Submitted:
02 April 2024
Posted:
02 April 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
2.1. Study Design and Sample
2.2. Group Allocation and Procedures
2.3. Blinding
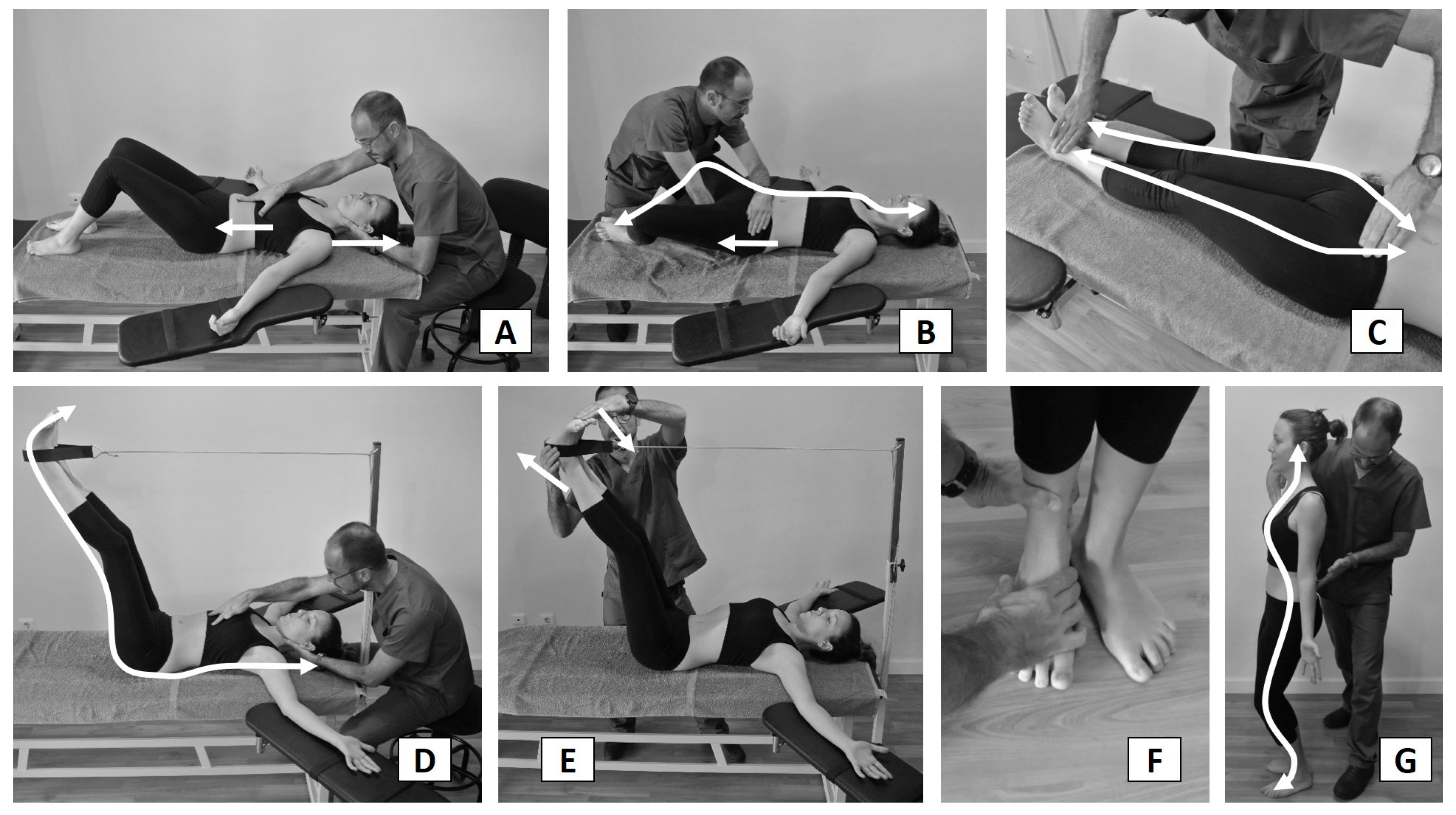
2.4. Intervention and Follow-Up
2.5. Outcomes Measures
2.5.1. Plantar Pressures
2.5.2. Lumbar RoM
2.6. Statistical Analyses
2.6.1. Sample Size Calculation
2.6.2. Data Analysis
3. Results
3.1. Flow of Subjects
3.2. Effect of the Intervention
4. Discussion and Conclusions
Supplementary Materials
References
- Watanabe, M., Kaneoka, K., Wada, Y., Matsui, Y., & Miyakawa, S. (2014). Trunk muscle activity with different sitting postures and pelvic inclination. Journal of Back and Musculoskeletal Rehabilitation, 27(4), 531-536. [CrossRef]
- Howarth, S.J., Glisic, D., Lee, J.G., & Beach, T.A. (2013). Does prolonged seated deskwork alter the lumbar flexion relaxation phenomenon? Journal of Electromyography and Kinesiology : Official Journal of the International Society of Electrophysiological Kinesiology, 23, 587–593. [CrossRef]
- Phimphasak, C., Swangnetr, M., Puntumetakul, R., Chatchawan, U., & Boucaut, R. (2016). Effects of seated lumbar extension postures on spinal height and lumbar range of motion during prolonged sitting. Ergonomics, 59(1), 112-120. [CrossRef]
- Shin, G., & Mirka, G.A. (2007). An in vivo assessment of the low back response to prolonged flexion: Interplay between active and passive tissues. Clinical Biomechanics (Bristol, Avon), 22(9), 965-971. [CrossRef]
- Bubric, K., & Hedge, A. (2016). Differential patterns of laptop use and associated musculoskeletal discomfort in male and female college students. Work (Reading, Mass.), 55(3), 663–671. [CrossRef]
- Serra-Ano, P., Lopez-Bueno, L., Garcia-Masso, X., Pellicer-Chenoll, M.T., & Gonzalez, L. M. (2015). Postural control mechanisms in healthy adults in sitting and standing positions. Perceptual and Motor Skills, 121(1), 119-134. [CrossRef]
- Ruhe, A., Fejer, R., & Walker, B. (2012). Pain relief is associated with decreasing postural sway in patients with non-specific low back pain. BMC Musculoskeletal Disorders, 13, 39-2474-13-39. [CrossRef]
