Submitted:
08 July 2024
Posted:
09 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Selection Criteria
- -
- Population: Person in a palliative situation, family members/caregivers.
- -
- Concept: Dimensions of communication and management of bad news in nursing.
- -
- Context: Inpatient, outpatient, and home units.
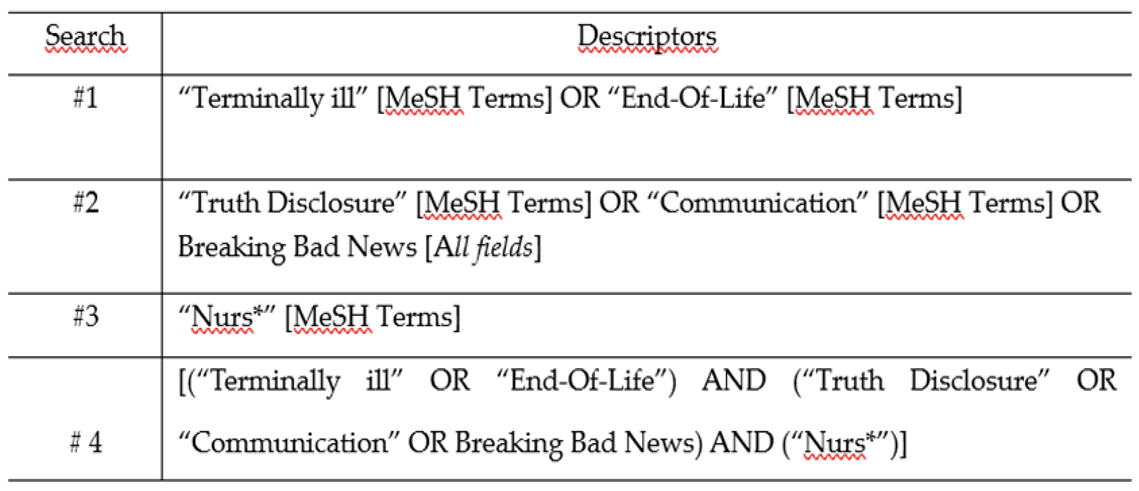
2.2. Search Strategy
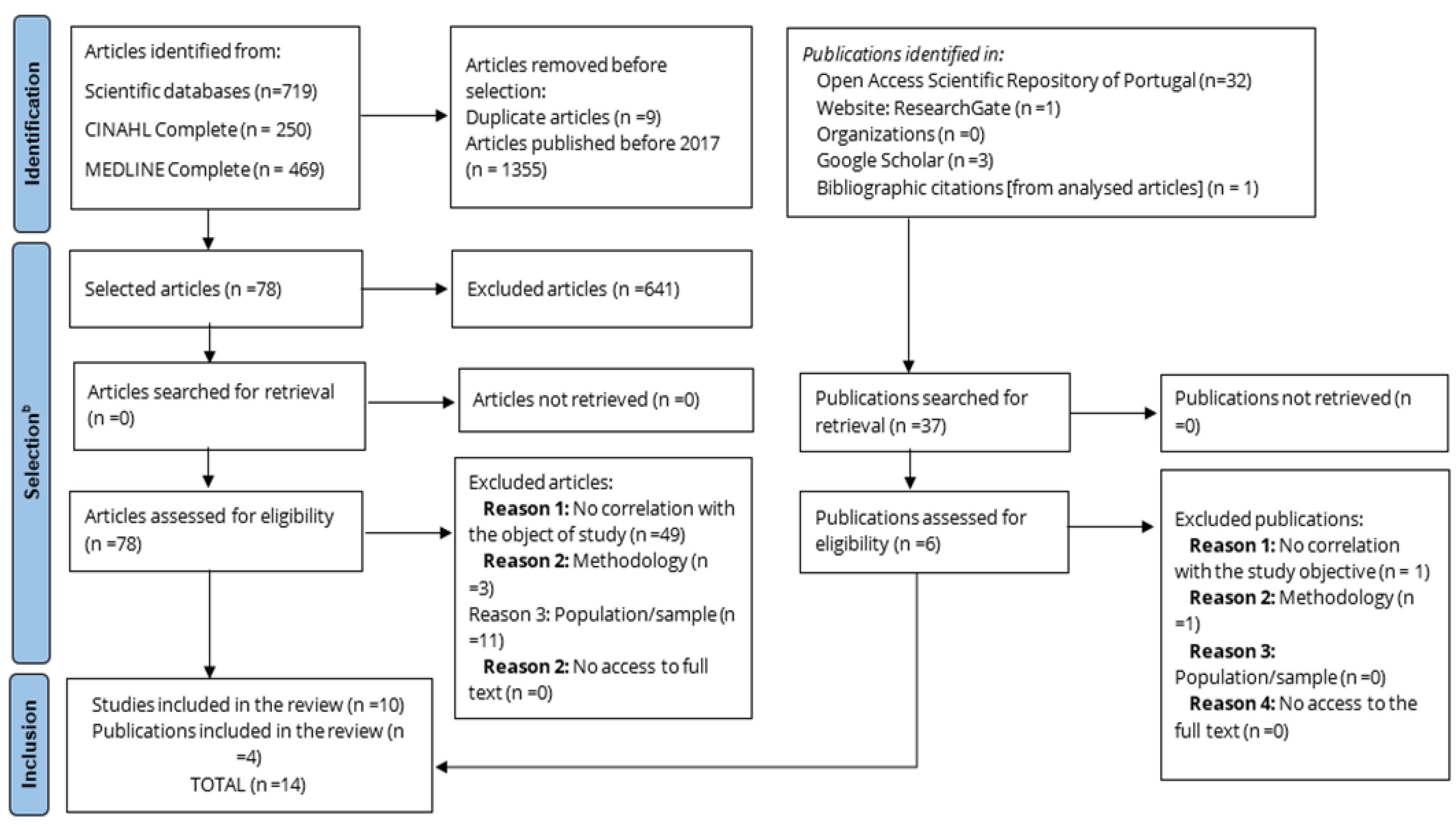
2.3. Selection Process and Article Eligibility Criteria
3. Results
3.1. Characteristics of Included Studies, Context, And Population
3.2. Data Presentation
4. Discussion
4.1. Dimensions of Structure of Communication and Management of Bad News
4.2. Dimensions of Process of Communication and Management of Bad News
4.3. Dimensions of Outcome of Communication and Management of Bad News
4.4. Limitations and Suggestions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- World Health Organization. Palliative Care factsheets [Internet]. 2020 [cited 2023 Nov 2]. Available online: https://www.who.int/news-room/fact-sheets/detail/palliative-care.
- World Health Organization. Palliative Care Key Facts [Internet]. 2023 [cited 2023 Nov 3]. Available online: https://www.who.int/europe/news-room/fact-sheets/item/palliative-care.
