Submitted:
25 May 2024
Posted:
27 May 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Methods
Data Sources and Study Period
Exploratory Data Analysis
Statistical Analysis
Results
Discussion
Conclusion
Funding
Informed Consent Statement
Data availability Statement
Conflicts of Interest
References
- Ho RJY. Warp-Speed Covid-19 Vaccine Development: Beneficiaries of Maturation in Biopharmaceutical Technologies and Public-Private Partnerships. J Pharm Sci. 2021;110(2):615-618. [CrossRef]
- Diaz GA, Parsons GT, Gering SK, et al. Myocarditis and Pericarditis After Vaccination for COVID-19. JAMA. 2021;326(12):1210-1212. [CrossRef]
- Mevorach D, Anis E, Cedar N, et al. Myocarditis after BNT162b2 mRNA Vaccine against Covid-19 in Israel. N Engl J Med. 2021;385(23):2140-2149. [CrossRef]
- Rose J, Hulscher N, McCullough PA. Determinants of COVID-19 vaccine-induced myocarditis. Ther Adv Drug Saf. 2024;15:20420986241226566. Published 2024 Jan 27. [CrossRef]
- Ho JSY, Sia CH, Ngiam JN, et al. A review of COVID-19 vaccination and the reported cardiac manifestations. Singapore Med J. 2023;64(9):543-549. [CrossRef]
- Zafar U, Zafar H, Ahmed MS, Khattak M. Link between COVID-19 vaccines and myocardial infarction. World J Clin Cases. 2022;10(28):10109-10119. [CrossRef]
- Aye YN, Mai AS, Zhang A, et al. Acute myocardial infarction and myocarditis following COVID-19 vaccination. QJM. 2023;116(4):279-283. [CrossRef]
- Bekal S, Husari G, Okura M, Huang CA, Bukari MS. Thrombosis Development After mRNA COVID-19 Vaccine Administration: A Case Series. Cureus. 2023;15(7):e41371. Published 2023 Jul 4. [CrossRef]
- Mani A, Ojha V. Thromboembolism after COVID-19 Vaccination: A Systematic Review of Such Events in 286 Patients. Ann Vasc Surg. 2022;84:12-20.e1. [CrossRef]
- Bernardi, Francesca Futura et al. “Thromboembolic Events after COVID-19 Vaccination: An Italian Retrospective Real-World Safety Study.” Vaccines vol. 11,10 1575. 10 Oct. 2023. [CrossRef]
- Yeo YH, Wang M, He X, et al. Excess risk for acute myocardial infarction mortality during the COVID-19 pandemic. J Med Virol. 2023;95(1):e28187. [CrossRef]
- Martin SS, Aday AW, Almarzooq ZI, et al. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association [published correction appears in Circulation. 2024 May 7;149(19):e1164]. Circulation. 2024;149(8):e347-e913. [CrossRef]
- King County. "Emergency Medical Services: Reports and Publications." King County, https://kingcounty.gov/en/dept/dph/health-safety/health-centers-programs-services/emergency-medical-services/reports-publications. Accessed 23 May 2024.
- U.S. Census Bureau. "Programs and Surveys: Population Estimates Tables." U.S. Census Bureau, U.S. Department of Commerce, https://www2.census.gov/programs-surveys/popest/tables/. Accessed 23 May 2024.
- King County, WA COVID-19 Vaccine Tracker. The Tennessean. https://data.tennessean.com/covid-19-vaccine-tracker/washington/king-county/53033/ (accessed 13 May 2024).
- Real Statistics Using Excel. "Proportion Parameter Confidence Interval." Real Statistics Using Excel, https://www.real-statistics.com/binomial-and-related-distributions/proportion-distribution/proportion-parameter-confidence-interval/. Accessed 23 May 2024.
- Coronavirus (COVID-19) Update: June 25, 2021 [Internet]. U.S. Food and Drug Administration. 2021. Available from: https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-june-25-2021. (accessed 15 May 2024).
- Janssen COVID-19 Vaccine EUA Fact Sheet for Healthcare Providers [Internet]. U.S. Food and Drug Administration; 2023. Available from: https://www.fda.gov/media/146304/download. (accessed 15 May 2024).
