1. Introduction
Maintaining quality of life for older adults is a vital component of healthy aging [
1]. Maintaining good physical and cognitive activity is essential to ensure quality of life and healthy aging [
2]. However, it is well established that as older adults age, they ordinarily disengage from social interactions, become increasingly sedentary and decline both physically and cognitively, especially in their later years [
3]. The combination of declines in real-life social interactions and increasingly sedentary lifestyles are antithetical to healthy aging among older adults, increasing the prevalence of a range of physical and cognitive ailments that decrease the quality and quantity of their lives [
2,
4].
While a sedentary lifestyle is generally frowned upon by public health experts as antithetical to healthy aging [
5,
6], some older adults might not have a choice. This can be due to injury, loss of mobility or any other ailment that may cause an older adult to remain in a sedentary activity state [
7]. Sedentary behaviours generally refer to activities that do not increase energy expenditure substantially above the resting level, for example sitting, lying down, or watching television [
8]. However, if older adults are engaged in seated activities that are associated with an increased ‘executive function’ these may result in greater positive health outcomes [
6,
8]. ‘Executive functions’(EFs) are an umbrella term that relates to higher-order cognitive processes that require focus, attention, goal orientation and the inhibition of impulses or interference [
9]. Types of seated activities can transcend passive behaviours and utilise EFs, [
6]. These can include listening to music, solving a puzzle, playing a game, or reading [
6,
10,
11]. These forms of seated activities that engage EFs can create cognitive and psychological outcomes for older adults who may not have a choice to have a sedentary lifestyle due to injury, extreme frailty, or loss of mobility [
5,
6].
2. Social Robots as Assistive Technologies
Assistive technologies are aids or devices specifically designed to help older adults who have physical or cognitive deficits [
12]. Social robots are a newer form of assistive technology, specifically designed to aid in social interactions or toward certain goals like gameplay or motivation to engage [
13]. Social robots are machines, equipped with a degree of artificial intelligence and human-like mechanics that can mimic or replicate a human interaction with a user [
14]. These interactions include touch, handshaking, greetings, verbal interactions, gameplay and recognising cues. Social robots take a variety of forms, including quasi-animals and humanoids [
14].
Social robot use among older adults is increasingly ubiquitous. The designation/setting for a social robot deployment among older adults ultimately depends on its design [
14]. As social robots’ primary function is for social interactions, their use among older adults has a pronounced focus on companionship [
15]. This was found by Sun & Liu [
16], whose research indicated an improvement in quality of life for older adults by using social robots to provide companionship. As demonstrated by Khosla et al. [
17], interactions between social robots and older people found significant improvements in observed states of well-being. This is reinforced by Ge & Schleimer [
18], whose analysis of older adults’ use and acceptance of social robots demonstrated a marked improvement in general well-being.
Other benefits and design features of social robots include their ability to engage or motivate older adults toward certain tasks or goals. These are usually called socially assistive robots (SARs) and can be deployed among older adults to aid in motivation behaviours to engage [
19]. For example, engage an older adult in an exercise routine, toward a social interaction with others or engage them in gameplay or a seated activity. This is consistent with Feil-Seifer & Mataric [
19] and Kyong et al. [
20], who demonstrated that SAR deployment among older adults can positively influence motivation to engage in an exercise routine. Furthermore, Macis et al. [
21], demonstrated that the deployment of a SAR among older adults can improve the motivation to engage and maintain a daily stretching and tai chi routine. Pharmacological disbursement is another area where SARs have been deployed with effectiveness. According to Smarr et al. [
22], reminders to take medications and management systems for medications by SARs have produced positive outcomes and a greater level of compliance among older adults.
Figure A & B.
Social Robot ‘PEPPER’ Engaging Older Adults in Meaningful Seated Activities.
Figure A & B.
Social Robot ‘PEPPER’ Engaging Older Adults in Meaningful Seated Activities.
