1. Introduction
The first few cases of the COVID-19 pandemic, caused by the SARS-CoV-2 virus, were detected in December 2019 in Wuhan, China. Since then, the virus rapidly spread to all parts of the world leading to an unprecedented number of cases and deaths, the likes of which humanity has not experienced in centuries [
1]. As of December 13, 2023, there have been 772,386,069 cases and 6,987,222 deaths on a global scale due to COVID-19 [
2].
Research indicates that during pandemics of the past, the prevalence of mental health issues seemed to surpass the number of individuals impacted by the illness [
3]. The COVID-19 pandemic has not only caused physical health issues, but it has also had global impacts on social, psychological, and economic aspects. The disruption of normal life including remote jobs, remote education, limited recreational activities for children, and fewer interactions with other people on account of social distancing, has led to an increase in mental health problems, such as fear of illness, stress, anxiety disorders, sleep problems, mood disorders, and suicidal thoughts [
4,
5,
6,
7]. Furthermore, the fear and stress caused by COVID-19 have resulted in symptoms such as changes in sleep and eating habits, deterioration of existing psychological disorders, and increased use of substances like alcohol, tobacco, and drugs [
8,
9,
10,
11]. In view of the same, the work presented in this paper aims to investigate multiple factors related to the fear and response associated with COVID-19 by performing a comprehensive analysis of survey responses from a dataset comprising responses of participants from 40 countries - Australia, Austria, Belgium, Canada, Chile, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hong Kong (S.A.R.), Hungary, India, Ireland, Israel, Italy, Japan, Latvia, Mexico, Netherlands, New Zealand, Norway, Peru, Poland, Portugal, Romania, Russian Federation, Slovenia, South Africa, South Korea, Spain, Sweden, Switzerland, Turkey, United Arab Emirates, United Kingdom, and USA.
1.1. Overview of COVID-19 and its Effect on Humans
The SARS-CoV-2 virus, responsible for causing COVID-19, is similar to SARS-CoV and MERS-CoV. However, compared to SARS and MERS, COVID-19 has a lower fatality rate (estimated at 2%–3%) but has caused a more widespread global impact [
12]. Coronaviruses (CoVs) exhibit distinctive peplomers resembling a crown under an electron microscope, which led to their name "corona" meaning “crown” or “halo” [
13,
14,
15]. The coronavirus family comprises four main subgroups: α, β, γ, and δ. The α subgroup includes members, such as Cov-229E and CoV-HKU1. Meanwhile, the β subgroup, housing human pathogens like CoV-OC43, SARS-CoV, and MERS-CoV, includes SARS-CoV-2 [
16]. The amino acid sequences in the genomic open reading frame 1ab (ORF1ab) show 94.6% identity between SARS-CoV-2 and the original SARS-CoV. The SARS-CoV-2 virus exhibits a virion diameter ranging from 60 to 140 nm and carries a positive-sense, single-stranded RNA genome of 29,891 base pairs [
17]. When comparing its genome sequence, there's a 79.5% identity with SARS-CoV and an impressive 93.1% identity with the RaTG12 virus found in a bat species called Rhinolophus affinis in Yunnan Province, China [
18,
19]. An in-depth examination of the SARS-CoV-2 genome alongside SARS-CoV has resulted in the identification of nearly thirty ORFs and two novel insertions [
20,
21,
22,
23].
The SARS-CoV-2 virus, akin to SARS-CoV, gains entry into human lung type II pneumocytes by binding its S protein to the cell surface receptor ACE2 [
24]. This S protein consists of two key domains: the S1 domain at the N-terminus binds to ACE2, while the C-terminal S2 domain facilitates viral membrane fusion with the host cell [
25]. The receptor-binding domain (RBD) within the S1 domain, specifically comprising amino acids 424–494, directly interacts with ACE2 [
26]. Cleavage sites at R667 and R797 in the S protein are crucial for viral entry, mediated by various proteases like cathepsin L, trypsin, and TMPRSSs [
27]. Comparative analysis shows limited homology between SARS-CoV-2 and SARS-CoV in the S1 domain (64%) but higher similarity in the S2 domain (up to 90%). Within the S1 RBD domain, there are four to five distinct amino acid changes in SARS-CoV-2, including X442, F472, C479, and N487 [
27]. The S protein of SARS-CoV-2 demonstrates a higher affinity for ACE2 than that of SARS-CoV, potentially up to 10–20 times stronger [
27,
28]. SARS-CoV-2's transmissibility, notably higher than SARS-CoV and MERS, is linked to its S protein sequence, which contains an insertion adjacent to the cleavage site. This insertion, comprising P681, R682, R683, and A684, creates an exposed loop, enhancing susceptibility to proteases like TMPRSS1 and TMPRSS2, thereby aiding in viral binding and entry [
29,
30,
31]. While many instances have indicated the infection of different organs in the human body, the SARS-CoV-2 virus primarily targets the respiratory systems of patients [
32,
33]. The investigation of the first few cases of COVID-19 from Wuhan, China has provided insights into a range of symptoms that patients often suffer during the first days after contracting COVID-19. These symptoms include fever, dry cough, breathing difficulties, headache, dizziness, fatigue, nausea, and diarrhea. It is important to note that individuals may not have identical symptoms and that the severity of one or more symptoms of COVID-19 may vary significantly from person to person [
34,
35].
1.2. An Overview of the Fear Related to COVID-19 on a Global Scale
Although fear is often categorized as a negative emotion, its functionality lies in its ability to ensure individuals’ survival in threatening situations. Humans have historically been exposed to a variety of pathogens and diseases. However, with the development of modern medicine, the risk of exposure to these pathogens has greatly decreased. For example, vaccination, nutrition, and better public health measures have completely eradicated the risk of multiple common diseases [
36].
Despite medical and technological innovations, infectious diseases such as COVID-19 remain a major cause of morbidity in the modern world. The enduring prevalence of such infectious diseases underscores the evolutionary pressure they have exerted on humans, leading to both physiological and behavioral adaptations. One such adaptation is the development of a behavioral immune system, comprising proactive mechanisms that actively prevent contact with infectious pathogens [
37,
38]. This system complements people’s physiological immune defenses and guides behaviors to minimize infection risk. For example, when an individual is faced with potential signals of infection, a collection of emotional, cognitive, and behavioral responses is triggered, with fear playing a central role. This fear, deeply rooted in human’s evolutionary past, is not just a reaction but a biologically predisposed form of learning, embedded in the human mind. In other words, fear of infection is ingrained in people’s emotional brain [
39]. In the context of COVID-19, fear of infection manifests itself through xenophobia, conformism, and authoritarianism. Moreover, fear has influenced public behaviors and attitudes ranging from adherence to health guidelines to social phenomena like “germ panic” [
38]. At the start of the pandemic, fear served as a motivator for people to maintain hygienic practices and follow social distancing rules. However, fear has also obstructed people’s ability to respond rationally to covid-19 pandemic. When fear becomes a present and constant component of life, it results in psychological issues such as depression, anxiety, stress, mood swings, and attention deficits [
40]. Thus, while fear is an innate protective mechanism it can also lead to irrational behaviors and stigmatization. Alongside the spread of COVID-19, was the spread of misinformation about the disease on social media. The extensive amount of misinformation further contributed to stigmatization and fear of infection.
Recent research in this field [
41] indicates that psychiatrists, psychologists, and therapists played a crucial role in helping those impacted by the fear of COVID-19 because they served as mediators to enhance awareness, attitudes, and behaviors related to the pandemic, while also addressing the widespread fear and anxiety. The interventions from psychiatrists, psychologists, and therapists included educating the public about the detrimental mental effects surrounding COVID-19 infections, promoting health-benefiting behaviors, and working alongside other healthcare professionals to develop intervention strategies for periods of heightened distress. Additionally, they facilitated adaptation to quarantine life, helped individuals maintain a positive outlook throughout the pandemic, and provided essential self-care methods, including peer support and therapy. On a global scale, virtual appointments with psychiatrists, psychologists, and therapists increased on account of lockdowns and social distancing guidelines in different regions [
42,
43,
44]. However, the response of the global population towards seeking and receiving mental health-related help from psychiatrists, psychologists, or therapists in the context of fear of COVID-19 was affected by multiple factors. First, virtual meetings were associated with challenges such as outdated software or hardware and the patient's inability to use the necessary software or hardware [
45]. Second, patients who were not content with the quantity of information related to COVID-19 showed a diminished degree of trust in their medical care providers [
46]. Third, as prior work in this field [
47] indicates, attitudes, values, and belief systems transmitted by family, companionship, and friendship networks influence the manner in which an individual defines and acts upon mental health-related problems. Fourth, most therapists had concerns about security and confidentiality in the context of virtually meeting their patients [
48]. Fifth, many psychologists felt that they required more skills to effectively manage crisis situations during online sessions [
48].
Even though there have been multiple works conducted in the last couple of years that focused on the investigation of the fear and response related to COVID-19, those works have multiple limitations (as discussed in detail in
Section 2). The work presented in this paper aims to address these limitations by performing a comprehensive analysis of a dataset of survey responses associated with the fear and response to COVID-19. The rest of this paper is organized as follows. A review of recent works in this field is presented in
Section 2.
Section 3 discusses the methodology that was followed in this study. The results are presented in
Section 4 which is followed by the conclusion in
Section 5.
3. Methodology
This section describes the step-by-step methodology that was followed for the work presented in this paper. The dataset used for this study was developed by Mertens et al. [
76]. In this work [
76] the authors developed an open-access dataset by using surveys that were intended to measure various characteristics related to the fear of COVID-19. This dataset comprises the data collected from two cohorts. The first cohort mostly comprised Dutch participants who participated in a cross-sectional survey in March 2020. The second cohort comprised a comprehensive longitudinal survey with a sample size of 2000. Participants in this cohort were from 40 countries - Australia, Austria, Belgium, Canada, Chile, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hong Kong (S.A.R.), Hungary, India, Ireland, Israel, Italy, Japan, Latvia, Mexico, Netherlands, New Zealand, Norway, Peru, Poland, Portugal, Romania, Russian Federation, Slovenia, South Africa, South Korea, Spain, Sweden, Switzerland, Turkey, United Arab Emirates, United Kingdom, and USA. The participants of the second cohort responded to the survey from April 2020 to August 2020. Furthermore, an additional assessment was conducted in June 2021. The survey encompassed various parameters such as the extent of fear towards COVID-19, demographic data, characteristics of anxious behavior, media consumption, self-assessed health status, perceived capability to prevent infection, and perceived risk for loved ones. The participants were also queried about their COVID-19 vaccination status and their intentions to get the vaccine. Mertens et al. [
76] recruited participants for the first cohort using online ads on various social media platforms. For the second cohort, they recruited participants through the Prolific platform. The only inclusion criteria for both cohorts was that individuals had a satisfactory level of proficiency in the English language. Questionnaires were administered via an online survey utilizing the Qualtrics platform in both cohorts. Participants did not receive any kind of compensation during the first cohort. However, during the second cohort, participants were remunerated according to the prevailing standard rate of Prolific at the time of data collection, which was £7.5 per hour. For the development of this dataset, Mertens et al. [
76] evaluated the fear of COVID-19 the Fear of the Coronavirus Questionnaire (FCQ) as prior works in this field showed the reliability of the same [
77,
78]. The questionnaire consisted of 8 items that assessed various aspects of fear. Participants were required to indicate their degree of agreement with each statement using a 5-point Likert scale, ranging from 1 (indicating "Strongly disagree") to 5 (indicating "Strongly agree").
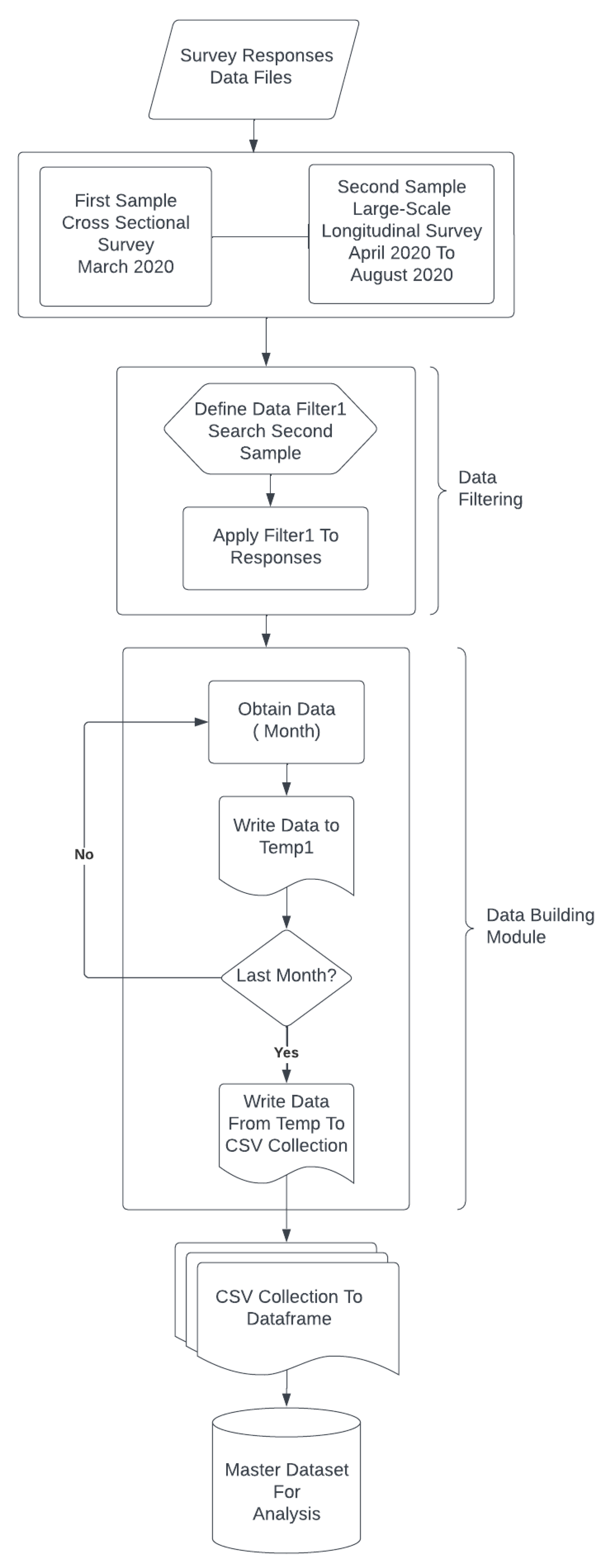
As the work presented in this paper analyzes the fear and response related to COVID-19 by also taking into account the age group of individuals, the data files related to the second cohort of the study performed by Mertens et al. [
76] were used to develop the master dataset for analysis. The process that was followed for the development of this master dataset for analysis is presented in
Figure 1. The responses for the specific questions from the master dataset that were analyzed in this study were “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am very worried about the coronavirus outbreak.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am taking precautions to prevent infection (e.g., washing hands, avoiding contact with people, avoiding door handles).”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am constantly following all news updates regarding the virus.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I have stocked up on supplies to prepare for problems related to the coronavirus outbreak.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - for my personal health I find the virus to be much more dangerous than the seasonal flu.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I feel that the health authorities are not doing enough to deal with the virus.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am worried that friends or family will be infected.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I take more precautions compared to most people to not become infected.”, “please describe briefly your biggest concern about coronavirus”, “are you currently seeing or planning to see a psychologist or psychiatrist for any mental health issues relating to the coronavirus?” and “what is your age?”. The responses for the first 8 questions were provided by the participants as “strongly agree”, “strongly disagree”, “somewhat agree”, “somewhat disagree”, or “neither agree nor disagree”. For the next question from this list, i.e. “please describe briefly your biggest concern about coronavirus”, participants stated their specific concerns using a choice of words. For the next question from this list, i.e. “are you currently seeing or planning to see a psychologist or psychiatrist for any mental health issues relating to the coronavirus?”, the participants provided their responses as “Yes”, “Yes (currently seeing a psychologist/psychiatrist)”, “Yes (planning to see a psychologist/psychiatrist)”, or “No”. In view of the fact that participants who selected “Yes” for this question could have meant either “Yes (currently seeing a psychologist/psychiatrist)” or “Yes (planning to see a psychologist/psychiatrist)” but were not specific, the responses “Yes (currently seeing a psychologist/psychiatrist)” and “Yes (planning to see a psychologist/psychiatrist)” were changed to “Yes” for data analysis. For the last question from this list – “what is your age?” the participants informed their age by selecting one option out of 11-20, 21-30, 31-40, 41-50, 51-60, 61-70, or 71-80.