- Ezer T, Lohman D, de Luca GB. Palliative Care and Human Rights: A Decade of Evolution in Standards. J Pain Symptom Manage [Internet]. 2018, 55, S163–9. [CrossRef]
- Lei 52/2012. Lei de Bases dos Cuidados Paliativos [Internet]. Assembleia da Republica, Serie I; 2012 p. 5119–24. Available online: https://data.dre.pt/eli/lei/52/2012/09/05/p/dre/pt/html.
- Harding Z, Hall C, Lloyd A. Rehabilitation in palliative care: a qualitative study of team professionals. BMJ Support Palliat Care [Internet]. 2022, 12, 28–38. [CrossRef]
- Silva R, Paiva M, Vital F, Moura MJ, Lourenço J, Lopes JM. Plano Estratégico para o Desenvolvimento dos Cuidados Paliativos 2021-2022 2 Comissão Nacional de Cuidados Paliativos: Com o contributo dos Coordenadores Regionais: Ordem dos Médicos Ordem dos Enfermeiros Ordem dos Psicólogos [Internet]. 2021. Available online: https://www.acss.min-saude.pt/wp-content/uploads/2017/01/PEDCP-2021_2022.pdf.
- Querido A, Salazar H, Neto IG. Comunicação. In: Barbosa A, Pina PR, Tavares F, Neto IG, editors. Manual de Cuidados Paliativos. 3rd ed. Lisboa: Faculdade de Medicina de Lisboa; 2016. p. 815–31.
- Kwame A, Petrucka PM. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs. 2021, 20, 1–11.
- McCormack B, McCance T. Person-centred Practice in Nursing and Health Care: Theory and Practice. 2nd ed. Wiley Blackwell; 2017.
