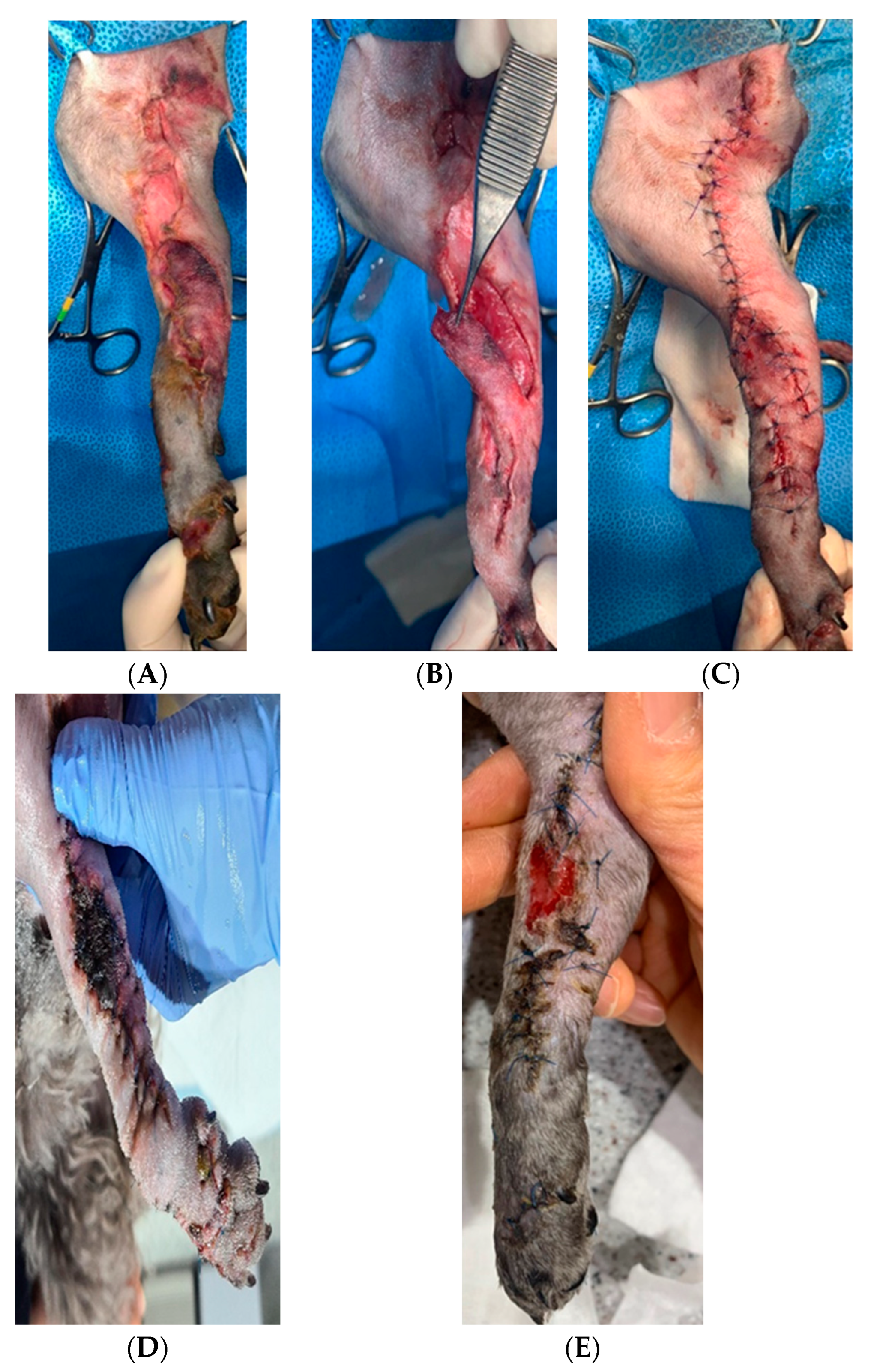
The skin had a long open wound from the axillary part to the carpal joint medially. There were some black necrotizing tissues around the periphery of the skin (
Figure 2A). The blackened necrotizing skin tissue was trimmed for suturing, and the spare tissue was identified to align the apposition (
Figure 2B). The skin was sutured in a reverse Y-shape with 4–0 nylon sutures in an interrupted suture pattern (
Figure 2C). Postoperative analgesia was induced with gabapentin (10 mg/kg, q12h, Gabalep Cap., Chong Kun Dang Pharmaceutical Corp., Korea) and tramadol (2 mg/kg, Tridol Inj. Wuhan Corp, Korea) every 12 hours for 5 days. Prophylactic intravenous antibiotics, cefazolin (25 mg/kg, q12h, IV, cefazolin inj., Chong Kun Dang Pharmaceutical Corp., Korea) and famotidine were used for gastric protection twice a day for five days.