After the development of the master dataset for analysis, subjectivity analysis of the responses of the participants per month for the question - “please describe briefly your biggest concern about coronavirus” was performed using TextBlob. TextBlob, developed by Lauria [
79], uses a lexicon-based approach with a set of built-in rules to perform subjectivity analysis. The subjectivity score for a sentence from TextBlob is a number that lies between 0 and 1. Subjectivity refers to the extent of personal opinion expressed in a sentence. A high degree of subjectivity, indicated by a value near 1, suggests that the text includes a greater amount of personal opinion rather than facts. TextBlob was used for performing subjectivity analysis in this work as TextBlob has been used for subjectivity analysis in several prior works [
80,
81,
82,
83] in this field. The subjectivity analysis was performed to compute the variation of subjectivity per month per age group where the analyzed age groups were 11-20, 21-30, 31-40, 41-50, 51-60, 61-70, 71-80, and 81-90. In addition to this, the percentage of highly opinionated, neutral opinionated, and least opinionated responses per age group was also computed. The pseudocode of the program that was written in Python 3.11.5 to perform this analysis is shown in Algorithm 1. As can be seen from the pseudocode of Algorithm 1, the responses were categorized into multiple subjectivity classes – least opinionated, neutral opinionated, and highly opinionated based on the subjectivity score. If the subjectivity score of a response was less than 0.4, then that response was categorized as “least opinionated”. If the subjectivity score of a response was greater than 0.6, then that response was categorized as “highly opinionated”. Finally, if the subjectivity score of a response was between 0.4 and 0.6, then that response was categorized as “neutral opinionated”. This approach for assigning a subjectivity class to a response based on the associated subjectivity score that was followed in this work is inspired by multiple prior works in this field (for example: [
84] and [
85]) where the same ranges of subjectivity scores were used to assign a subjectivity class out of “least opinionated”, “neutral opinionated”, and “high opinionated”, to a given text.


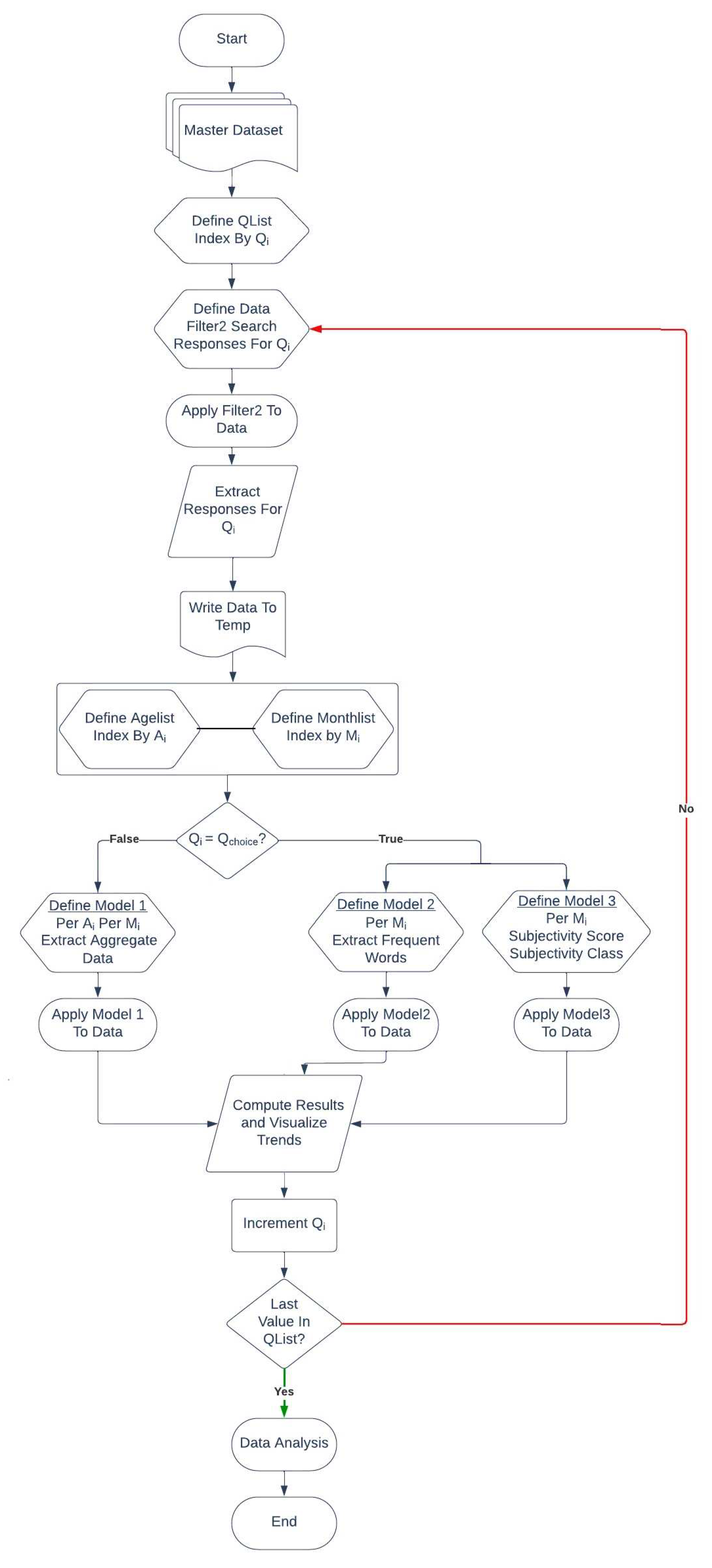
Thereafter, the responses to this question on a monthly basis were studied using a word cloud-based analysis. Word clouds, also known as tag clouds, are visual depictions of word frequency that emphasize terms that occur more often in a given text. The size of a word in a word cloud indicates its frequency of occurrence in the document(s) [
86]. The pseudocode of the program that was written in Python 3.11.5 to perform this analysis is shown in Algorithm 2. After completion of this analysis, the number of responses per age group for the questions (Qlist) - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am very worried about the coronavirus outbreak.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am taking precautions to prevent infection (e.g., washing hands, avoiding contact with people, avoiding door handles).”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am constantly following all news updates regarding the virus.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I have stocked up on supplies to prepare for problems related to the coronavirus outbreak.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - for my personal health I find the virus to be much more dangerous than the seasonal flu.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I feel that the health authorities are not doing enough to deal with the virus.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am worried that friends or family will be infected.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I take more precautions compared to most people to not become infected.”, “are you currently seeing or planning to see a psychologist or psychiatrist for any mental health issues relating to the coronavirus?” were analyzed in an aggregate manner using stacked bar charts. In other words, this analysis took into account the responses for Qlist for all the months from the master dataset. The pseudocode of the program that was in Python 3.11.5 to perform this analysis is shown in Algorithm 3. The step-by-step working of Algorithms 1 to 3 on the master dataset is shown in
Figure 2.


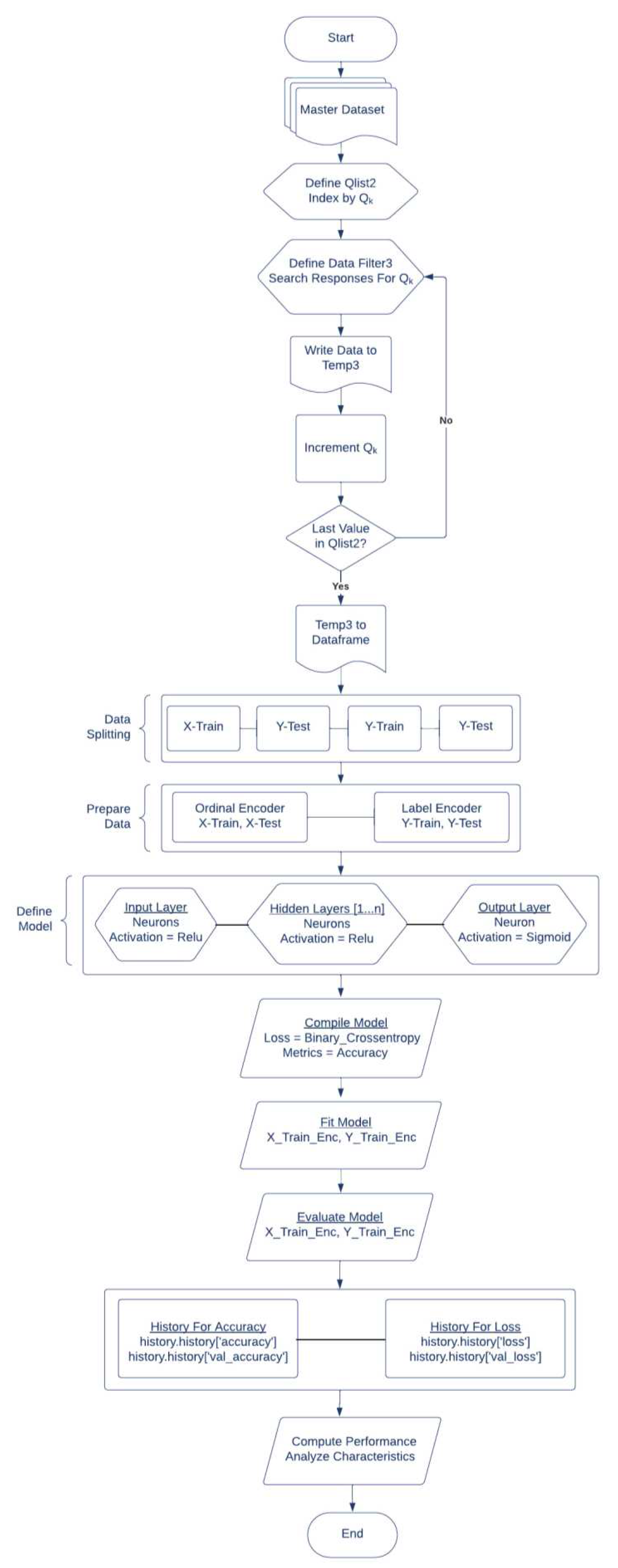
Thereafter, a Deep learning model [
87] was developed to detect if the survey respondents were seeing or planning to see a psychologist or psychiatrist for any mental health issues related to COVID-19. Deep learning is regarded as an evolution of machine learning that integrates algorithms to acquire knowledge from data in order to perform certain tasks without the need for explicit programming [
88]. Deep learning methods are more accurate than typical machine-learning approaches. For a long time, the task of creating a feature extractor for machine learning systems required the manual creation of features in order to streamline the learning process which requires human experience and substantial domain comprehension [
89]. Deep learning enables systems to learn from errors. During this learning process, systems acquire information from data by using a general-purpose learning process, hence reducing the need for extensive human experience to explicitly specify all the necessary knowledge for the system [
90]. Deep learning models use a hierarchical network structure, referred to as an artificial neural network, that is designed to mimic the interconnected networks observed in the human brain. Embedding layers in this structure gives a much more efficient learning experience for the system as compared to conventional machine learning models. Furthermore, deep learning sets itself apart from machine learning by its capacity to extract sophisticated features from vast quantities of input data, known as feature engineering [
91]. Therefore, deep learning was used in this research work. Specifically, this deep learning model detected the response to the question “are you currently seeing or planning to see a psychologist or psychiatrist for any mental health issues relating to the coronavirus?” (QSpecific).
The specific responses that were used to develop this Deep Learning model comprised their responses to the questions “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am very worried about the coronavirus outbreak.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am taking precautions to prevent infection (e.g., washing hands, avoiding contact with people, avoiding door handles).”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am constantly following all news updates regarding the virus.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I have stocked up on supplies to prepare for problems related to the coronavirus outbreak.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - for my personal health I find the virus to be much more dangerous than the seasonal flu.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I feel that the health authorities are not doing enough to deal with the virus.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am worried that friends or family will be infected.”, and “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I take more precautions compared to most people to not become infected”. The developed deep learning model used 75% data for the training set and 25% data for the test set. The design of the deep learning model comprised 8 neurons for the input layer with the ReLU activation function, the ReLU activation function for all the hidden layers with 12 neurons, and the sigmoid activation function for the output layer with 1 neuron. The model used the rectifier or ReLU (rectified linear unit) activation function for the input layer and all the hidden layers and the sigmoid activation function for the output layer. The pseudocode of the program that was written in Python 3.11.5 to develop this model is shown in Algorithm 4 and the step-by-step working of Algorithm 4 is shown in
Figure 3.

4. Results and Discussions
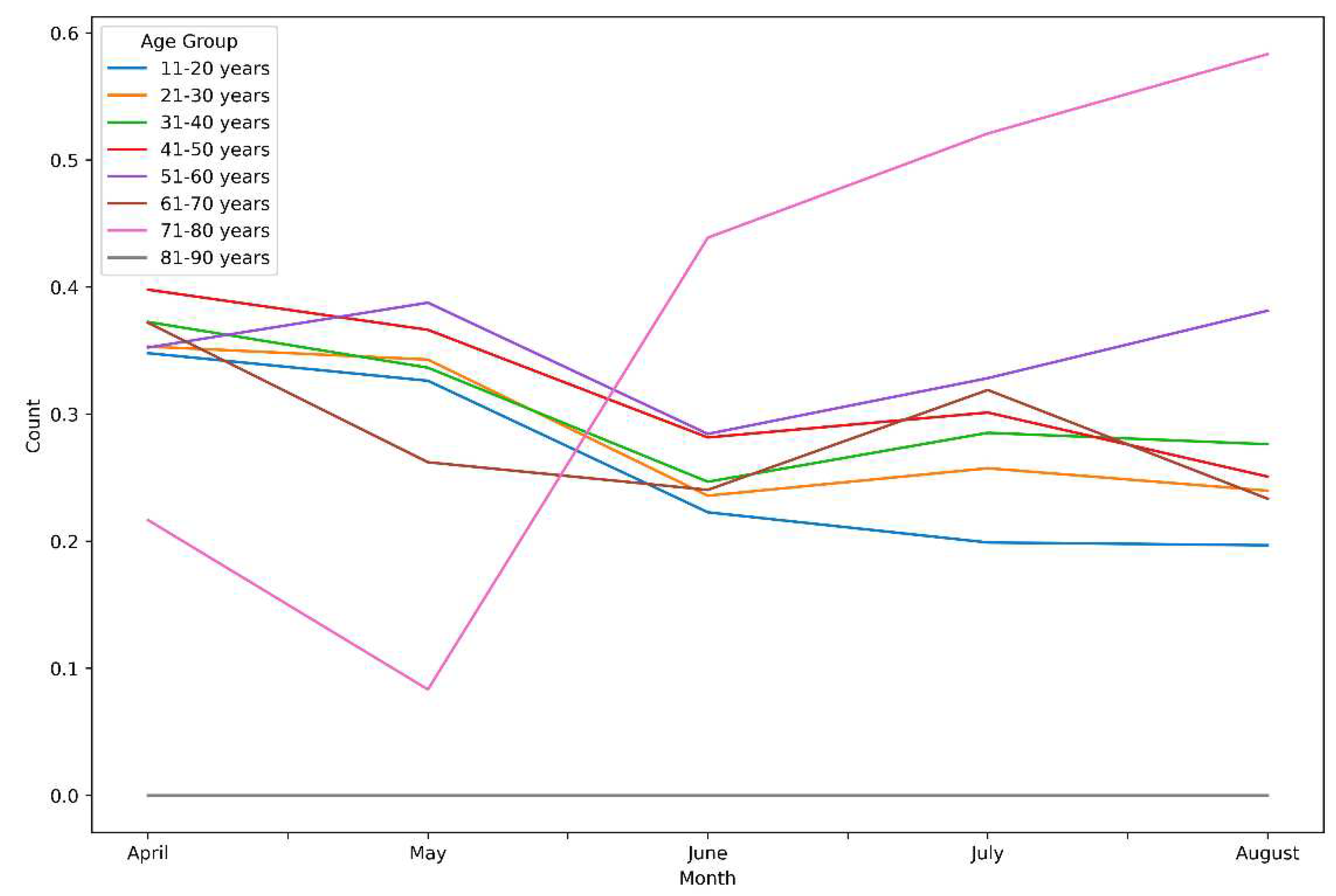
This section presents the results of this research work. As discussed in
Section 3, Algorithm 1 performed subjectivity analysis of the responses per age group for the question - “please describe briefly your biggest concern about coronavirus”. The results of this analysis are shown in
Figure 4. The subjectivity score for a sentence was output by Algorithm 3 as a number that lies between 0 and 1 where a high degree of subjectivity is indicated by a value near 1.
Figure 4 reveals multiple novel insights in this context. For example, the average subjectivity in responses by the age group of 41-50 decreased from April 2020 to June 2020. The average subjectivity in responses by the age group of 71-80 drastically increased from May 2020. The age group of 11-20 indicated the least level of subjectivity in their responses between June 2020 to August 2020.