- Alfriyie, D. Effective Communication between nurses and patients: an evolutionary concept analysis. Brittish J Community Nurs. 2020, 7, 505–512. [Google Scholar]
- Mehnert A, Koranyi S. Kommunikation mit schwerstkranken Patienten – mehr als nur Breaking Bad News. Ther Umschau [Internet]. 2022, 79, 29–35. [CrossRef]
- Pontes AC, Leitão IMTA, Ramos IC. Comunicação terapêutica em Enfermagem: instrumento essencial do cuidado. Rev Bras Enferm. 2008, 61, 312–318.
- Wittenberg-Lyles E, Goldsmith J V., Ferrell BR, Ragan SL, Oxford University Press. Communication in Palliative Nursing. Druk: Oxford University Press; 2017.
- Dahlin C, Wittenberg E. Communication in Palliative Care. In: Ferrell BR, Paice JA, editors. Oxford Textbook of Palliative Nursing. 5th ed. Oxford: Oxford University Press; 2020. p. 55–77.
- Sánchez AR, Beltrán MJM, Arribas Marín JM, de la Torre-Montero JC, Gil BB, García M del CM, et al. The Communication of Bad News in Palliative Care: The View of Professionals in Spain. Am J Hosp Palliat Med. 2023, 1–12.
- Al-Johani WM, Alshamlan NA, Alghamdi MF, Alabdulkader AM, Aljohani WM, Alghamdi RF, et al. Breaking Bad News of a Cancer Diagnosis: A Mixed-Methods Study of Patients’ Perspectives. Patient Prefer Adherence. 2022, 16, 3357–3369.
- Kumar V, Sarkhel S. Clinical practice guidelines on breaking bad news. Indian J Psychiatry. 2023;65(2):238.
- Arber A, Gallagher A. Breaking bad news revisited: the push for negotiated disclosure and changing practice implications. Int J Palliat Nurs. 2003, 9, 166–172.
- Wahyuni S, Gautama MSN, Simamora TY. A Literature Review of Nurses Challenges and Barriers in Assisting Patients and Families Facing Breaking Bad News. Indian J Palliat Care. 2023, 29, 243–249.
- Ptacek JT, Ptacek JJ, N. M. E. I’m sorry to tell you..." - Physicians’ reports of breaking bad news. J Behav Med [Internet]. 2001, 24, 205–217. [CrossRef]
- Koch A, Mantzouris S. Nurses’ Role in Providing Comprehensive Communication, Prognostication, and Palliative Care During the COVID-19 Pandemic. J Hosp Palliat Nurs [Internet]. 2020, 22, 442–446, Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=mdc&AN=32947392&lang=pt-pt&site=ehost-live.
- Hernández-Marrero P, Fradique E, Pereira SM. Palliative care nursing involvement in end-of-life decision-making: Qualitative secondary analysis. Nurs Ethics [Internet]. 2019, 26, 1680–1695, Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=mdc&AN=29807491&lang=pt-pt&site=ehost-live.
- Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020, 18, 2119–2126.
- Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis [Internet]. JBI; 2020. [CrossRef]
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018, 169, 467–473.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021, 372.
- Aromataris E, Munn Z. JBI Manual for Evidence Synthesis. 2020.
- Rylander A, Fredriksson S, Stenwall E, Gustafsson LK. Significant aspects of nursing within the process of end-of-life communication in an oncological context. Nord J Nurs Res [Internet]. 2018, 39, 85–91, Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=ccm&AN=136876626&lang=pt-pt&site=ehost-live.
- Yazdanparast E, Arasteh A, Ghorbani SH, Davoudi M. The effectiveness of communication skills training on nurses’ skills and participation in the breaking bad news. Iran J Nurs Midwifery Res. 2021, 26, 337–341.
- Kerr D, Milnes S, Ammentorp J, McKie C, Dunning T, Ostaszkiewicz J, et al. Challenges for nurses when communicating with people who have life-limiting illness and their families: A focus group study. J Clin Nurs [Internet]. 2019, 29, 416–428, Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=ccm&AN=141095716&lang=pt-pt&site=ehost-live.
- Gonella S, Basso I, Clari M, Dimonte V, Di Giulio P. A qualitative study of nurses’ perspective about the impact of end-of-life communication on the goal of end-of-life care in nursing home. Scand J Caring Sci [Internet]. 2020, 35, 502–511, Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=ccm&AN=150251590&lang=pt-pt&site=ehost-live.