- Gerasimenko, Y., Gad, P., Sayenko, D., McKinney, Z., Gorodnichev, R., Puhov, A., …, & Edgerton, V.R. (2016). Integration of sensory, spinal, and volitional descending inputs in regulation of human locomotion. J Neurophysiol, 116(1), 98-105. [CrossRef]
- Peterka, R.J. (2002). Sensorimotor integration in human postural control. Journal of Neurophysiology, 88(3), 1097-1118.
- Lopez-Rodriguez, S., Fernandez de-Las-Penas, C., Alburquerque-Sendin, F., Rodriguez-Blanco, C., & Palomeque-del-Cerro, L. (2007). Immediate effects of manipulation of the talocrural joint on stabilometry and baropodometry in patients with ankle sprain. Journal of Manipulative and Physiological Therapeutics, 30(3), 186-192. [CrossRef]
- Rosario, J.L. (2014). A review of the utilization of baropodometry in postural assessment. Journal of Bodywork and Movement Therapies, 18(2), 215-219. [CrossRef]
- Ferreira, G.E., Viero, C.C., Silveira, M.N., Robinson, C.C., & Silva, M.F. (2013). Immediate effects of hip mobilization on pain and baropodometric variables--a case report. Manual Therapy, 18(6), 628-631. [CrossRef]
- Mendez-Sanchez, R., Gonzalez-Iglesias, J., Sanchez-Sanchez, J.L., & Puente-Gonzalez, A.S. (2014). Immediate effects of bilateral sacroiliac joint manipulation on plantar pressure distribution in asymptomatic participants. Journal of Alternative and Complementary Medicine (New York, N.Y.), 20(4), 251-257. [CrossRef]
- Bordoni, B., & Myers, T. (2020). A Review of the Theoretical Fascial Models: Biotensegrity, Fascintegrity, and Myofascial Chains. Cureus, 12(2):e7092. [CrossRef]
- Krause, F., Wilke, J., Vogt, L., & Banzer, W. (2016). Intermuscular force transmission along myofascial chains: a systematic review. J Anat, 228(6):910-8. [CrossRef]
- Borman, N.P., Trudelle-Jackson, E., & Smith, S.S. (2011). Effect of stretch positions on hamstring muscle length, lumbar flexion range of motion, and lumbar curvature in healthy adults. Physiotherapy Theory and Practice, 27(2), 146-154. [CrossRef]
- Li, Y., McClure, P.W., & Pratt, N. (1996). The effect of hamstring muscle stretching on standing posture and on lumbar and hip motions during forward bending. Physical Therapy, 76(8), 836-45; discussion 845-9.