Two days after surgery, the middle of the sutures turned black, and necrosis continued to progress (
Figure 2D). The forearm was also swollen, and serous exudate was observed between the sutures. Sugar dressing was applied to the necrotizing tissues. Ten days after surgery, the necrotic area was naturally detached, and a healthy granulation bed was identified. The skin was then epithelialized at the periphery and showed no signs of infection or complications (
Figure 2E). Fifteen days after surgery, the open wound on the skin was fully repaired.
2.4. Surgical Intervention for an Ulnar Bone Autograft
Weight-bearing was not possible due to the loss of the radial bone in the right forelimb. The dog underwent surgical intervention with cortical bone autografts seven days after discharge. The blood test results were unremarkable. The entire process of anesthesia induction, the type and dose of drugs administered, and the disinfection procedure for surgery were performed in the same manner as in skin reconstruction. To promote osteogenic properties, the cranial surface of the right proximal humerus was clipped and disinfected to collect cancellous bone. Both forelimbs were also clipped and disinfected at the same time.
2.5. Intraoperative Procedure
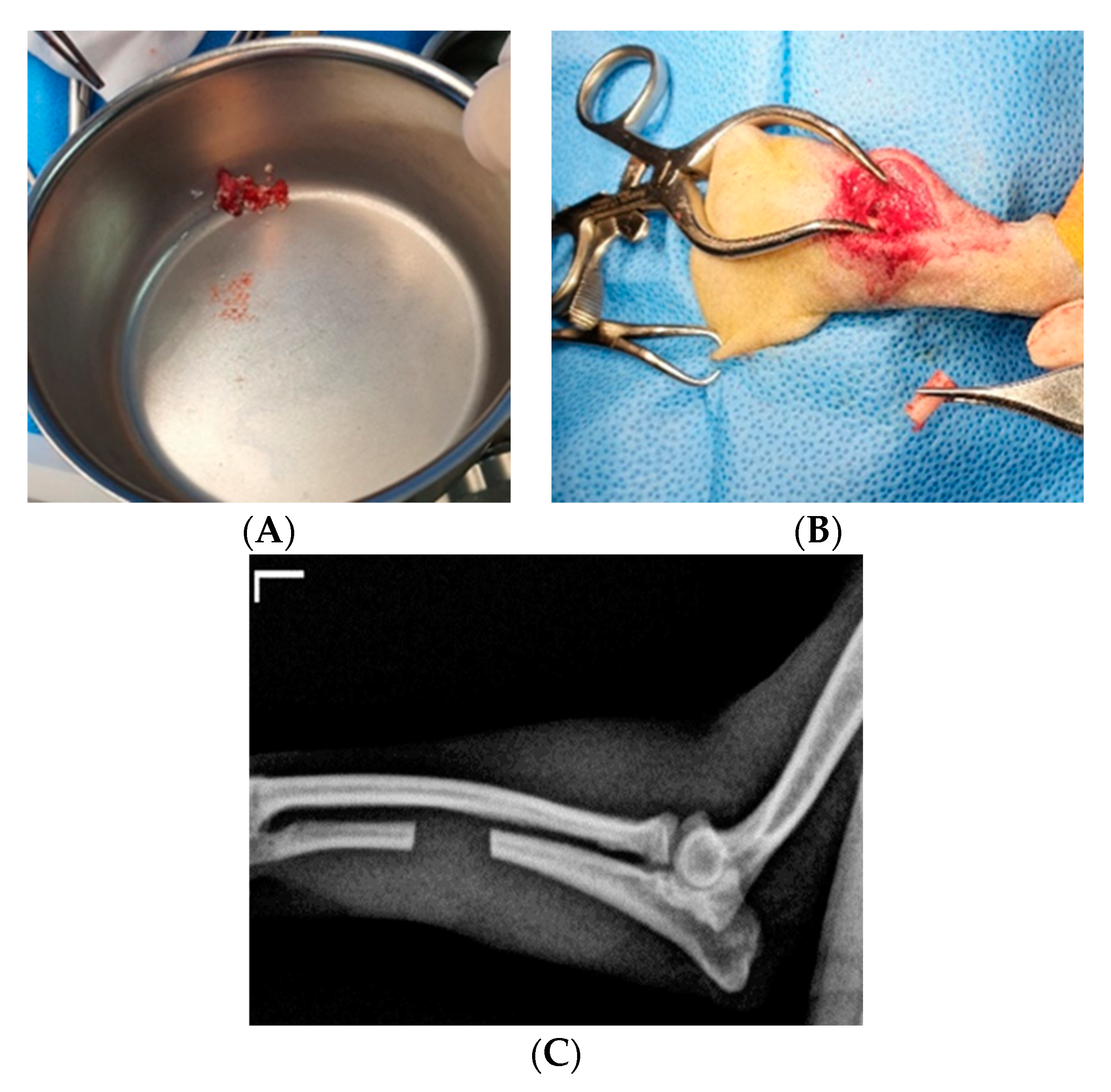
First, the dog was anesthetized and placed in the left lateral recumbency position to collect cancellous bone grafts. The skin was dissected to loosen the fascia to expose the greater tubercle of the humerus and the tendon of the insertion of the infraspinatus. The entry point was located immediately cranial to the insertion of the infraspinatus tendon. The first hole was created using a 1.5 drill bit. Then, the hole in the humerus was extended through the thin cortical bone by using a bone curette. The cancellous bone was then collected. It was stored with recombinant human bone morphogenetic protein-2 (rhBMP-2, Novosis, Dewoong Pharmaceutical Company, Seoul, Korea) until it was transplanted into a sterilized bowl with blood-soaked gauze (
Figure 3A). The subcutaneous tissues and skin were closed.