2.1. Acceptance of Social Robots by Older Adults
Assistive technology use among older adults is commonplace as it can bring some normalcy back into their lives following an injury or negative health diagnosis [
23]. While the benefits of using assistive technologies are clear, their regular use by older adults can be challenging [
24]. Resistance, hesitancy, and non-compliance with the use of interventions like assistive technology are commonplace among older adults [
25]. Depending on the type of assistive technology this resistance by an older adult can be due to many factors. This includes a perceived loss of autonomy, fear of change, history or experience, loss of motivation or drive, decline in cognition, religious or belief reasons, and/or any other subjective perception that an older adult may have to not want to engage or use the assistive technology [
26,
27]. As social robots are a newer form of assistive technology, their benefits to older adults are still being explored. Subsequently, barriers to their acceptance and use by older adults have been documented and are expected in future research.
3. Publication Aims
The use of social robots among older adults is an emerging field of study in an Australian context. As with many other interventions and assistive technology, hesitancy, or resistance to their use by older adults are expected. Subsequently, the exploratory research being conducted in Australia on social robots and older adults is primarily concerned with understanding what will drive their acceptance and use.
The main aim of this paper is to provide a combined conceptual framework, using the well-established Activity Theory of Aging (ATA) and the Unified Theory of Acceptance and Use of Technology (UTAUT) that may provide insight into the factors influencing older adults’ acceptance of using social robots for meaningful seated activities.
4. Theoretical Frameworks
4.1. The Activity Theory of Aging (ATA)
Concerns over the quality of life for older adults and what constitutes healthy aging were first documented within the “Activity Theory of Aging (ATA)”. This theory proposes that well-being and longevity for older adults depend on the quality of their social interactions and maintaining an active lifestyle [
2]. This is particularly important in an individual’s later years [
28]. In contrast, a deterioration of social relationships and a decline in activity have demonstrated a decrease in the quality and quantity of life for an older adult [
2].
The older population is set to increase exponentially and move into assisted living facilities. This has raised concerns for clinicians over how to maintain a healthy aging protocol through activity and social connections in aged care facilities. Highlighted by Peri et al. [
1], mobility into a care facility can reduce the autonomy of an older adult, further declining their social interactions and daily activities [