- Lopez-Minarro, P.A., Muyor, J.M., Belmonte, F., & Alacid, F. (2012). Acute effects of hamstring stretching on sagittal spinal curvatures and pelvic tilt. Journal of Human Kinetics, 31, 69-78. [CrossRef]
- Ferreira, G.E., Barreto, R.G., Robinson, C.C., Plentz, R.D., & Silva, M.F. (2016). Global postural reeducation for patients with musculoskeletal conditions: A systematic review of randomized controlled trials. Brazilian Journal of Physical Therapy, 20(3), 194-205. [CrossRef]
- Castagnoli, C., Cecchi, F., Del Canto, A., Paperini, A., Boni, R., Pasquini, G., Vannetti, F., & Macchi, C. (2015). Effects in Short and Long Term of Global Postural Reeducation (GPR) on Chronic Low Back Pain: A Controlled Study with One-Year Follow-Up. TheScientificWorldJournal, 2015, 271436. [CrossRef]
- Lawand, P., Lombardi Júnior, I., Jones, A., Sardim, C., Ribeiro, L. H., & Natour, J. (2015). Effect of a muscle stretching program using the global postural reeducation method for patients with chronic low back pain: A randomized controlled trial. Joint bone spine, 82(4), 272–277. [CrossRef]
- Lozano-Quijada, C., Poveda-Pagan, E.J., Segura-Heras, J.V., Hernandez-Sanchez, S., & Prieto-Castello, M.J. (2017). Changes in postural sway after a single global postural reeducation session in university students: A randomized controlled trial. Journal of Manipulative and Physiological Therapeutics, 40(7), 467-476. [CrossRef]
- Atya, A.M. (2013). The validity of spinal mobility for prediction of functional disability in male patients with low back pain. Journal of Advanced Research, 4(1), 43-49. [CrossRef]
- Cunha, A.C., Burke, T.N., Franca, F.J., & Marques, A.P. (2008). Effect of global posture reeducation and of static stretching on pain, range of motion, and quality of life in women with chronic neck pain: A randomized clinical trial. Clinics (Sao Paulo, Brazil), 63(6), 763-770. [CrossRef]
- Estepa-Gallego, A., Ibañez-Vera, A.J., Estudillo-Martínez, M.D., Castellote-Caballero, Y., Bergamin, M., Gobbo, S., …, & Cruz-Díaz, D. (2022). Effects of global postural reeducation on postural control, dynamic balance, and ankle range of motion in patients with hallux abducto valgus. A randomized controlled trial. J Orthop Res, 40(6):1436-1445. [CrossRef]
- Matos, F.P., Dantas, E.H.M., de Oliveira, F.B., de Castro, J.B.P., Conceição, M.C.S.C., Nunes, R.A.M, & Vale, R.G.S. (2020) Analysis of pain symptoms, flexibility and hydroxyproline concentration in individuals with low back pain submitted to Global Postural Re- education and stretching. Pain Manag, 10(3):167-177. [CrossRef]
- Gonzalez-Medina, G., Perez-Cabezas, V., Ruiz-Molinero, C., Chamorro-Moriana, G., Jimenez-Rejano, J.J., & Galán-Mercant, A. (2021). Effectiveness of Global Postural Re-Education in Chronic Non-Specific Low Back Pain: Systematic Review and Meta-Analysis. J Clin Med,10(22):5327. [CrossRef]
- Lomas-Vega, R., Garrido-Jaut, M.V., Rus, A., & Del-Pino-Casado, R. (2017). Effectiveness of Global Postural Re-education for Treatment of Spinal Disorders: A Meta-analysis. Am J Phys Med Rehabil, 96(2):124-130. [CrossRef]