- Hulscher N, Alexander PE, Amerling R, et al. A SYSTEMATIC REVIEW OF AUTOPSY FINDINGS IN DEATHS AFTER COVID-19 VACCINATION. Zenodo. 2023. [CrossRef]
- Hulscher N, Hodkinson R, Makis W, McCullough PA. Autopsy findings in cases of fatal COVID-19 vaccine-induced myocarditis. ESC Heart Fail. Published online January 14, 2024. [CrossRef]
- Janus SE, Makhlouf M, Chahine N, Motairek I, Al-Kindi SG. Examining Disparities and Excess Cardiovascular Mortality Before and During the COVID-19 Pandemic. Mayo Clin Proc. 2022;97(12):2206-2214. [CrossRef]
- Sun, Christopher L F et al. “Increased emergency cardiovascular events among under-40 population in Israel during vaccine rollout and third COVID-19 wave.” Scientific reports vol. 12,1 6978. 28 Apr. 2022. [CrossRef]
- Woodruff RC, Tong X, Khan SS, et al. Trends in Cardiovascular Disease Mortality Rates and Excess Deaths, 2010-2022. Am J Prev Med. 2024;66(4):582-589. [CrossRef]
- Faksova K, Walsh D, Jiang Y, et al. COVID-19 vaccines and adverse events of special interest: A multinational Global Vaccine Data Network (GVDN) cohort study of 99 million vaccinated individuals. Vaccine. 2024;42(9):2200-2211. [CrossRef]
- Parry PI, Lefringhausen A, Turni C, et al. 'Spikeopathy': COVID-19 Spike Protein Is Pathogenic, from Both Virus and Vaccine mRNA. Biomedicines. 2023;11(8):2287. Published 2023 Aug 17. [CrossRef]
- Hulscher N, Procter BC, Wynn C, McCullough PA. Clinical Approach to Post-acute Sequelae After COVID-19 Infection and Vaccination. Cureus. 2023;15(11):e49204. Published 2023 Nov 21. [CrossRef]
- Baumeier, Christian et al. “Intramyocardial Inflammation after COVID-19 Vaccination: An Endomyocardial Biopsy-Proven Case Series.” International journal of molecular sciences vol. 23,13 6940. 22 Jun. 2022. [CrossRef]
- Schreckenberg R, Woitasky N, Itani N, Czech L, Ferdinandy P, Schulz R. Cardiac side effects of RNA-based SARS-CoV-2 vaccines: Hidden cardiotoxic effects of mRNA-1273 and BNT162b2 on ventricular myocyte function and structure. Br J Pharmacol. 2024;181(3):345-361. [CrossRef]