4]. In line with the Activity Theory of Aging (ATA), which is foundational to this research, this article proposes the use of social robots by older adults for engagement in meaningful seated activities and social interactions.
4.2. The Unified Theory of Acceptance & Use of Technology (UTAUT)
Research on social robots and older adults is in its early stages of study in Australia. Whilst they hold promise to improve the quality of life for older adults, gaining their acceptance and use by this demographic poses an obstacle [
29]. Generally, older adults have lower adoption rates of newer technologies, have a difficult time navigating the technology and are more likely to disengage [
30]. This is consistent with other forms of assistive technologies and older adults, where compliance obstacles remain prominent throughout clinical aged care [
25].
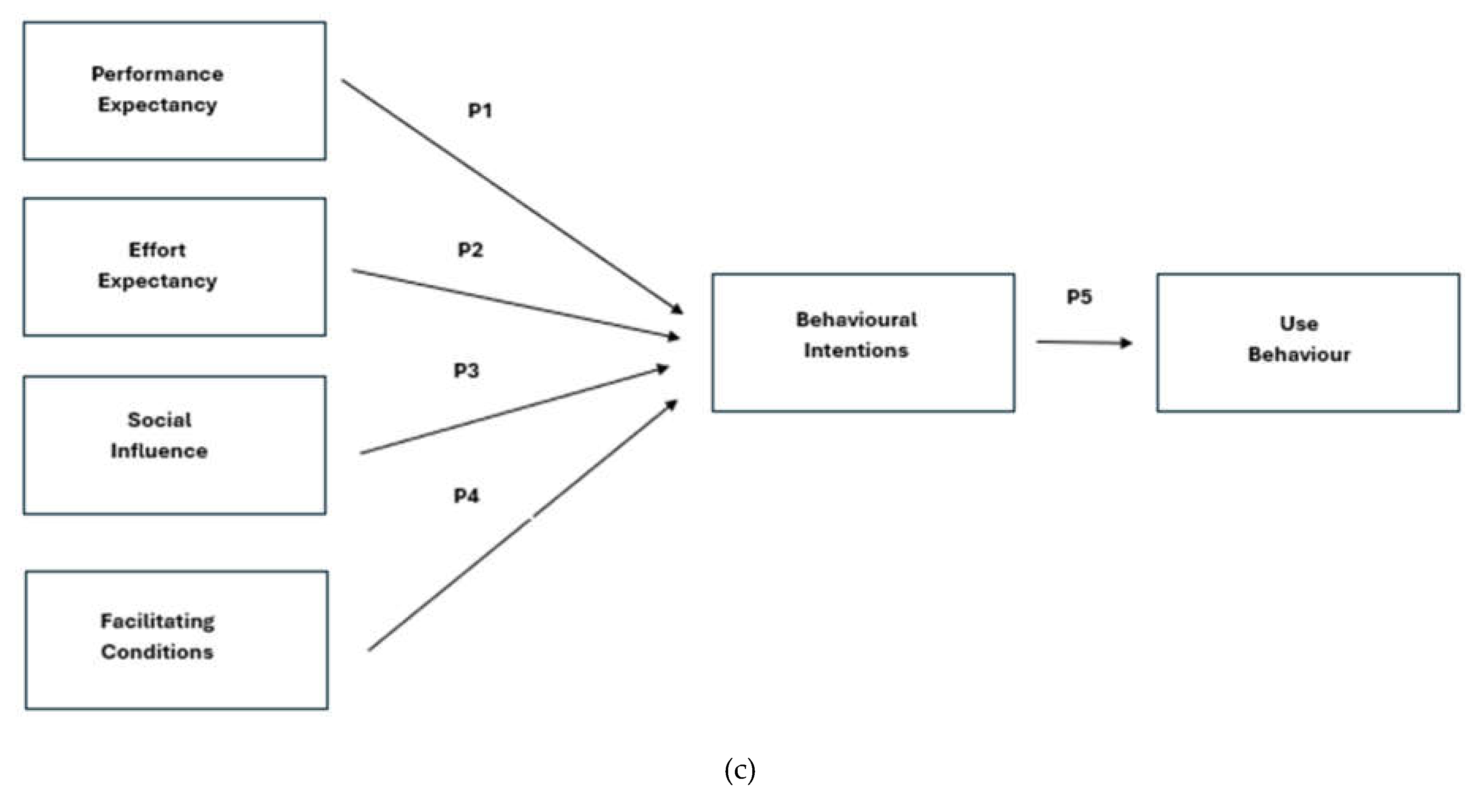
The Unified Theory of Acceptance and Use of Technology (UTAUT) is the conceptual framework at the basis of this research. Namely, what driving factors will contribute to an older adult’s acceptance and use of assistive technologies like social robots? Other studies that have used the UTAUT model to assess the acceptance and use of assistive technologies by older adults indicate similarly. Consistent with Hsu et al. [
31], older adults are usually the last in a population to adopt newer technologies, even if it can bring a tangible benefit to their quality and quantity of life. This was explored in research by Bixter et al. [
30], who investigated what would drive older adults to be more likely to adopt social media technologies using the UTAUT model. Subsequently, the UTAUT model provides a robust framework for understanding the motivating factors that will drive older adults to accept and use newer forms of assistive technologies like social robots. The UTAUT model used in this context has been modified to include four primary concepts that researchers believe are imperative in driving behavioural intentions: Performance Expectancy, Effort Expectancy, Social Influence and Facilitating Conditions [
32].
Figure C.
Model Adopted from the Unified Theory of Acceptance & Use of Technology.
Figure C.
Model Adopted from the Unified Theory of Acceptance & Use of Technology.
5. Theoretical Propositions
5.1. UTAUT Performance Expectancy
Performance Expectancy relates to whether an individual believes that a system or technology will help or benefit them [
32]. This concept is broad, can be expressed in multiple ways and applies to a range of circumstances regarding technology acceptance and use by an individual [
32]. The concept of Performance Expectancy is also foundational in other models such as the Technology Acceptance Model (TAM). Conversely, in the TAM model, it is referred to as “Perceived Usefulness” [
33]. As defined in TAM, this concept relates to the degree an individual believes using the technology or system will help them [
33]. Simply, if an individual believes that the technology is useful for him or her, then the likelihood of using the technology is high [
34].