- Toh SW, Hollen VT, Ang E, Lee YM, Devi MK. Nurses’ communication difficulties when providing end-of-life care in the oncology setting: a cross-sectional study. Support Care Cancer [Internet]. 2020, 29, 2787–2794, Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=mdc&AN=32997186&lang=pt-pt&site=ehost-live.
- Francis L, Robertson N. Healthcare practitioners’ experiences of breaking bad news: A critical interpretative meta synthesis. Patient Educ Couns. 2023, 107, 107574.
- Lukewich JA, Tranmer JE, Kirkland MC, Walsh AJ. Exploring the utility of the Nursing Role Effectiveness Model in evaluating nursing contributions in primary health care: A scoping review. Nurs Open. 2019, 6, 685–697.
- Kimura Y, Hosoya M, Toju K, Shimizu C, Morita T. Barriers to end-of-life discussion with advanced cancer patient as perceived by oncologists, certified/specialized nurses in cancer nursing and medical social workers. Jpn J Clin Oncol [Internet]. 2020, 50, 1426–1433, Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=mdc&AN=32844993&lang=pt-pt&site=ehost-live.
- Alshammari F, Sim J, Lapkin S, McErlean G. Registered Nurses’ attitudes towards end-of-life care: A sequential explanatory mixed method study. J Clin Nurs [Internet]. 2023, 32, 7162–7174, Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=ccm&AN=172046230&lang=pt-pt&site=ehost-live.
- Fuoto A, Turner KM. Palliative Care Nursing Communication: An Evaluation of the COMFORT Model. J Hosp Palliat Nurs [Internet]. 2019, 21, 124–130, Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=ccm&AN=135343052&lang=pt-pt&site=ehost-live.
- Gonella S, Conti A, Albanesi B, Antal A, Dimonte V, Di Giulio P. Lived experiences of end-of-life communication among nursing home staff: An interpretive phenomenological study. J Adv Nurs [Internet]. 2022, 79, 698–710, Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=ccm&AN=161474312&lang=pt-pt&site=ehost-live.
- Ibañez-Masero O, Carmona-Rega IM, Ruiz-Fernández MD, Ortiz-Amo R, Cabrera-Troya J, Ortega-Galán ÁM. Communicating Health Information at the End of Life: The Caregivers’ Perspectives. Int J Environ Res Public Health [Internet]. 2019, 16, 2469, Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=mdc&AN=31336698&lang=pt-pt&site=ehost-live.
- Tang, Y. Death attitudes and truth disclosure: A survey of family caregivers of elders with terminal cancer in China. Nurs Ethics [Internet]. 2018, 26, 1968–1975, Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=mdc&AN=30428754&lang=pt-pt&site=ehost-live. [Google Scholar] [CrossRef]
 |
| Author(s)/ Publication year/ Country |
Objective/ Aim |
Methods |
Population under study Sample composition Context of care |
Dimensions of communication and management of bad news carried out by nurses, to the readaptation in palliative care |
|---|---|---|---|---|
| Alshammari et al. (2023) [28] Saudi Arabia |
To examine nurses' attitudes towards end-of-life care and explore barriers and facilitating factors that influence the provision of quality end-of-life care. | Mixed methods. (Data collection instruments: questionnaire and semi-structured interviews) |
1293 nurses in a hospital context Inpatient services: internal medicine, surgery, cardiology, oncology and palliative care in five major hospitals. |
Research indicates that nurses exhibit confidence and readiness in administering end-of-life care, yet they express a lack of preparedness in effectively communicating about end-of-life matters and managing associated emotions. Their deficient communication skills present a notable barrier to delivering high-quality end-of-life care. Furthermore, there is a demonstrable absence of experience and assurance in initiating nuanced conversations that navigate the delicate balance between fostering optimism and conveying challenging realities. |
| Fuoto & Turner (2019) [29] United Satates of America) |
Implement the COMFORT communication model to increase nurses' confidence and satisfaction in end-of-life communication and improve patient-family satisfaction with the care provided after implementing the COMFORT model. |
Mixed methods. (Data collection instrument: questionnaire) |
19 nurses working in a long-term palliative care inpatient unit. 50 family members of people living in an inpatient unit who had died, within a certain time limit. |
Training nurses in communication using the COMFORT model has been shown to increase their confidence and satisfaction when interacting with end-of-life clients. The potential of the COMFORT model extends beyond end-of-life care and could be utilized in other areas of nursing to develop skills necessary for facilitating care approaches. |
| Tang (2018) [30] China |
Describe the attitudes of family caregivers towards death and revealing the truth. | Quantitative study (Data collection instrument: questionnaire survey) |
140 caregivers/ family members of elderly people with terminal cancer admitted to long-term care units | Ineffective communication of content related to the end of life results from the lack of discussion with family caregivers about this topic as well as their difficulty in managing bad news related to the end of life of their family members. Family caregivers perceive the training of health professionals in communicating and managing bad news as being fundamental; They also understand that training in this area influences how each health professional approaches bad news situations in their daily practice. |