For autologous ulnar transplantation, 15 mm of the diaphysis of the ulna was collected through an incision in the middle of the left forearm using a sagittal saw (Stryker TPS System, Stryker, Kalamazoo, Michigan, United States) (
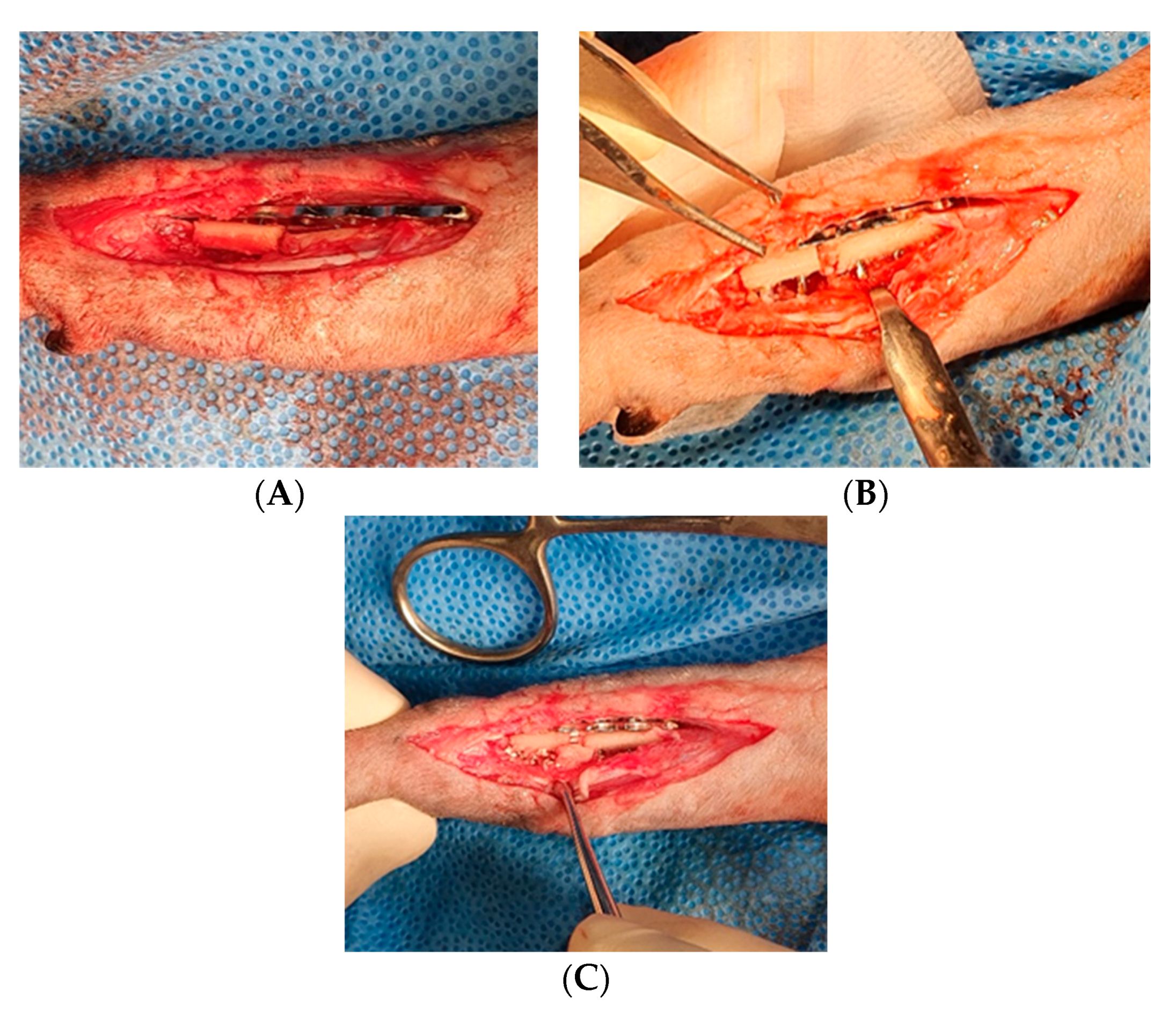
Figure 3B and C). The collected ulnar bone was protected with gauze soaked in saline until transplantation. The incision in the left forearm was routinely sutured. A cranial lateral approach to the right forearm was used for the transplantation of the radius bone defect. The edge of the atrophied bone was arranged using a single bone rongeur (12 cm, Mabson Industry, Pakistan), and the bone marrow cavity was widened using a 1.2 mm K-wire (1.2 mm×229 mm, General Vet Products, Australia). A 1.5 mm titanium T-shaped plate (Radius Reduction Plate TH type, Doiff, Korea) was placed on the bone defect to check its size (
Figure 4A), one 1.5 mm screw was inserted into the proximal radius bone, and the remaining 1.5 mm screws were inserted alternately into the collected ulnar bone and radius bone. It was inserted through the cortical bone opposite to the ulnar and radius bone (
Figure 4B). Cancellous bone collected from the nonaffected humerus and BMP were transplanted at both ends of the fractured radius bone and around the ulnar bone fragments (
Figure 4C). The muscles, subcutaneous tissue, and skin were routinely sutured.