Older adults are sometimes unaware of how a specific technology can benefit them or what types of technologies are available for them to use [
35]. This is explained by the Life Course Theory. The Life Course Theory, as proposed by Glen Elder provides insight into older adults’ technology perceptions and their usage over some time considering previous event histories that may influence later outcomes in individuals’ lives [
36]. Older adults did not grow up with these types of technologies that may be prevalent in their lives today [
37]. Therefore, their interaction with these technologies then was non-existent. Thus, their expectations from the technology may also be limited.
On the other hand, if older adults are exposed to technology such as social robots and are provided with an opportunity to familiarize themselves with the use of this technology, for example undertaking seated activities or socially interacting, then researchers propose that this would increase older adults’ intentions to use this technology. Subsequently, this will also drive their self-efficacy in the technology and would be more likely to continue its use and recommend it to their peers [
38].
Proposition 1. Older adults’ expectations regarding a social robot’s usefulness will affect their intentions to use the humanoid.
5.2. UTAUT Effort Expectancy
Effort expectancy or ‘perceived ease of use’ relates to whether an individual perceives the technology as easy to adopt or use, for themselves and/or others [
32]. Among Australia’s older adults, effort expectancy ordinarily raises many challenges due to older adults’ general averseness to technology [
30]. For example, whereas older adults may be able to comprehend the benefits of assistive technology, they may perceive the product, service, or device as being difficult to use and not want to try it [
39].
As people age, they begin to experience problems with their overall health, including cognitive functions [
40]. The cognitive load theory first proposed by John Sweller helps to explain the reason. This theory is based on the amount of information a human can hold and analyse [
41]. Highlighted by Van Gerven et al. [
42] there are three types of cognitive declines that seniors experience: a) a decrease in working memory capacity, which means short-term memory loss; b) a decline in the rate at which information is processed and understood, which means it takes longer for older adults to comprehend information; c) a decline in the ability to ignore irrelevant information, which means older adults may get distracted with information which is not relevant to a task.
In the context of this research, ‘effort expectancy’ refers to older adults’ perceptions regarding the amount of effort required to use a social robot. The greater the amount of effort needed, the less likely they are to want to engage with it. On the other hand, if older adults are exposed to technology such as social robots and are provided with assistance and time to use and build experience with this technology, then researchers expect that this would assist older adults in using the robot, and consequently increase their intentions to use a social robot. As older adults’ belief in their capability to use a robot increases, they would be more likely to continue its use and recommend it to their peers [
38]
Proposition 2. Older adults’ perceptions regarding the ease with which a social robot can be used will be linked to their intentions to use the humanoid social robot (for meaningful seated activities).
5.3. UTAUT Social Influence
Social influence, also referred to as ‘social norm’ is defined as the degree to which an individual perceives that ‘important others’ believe he or she should use the new technology [
32]. ‘Important others’ can include an individual’s peers, partners, colleagues, and media consumed [
43], and even superiors in mandatory setting [
32].
The Disengagement Theory [
3] (p. 227) states that "aging is an inevitable, mutual withdrawal or disengagement, resulting in decreased interaction between the aging person and others in the social system he belongs to". The theory claims that it is natural and acceptable for older adults to withdraw from society [
44]. However, it should be noted that the older adult cohort could still be influenced by people beyond family and close friends. In an aged care setting, older adults usually interact with carers, healthcare professionals, volunteers, and other residents of the care facility [
45]. Previous research by Ashida et al. [
46] has shown that when individuals receive encouragement from other members of their network, it is associated with higher motivation to engage in health screenings. Furthermore, Ashida et al. [
47] demonstrated that older adults are more likely to consume and stick with a healthy diet if their peers do [
48]. A systematic review by Burton et al. [
49], found that the most frequently identified motivators for older people to participate in training activities were social support and engagement with older peers. Peer-led exercise programs also were reported to be as effective as those led by a professional instructor [
50].