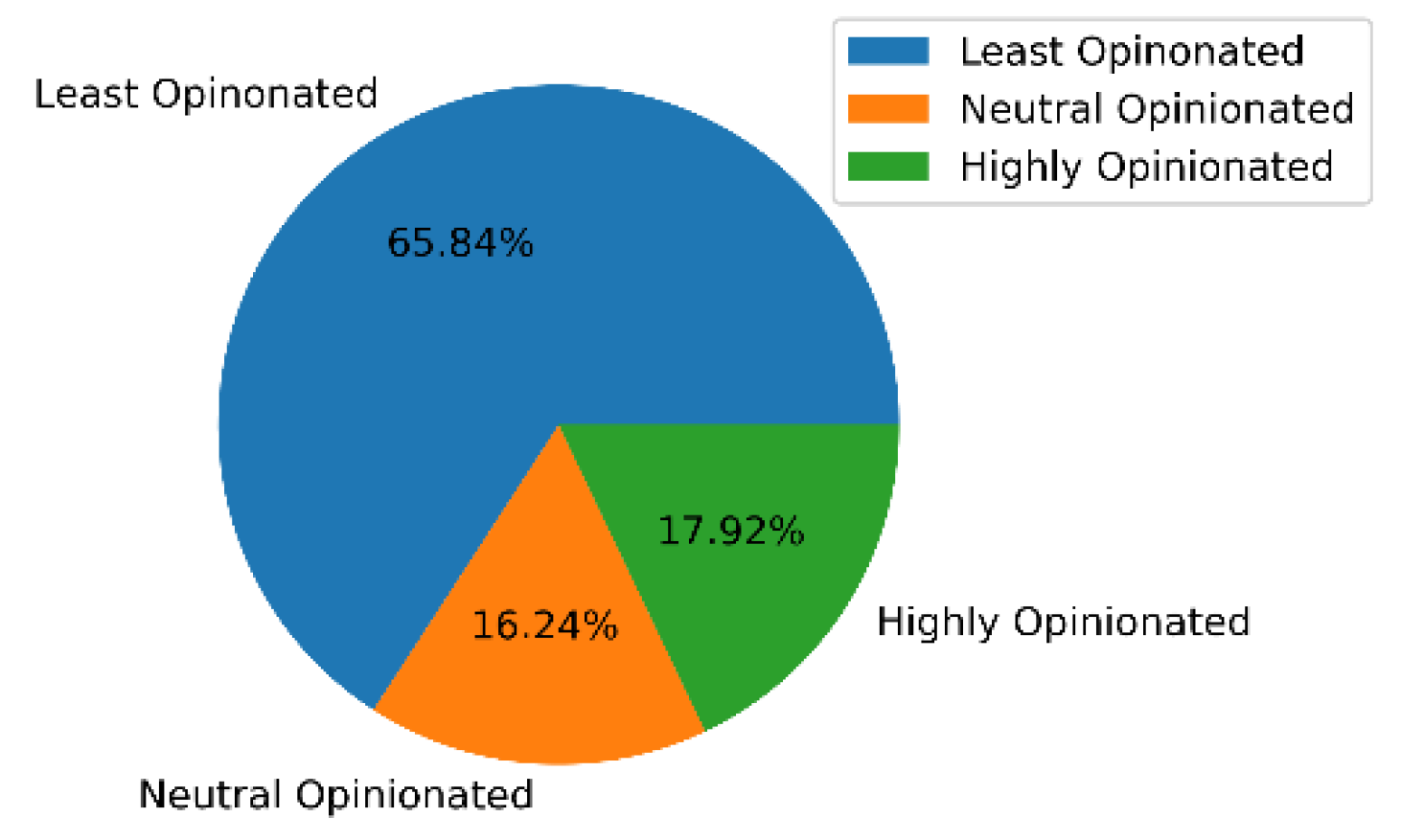
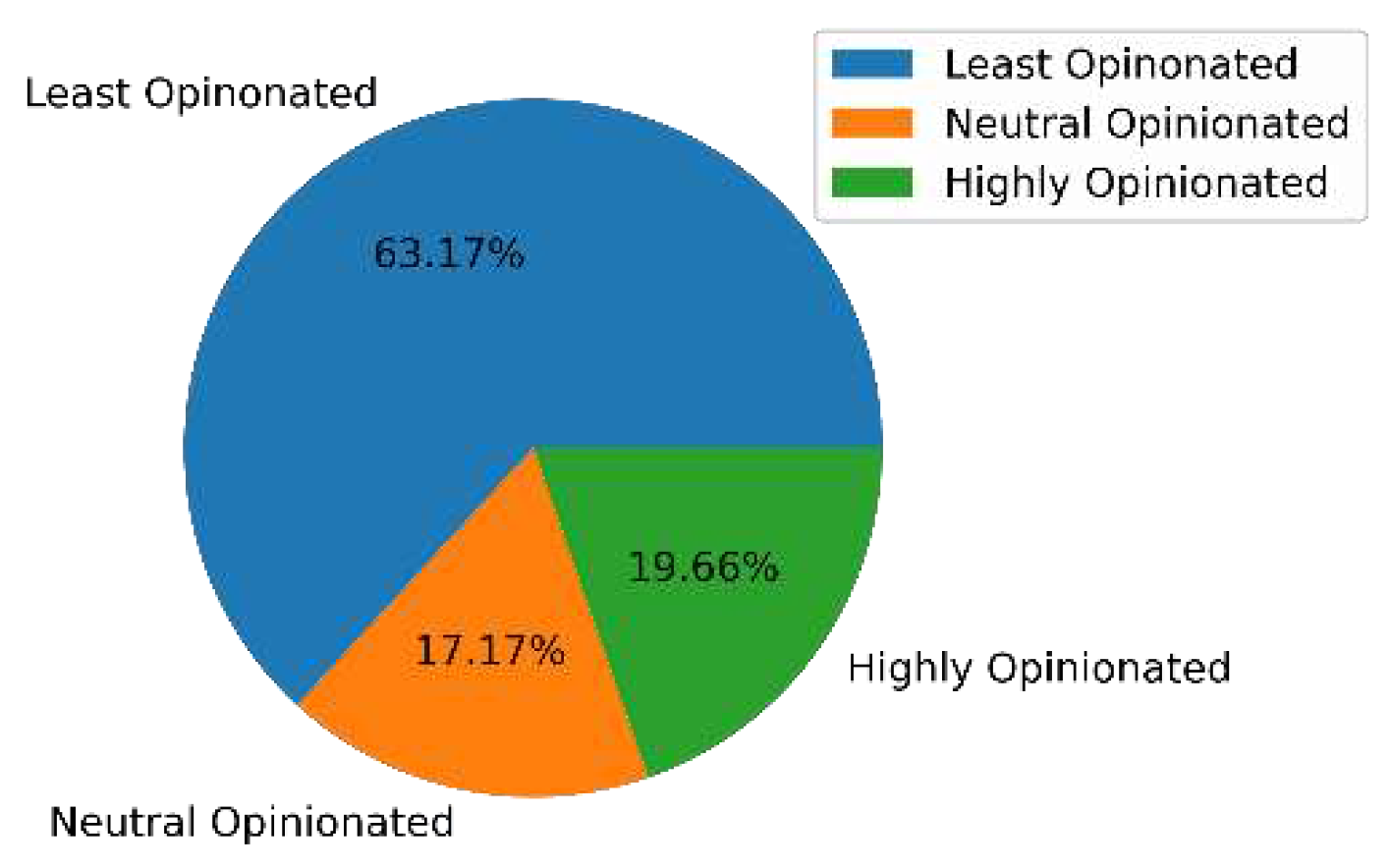
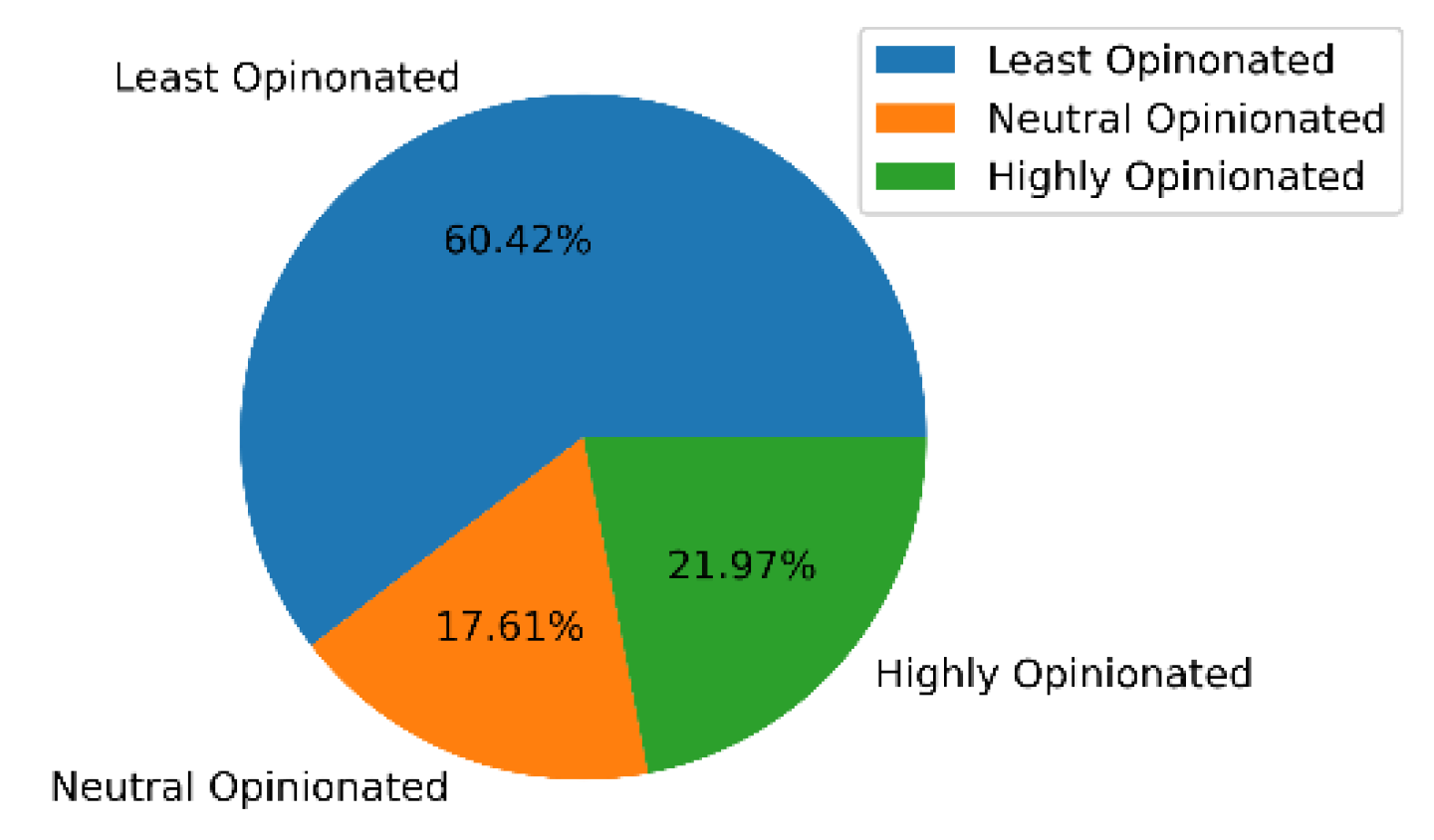
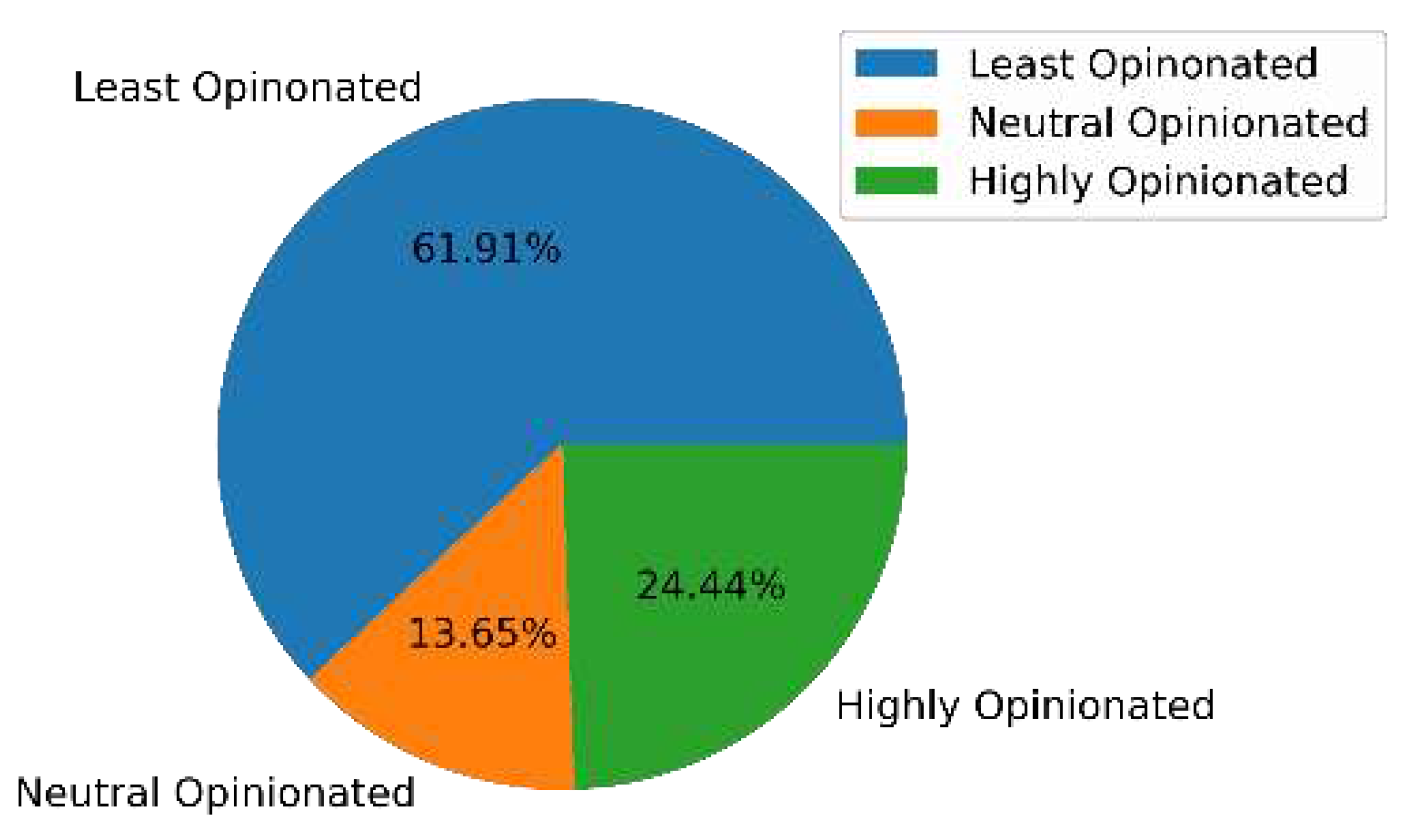
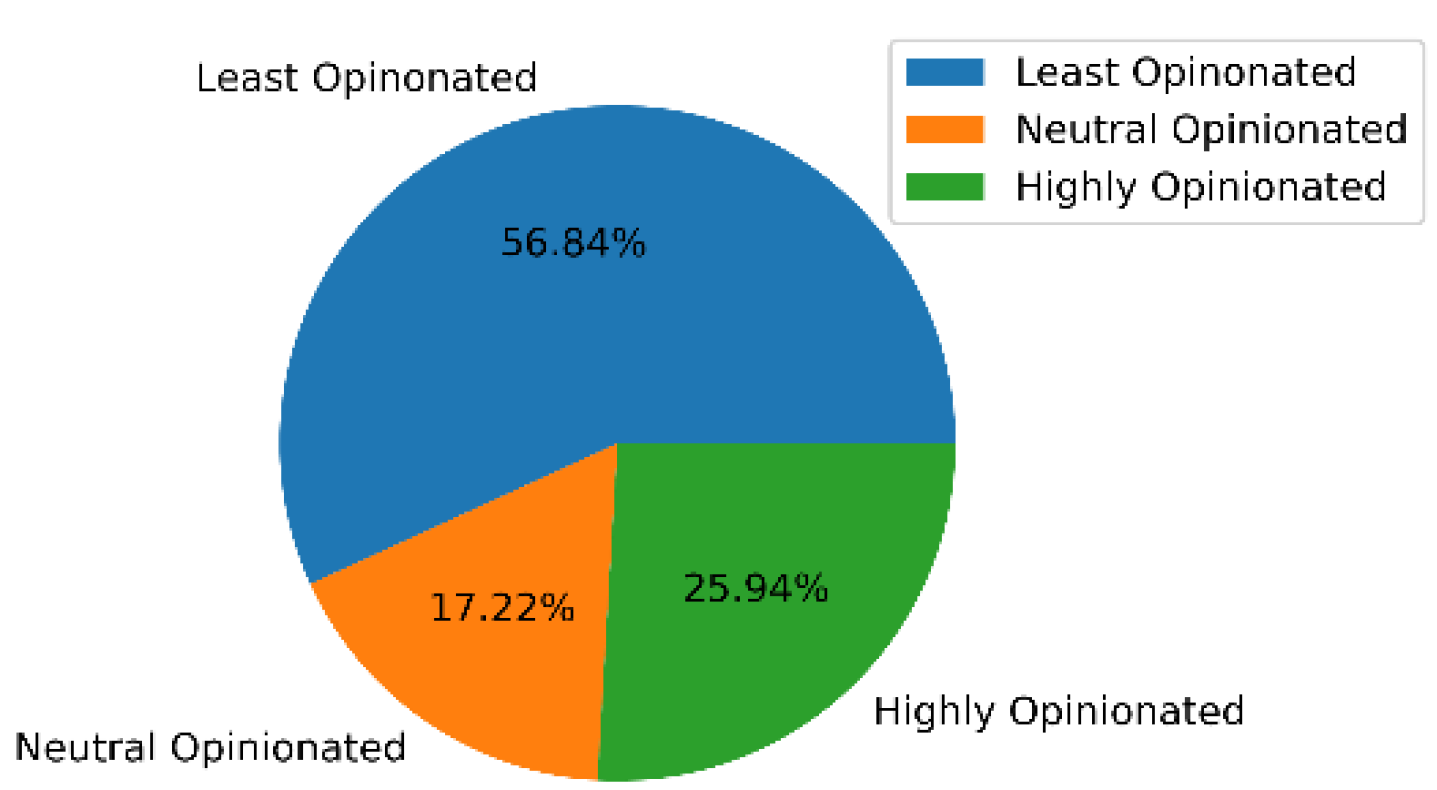
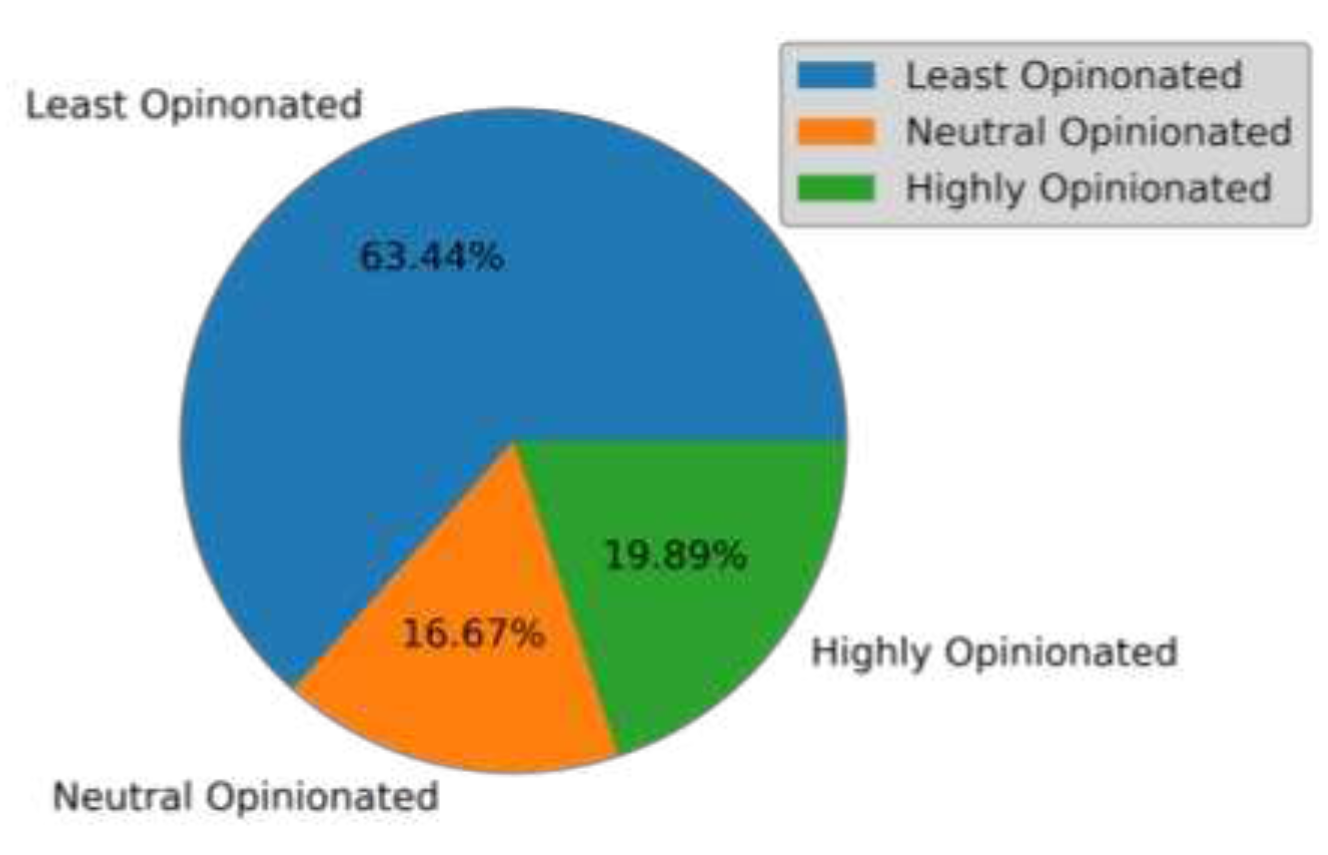
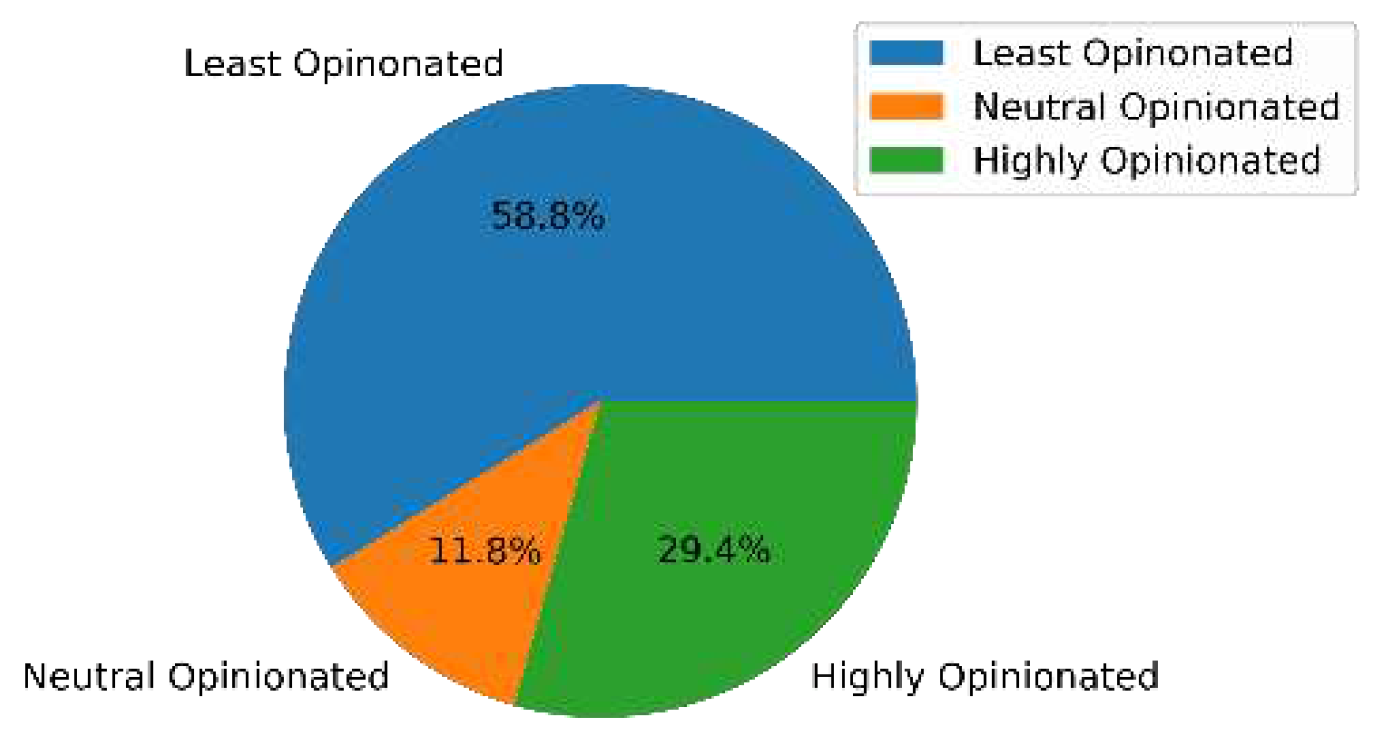
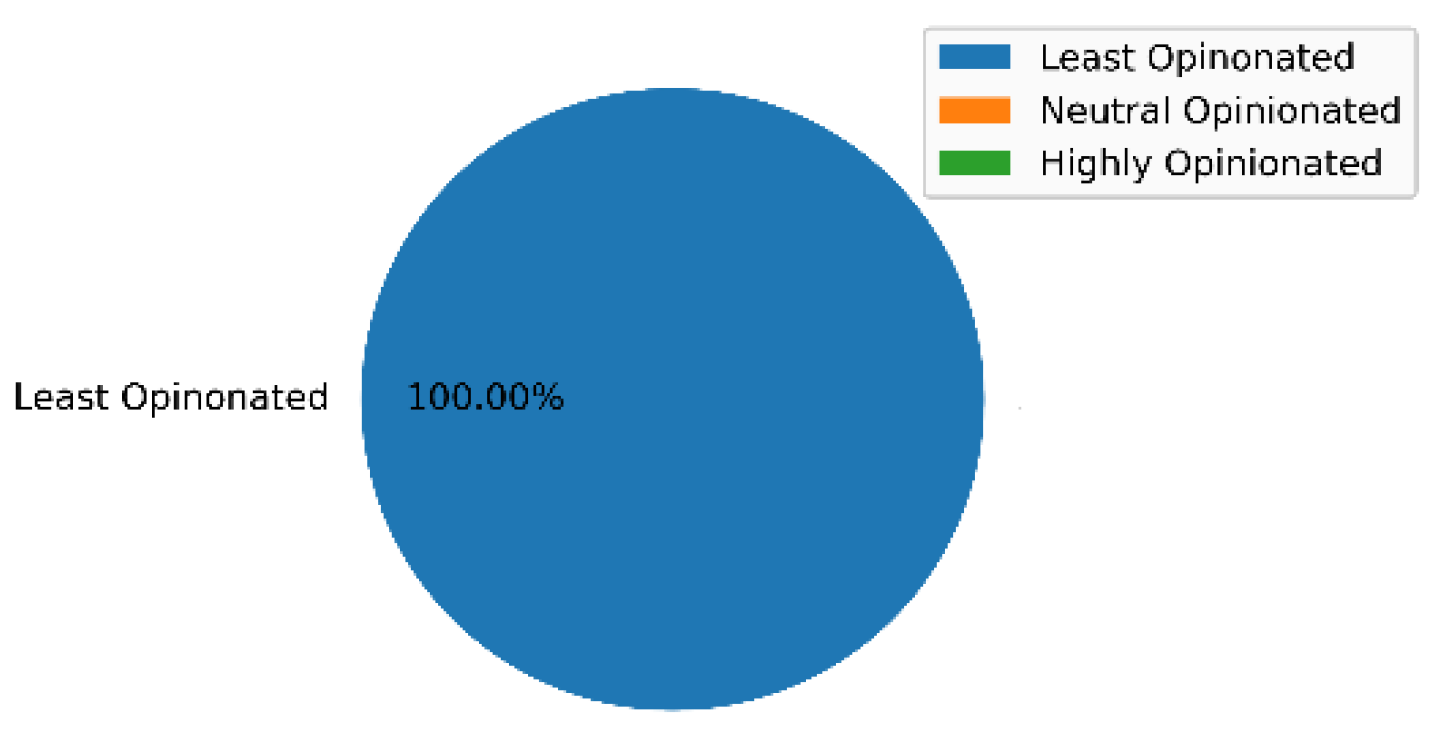
Thereafter, fine-grain analysis of these responses per age group was performed by Algorithm 1 to classify the responses as highly opinionated, neutral opinionated, and least opinionated. The results of the same are shown in
Figure 5,
Figure 6,
Figure 7,
Figure 8,
Figure 9,
Figure 10,
Figure 11 and
Figure 12, respectively.
The results of this analysis reveal the response patterns per age group. For instance, the percentage of highly opinionated, neutral opinionated, and least opinionated responses by the age group of 11-20 were 17.92%, 16.24%, and 65.84%, respectively. From this distribution, it can be inferred that a majority of the responses from the age group of 11-20 were least opinionated. A similar distribution can be seen for the age groups of 21-30 and 31-40 as well. Comparison of these distributions also revealed novel patterns related to the responses provided by different age groups. For instance, the age group of 71-80 posted the highest percentage of highly opinionated responses and the age group of 31-40 posted the highest percentage of neutral opinionated responses.