2.6. Postoperative Management and Radiographic Evaluation
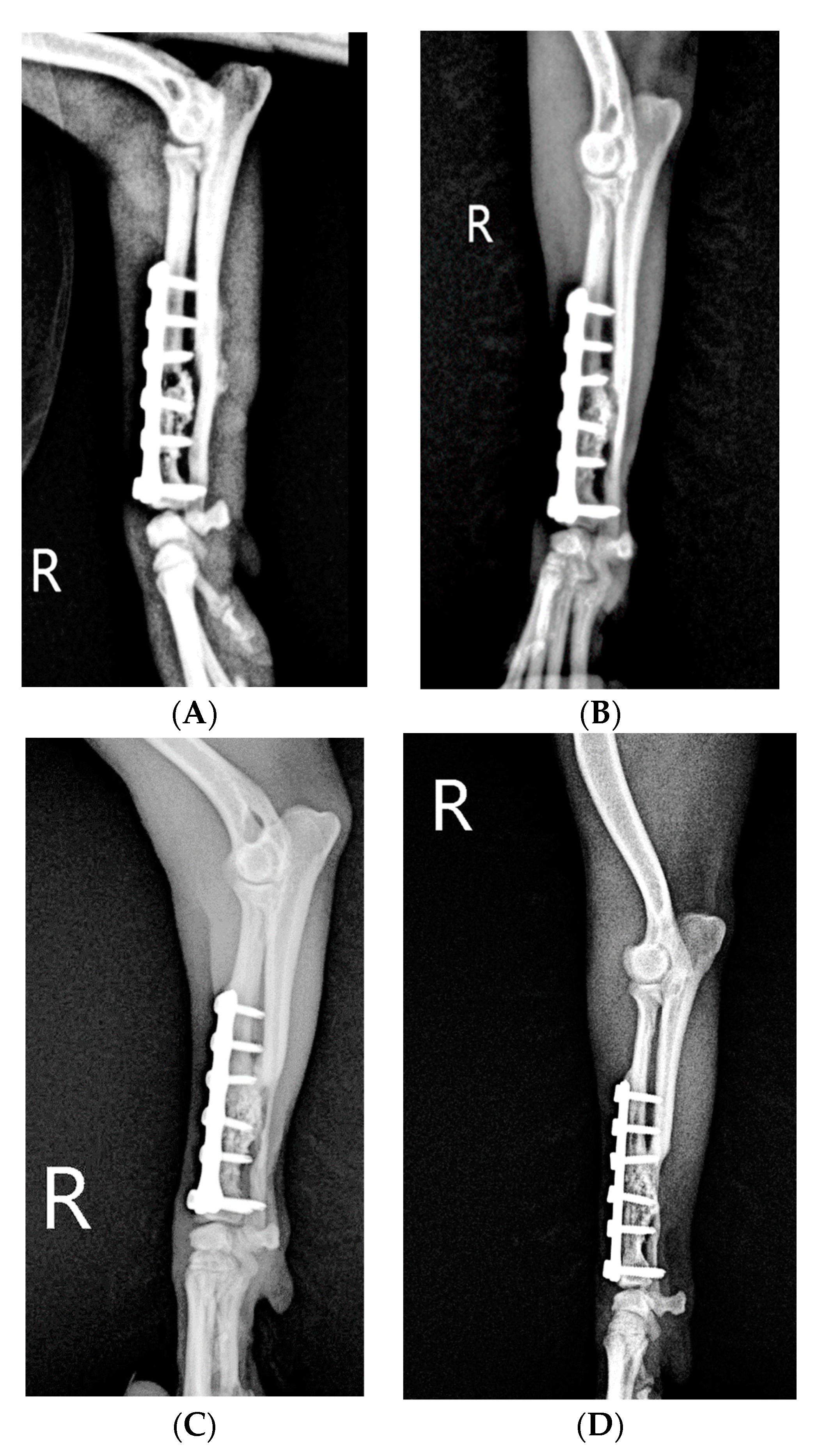
A Robert Johnson bandage was applied for two weeks and then replaced every three days to check for skin healing and edema. Tramadol (2 mg/kg) and cefazolin (22 mg/kg) were administered intravenously for 3 days as pain controls and antibiotics, respectively. Subsequently, cephalexin 22 mg/kg (25 mg/kg, q12h, Cephalexin cap. Ildong Pharm, Korea), famotidine 0.5 mg/kg (0.5 mg/kg, q12h, Gaster, Donga ST, Korea), tramadol 2 mg/kg, and streptokinase 0.5T were prescribed as oral drugs for 5 days. After discharge, the dog was presented once every three days to check her condition and to undergo laser treatment. The owner was asked to restrict activity at home per the surgeon’s instructions. The dog was not allowed to bear weight on postoperative day 1, and there was BMP and autogenous cancellous bone around the transplanted ulnar (
Figure 5A).