In an aged care context, group activities and group settings are commonplace [
10]. Older adults’ peers often share similar characteristics – for example, age, life experience and similarities in history. Peers also have an enhanced capacity to share, relate and empathise with their group in a way that non-peers are often not able to [
51]. According to Simoni et al. [
52], an aged care facility needs to have a well-managed peer program, in which peers are valued and clinicians are trained to deliver specific interventions to residents together. In our context, meaningful seated activities like bingo, listening to music or drawing, then it is quite possible that older adults develop more positive attitudes towards using a social robot.
Meanwhile, previous research by Wu et al. [
27], has highlighted the presence of fear amongst older adults of losing human contact because of the introduction of social robots in a care setting. This highlights the need to ensure that any intervention involving a social robot must be effectively planned and managed, and adequately addresses any concerns of older adults.
Proposition 3. Older adults are more likely to use a social robot if they are adequately introduced to and encouraged by important members of their social network in an aged care facility to use the technology.
5.4. UTAUT Facilitating Conditions
Facilitating conditions relate to whether an individual believes that the infrastructure within an organisation exists to use a system or technology [
32]. Facilitating conditions such as the availability of help, support, training, and the like help older adults in adopting a new technology.
Older adults in an aged care environment expect support while using new technology. Older adults have reportedly been concerned about operating devices and the implications around the malfunction of technology [
27]. At home, informal sources of support may come from the immediate family, friends, and neighbours [
53]. However, in a formal, aged care setting it would be expected that professional support is available in learning, continued use, maintenance, and repair of any technology-related devices [
54].
It is well-recognised that resource constraints - at times - limit the deployment and effective use of technology in aged care. Organisations may face financial constraints in procuring and maintaining technology. Tight budgets may also limit the number of staff who are available to run technology-based activity programs. Moreover, there could be constraints on staff time which may result in a preference for group activities over single-user technology-based activities (such as interacting with a social robot). Finally, staff may also need time to not only facilitate activities but also learn how to use the technology [
55].
Proposition 4. When older adults feel assured that there is adequate technical help and support available, they will be more likely to use a social robot for meaningful seated activities.
5.5. Behavioural Intentions to Use Social Robots
The stronger an individual’s intention to engage in a behaviour, the more likely that the behaviour will be performed [
56]. Therefore, if an older adult is strongly motivated to use a social robot for a particular task, chances are that he or she will do so.
On the other hand, the intention-behaviour gap is a reality [
56]. Despite older adults’ intentions to use a robot, the behaviour may not be performed. As has been argued there could be a range of external factors – such as a power failure - which may inhibit an individual’s adoption of a new technology [
56], even though the intention was there. However, given researchers’ agreement that intention is a significant antecedent of behaviour, it is proposed that:
Final Proposition. Older adults’ use of a social robot will be driven by their intention to use this technology.
6.0. Conclusion
Research on social robots and older adults in Australia is still emerging. The primary objective of this study is to explore whether older adults will be ready to engage in meaningful seated activities initiated by a social robot within a care setting. To effectively explore and understand this phenomenon, it is the contention of the researchers to apply the UTAUT model to these concepts. This study will contribute to the emerging literature by exploring if the expected propositions for each concept of the UTAUT model are satisfied when applied to older adults and social robot-initiated, meaningful seated activities in an Australian care setting.
Author Contributions
Conceptualization, J.S. and A.K.; validation, J.S. and A.K.; writing—original draft preparation, J.S.; writing—review and editing, A.K.; visualization, A.K.; supervision, A.K., O.M., M.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Human Research Ethics Committee of Western Sydney University reference number: H15666 on 14th December 2023 for studies involving humans.
Informed Consent Statement
Not applicable for studies not involving humans.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Peri, K, Broad, JB, Hikaka, J, Boyd, M, Bloomfield, K, Wu, Z, et al. 2020, ‘Study protocol: Older people in retirement villages. A survey and randomised trial of a multi-disciplinary invention designed to avoid adverse outcomes’, BMC Geriatrics, vol. 20, no. 1, pp. 1–9.
- Havighurst, R 1961, “Successful Aging,” The Gerontologist, vol. 1, no. 1, pp. 8–13.
- Cumming, E & Henry, WE 1961, Growing old 1st edn, Basic Books, New York, NY.
- Giles, LC, Crotty, M & Cameron, ID 2003, “Disability in older Australians: Projections for 2006–2031,” Medical Journal of Australia, vol. 179, no. 3, pp. 130–133.