- Moutzouri, M., Billis, E., Strimpakos, N., Kottika, P., & Oldham, J.A. (2008). The effects of the mulligan sustained natural apophyseal glide (SNAG) mobilisation in the lumbar flexion range of asymptomatic subjects as measured by the zebris CMS20 3-D motion analysis system. BMC Musculoskeletal Disorders, 9, 131-2474-9-131. [CrossRef]
- Stamos-Papastamos, N., Petty, N.J., & Williams, J.M. (2011). Changes in bending stiffness and lumbar spine range of movement following lumbar mobilization and manipulation. Journal of Manipulative and Physiological Therapeutics, 34(1), 46-53. [CrossRef]
- Shankar Ganesh, G., Mohanty, P., & Smita Pattnaik, S. (2015). The immediate and 24-hour follow-up effect of unilateral lumbar Z-joint mobilisation on posterior chain neurodynamics. Journal of Bodywork and Movement Therapies, 19(2), 226-231. [CrossRef]
- Lima, B.N., Lucareli, P.R., Gomes, W.A., Silva, J.J., Bley, A.S., Hartigan, E.H., & Marchetti, P.H. (2014). The acute effects of unilateral ankle plantar flexors static- stretching on postural sway and gastrocnemius muscle activity during single-leg balance tasks. Journal of Sports Science & Medicine, 13(3), 564-570.
- Romero-Franco, N., Martinez-Lopez, E.J., Lomas-Vega, R., Hita-Contreras, F., Osuna-Perez, M.C., & Martinez-Amat, A. (2013). Short-term effects of proprioceptive training with unstable platform on athletes' stabilometry. Journal of Strength and Conditioning Research / National Strength & Conditioning Association, 27(8), 2189-2197. [CrossRef]
- Keijsers, N.L., Stolwijk, N.M., & Pataky, T.C. (2010). Linear dependence of peak, mean, and pressure-time integral values in plantar pressure images. Gait & Posture, 31(1), 140-142. [CrossRef]
- Takahashi, H.A., & Quevedo, A.A.F. (2021). Quantitative study of PIMT technique aiming its validation as physical therapy procedure. Foot (Edinb), 47:101800. [CrossRef]
- Teodori, M.S., Guirro, E.C.O., & Santos, R.M. (2005). Plantar pressure distribution and center force location after postural global reeducation: A case relate. Physical Therapy in Movement, 18(1), 27-35.
- Grassi Dde, O., de Souza, M.Z., Ferrareto, S.B., Montebelo, M.I., & Guirro, E.C. (2011). Immediate and lasting improvements in weight distribution seen in baropodometry following a high-velocity, low-amplitude thrust manipulation of the sacroiliac joint. Manual Therapy, 16(5), 495-500. [CrossRef]
- Martínez-Jiménez, E.M., Becerro-de-Bengoa-Vallejo, R., Losa-Iglesias, M.E., Rodríguez-Sanz, D., Díaz-Velázquez, J. I., Casado-Hernández, I., …, & López-López, D. (2020). Acute effects of myofascial induction technique in plantar fascia complex in patients with myofascial pain syndrome on postural sway and plantar pressures: A quasi-experimental study. Physical Therapy in Sport: Official Journal of the Association of Chartered Physiotherapists in Sports Medicine, 43, 70-76. [CrossRef]
- Hawrylak, A., Chromik, K., Ratajczak, B., Barczyk-Pawelec, K., & Demczuk-Włodarczyk, E. (2017). Spinal range of motion and plantar pressure in sport climbers. Acta of Bioengineering and Biomechanics, 19(2), 169-173.