Slight weight bearing was allowed on postoperative day 65. On postoperative day 65, the callus was more abundant than before, the autologous ulnar bone fragment was fused with the existing radius, and the implant was stable. (
Figure 5B). On postoperative day 142, the callus at the fracture end had invaded the ulnar bone fragments grafted in the fracture gap and was much thicker than before the initial presentation. Slight lameness was still observed upon walking and trotting (
Figure 5C). On postoperative day 233, the transplanted ulnar bone was stable, with further increased radiopacity at both ends on the ventral side of the plate. There was no longer any lameness upon walking (
Figure 5D).
3. Discussion
This patient presented with a full-thickness skin defect and bone loss with radial fracture following bicycle trauma. This report describes the repair of the radial bone using an ulnar cortical bone graft and an advancement flap for the reconstruction of a skin defect of the medial forelimb at the elbow level. The mobile skin of dogs and cats lends to large pedicles or free grafts; therefore, several strategies exist for closing wounds on the trunk and extremities. In dogs and cats, reconstructive techniques used for repairing skin defects using skin fold advancement flaps have been described [
14]. In this case, some necrotic tissue was surgically debrided from the forearm, and reconstruction was attempted with an advancement flap of viable tissue retrieved dorsally, as shown in
Figure 2A and 2C. In a study of skin reconstruction with axial flaps in 73 dogs and cats, 64 dogs suffered adverse events, with necrosis occurring in 23 of them [
15].
As shown in
Figure 2D, necrosis developed in the flap-applied area on postoperative day 2, but the treatment strategy involved a second intervention involving the use of sugar. In secondary intent healing, the process of epithelialization involves the migration of epithelial cells from the epithelial edge across the wound surface [
16]. Numerous techniques for managing contaminated wound beds have been described in veterinary literature. The application of sugar to contaminated wounds has a good effect [
17]. It has been suggested that the increase in osmolarity caused by the use of sugar causes a decrease in free water available for bacterial replication, which inhibits bacterial growth and stimulates the influx of macrophages and lymphatic fluid, which promotes granulation tissue formation and epithelialization [
18].
Figure 2e shows that sugar promoted second intention healing, as a result of necrotic tissue removal and epithelialization on day 10 of the sugar therapy intervention. In this study, an autologous cortical bone fragment (15 mm in diameter) from the ulna was used as a graft and implanted into the midshaft of the contralateral missing radius. In dogs, the iliac crest, proximal humerus, and proximal tibia are considered the most plentiful sources of autologous cancellous bone [
19].
In some cases, autogenous bone graft procedures may not result in adequate healing due to sequestration or resorption of the grafted bone [
20]. BMPs enhance the osteoinductivity of autologous bone grafts and stimulate osteoblast proliferation, and the combination of BMPs and cancellous bone grafting may improve bone healing more effectively than either treatment alone [
21]. The use of coccyx as an autogenous bone graft has proven to be an excellent option for the treatment of femoral fracture nonunion. In addition to proper mechanical fixation, various adjunctive methods, including BMPs, may be useful for increasing the engraftment of autogenous bone [
13].