- Krauson AJ, Casimero FVC, Siddiquee Z, Stone JR. Duration of SARS-CoV-2 mRNA vaccine persistence and factors associated with cardiac involvement in recently vaccinated patients. NPJ Vaccines. 2023;8(1):141. Published 2023 Sep 27. [CrossRef]
- De Michele M, d'Amati G, Leopizzi M, et al. Evidence of SARS-CoV-2 spike protein on retrieved thrombi from COVID-19 patients. J Hematol Oncol. 2022;15(1):108. Published 2022 Aug 16. [CrossRef]
- Bharmal, Murtaza et al. “Impact of Coronavirus Disease 2019 Pandemic on Cardiac Arrest and Emergency Care.” Heart failure clinics vol. 19,2 (2023): 231-240. [CrossRef]
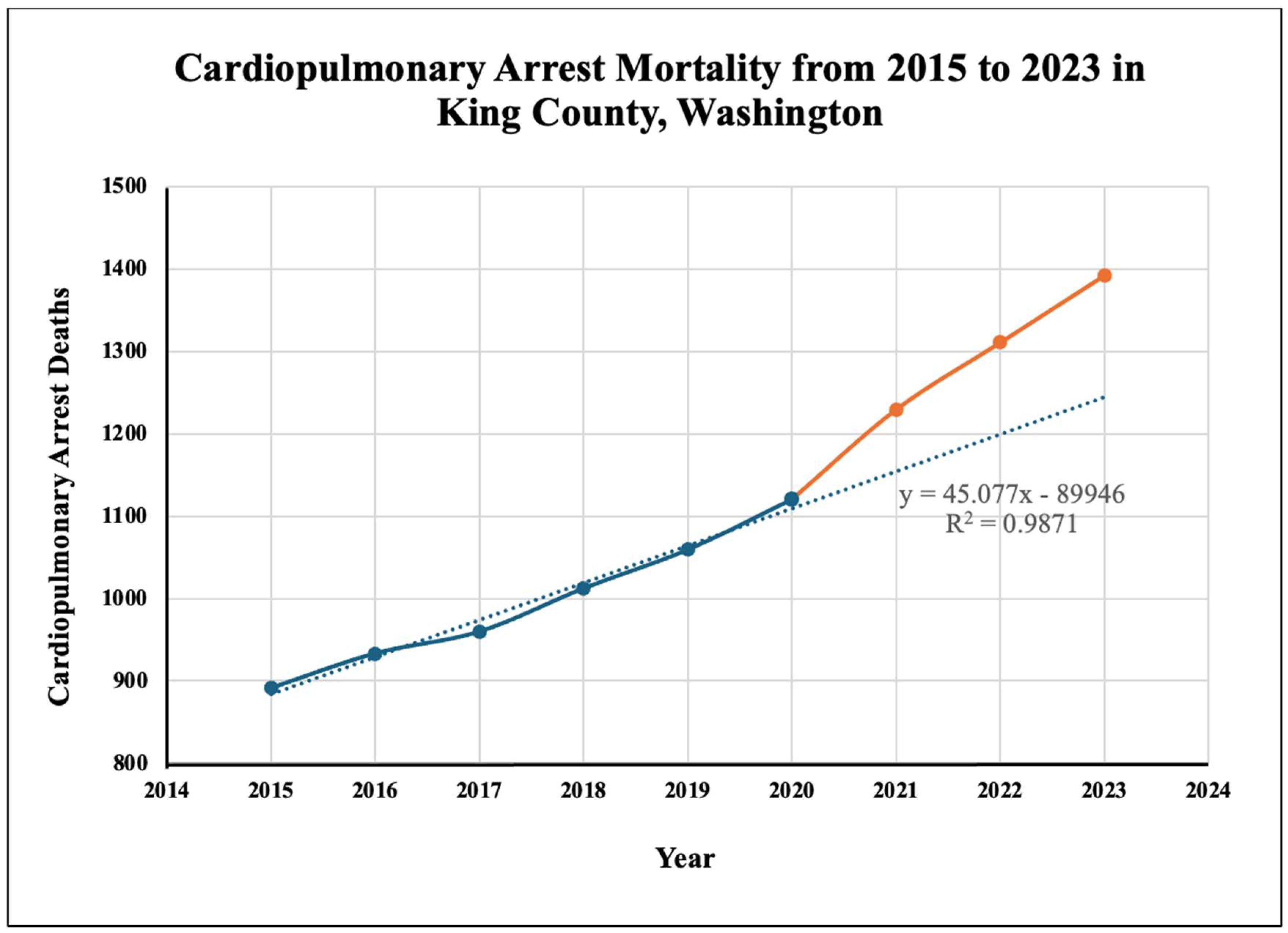
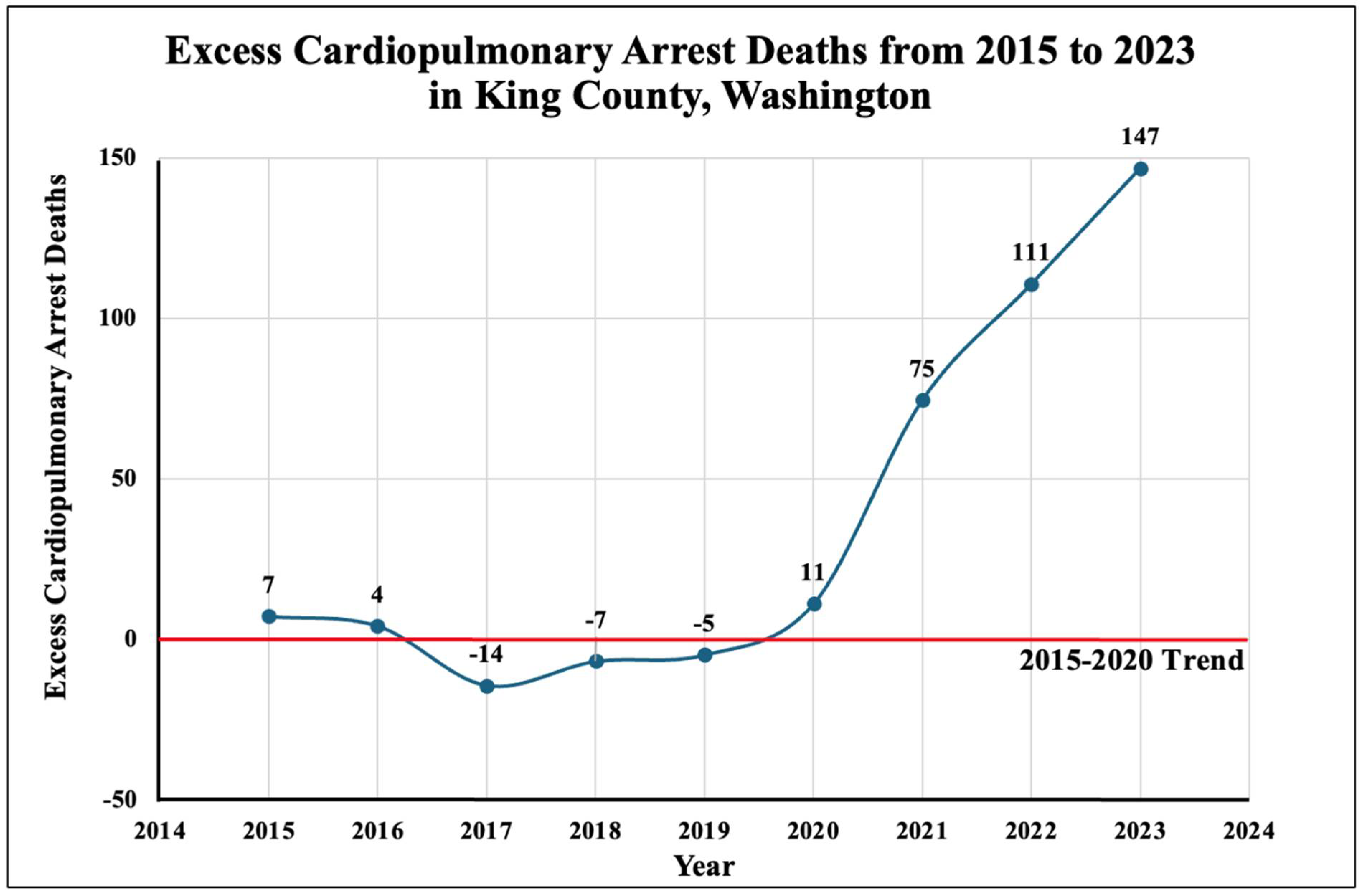

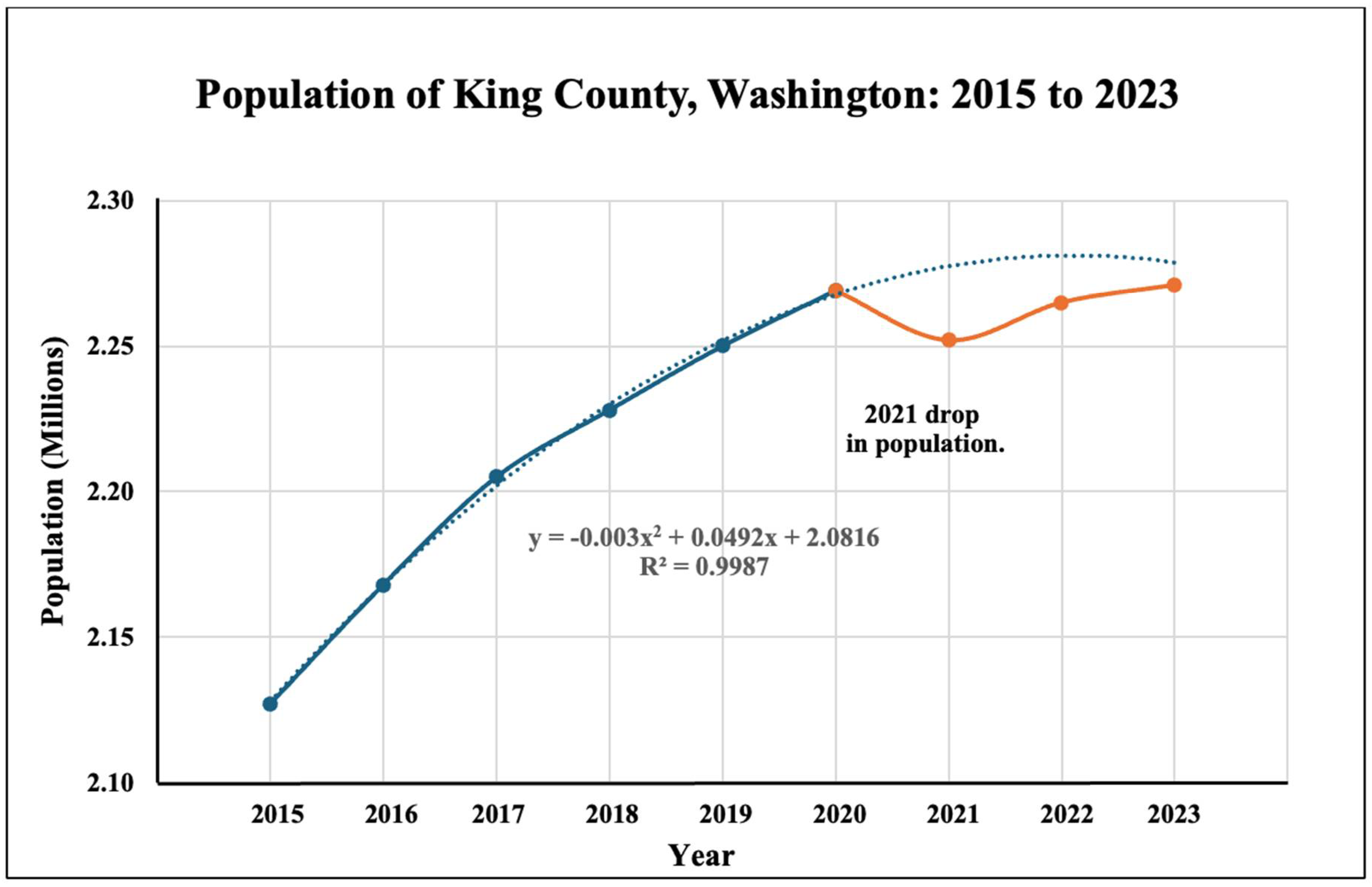
| Year | Cardiopulmonary arrests | Survival rate | Mortality* | Trend line | Excess deaths** | Population (mil) | Excess deaths of population (%)*** | COVID-19 Vaccination rate |