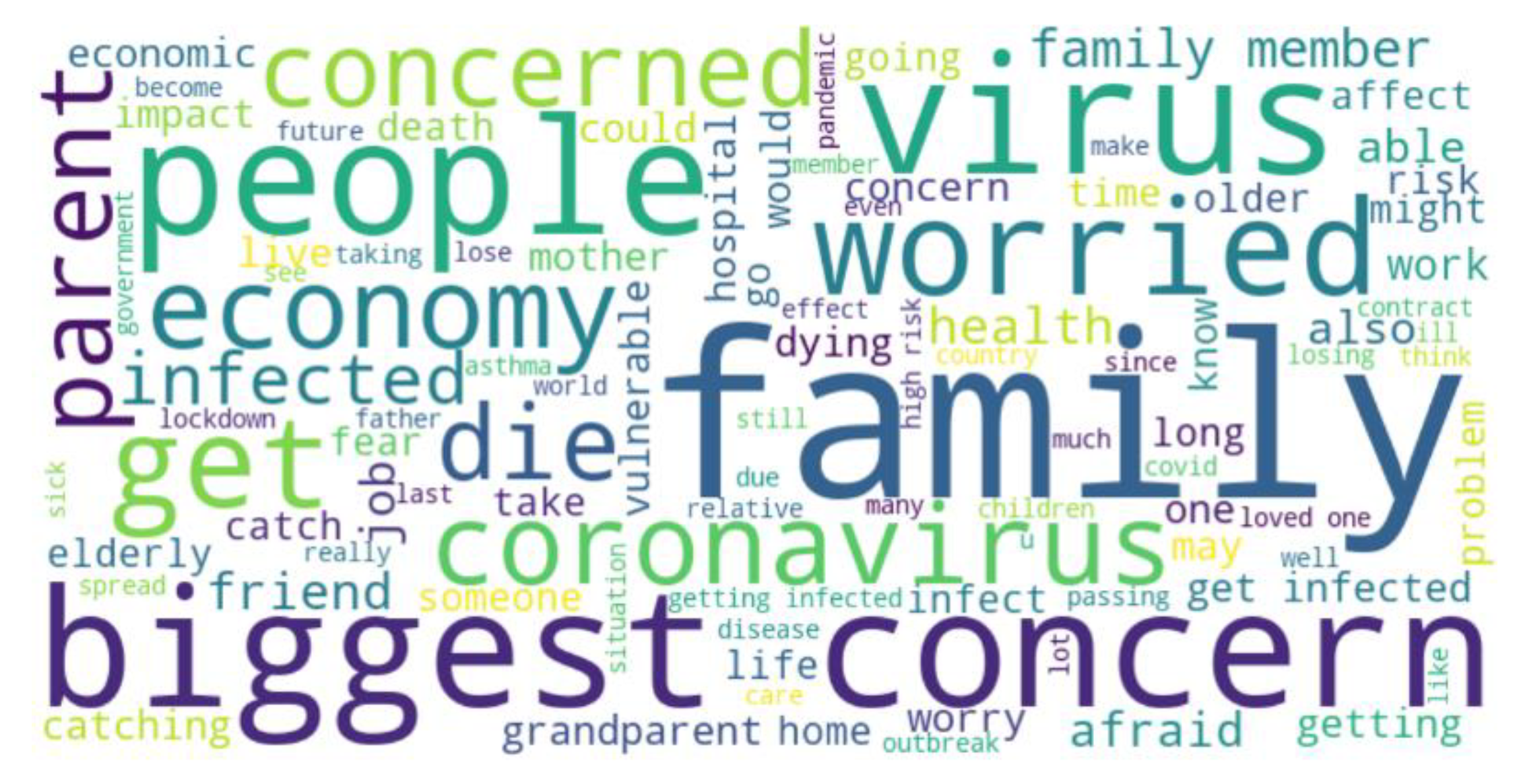
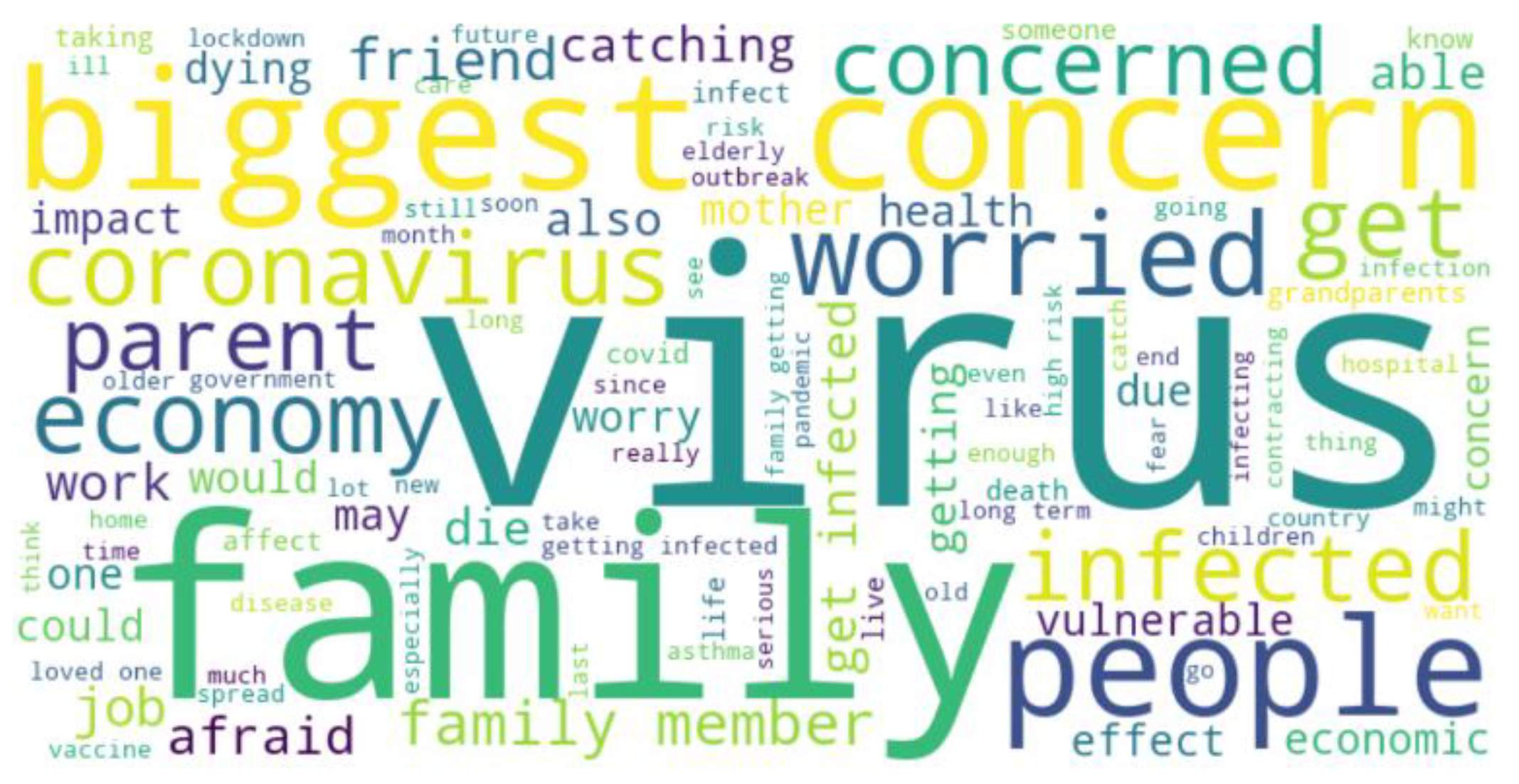
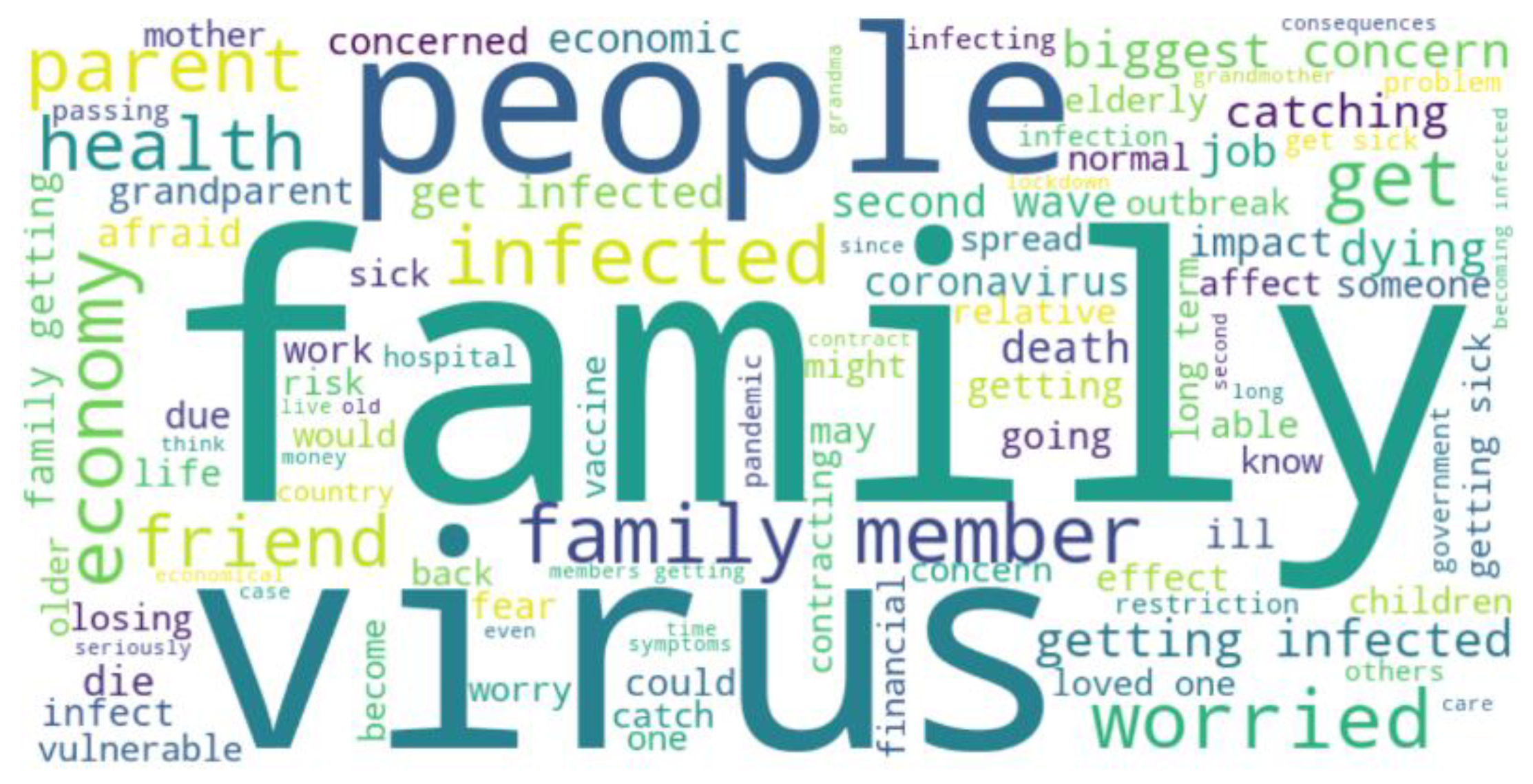
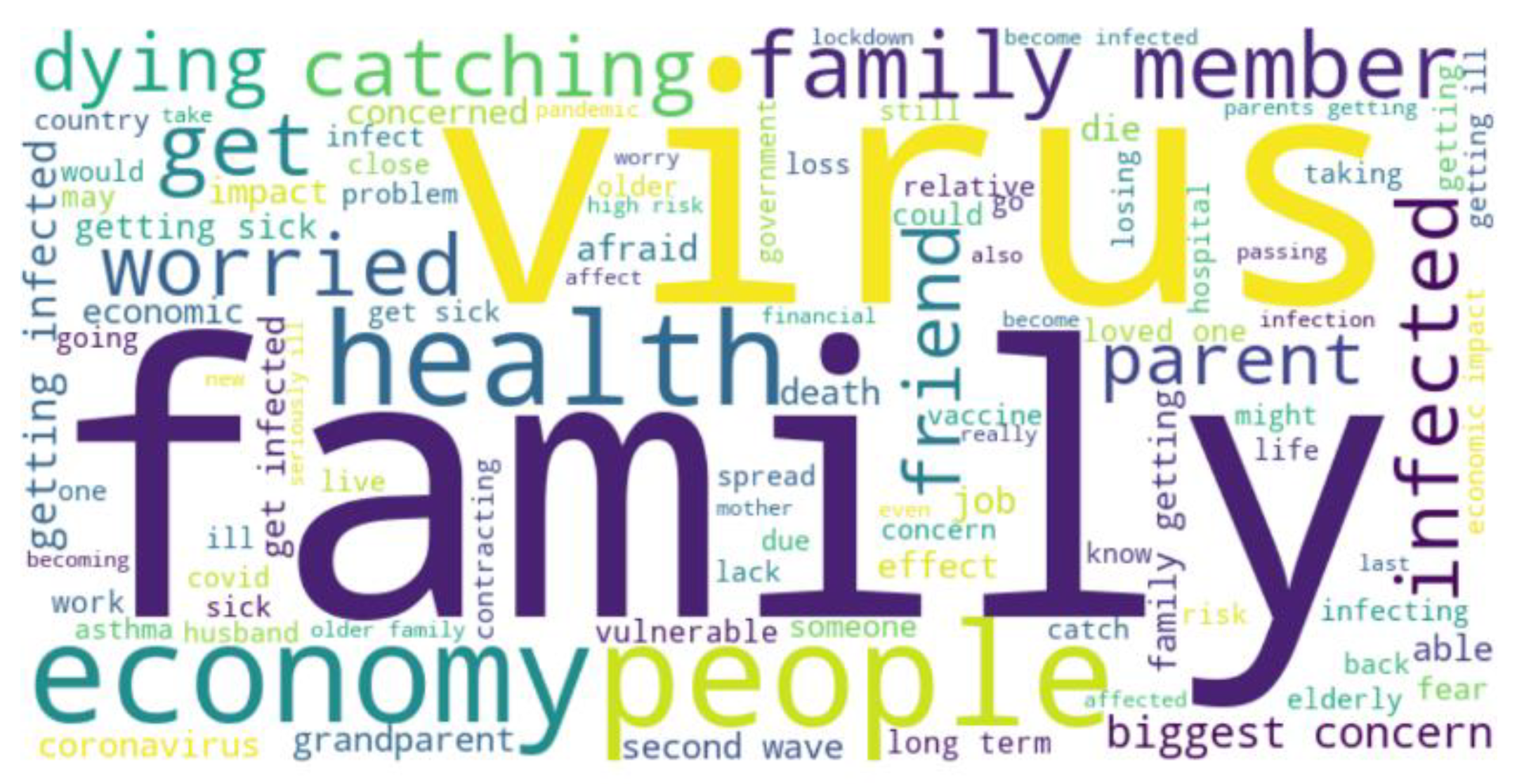
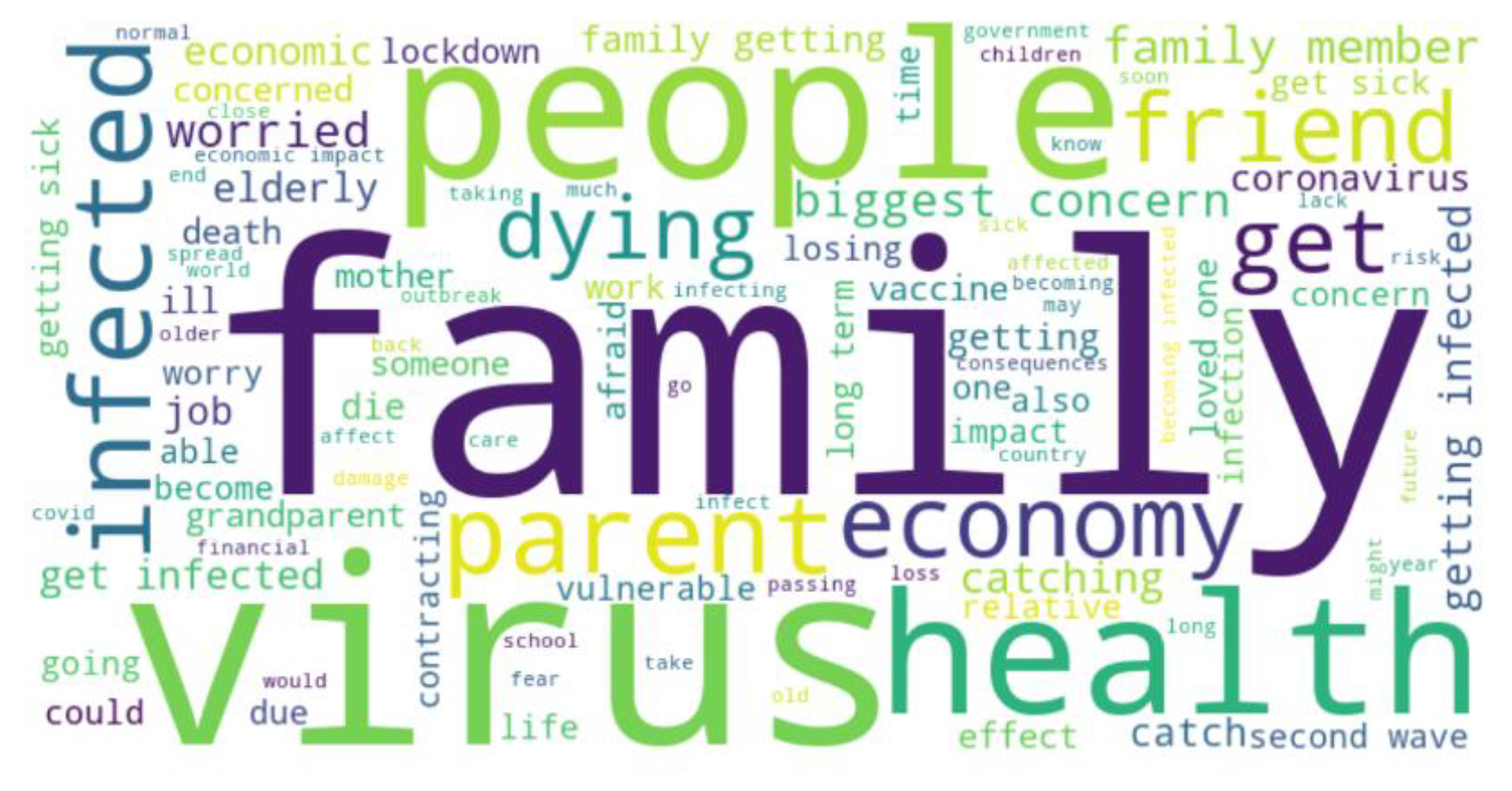
The results from Algorithm 2 are presented next. Algorithm 2 performed word frequency analysis for the responses to the question - “please describe briefly your biggest concern about coronavirus” per month. The results were generated in the form of word clouds and are shown in
Figure 13,
Figure 14,
Figure 15,
Figure 16 and
Figure 17, respectively. The word clouds shown in these figures represent the top 100 frequently used words by individuals of all age groups in their responses to this question. The analysis of
Figure 13,
Figure 14,
Figure 15,
Figure 16 and
Figure 17 reveals novel patterns related to the concerns of the general population from April 2020 to August 2020. For instance, as can be seen from
Figure 13,
Figure 14,
Figure 15,
Figure 16 and
Figure 17, the word “family” consistently featured in the list of 100 frequently used words to represent concerns about COVID-19. This indicates that during this time range one of the biggest concerns of the general population in the context of COVID-19 was their family.