- Mansbach, WE & Mace, RA 2018, ‘Predicting functional dependence in mild cognitive impairment: Differential contributions of memory and executive functions’, The Gerontologist.
- Yang, Z, Hotterbeex, P, Marent, P-J, Cerin, E, Thomis, M & van Uffelen, J 2024, ‘Physical activity, sedentary behaviour, and cognitive function among older adults: A bibliometric analysis from 2004 to 2024’, Ageing Research Reviews, p. 102283.
- Kurrle, SE, Cameron, ID & Quine, S 2004, ‘Predictors of adherence with the recommended use of hip protectors’, The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, vol. 59, no. 9.
- Tremblay, MS, Aubert, S, Barnes, JD, Saunders, TJ, Carson, V, Latimer-Cheung, AE, et al. 2017, ‘Sedentary behavior research network (SBRN) – terminology consensus project process and outcome’, International Journal of Behavioral Nutrition and Physical Activity, vol. 14, no. 1.
- Best, JR, Miller, PH & Jones, LL 2009, ‘Executive functions after age 5: Changes and correlates’, Developmental Review, vol. 29, no. 3, pp. 180–200.
- Edvardsson, D, Petersson, L, Sjogren, K, Lindkvist, M & Sandman, P-O 2013, ‘Everyday activities for people with dementia in residential aged care: Associations with person-centredness and quality of life’, International Journal of Older People Nursing, vol. 9, no. 4, pp. 269–276.
- Espinel, PT, Chau, JY, Van Der Ploeg, HP & Merom, D 2015, ‘Older adults’ time in sedentary, light and moderate intensity activities and correlates: Application of Australian time use survey’, Journal of Science and Medicine in Sport, vol. 18, no. 2, pp. 161–166.
- Shin, HR, Um, SR, Yoon, HJ, Choi, EY, Shin, WC, Lee, HY, et al. 2023, ‘Comprehensive Senior Technology Acceptance Model of daily living assistive technology for older adults with frailty: Cross-sectional study’, Journal of Medical Internet Research, vol. 25, pp. 1-11.
- Henschel, A., Laban, G., and Cross, E.S. 2021, ‘What Makes a Robot Social? A Review of Social Robots from Science Fiction to a Home or Hospital Near You,’ Current Robotics Reports, vol. 2, pp. 9-19.
- Hegel, F., Muhl, C., Wrede, B., Hielscher-Fastabend, M. and Sagerer, G. 2009, ‘Understanding social Robots’, In 2009 Second International Conferences on Advances in Computer Human Interactions, Feb 1-7, Cancun, Mexico, pp. 169-174.
- Pirhonen, J, Tiilikainen, E, Pekkarinen, S, Lemivaara, M & Melkas, H 2020, “Can robots tackle late-life loneliness? scanning of future opportunities and challenges in assisted living facilities,” Futures, vol. 124, pp. 1–12.
- Sun, R & Liu, Y 2006, “Mortality of the Oldest Old in China,” Journal of Aging & Health, vol. 18, no. 1, pp. 3–141.
- Khosla, R, Nguyen, K & Chu, M-T 2016, “Human Robot Engagement and Acceptability in Residential Aged Care,” International Journal of Human–Computer Interaction, vol. 33, no. 6, pp. 510–522.
- Ge, G & Schleimer, SC 2022, “Robotic Technologies and Well-being for Older Adults Living at Home,” Academy of Management Proceedings, vol. 37, no. 3, pp. 340–350.
- Feil-Seifer, D & Mataric, MJ 2005, ‘Socially assistive robotics’, 9th International Conference on Rehabilitation Robotics, 2005. ICORR 2005., pp. 465–468.
- Kyong, K, Freedman, S, Mataric, M, Lopez, B & Cunningham, M 2005, ‘A hands-off physical therapy assistance robot for cardiac patients’, 9th International Conference on Rehabilitation Robotics, ICORR 2005., 28 June-1 July 2005 2005. 337-340.
- Macis, D, Perilli, S & Gena, C 2022, ‘Employing socially assistive robots in elderly care’, Adjunct Proceedings of the 30th ACM Conference on User Modeling, Adaptation and Personalization.