|---|---|---|---|---|---|---|---|---|
| 2015 | 1114 | 20% | 891 | 884 | 7 | 2.127 | 0.0003% | - |
| 2016 | 1228 | 24% | 933 | 929 | 4 | 2.168 | 0.0002% | - |
| 2017 | 1215 | 21% | 960 | 974 | -14 | 2.205 | -0.0007% | - |
| 2018 | 1298 | 22% | 1012 | 1019 | -7 | 2.228 | -0.0003% | - |
| 2019 | 1308 | 19% | 1059 | 1064 | -5 | 2.250 | -0.0002% | - |
| 2020 | 1350 | 17% | 1121 | 1110 | 11 ( 95% CI: -12, 34) | 2.274 | 0.0005% | - |
| 2021 | 1499 | 18% | 1229 | 1155 | 75 (95% CI: 51, 98) | 2.252 | 0.0033% | 66.59% |
| 2022 | 1598 | 18% | 1310 | 1200 | 111 (95% CI: 87, 134) | 2.265 | 0.0049% | 85.19% |
| 2023 | 1697 | 18% | 1392 | 1245 | 147 (95% CI: 123, 170) | 2.271 | 0.0065% | 98.0% |
| Region | Year | Population (Mil) | Excess Deaths* |
|---|---|---|---|
| King County, WA | 2021 | 2.252 | 75 |
| 2022 | 2.265 | 111 | |
| 2023 | 2.271 | 147 | |
| USA | 2021 | 332.0 | 10,990 |
| 2022 | 333.3 | 16,280 | |
| 2023 | 340.0 | 21,970 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