| Control (n=32) Mean (SD) |
Global Stretching (n=32) Mean (SD) |
p-value (Effect size) |
||||
| Age (year) | 22.66 (4.08) | 21.38 (3.10) | .162 (.083) | |||
| Weight (kg) | 70.14 (15.97) | 61.88 (10.89) | .019 (.183) | |||
| Height (m) | 170.81 (10.64) | 167.58 (9.32) | .201 (.027) | |||
| BMI (kg/m2) | 23.78 (3.24) | 21.94 (2.86) | .019 (.117) | |||
| Lumbar ROM | Flexion | 50.42 (7.12) | 48.34 (6.62) | .233 (.060) | ||
| Extension | 17.21 (8.16) | 19.83 (10.58) | .271 (.173) | |||
| Right Rotation | 10.81 (16.31) | 13.42 (14.11) | .497 (.175) | |||
| Left Rotation | 8.96 (13.41) | 12.42 (13.65) | .310 (.380) | |||
| Right Lateral Flexion | 27.65 (4.48) | 27.35 (5.02) | .807 (.015) | |||
| Left Lateral Flexion | 26.06 (5.01) | 25.54 (5.1) | .681 (.028) | |||
| Plantar Pressures | Right Pmax | 613.63 (114.21) | 654.72 (125.82) | .176 (.087) | ||
| Left Pmax | 607.31 (119.5) | 647.03 (126.71) | .202 (.085) | |||
| Right Pmean | 294.63 (58.36) | 308.09 (56.87) | .353 (.061) | |||
| Left Pmean | 291.09 (59.27) | 308.03 (60.56) | .263 (.076) | |||
| Right Pmax-mean | 319 (59.48) | 346.63 (76.02) | .111 (.109) | |||
| Left Pmax-mean | 316.22 (66.6) | 339 (72.21) | .194 (.093) | |||
| Dif.Load% | 0.5 (5.97) | -0.5 (7.22) | .548 (.236) | |||
| Gender | n (%) | n (%) | ||||
| Male | 13 (40.6) | 12 (37.5) | .798 | |||
| Female | 19 (59.4) | 20 (62.5) | ||||
| Within-Group change scores immediately after session |
Within-Group change scores 2 days after session |
Within-Group change scores 7 days after session |
|||||||||
| Mean diff. | CI 95% | p-value (Effect size) |
Mean diff. | CI 95% | p-value (Effect size) |
Mean diff. | CI 95% | p-value (Effect size) |
|||
| LUMBAR ROM | Flexion | ||||||||||
| Control | -1.46 | (-3.52,0.6) | .159 (.203) | 1,0 | (-0.97,2.97) | .309 (.138) | 6.19 | (-6.8,19.18) | .339 (.263) | ||
| Stretching | -0.53 | (-3.2,2.14) | .688 (.074) | 1.24 | (-0.69,3.17) | .199 (.180) | 0.64 | (-1.69,2.96) | .581 (.092) | ||
| Extension | |||||||||||
| Control | 1.31 | (-0.67,3.29) | .186 (.165) | -0.31 | (-2.38,1.76) | .760 (.037) | 0.13 | (-2.05,2.3) | .908 (.016) | ||
| Stretching | -1.54 | (-3.69,0.61) | .154 (.151) | -1.44 | (-3.83,0.96) | .230 (.138) | -1.15 | (-3.78,1.48) | .381 (.116) | ||
| Right Rotation | |||||||||||
| Control | -0.21 | (-1.41,1) | .727 (.013) | -1.38 | (-3.52,0.77) | .201 (.082) | -1.25 | (-3.59,1.09) | .284 (.078) | ||
| Stretching | 2.44 | (0.92,3.96) | .003 (.144) | 2.04 | (-0.17,4.26) | .070 (.137) | 2.56 | (0.17,4.96) | .037 (.172) | ||
| Left Rotation | |||||||||||
| Control | -0.42 | (-1.6,0.77) | .479 (.031) | -0.27 | (-1.25,0.71) | .578 (.020) | -0.67 | (-2.18,0.85) | .377 (.050) | ||