| Gonella et al. (2020) [31] Italy |
Explore nurses’ perspectives on how communication influences end-of-life care planning in long-term care. | Qualitative descriptive study (Data collection instrument: semi-structured interviews) |
14 nurses working in different long-term care institutions and involved in caring for residents during their last week of life. | Factors that influence the quality of communication at the end of life: life crises/transitions (physical deterioration; social problems, multiple hospitalisations and warning shots); person-centred environment; occasion of addressing the possibility of death, quality of relationships and culture of care. |
| Gonella et al. (2022) [32] Italy |
Explore and understand experiences about end-of-life communication among professionals in long-term care institutions. | Qualitative study (Data collection instrument: semi-structured interviews) |
21 multidisciplinary team members involved in end-of-life communication in long-term care institutions. |
Factors that hinder communication at the end of life: difficulty in managing feelings and emotions (of oneself and of family members/caregivers); high workload and inadequate professional/institutionalized individual ratio. Teamwork as a facilitator of the quality of communication at the end of life: promotes reflection on the quality of communication; facilitates the management of feelings, emotions and complex situations; facilitates time management for communication and allows families/caregivers to prepare for death. |
| Toh et al. (2020) [33] Singapore |
Examine communication difficulties experienced by nurses when providing end-of-life care; establish a correlation between communication difficulties and the participants and determine the impact of sociodemographic factors on the communication difficulties experienced. | Quantitative study (Data collection instrument: cross-sectional questionnaire survey) |
124 nurses working in four oncology inpatient units of a hospital. | Nurses experience greater difficulties in communicating with the person in a palliative situation/ family/ caregiver than with the multidisciplinary team, however, when difficulties are experienced in communicating with the multidisciplinary team, these are even more evident in communicating with the person in a palliative situation/ family/caregiver. Nurses who experience greater difficulty in communication are: younger, more inexperienced, have less academic training, have no training in end-of-life care and have religious practices. |
| Ibañez-Masero et al. (2019) [34] Spain |
Understand the experiences of caregivers in relation to health information and communication through the course of illness and death of family members. | Phenomenological qualitative study (Data collection instruments: unstructured interviews) |
123 caregivers accompanying people at the end of life for more than 2 months and less than 2 years | Inadequate communication of bad news causes distress for the person and their family/caregivers. Training in communicating bad news is recognized by caregivers as important and has positive repercussions on the process of illness and death. Conspiracy/Pact of silence: greater suffering, isolation and complicated grief. Society's secrecy attitude towards death makes it difficult to normalize it and prepare each person for death. |
| Rylander et al. (2018) [35] Sweden |
Describe important nursing aspects in the end-of-life communication process in the context of oncological palliative care. | Qualitative, descriptive and exploratory study (Data collection instrument: semi-structured interviews) |
10 nurses working in an oncology inpatient service (acute and chronic both in active and palliative treatment) at a university hospital. | Nurses have a crucial role in all phases of the process of revealing the truth/communicating and managing bad news, having the ability to reduce anxiety and the suffering resulting from it for the person in a palliative situation, family and/or caregivers. Members of the multidisciplinary team must bring clarity to care, being interconnected in a unidirectional flow of care aimed at the person's well-being. Barriers to communicating and managing bad news: lack of information about the person's prior knowledge; single-minded focus on medical issues despite poor prognosis; revelation of the truth controlled by the medical team and lack of cooperation; non-existent or weak therapeutic relationships. |
| Kerr et al. (2019) [36] Australia |
List the communication problems that nurses consider challenging when caring for people with life-limiting illnesses | Qualitative study (Data collection instrument: focus group) |
39 nurses working in three hospital inpatient units. |
Communication problems identified: Deficit in skills for communicating bad news/complex conversations; complexity in the interaction between the professional and the families and caregivers of the person in a palliative situation; Organizational factors impede nurses' ability to have meaningful conversations with the person in a palliative situation and their caregivers/family members. |