- Smarr, C-A, Prakash, A, Beer, JM, Mitzner, TL, Kemp, CC & Rogers, WA 2012, ‘Older adults’ preferences for and acceptance of robot assistance for everyday living tasks’, Proceedings of the Human Factors and Ergonomics Society Annual Meeting, vol. 56, no. 1, pp. 153–157.
- Scherer, MJ 1996, ‘Outcomes of assistive technology use on quality of life’, Disability and Rehabilitation, vol. 18, no. 9, pp. 439–448.
- Mortenson, WB, Demers, L, Fuhrer, MJ, Jutai, JW, Lenker, J & DeRuyter, F 2013, ‘Effects of an assistive technology intervention on older adults with disabilities and their informal caregivers’, American Journal of Physical Medicine & Rehabilitation, vol. 92, no. 4, pp. 297–306.
- Kurrle, S, Bateman, C, Cumming, A, Pang, G, Patterson, S & Temple, A 2019, “Implementation of a model of care for hospitalised older persons with cognitive impairment (the confused hospitalised older persons program) in six New South Wales Hospitals,” Australasian Journal on Ageing, vol. 38, no. S2, pp. 98–106.
- Lancioni, GE & Singh, NN 2014, Assistive technologies for people with diverse abilities 1st edn, Springer, New York, NY.
- Wu, Y-H, Wrobel, J, Cornuet, M, Kerhervé, H, Damnée, S & Rigaud, A-S 2014, ‘Acceptance of an assistive robot in older adults: A mixed-method study of human–robot interaction over a 1-month period in the Living Lab Setting’, Clinical Interventions in Aging, vol. 9, pp. 801–811.
- Blazer, DG, Beane, S, Boyd, C, Bolton, L, Demiris, G, Donovan, NJ, et al. 2020, Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System, National Academies Press, Washington, District of Columbia.
- Kang, HS, Koh, IS, Makimoto, K & Yamakawa, M 2023, ‘Nurses’ perception towards care robots and their work experience with socially assistive technology during COVID-19: A qualitative study’, Geriatric Nursing, vol. 50, pp. 234–239.
- Bixter, MT, Blocker, KA, Mitzner, TL, Prakash, A & Rogers, WA 2019, ‘Understanding the use and non-use of social communication technologies by older adults: A qualitative test and extension of the ATAUT model’, Gerontechnology, vol. 18, no. 2, pp. 70–88.
- Hsu, C-C, Sandford, B, Ling, C-J & Lin, C-T 2021, ‘Can the unified theory of acceptance and use of technology (utaut) help explain subjective well-being in senior citizens due to gateball participation?’, International Journal of Environmental Research and Public Health, vol. 18, no. 17, p. 9015.
- Venkatesh, V, Morris, M, Davis, GB & Davis, FB 2003, ‘User acceptance of information technology: Toward a unified view’, MIS Quarterly, vol. 27, no. 3, pp. 425–478.
- He, Y, Chen, Q & Kitkuakul, S 2018, ‘Regulatory focus and technology acceptance: Perceived ease of use and usefulness as efficacy’, Cogent Business & Management, vol. 5, no. 1, p. 1459006.
- Xue, L, Rashid, AM & Ouyang, S 2024, ‘The unified theory of acceptance and use of Technology (UTAUT) in Higher Education: A systematic review’, Sage Publications, vol. 14, no. 1.
- Zajicek, M 2006, ‘Aspects of HCI research for older people’, Universal Access in the Information Society, vol. 5, no. 3, pp. 279–286.
- Elder, GH 1998, ‘The life course as developmental theory’, Child Development, vol. 69, no. 1, pp. 1–12.
- Levesque, RJR 2011, Encyclopedia of Adolescence 1st edn, Springer, New York, NY.
- Lu, l., Cai, R. & Gursoy, D. 2019, ‘Developing and validating a service robot integration willingness scale’, International journal of hospitality management, vol. 80, pp. 36-51.
- Hebesberger, D, Koertner, T, Gisinger, C & Pripfl, J 2017, ‘A long-term autonomous robot at a care hospital: A mixed methods study on social acceptance and experiences of staff and older adults’, International Journal of Social Robotics, vol. 9, no. 3, pp. 417–429.