| Stretching | 0.5 | (-1.49,2.49) | .612 (.037) | 1.5 | (-0.55,3.55) | .145 (.107) | 1.08 | (-1,3.17) | .297 (.080) | ||
| Right Lateral | |||||||||||
| Control | -0.9 | (-1.93,0.14) | .087 (.186) | 0.65 | (-0.36,1.65) | .201 (.143) | -0.56 | (-1.69,0.57) | .318 (.124) | ||
| Stretching | 1.21 | (-0.14,2.55) | .077 (.253) | 1.46 | (0.01,2.91) | .049 (.317) | 1.58 | (0.14,3.03) | .033 (.323) | ||
| Left Lateral | |||||||||||
| Control | -1.04 | (-1.8,-0.29) | .008 (.208) | 0.63 | (-0.24,1.49) | .150 (.127) | -0.63 | (-1.73,0.48) | .256 (.132) | ||
| Stretching | 0.58 | (-0.56,1.73) | .308 (.111) | 0.63 | (-0.75,2) | .360 (.124) | 1.21 | (0.02,2.4) | .047 (.253) | ||
| PLANTAR PRESSURES | Right Pmax | ||||||||||
| Control | -2.53 | (-23.71,18.65) | .809 (.023) | 9,0 | (-7.08,25.08) | .262 (.080) | -0.13 | (-21.74,21.49) | .991 (.001) | ||
| Stretching | 14.84 | (-9.24,38.93) | .218 (.106) | -21.03 | (-49.25,7.19) | .139 (.161) | -15.44 | (-41.83,10.96) | .242 (.121) | ||
| Left Pmax | |||||||||||
| Control | -11.56 | (-34.39,11.27) | .310 (.101) | 3.09 | (-12.72,18.91) | .693 (.026) | -2.28 | (-24.86,20.29) | .838 (.019) | ||
| Stretching | 6.41 | (-15.15,27.97) | .549 (.046) | -28.09 | (-61.83,5.64) | .099 (.211) | -17.59 | (-43.33,8.14) | .173 (.139) | ||
| Right Pmean | |||||||||||
| Control | 1.72 | (-8.22,11.66) | .727 (.030) | 3.19 | (-5.5,11.88) | .460 (.056) | -0.06 | (-10.09,9.96) | .990 (.001) | ||
| Stretching | 15.22 | (5.54,24.9) | .003 (.231) | -2.16 | (-13.56,9.25) | .702 (.037) | 0.06 | (-11.62,11.74) | .991 (.001) | ||
| Left Pmean | |||||||||||
| Control | -5.81 | (-16.39,4.76) | .271 (.101) | -0.72 | (-9.66,8.22) | .871 (.012) | -0.75 | (-13.36,11.86) | .904 (.013) | ||
| Stretching | 14.69 | (4.64,24.73) | .006 (.207) | -2.03 | (-14.36,10.3) | .739 (.032) | -2.47 | (-14.36,9.42) | .675 (.041) | ||
| Right Pmax-mean | |||||||||||
| Control | -4.25 | (-18.39,9.89) | .544 (.720) | 5.81 | (-5.4,17.03) | .299 (.093) | -0.06 | (-14.07,13.94) | .993 (.001) | ||
| Stretching | -0.38 | (-17.49,16.74) | .965 (.005) | -18.88 | (-38.23,0.48) | .056 (.242) | -15.5 | (-32.58,1.58) | .074 (.209) | ||
| Left Pmax-mean | |||||||||||
| Control | -5.75 | (-19.93,8.43) | .415 (.091) | 3.81 | (-6.31,13.93) | .448 (.058) | -1.53 | (-14.8,11.74) | .815 (.024) | ||
| Stretching | -8.28 | (-23.33,6.76) | .270 (.111) | -26.06 | (-49.91,-2.22) | .033 (.334) | -15.13 | (-31.31,1.06) | .066 (.211) | ||
| Dif.Load% | |||||||||||
| Control | -3.31 | (-5.61,-1.01) | .006 (.536) | -2.13 | (-4.03,-0.22) | .030 (.364) | -1.31 | (-3.11,0.49) | .147 (.229) | ||
| Stretching | -0.13 | (-1.91,1.66) | .887 (.019) | 0.19 | (-1.45,1.83) | .817 (.027) | 0.25 | (-2.23,2.73) | .838 (.038) | ||