| Kimura et al. (2020) [37] Japan |
Identify barriers to discussing the end of life with people with advanced cancer/ family members perceived by oncologists, oncology nurses and social workers; Clarify views on effective strategies to facilitate end-of-life discussion. |
Quantitative study (Data collection instrument: questionnaires) |
4354 healthcare professionals in the field of medical oncology working in 402 hospitals (494 oncologists, 993 nurses and 387 social workers) |
Barriers related to the person/family/caregivers: acceptance of a bad prognosis; understanding the limitations and complications of supportive treatments; conflicting care goals; difficulty accepting bad news as it affects previous expectations. Organizational barriers: lack of treatment protocols; lack of informative documents; lack of time for clinical discussion; lack of home support and back-up facilities; lack of private place for communication. Barriers related to healthcare professionals: lack of training in carrying out difficult conversations/ communicating bad news; lack of agreement between team members regarding the objectives of care/treatment; diagnostic uncertainty; poor communication between team members. |
| Sánchez et al. (2023) [15] Spain |
Identify the aspects associated with communicating bad news in the context of palliative care. | Descriptive cross-sectional quantitative study (Data collection instrument: online questionnaire) |
206 health professionals (102 nurses, 88 doctors and 16 psychologists) working in palliative care teams. | Referrals to palliative care teams are often initiated without adequately informing individuals in palliative situations about their diagnoses or prognoses. Barriers to effectively communicating bad news by health professionals include a lack of specific training in this area, inadequate training in the use and management of a bad news reporting protocol, challenges in maintaining a delicate balance between honesty and promoting hope, and the implications for individuals in palliative situations, as well as their caregivers and young family members. |
| Wahyuni et al. (2023) [19] Iran (n=3) USA (n=3) United Kingdom (n=4) New Zealand (n=1) Jordan (n=1) |
Understanding the role, methods, obstacles, and challenges nurses face when communicating bad news in healthcare settings. | Systematic literature review | 12 articles were included, out of a total of 1075 articles. | Nursing intervention in the process of delivering bad news includes essential steps such as preparing the individual to receive distressing information, effectively communicating the news, managing the subsequent reactions, fostering interpersonal relationships, engaging in therapeutic communication, and providing emotional support. The barriers and challenges faced by nurses in this context are primarily attributed to a lack of skills and preparedness in handling the emotional reactions of others, as well as difficulties in managing their own emotional responses and those of others. The acquisition of skills through education and training is imperative for overcoming these existing barriers and elevating the overall quality of care provided in such situations. |
| Francis & Robertson (2023) [38] USA (n=1) United Kingdom (n=3) Sweden (n=1) Canada (n=2) South Africa (n=1) Israel (n=1) Australia (n=2) Brazil (n=1) Spain (n=1) Italy (n=1 |
Provide an overview of healthcare professionals' experiences in communicating bad news. | Systematic literature review | 14 articles were included, out of a total of 1723. | Experiences in communicating and managing bad news often involve discomfort, challenging emotional regulation, and physiological responses to the delivery of negative information. Healthcare professionals may also experience emotional distress due to their empathic connection with the situations of the sick individuals and their caregivers/family members. Furthermore, inadequate communication, fear of committing errors, and a prevailing culture of invulnerability that undervalues professional self-care can exacerbate these challenges. Revealing the truth can precipitate a challenging dialogue, potentially evoking feelings of professional isolation. Failing to acknowledge this difficulty, often associated with a culture of invulnerability that discourages the open expression of emotions, can elevate the risk of burnout and exhaustion among healthcare professionals. |
| Davoudi et al. (2021) [39] Iran |
Evaluate the effect of communication training on the level of skills and participation of nurses in communicating bad news. | Semi-experimental quantitative study (Data collection instrument: questionnaires |
60 nurses working in university hospitals in a city. | Barrier to communication/participation in communicating bad news: lack of skills and knowledge. To enhance nurses' involvement in breaking bad news, it is essential for them to acquire communication skills through training. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