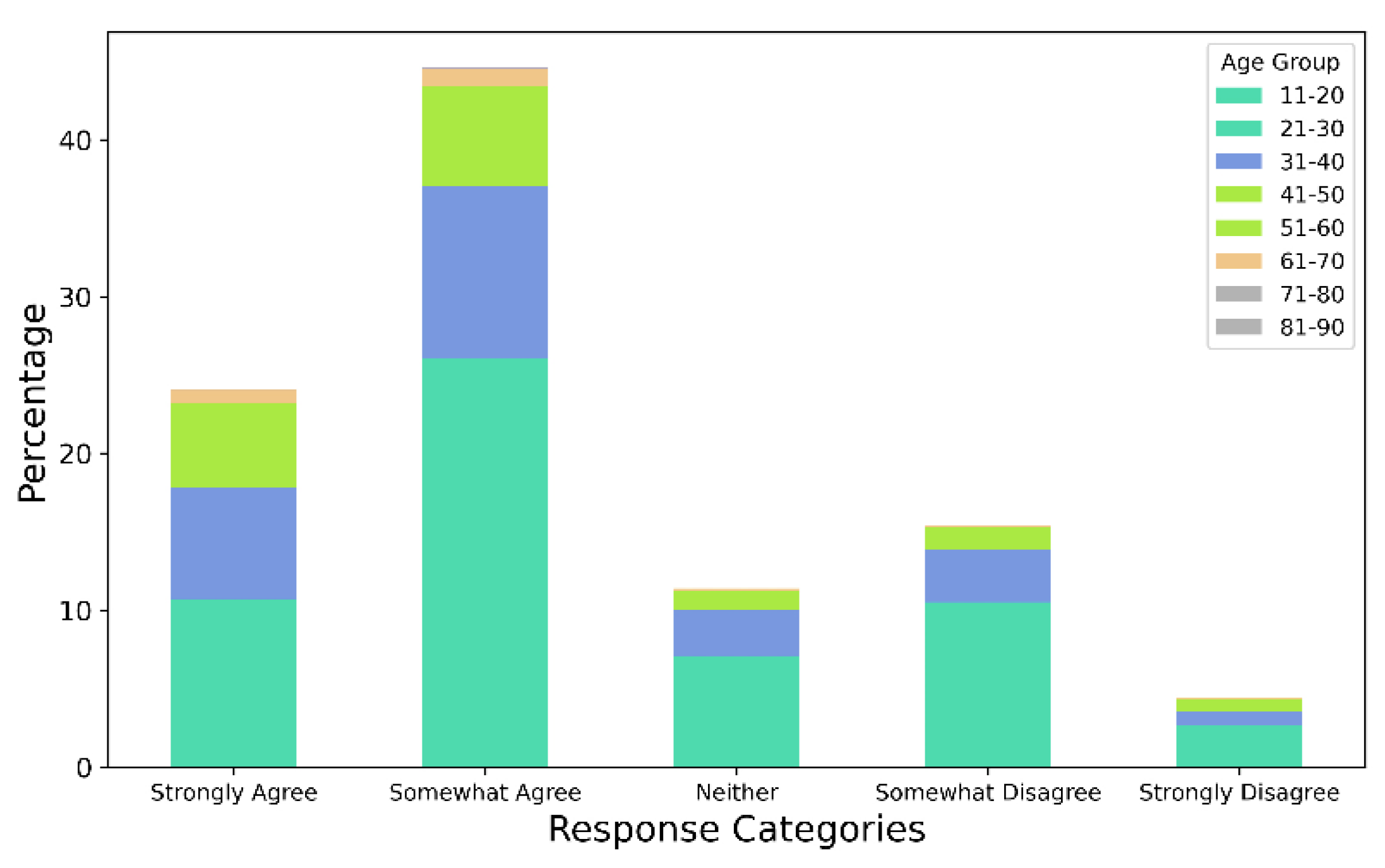
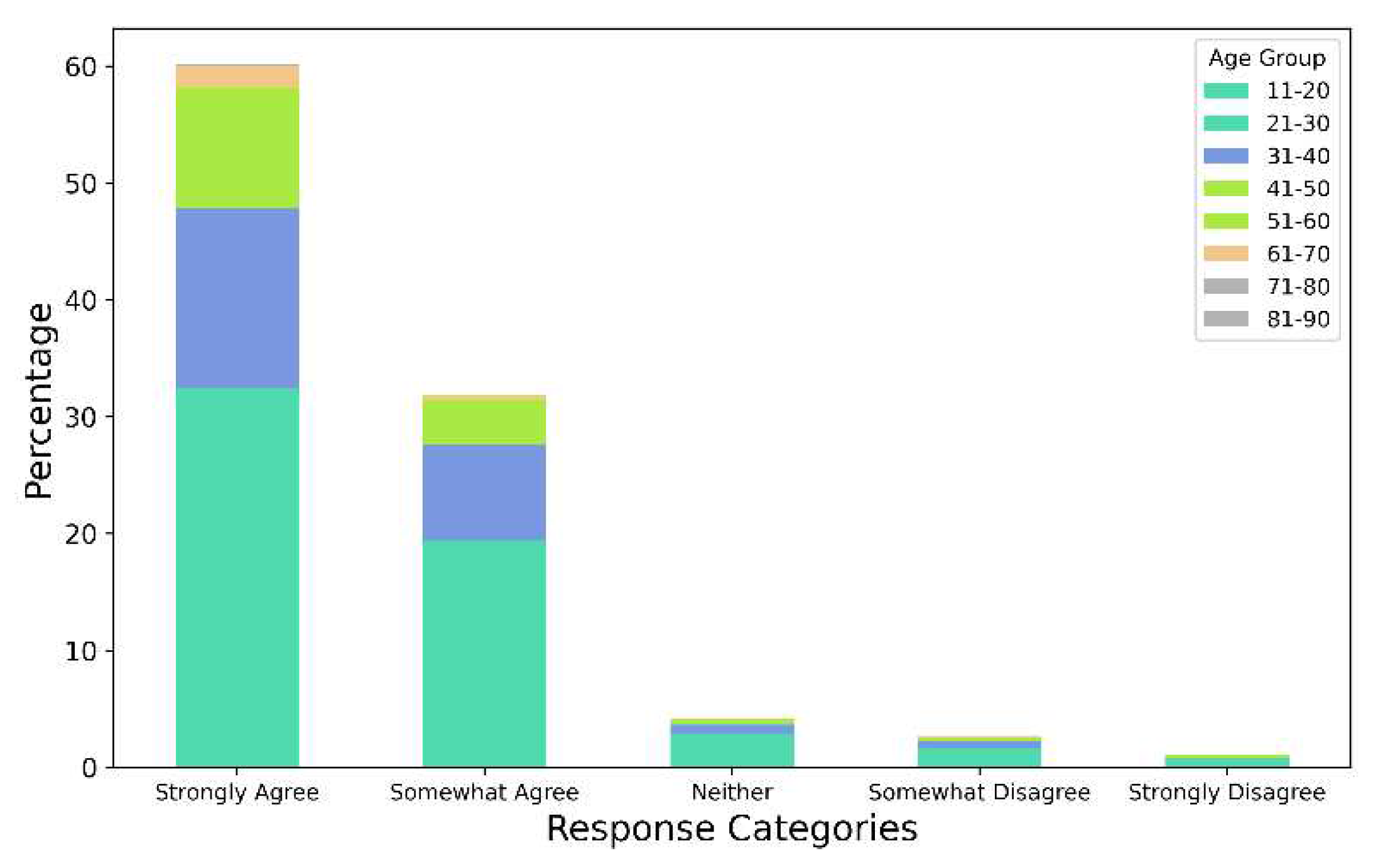
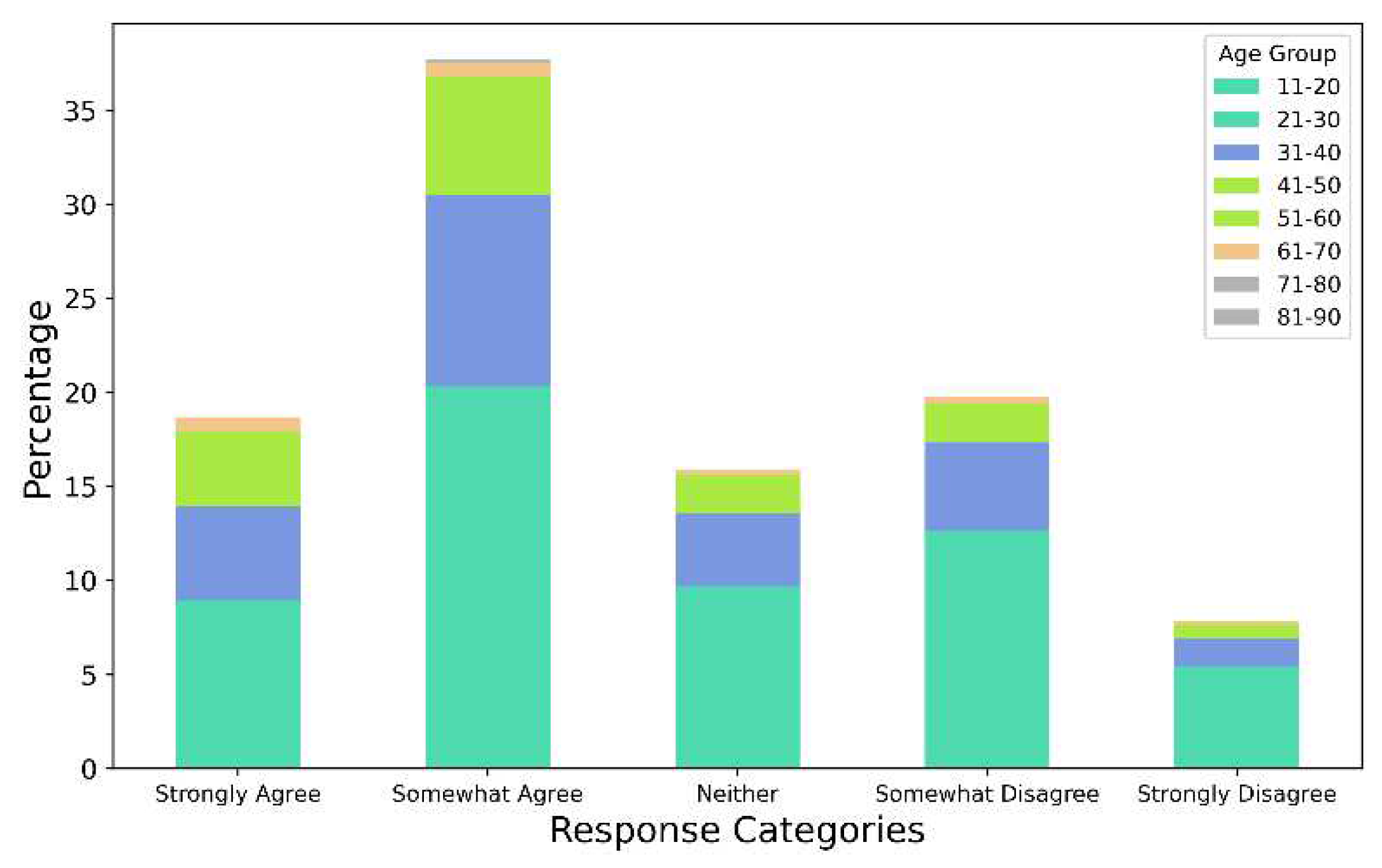
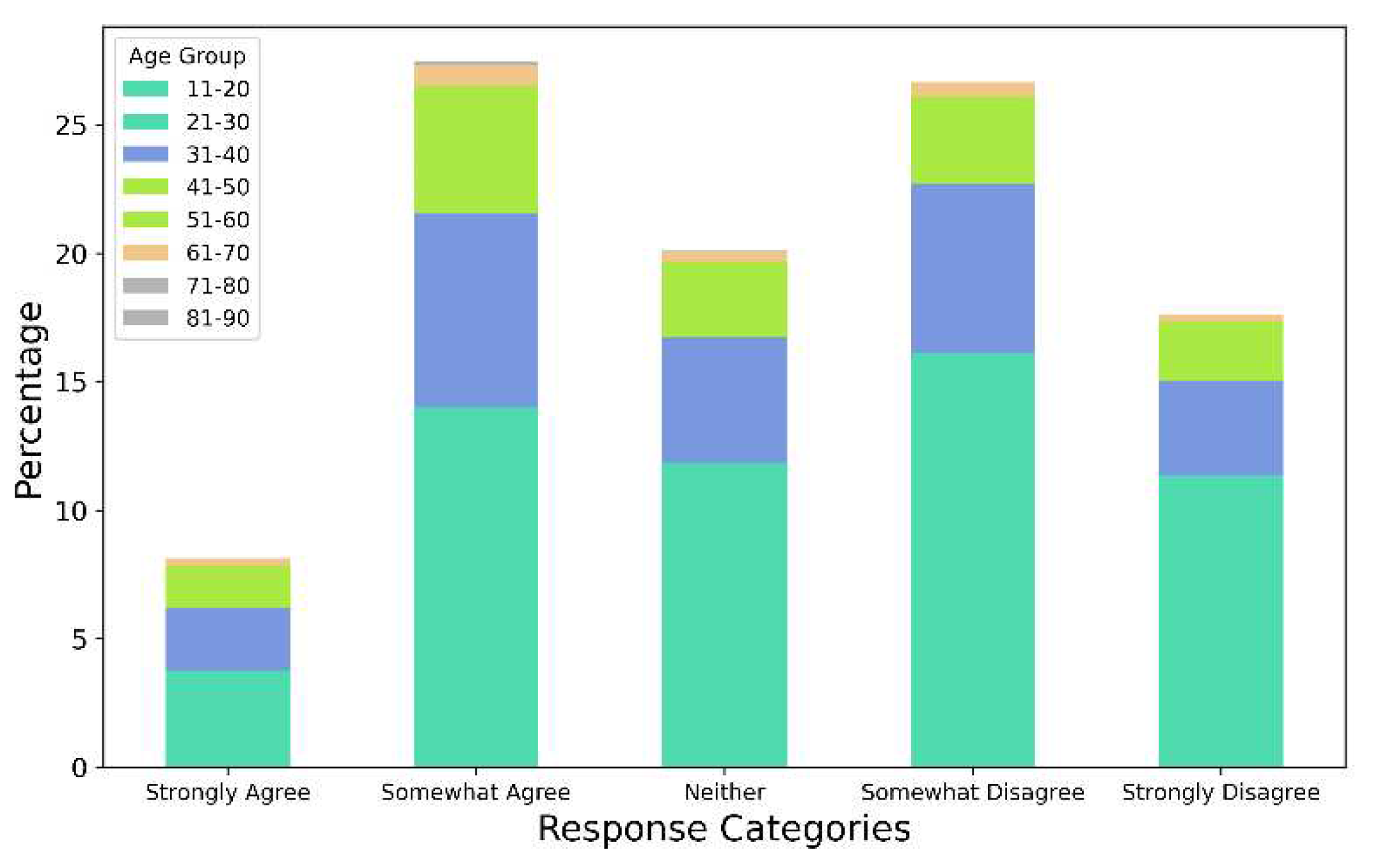
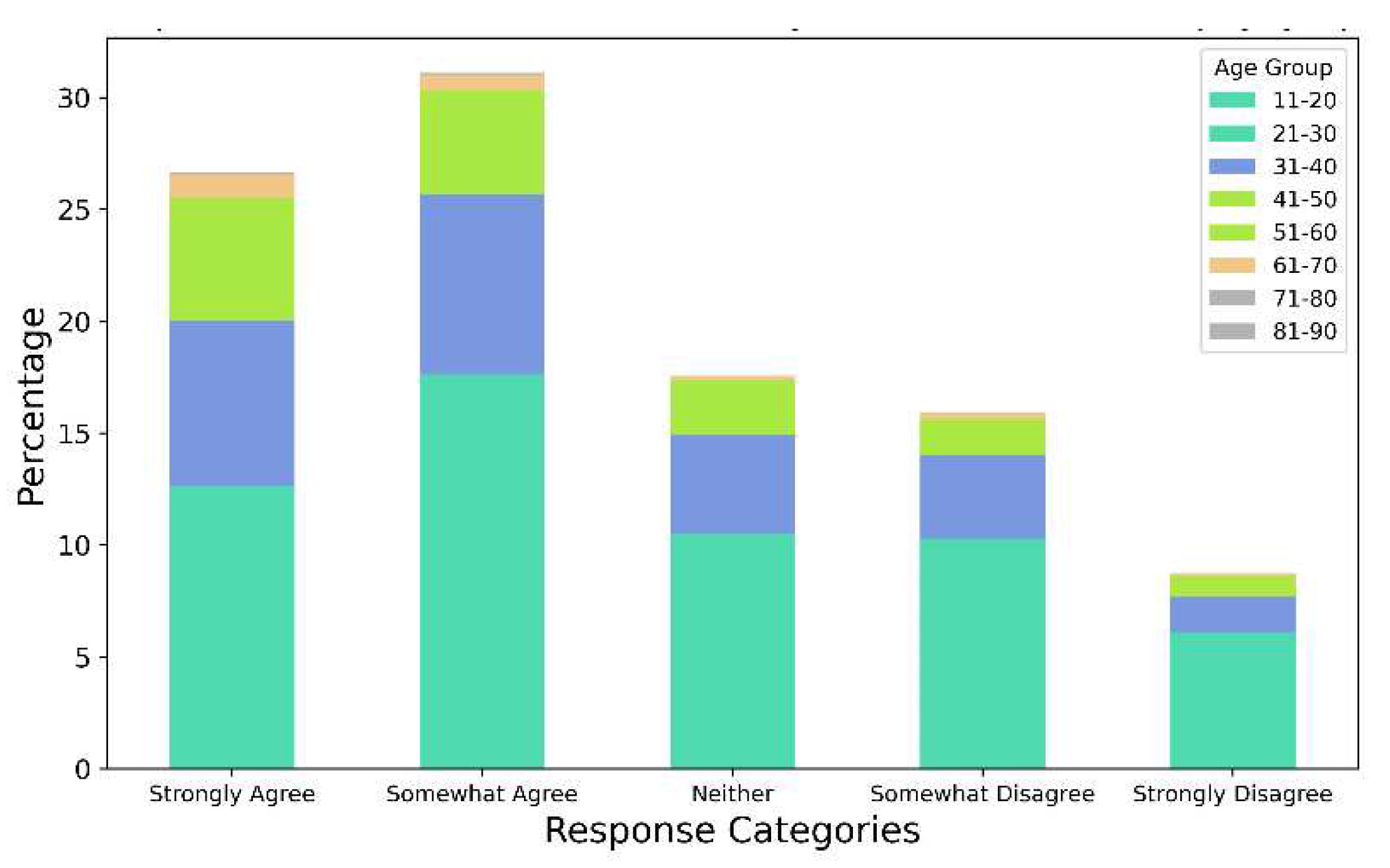
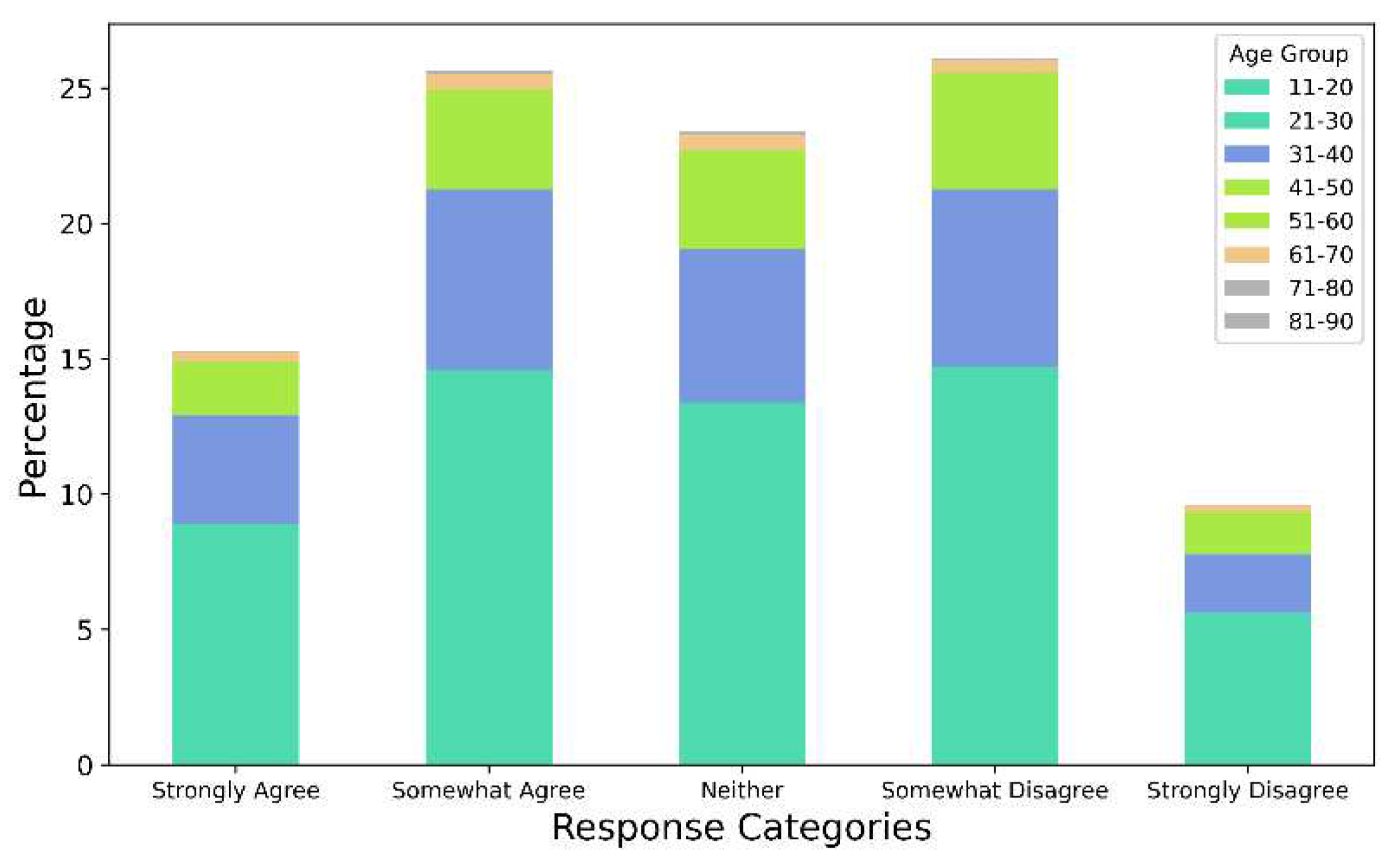
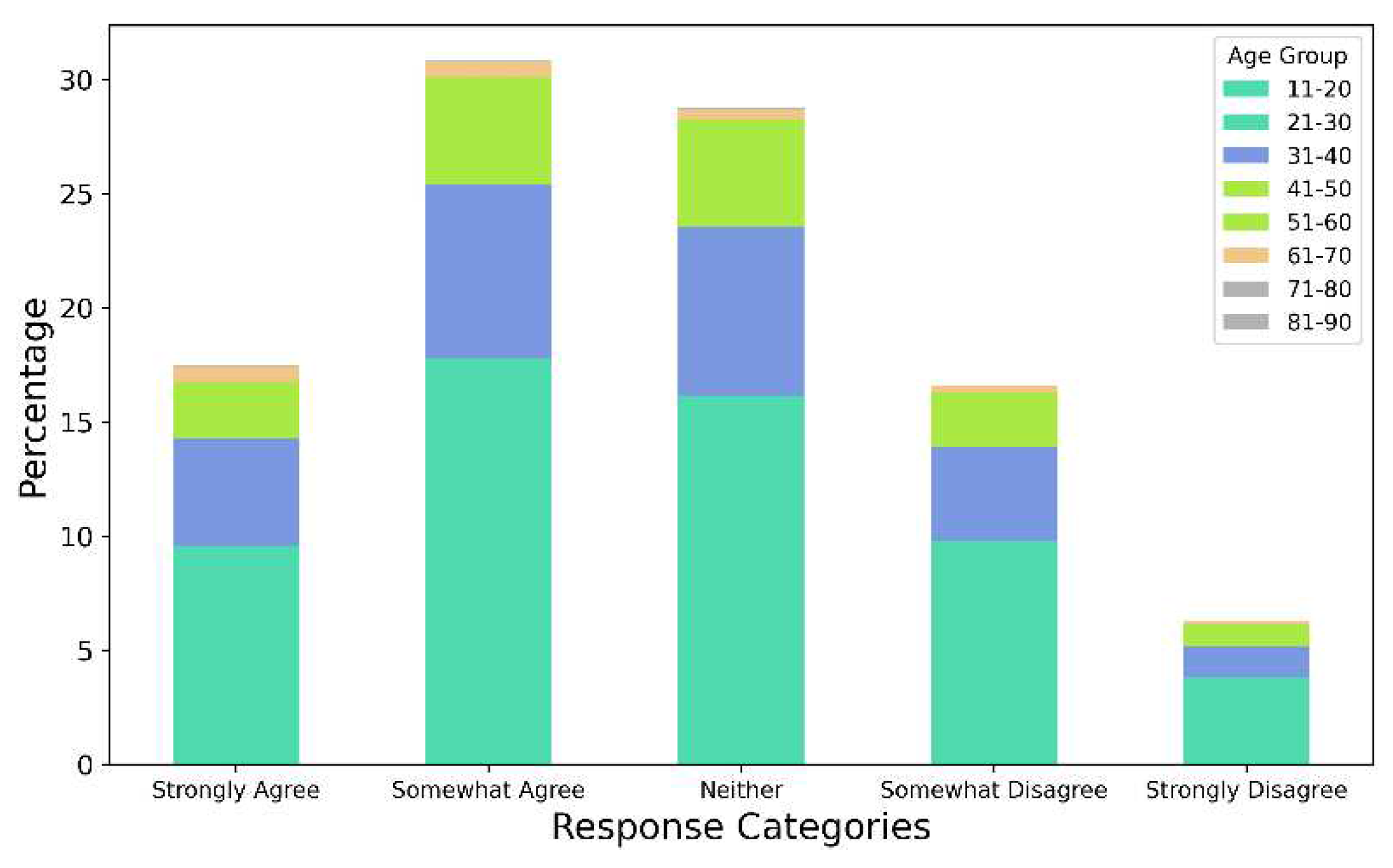
The results of applying Algorithm 3 are presented and discussed next. As discussed in
Section 3, Algorithm 3 computed the responses per age group per question (from Qlist). The questions that comprised Qlist were “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am very worried about the coronavirus outbreak.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am taking precautions to prevent infection (e.g., washing hands, avoiding contact with people, avoiding door handles).”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am constantly following all news updates regarding the virus.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I have stocked up on supplies to prepare for problems related to the coronavirus outbreak.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - for my personal health I find the virus to be much more dangerous than the seasonal flu.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I feel that the health authorities are not doing enough to deal with the virus.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am worried that friends or family will be infected.”, and “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I take more precautions compared to most people to not become infected”. These results are shown in
Figure 18,
Figure 19,
Figure 20,
Figure 21,
Figure 22,
Figure 23 and
Figure 24, respectively.
The results from Algorithm 3 reveal multiple novel insights in the context of fear of COVID-19 in an age-group-specific manner. For instance,
Figure 18 shows that the highest percentage of responses indicating that they were very worried about COVID-19 came from individuals in the age group of 21-30.
Figure 19 shows that in the context of taking precautions to prevent contracting COVID-19, individuals in the age group of 31-40 represented a higher percentage as compared to the percentages of individuals from the age groups of 41-50, 51-60, 61-70, 71-80, and 81-90. In a similar manner, the variations and trends of responses from individuals from different age groups in the context of fear of COVID-19 can be analyzed from