In this study, the radial midshaft of the right forearm was lost in a bicycle accident. Opposite midshaft ulnar bone with BMPs and autologous cancellous bone for grafting were used for bone union. A fairly good amount of callus was evident in the bone graft area. Radiographs were taken immediately after fracture repair and bone grafting to assess the bone gap and bridging of the fractured ends. In this case, the gap was filled well, and there was good alignment of the fractured ends, indicating that the bone graft was stable.
According to the radiographs taken on day 65, a callus clearly emerged from the fracture ends in the bone graft area, but the whole bone graft area was not covered by the bony density. Even though the interfragmentary space was checked proximally, the screw fixed between the fragment and plate was well maintained. Moreover, on day 142, the density of the fragments increased, indicating that they were fused. The callus from the fracture ends seemed to be mixed with the ulnar bone graft, BMP and cancellous bone in the fracture gap. This shows that cortical bone fragments were resorbed and replaced by the callus from fracture ends at a faster rate according to the radiograph obtained on day 65, in which the bone graft area was not covered by bony density even on the radiograph obtained on day 60. Four months after grafting, the dog was instructed to keep the limb off the ground or to intermittently support the limb at the toe with slight weight bearing. Eventually, the dog was eventually able to perform activities of daily living with full weight bearing. These results also support clinical evidence that fragmented ulnar bone fragments are not rejected as foreign bodies. However, further histologic and histochemical studies may be needed to determine their role in osteoinduction and osteogenesis.Authors should discuss the results and how they can be interpreted from the perspective of previous studies and of the working hypotheses. The findings and their implications should be discussed in the broadest context possible. Future research directions may also be highlighted.
4. Conclusions
Despite some limitations, the use of autologous ulnar grafts has proven to be an excellent option for replacement material in cases of radial bone loss. In addition to proper mechanical fixation, various supplementary methods, such as BMP and autogenous cancellous bone, can be useful for enhancing the engraftment rate of autologous bone. This is a report of an autologous ulna implanted into a dog with radial bone loss, where the grafted bone healed successfully and eventually allowed the patient to regain mobility.
Author Contributions
Conceptualization, S.H. L., J.H.S. and J.H.C.; methodology, S.H.L. and J.H.S .; investigation, S.H.L., J.H.S. and J.H.C.; data curation, S.H. L., J.H.S. and J.H.C.; writing—original draft preparation, S.H.L. and J.H.C.; writing—review and editing, S.H. L. and J.H.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the animals’ owners to permit examination, surgery, and treatment. Additional consent was obtained for using the images for research purposes.