- Smith, TJ 2008, ‘Senior citizens and e-commerce websites: The role of perceived usefulness, perceived ease of use, and web site usability’, Informing Science: The International Journal of an Emerging Transdiscipline, vol. 11, pp. 59–83.
- Sweller, J 1988, ‘Cognitive load during problem solving: Effects on learning’, Cognitive Science, vol. 12, no. 2, pp. 257–285.
- Van Gerven, P, Schmidt, H, Hendriks, M, Merrienboer, J & Paas, F 2010, ‘The efficiency of multimedia learning into old age’, British Journal of Educational Psychology, vol. 73, no. 4, pp. 489–505.
- Abbad, MM 2021, ‘Using the UTAUT model to understand students’ usage of e-learning systems in developing countries’, Education and Information Technologies, vol. 26, no. 6, pp. 7205–7224.
- Ebersole, P, Hess, P & Luggen, A 1994, Toward Healthy Aging: Human Needs and Nursing Response 1st edn, Mosby, St Louis, MI.
- Boamah, SA, Weldrick, R, Lee, T-SJ & Taylor, N 2021, ‘Social Isolation Among Older Adults in Long-Term Care: A Scoping Review’, Journal of Aging and Health, vol. 33, pp. 618–632.
- Ashida, S, Hadley, DW, Goergen, AF, Skapinsky, KF, Devlin, HC & Koehly, LM 2011, ‘The importance of older family members in providing social resources and promoting cancer screening in families with a hereditary cancer syndrome’, The Gerontologist, vol. 51, no. 6, pp. 833–842.
- Ashida, S, Wilkinson, AV & Koehly, LM 2012, ‘Social influence and motivation to change health behaviors among Mexican-origin adults: Implications for diet and physical activity’, American Journal of Health Promotion, vol. 26, no. 3, pp. 176–179.
- Thrasher, JF, Campbell, MK & Oates, V 2004, ‘Behavior-specific social support for healthy behaviors among African American church members: Applying optimal matching theory’, Health Education & Behavior, vol. 31, no. 2, pp. 193–205.
- Burton, E, Farrier, K, Lewin, G, Pettigrew, S, Hill, A-M, Airey, P, et al. 2017, ‘Motivators and barriers for older people participating in resistance training: A systematic review’, Journal of Aging and Physical Activity, vol. 25, no. 2, pp. 311–324.
- Layne, JE, Sampson, SE, Mallio, CJ, Hibberd, PL, Griffith, JL, Das, SK, et al. 2008, ‘Successful dissemination of a community-based Strength Training Program for older adults by peer and professional leaders: The people exercising program’, Journal of the American Geriatrics Society, vol. 56, no. 12, pp. 2323–2329.
- Doull, M, O’Connor, AM, Welch, V, Tugwell, P & Wells, GA 2005, ‘Peer support strategies for improving the health and well-being of individuals with chronic diseases’, Cochrane Database of Systematic Reviews, vol. 3.
- Simoni, JM, Franks, JC, Lehavot, K & Yard, SS 2011, ‘Peer interventions to promote health: Conceptual considerations.’, American Journal of Orthopsychiatry, vol. 81, no. 3, pp. 351–359.
- Barnard, Y, Bradley, MD, Hodgson, F & Lloyd, AD 2013, ‘Learning to use new technologies by older adults: Perceived difficulties, experimentation behaviour and usability’, Computers in Human Behavior, vol. 29, no. 4, pp. 1715–1724.
- Lee, C 2013, ‘Adoption of smart technology among older adults: Challenges and issues’, Public Policy & Aging Report, vol. 24, no. 1, pp. 14–17.
- Waycott, J, Zhao, W, Kelly, RM & Robertson, E 2022, ‘Technology-mediated enrichment in aged care: Survey and interview study’, JMIR Aging, vol. 5, no. 2.
- Davis, F.D. 1989, ‘Perceived usefulness, perceived ease of use, and user acceptance of information technology’, MIS quarterly, vol. 12, no. 3, pp. 319-340.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).