| Preintervention | 0 h Postintervention |
2 days Postintervention |
7 days Postintervention |
Group x Time P-value |
Effect Size | |||
| Lumbar ROM | Flexion | .362 | .014 | |||||
| Control | 50.4 (7.1) | 49 (7.3) | 51.4 (7.3) | 56.6 (34.1) | ||||
| Stretching | 48.3 (6.6) | 47.8 (7.6) | 49.6 (7.1) | 49 (7.1) | ||||
| Extension | .380 | .015 | ||||||
| Control | 17.2 (8.2) | 18.5 (7.6) | 16.9 (8.7) | 17.3 (7.1) | ||||
| Stretching | 19.8 (10.6) | 18.3 (9.5) | 18.4 (10.2) | 18.7 (8.6) | ||||
| Right Rotation | .610 | .007 | ||||||
| Control | 10.8 (16.3) | 10.6 (15.6) | 9.4 (13.6) | 9.6 (14.2) | ||||
| Stretching | 13.4 (14.1) | 15.9 (16.1) | 15.5 (15.2) | 16 (15.3) | ||||
| Left Rotation | .569 | .009 | ||||||
| Control | 9 (13.4) | 8.5 (12.9) | 8.7 (12.9) | 8.3 (12.2) | ||||
| Stretching | 12.4 (13.6) | 12.9 (13.1) | 13.9 (14.2) | 13.5 (13.5) | ||||
| Right Lateral | .195 | .026 | ||||||
| Control | 27.6 (4.5) | 26.8 (5) | 28.3 (4.5) | 27.1 (4.6) | ||||
| Stretching | 27.4 (5) | 28.6 (4.4) | 28.8 (3.9) | 28.9 (4.8) | ||||
| Left Lateral | .044 | .051 | ||||||
| Control | 26.1 (5) | 25 (5) | 26.7 (4.8) | 25.4 (3.9) | ||||
| Stretching | 25.5 (5.1) | 26.1 (5.4) | 26.2 (5) | 26.8 (3.8) | ||||
| Plantar Pressures | Right Pmax | .003 | .088 | |||||
| Control | 613.6 (114.2) | 611.1 (103.5) | 622.6 (111.9) | 613.5 (117.3) | ||||
| Stretching | 654.7 (125.8) | 669.6 (143.9) | 633.7 (133.8) | 639.3 (128.8) | ||||
| Left Pmax | .008 | .074 | ||||||
| Control | 607.3 (119.5) | 595.8 (103.7) | 610.4 (113.4) | 605 (115.3) | ||||
| Stretching | 647 (126.7) | 653.4 (141.5) | 618.9 (137.6) | 629.4 (125.9) | ||||
| Right Pmean | .025 | .057 | ||||||
| Control | 294.6 (58.4) | 296.3 (53.1) | 297.8 (55) | 294.6 (60) | ||||
| Stretching | 308.1 (56.9) | 323.3 (66.6) | 305.9 (59.6) | 308.2 (60.2) | ||||
| Left Pmean | .002 | .097 | ||||||
| Control | 291.1 (59.3) | 285.3 (55.4) | 290.4 (62.1) | 290.3 (59.7) | ||||
| Stretching | 308 (60.6) | 322.7 (71.1) | 306 (66.1) | 305.6 (60.6) | ||||
| Right Pmax-Mean | .007 | .077 | ||||||
| Control | 319 (59.5) | 314.8 (58.6) | 324.8 (64) | 318.9 (63.3) | ||||
| Stretching | 346.6 (76) | 346.3 (82.4) | 327.8 (79.5) | 331.1 (71.7) | ||||
| Left Pmax-Mean | .065 | .045 | ||||||
| Control | 316.2 (66.6) | 310.5 (54.5) | 320 (57.6) | 314.7 (59.4) | ||||
| Stretching | 339 (72.2) | 330.7 (76) | 312.9 (82.3) | 323.9 (70.9) | ||||
| Dif.Load% | .463 | .012 | ||||||
| Control | 0.5 (6) | -2.8 (6.4) | -1.6 (5.7) | -0.8 (5.4) | ||||
| Stretching | -0.5 (7.2) | -0.6 (5.2) | -0.3 (6.1) | -0.3 (5.7) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