Data Availability Statement
The data presented in the study are available on request from the corresponding author. The data are not publicly available due to ethical and privacy concerns.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Repellin, R.L.; Pitt, K.A.; Lu, M.; Welker, J.; Noland, E.L.; Stanley, B.J. The effects of a proprietary Manuka honey and essential oil hydrogel on the healing of acute full-thickness wounds in dogs. Vet Surg. 2021, 50, 1634–1643. [Google Scholar] [CrossRef] [PubMed]
- Crowley, J.D.; Hosgood, G.; Appelgrein, C. Seed skin grafts for reconstruction of distal limb defects in 15 dogs. Journal of Small Animal Practice. 2020, 61, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Swaim, S.F. Skin grafts. Vet. Clin. North Am. Small Anim. Pract. 1990, 20, 147–175. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.W.; Fowler, J.D.; Bowen, C.V.A.; Chang, P. Experimental and clinical free cutaneous transfers in the dog. Microsurgery 1991, 12, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Prpich, C.Y.; Santamaria, A.C.; Simcock, J.O.; Wong, H.K.; Nimmo, J.S.; Kuntz, C.A. Second intention healing after wide local excision of soft tissue sarcomas in the distal aspects of the limbs in dogs: 31 cases (2005-2012). Journal of the American Veterinary Medical Association. 2014, 244, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Johnston, D.E. Care of accidental wounds. Vet Clin North Am Small Anim Pract. 1990, 20, 27–46. [Google Scholar] [CrossRef] [PubMed]
- Martinez, S.A.; Walker, T. Bone grafts. Vet Clin North Am Small Anim Pract. 1999, 29, 1207–1219. [Google Scholar] [CrossRef] [PubMed]
- Frölke, J.P.M.; Patka, P. Definition and classification of fracture non-unions. Injury. 2007, 38, 19–22. [Google Scholar] [CrossRef] [PubMed]
- Phillips, I.R. A survey of bone-fractures in the dog and cat. J Small Anim Pract. 1979, 20, 661–674. [Google Scholar] [CrossRef] [PubMed]
- Kerwin, S.C.; Lewis, D.D.; Elkins, A.D.; Oliver, J.; Pechman, R.; McCarthy, R.J.; Hosgood, G. Deep frozen allogeneic cancellous bone grafts in 10 dogs: A case series. Vet Surg. 1996, 25, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Johnston, S.; Tobias, K. Veterinary Surgery: Small Animal Expert Consult, 2nd ed.; Saunders. 2012, 676–684.
- Sheller, M.R.; Crowther, R.S.; Kinney, J.H.; Yang, J.; Di Jorio, S.; Breunig, T.; Carney, D.H.; Ryaby, J.T. Repair of rabbit segmental defects with the thrombin peptide, TP508. J Orthop Res. 2004, 22, 1094–1099. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.; Lee, K.; Kang, K.; Kim, M. Treatment of a Large Defect Induced by Atrophic Nonunion of Femoral Fracture in a Dog with Autogenous Coccygeal Bone Grafting. Vet Sci. 2023, 10, 388. [Google Scholar] [CrossRef] [PubMed]
- Hunt, G.B.; Tisdall, P.L.; Liptak, J.M.; Beck, J.A.; Swinney, G.R.; Maliket, R. Skin-fold advancement flaps for closing large proximal limb and trunk defects in dogs and cats. Vet Surg. 2001, 30, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Field, E.J.; Kelly, G.; Pleuvry, D.; Demetriou, J.; Baines, S.J. Indications, outcome and complications with axial pattern skin flaps in dogs and cats: 73 cases. J Small Anim Pract. 2015, 56, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Pastar, I.; Stojadinovic, O.; Yin, N.C.; Ramirez, H.; Nusbaum, A.G.; Sawaya, A.; Patel, S.B.; Khalid, L.; Isseroff, R.R.; Tomic-Canic, M. Epithelialization in wound healing: a comprehensive review. Advances in Wound Care. 2014, 3, 445–464. [Google Scholar] [CrossRef] [PubMed]
- Mathews, K.A.; Binnington, A.G. Wound management using sugar. Comp Cont Educ Pract Vet. 2002, 24, 41–50. [Google Scholar]
- Wells, S.; Gottfied, S.D. Utilization of the scrotum as a full thickness skin graft in a dog. Can Vet J. 2010, 51, 1269–1273. [Google Scholar] [PubMed]
- Penwick, R.C.; Mosier, D.A.; Clark, D.M. Healing of canine autogenous cancellous bone graft donor sites. Veterinary Surgery 1991, 20, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.L.; Houlton, J.; Vannini, R. AO Principles of Fracture Management in the Dog and Cat. Thieme. 2005, 81–88. [Google Scholar]
- Bharadwaz, A.; Jayasuriya, A.C. Osteogenic differentiation cues of the bone morphogenetic protein-9 (BMP-9) and its recent advances in bone tissue regeneration. Mat. Sci. Eng. C-Mater. 2021, 120, 111748. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).