Figure 18,
Figure 19,
Figure 20,
Figure 21,
Figure 22,
Figure 23 and
Figure 24.
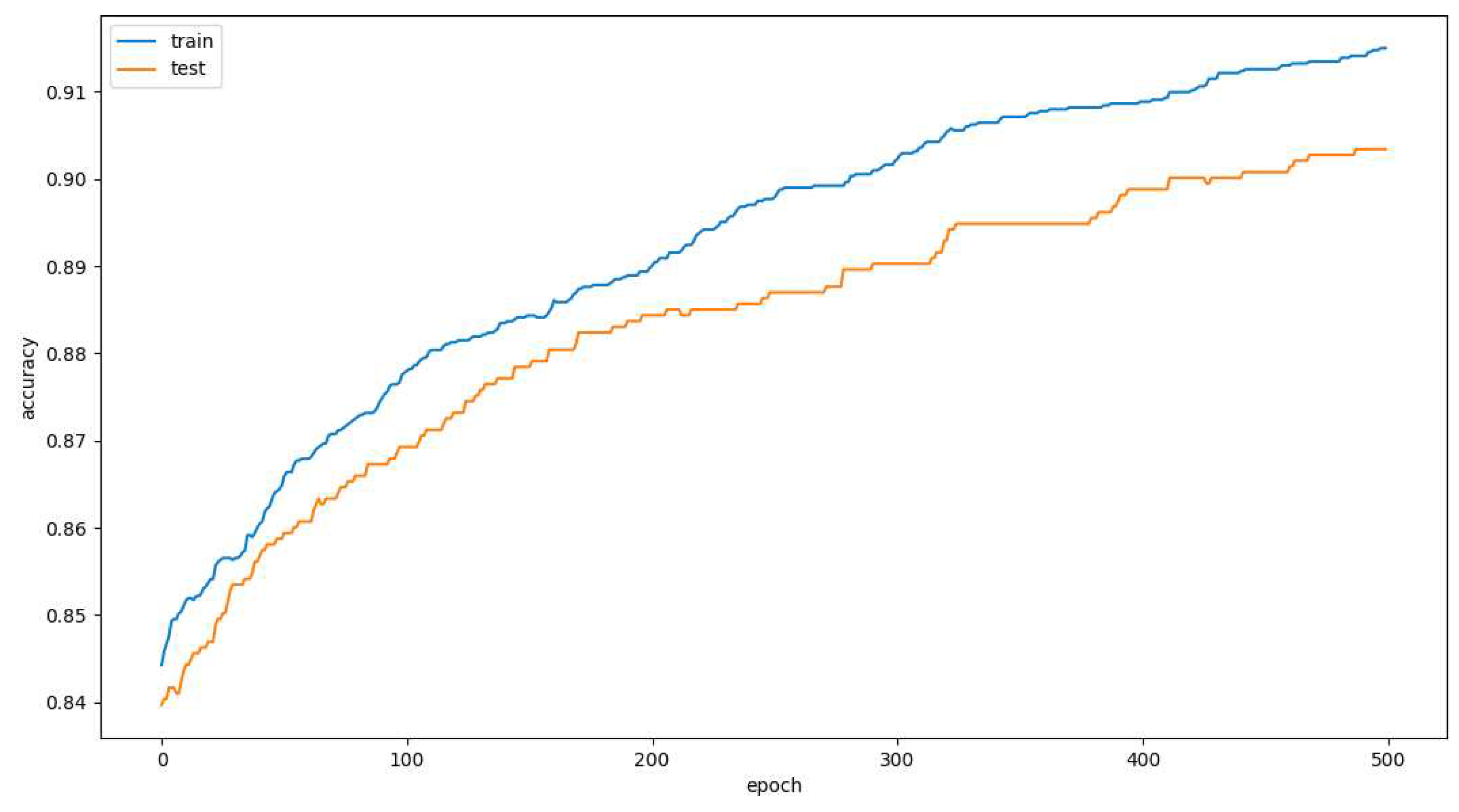
Thereafter, Algorithm 4 was applied to the master dataset. As discussed in
Section 3, Algorithm 4 comprised a deep learning model that was developed to detect the response to the question “are you currently seeing or planning to see a psychologist or psychiatrist for any mental health issues relating to the coronavirus?”. The specific responses that were used to develop this Deep Learning model comprised their responses to the questions “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am very worried about the coronavirus outbreak.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am taking precautions to prevent infection (e.g., washing hands, avoiding contact with people, avoiding door handles).”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am constantly following all news updates regarding the virus.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I have stocked up on supplies to prepare for problems related to the coronavirus outbreak.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - for my personal health I find the virus to be much more dangerous than the seasonal flu.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I feel that the health authorities are not doing enough to deal with the virus.”, “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I am worried that friends or family will be infected.”, and “please select the extent to which the following thoughts, feelings and behaviors apply to you: - I take more precautions compared to most people to not become infected”. This deep learning model was run for 500 epochs and for each epoch the accuracy of the model was computed.
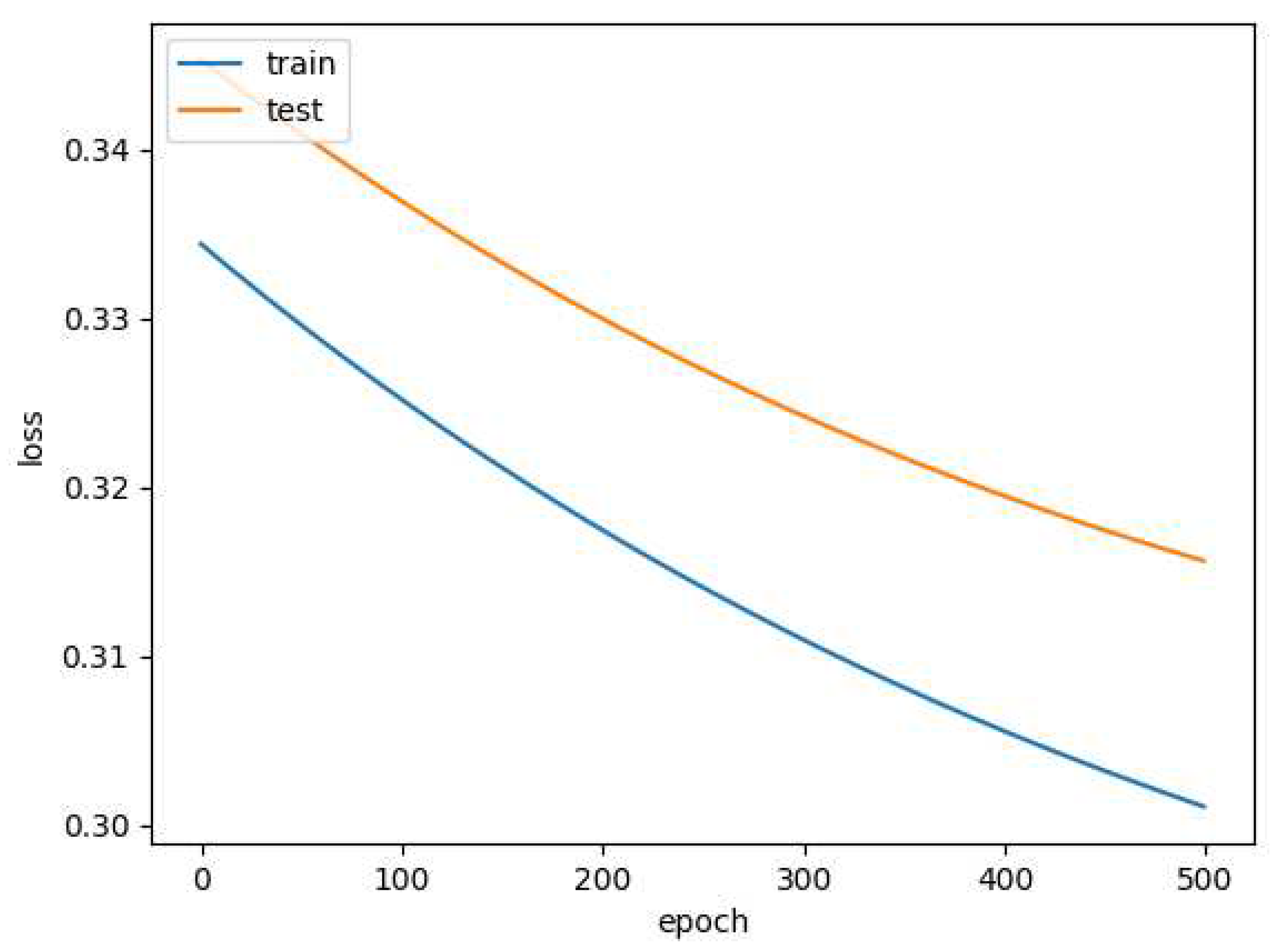
Figure 25 shows the variation in the accuracy of this model per epoch for each of these 500 epochs. This model achieved an overall accuracy of 91.62%. The values of precision and recall were observed to be 0.92 and 0.85. The variation of the loss per epoch was also computed, and
Figure 26 represents the same.
Finally, two comparative studies were conducted to compare this work with prior works in this field. These comparative studies are presented in
Table 1 and
Table 2, respectively.
As can be seen from
Table 1, the work presented in this paper is the first work in this area of research that focuses on machine learning, data analysis, content analysis, and subjectivity analysis related to the investigation of the fear of COVID-19 and the associated response.
Since the initial outbreak, the SARS-CoV-2 mutated multiple times, resulting in cases and deaths in different countries of the world, the likes of which humanity had not witnessed in centuries [
92]. To contain and reduce the spread of the virus, different countries implemented various degrees of lockdown or isolation measures [
93]. The majority of countries implemented different levels of "shelter-in-place" mandates [
94] and about one-third of the world's population experienced some type of quarantine as a result of the COVID-19 pandemic [
95]. There is compelling evidence from several prior works [
96,
97,
98] indicating that experiencing quarantine may have adverse impacts on an individual's psychological well-being, including the development of fear or anxiety towards COVID-19. Furthermore, cultural values are different across different parts of the world [
99]. Prior works have found that some cultural values are associated with death rates [
100], safe-distancing behaviors [
101], and mental resilience [
102] during COVID-19. This highlights the need for a study that investigates the fear of COVID-19 by taking into account the responses of individuals from different countries. The work presented in this paper addresses this research gap as can be seen from
Table 2.
Table 2 further highlights the fact that the number of countries represented in the survey data that were analyzed in this study is considerably higher as compared to prior works in this field. It is worth mentioning here that the works of Albagmi et al. [
51], Roy et al. [
53], Kalita et al. [
54], and Khalaf et al. [
69] did not provide information related to the specific countries or number of countries represented in the data that they analyzed. So, these works were not included in the second comparative study shown in
Table 2.
The work presented in this paper has a limitation. The results presented in this work are based on the analysis of the data available in the dataset developed by Mertens et al. [
76] where the survey respondents were from 40 countries. So, the results presented in this study reflect the views, perspectives, and opinions in the context of fear of COVID-19 and the associated response from individuals in those countries. It is possible that if a comprehensive data collection is performed to include participants from every country and the methodology described in this paper is applied to that dataset the results obtained may differ from the results presented in
Section 4 of this paper on account of user diversity and the variations in global preparedness and response towards COVID-19. At the time of writing this paper, there wasn’t any data set available comprising the data of participants from every country of the world in the context of fear of COVID-19 and the associated response. So, this limitation could not be addressed in this study.
5. Conclusions
Since the beginning of the COVID-19 pandemic, the fear associated with the same has had several effects on the global population including but not limited to mental health problems, such as fear of illness, stress, anxiety disorders, sleep problems, mood disorders, and suicidal thoughts. Even though there have been multiple works conducted related to the investigation and analysis of the fear of COVID-19 in the last couple of years or so, those works have multiple limitations. First, prior works in this field have focused on investigating the fear and response towards COVID-19 by taking into account survey responses primarily from one country. The rate of COVID-19 cases, the varying nature of lockdown or isolation measures, and diverse cultures in different countries highlight the need for a study in this area of research that investigates the fear of COVID-19 by taking into account the responses of individuals from different countries. Second, most of the studies in this field have focused only on the data analysis or content analysis of survey responses and did not apply any approaches such as subjectivity analysis to understand the degrees of personal opinions and facts represented in the survey responses. Third, even though there have been multiple studies where machine learning algorithms were used, none of those works focused on the development of a machine learning or deep learning model that could detect if a person was receiving mental health-related help based on their responses to surveys in the context of fear of COVID-19.
The work presented in this paper addresses these limitations by performing a comprehensive analysis of a dataset of survey responses related to the fear of COVID-19, where the dataset comprised responses from participants from 40 countries. First, the results of subjectivity analysis regarding the biggest concern about COVID-19 showed that the average subjectivity in responses by the age group of 41-50 decreased from April 2020 to June 2020, the average subjectivity in responses by the age group of 71-80 drastically increased from May 2020, and the age group of 11-20 indicated the least level of subjectivity in their responses between June 2020 to August 2020. Second, subjectivity analysis also revealed the percentage of highly opinionated, neutral opinionated, and least opinionated responses per age group. For example, the percentage of highly opinionated, neutral opinionated, and least opinionated responses by the age group of 11-20 were 17.92%, 16.24%, and 65.84%, respectively. A similar distribution was observed for the age groups of 21-30 and 31-40 as well. Comparison of these distributions also revealed novel patterns related to the responses provided by different age groups. For instance, the age group of 71-80 posted the highest percentage of highly opinionated responses and the age group of 31-40 posted the highest percentage of neutral opinionated responses. Third, data analysis of the survey responses showed that the percentage of responses indicating that they were very worried about COVID-19 came from individuals in the age group of 21-30. Furthermore, the findings of data analysis also revealed that in the context of taking precautions to prevent contracting COVID-19, individuals in the age group of 31-40 represented a higher percentage as compared to the percentages of individuals from the age groups of 41-50, 51-60, 61-70, 71-80, and 81-90. Fourth, a deep learning model was developed to detect if an individual was currently seeing or planning to see a psychologist or psychiatrist for any mental health issues related to COVID-19. The deep learning model used the responses for multiple questions related to fear of COVID-19 and achieved an overall accuracy of 91.62% after 500 epochs. Finally, two comparative studies in terms of focus areas of investigation and the number of countries represented in the analyzed data are presented in this paper to highlight the novelty and scientific contributions of the same.
As per the best knowledge of the authors, no similar work has been conducted in this field thus far. Future work in this area would involve performing sentiment analysis of the survey responses from this dataset to interpret and analyze the similarities, variations, and trends of sentiments represented in the survey responses in an age-group-specific and country-specific manner.
Author Contributions
Conceptualization, N.T.; methodology, N.T., K.A.P., A.P. and R.S.; software, N.T., K.A.P., A.P. and R.S.; validation, N.T., K.A.P., A.P. and R.S.; formal analysis, N.T., K.A.P., A.P., R.S., N.A. and C.H.; investigation, N.T., K.A.P., A.P., R.S., N.A. and C.H.; resources, N.T., K.A.P., A.P. and R.S.; data curation, N.T., K.A.P., A.P. and R.S.; writing—original draft preparation, N.T., C.H., N.A., K.A.P., A.P. and R.S.; writing—review and editing, N.T.; visualization, N.T., K.A.P., A.P. and R.S.; supervision, N.T.; project administration, N.T.; funding acquisition, not applicable. All authors have read and agreed to the published version of the manuscript.
Figure 1.
A flowchart that demonstrates the methodology followed for the development of the master dataset for analysis.
Figure 1.
A flowchart that demonstrates the methodology followed for the development of the master dataset for analysis.
Figure 2.
Representation of the step-by-step working of Algorithm 1, Algorithm 2, and Algorithm 3 on the master dataset.
Figure 2.
Representation of the step-by-step working of Algorithm 1, Algorithm 2, and Algorithm 3 on the master dataset.
Figure 3.
Representation of the step-by-step working of Algorithm 4 on the master dataset.
Figure 3.
Representation of the step-by-step working of Algorithm 4 on the master dataset.
Figure 4.
Representation of average subjectivity per age group per month.
Figure 4.
Representation of average subjectivity per age group per month.
Figure 5.
Results of subjectivity analysis of the responses for the age group of 11-20.
Figure 5.
Results of subjectivity analysis of the responses for the age group of 11-20.
Figure 6.
Results of subjectivity analysis of the responses for the age group of 21-30.
Figure 6.
Results of subjectivity analysis of the responses for the age group of 21-30.
Figure 7.
Results of subjectivity analysis of the responses for the age group of 31-40.
Figure 7.
Results of subjectivity analysis of the responses for the age group of 31-40.
Figure 8.
Results of subjectivity analysis of the responses for the age group of 41-50.
Figure 8.
Results of subjectivity analysis of the responses for the age group of 41-50.
Figure 9.
Results of subjectivity analysis of the responses for the age group of 51-60.
Figure 9.
Results of subjectivity analysis of the responses for the age group of 51-60.
Figure 10.
Results of subjectivity analysis of the responses for the age group of 61-70.
Figure 10.
Results of subjectivity analysis of the responses for the age group of 61-70.
Figure 11.
Results of subjectivity analysis of the responses for the age group of 71-80.
Figure 11.
Results of subjectivity analysis of the responses for the age group of 71-80.
Figure 12.
Results of subjectivity analysis of the responses for the age group of 81-90.
Figure 12.
Results of subjectivity analysis of the responses for the age group of 81-90.
Figure 13.
Word Cloud-based Analysis of the biggest concerns about COVID-19 from April 2020.
Figure 13.
Word Cloud-based Analysis of the biggest concerns about COVID-19 from April 2020.
Figure 14.
Word Cloud-based Analysis of the biggest concerns about COVID-19 from May 2020.
Figure 14.
Word Cloud-based Analysis of the biggest concerns about COVID-19 from May 2020.
Figure 15.
Word Cloud-based Analysis of the biggest concerns about COVID-19 from June 2020.
Figure 15.
Word Cloud-based Analysis of the biggest concerns about COVID-19 from June 2020.
Figure 16.
Word Cloud-based Analysis of the biggest concerns about COVID-19 from July 2020.
Figure 16.
Word Cloud-based Analysis of the biggest concerns about COVID-19 from July 2020.
Figure 17.
Word Cloud-based Analysis of the biggest concerns about COVID-19 from August 2020.
Figure 17.
Word Cloud-based Analysis of the biggest concerns about COVID-19 from August 2020.
Figure 18.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am very worried about the coronavirus outbreak.”.
Figure 18.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am very worried about the coronavirus outbreak.”.
Figure 19.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am taking precautions to prevent infection (e.g., washing hands, avoiding contact with people, avoiding door handles)”.
Figure 19.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am taking precautions to prevent infection (e.g., washing hands, avoiding contact with people, avoiding door handles)”.
Figure 20.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am constantly following all news updates regarding the virus.”.
Figure 20.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am constantly following all news updates regarding the virus.”.
Figure 21.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I have stocked up on supplies to prepare for problems related to the coronavirus outbreak”.
Figure 21.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I have stocked up on supplies to prepare for problems related to the coronavirus outbreak”.
Figure 22.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - for my personal health I find the virus to be much more dangerous than the seasonal flu.”.
Figure 22.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - for my personal health I find the virus to be much more dangerous than the seasonal flu.”.
Figure 23.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am worried that friends or family will be infected.”.
Figure 23.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I am worried that friends or family will be infected.”.
Figure 24.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I take more precautions compared to most people to not become infected.”.
Figure 24.
Percentage of responses per age group for the question - “please select the extent to which the following thoughts, feelings, and behaviors apply to you: - I take more precautions compared to most people to not become infected.”.
Figure 25.
Representation of the accuracy of the model from Algorithm 4 per epoch (number of epochs = 500).
Figure 25.
Representation of the accuracy of the model from Algorithm 4 per epoch (number of epochs = 500).
Figure 26.
Representation of the loss of the model from Algorithm 4 per epoch (number of epochs = 500).
Figure 26.
Representation of the loss of the model from Algorithm 4 per epoch (number of epochs = 500).
Table 1.
Comparative Study of this work with prior works in this field based on the focus areas of investigation.
Table 1.
Comparative Study of this work with prior works in this field based on the focus areas of investigation.
| Work |
Focus Areas of the Works |
| |
Machine Learning or Applications of Machine Learning |
Data Analysis or Content analysis |
Subjectivity Analysis |
| Elhai et al. [49] |
√ |
|
|
| Eder et al. [50] |
√ |
|
|
| Albagmi et al. [51] |
√ |
|
|
| Feng et al. [52] |
√ |
|
|
| Roy et al. [53] |
√ |
|
|
| Kalita et al. [54] |
√ |
|
|
| Fitzpatrick et al. [55] |
|
√ |
|
| Mistry et al. [56] |
|
√ |
|
| Avazzadeh et al. [57] |
|
√ |
|
| Demirbas et al. [58] |
|
√ |
|
| Suhail et al. [59] |
|
√ |
|
| Chair et al. [60] |
|
√ |
|
| Elhessewi et al. [61] |
|
√ |
|
| Ambelu et al. [62] |
|
√ |
|
| Traunmüller et al. [63] |
|
√ |
|
| Lee et al. [64] |
|
√ |
|
| Verma et al. [65] |
|
√ |
|
| Villani et al. [66] |
|
√ |
|
| Fodjo et al. [67] |
|
√ |
|
| Sakib et al. [68] |
|
√ |
|
| Khalaf et al. [69] |
|
√ |
|
| Kabasakal et al. [70] |
|
√ |
|
| Malik et al. [71] |
|
√ |
|
| Jue et al. [72] |
|
|
√ |
| Satici et al. [73] |
|
|
√ |
| Blasco et al. [74] |
|
|
√ |
| Gritzka et al. [75] |
|
|
√ |
Thakur et al.
[this work] |
√ |
√ |
√ |
Table 2.
Comparative Study of this work with prior works in this field based on the number of countries that were represented in the survey data which was studied or analyzed.
Table 2.
Comparative Study of this work with prior works in this field based on the number of countries that were represented in the survey data which was studied or analyzed.
| Work |
Information about the Represented Countries in the Survey Data |
| |
Names of Countries |
Number of Countries |
| Elhai et al. [49] |
China |
1 |
| Feng et al. [52] |
China |
1 |
| Fitzpatrick et al. [55] |
United States |
1 |
| Mistry et al. [56] |
Bangladesh |
1 |
| Avazzadeh et al. [57] |
Iran |
1 |
| Demirbas et al. [58] |
Turkey |
1 |
| Suhail et al. [59] |
India |
1 |
| Chair et al. [60] |
Hong Kong |
1 |
| Elhessewi et al. [61] |
Saudi Arabia |
1 |
| Ambelu et al. [62] |
Ethiopia |
1 |
| Traunmüller et al. [63] |
Austria |
1 |
| Lee et al. [64] |
United States |
1 |
| Verma et al. [65] |
India |
1 |
| Villani et al. [66] |
Italy |
1 |
| Fodjo et al. [67] |
Cameroon |
1 |
| Sakib et al. [68] |
Bangladesh |
1 |
| Kabasakal et al. [70] |
Turkey |
1 |
| Malik et al. [71] |
Pakistan |
1 |
| Jue et al. [72] |
Korea |
1 |
| Satici et al. [73] |
Turkey |
1 |
| Blasco et al. [74] |
Spain |
1 |
| Gritzka et al. [75] |
Germany |
1 |
| Eder et al. [50] |
Austria, Spain, Poland, and Czech Republic |
4 |
Thakur et al.
[this work] |
Australia, Austria, Belgium, Canada, Chile, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hong Kong (S.A.R.), Hungary, India, Ireland, Israel, Italy, Japan, Latvia, Mexico, Netherlands, New Zealand, Norway, Peru, Poland, Portugal, Romania, Russian Federation, Slovenia, South Africa, South Korea, Spain, Sweden, Switzerland, Turkey, United Arab Emirates, United Kingdom, and USA |
40 |