1. Introduction
In today’s digitalized world, having optimal visual performance is increasingly important for a modern lifestyle. As the aging population continues to undergo cataract surgeries, patients have higher expectations of satisfactory outcomes that allow them to have clear vision without obstacles, particularly when using digital devices [
1]. Among the options available for intraocular lenses (IOLs) in cataract surgery, multifocal intraocular lenses (MF-IOLs) have become increasingly popular. Initially approved by the US Food and Drug Administration in 1977, MF-IOLs required careful selection to meet each patient’s specific needs [
2]. Early-generation MF-IOLs were designed to provide clear vision both at around 4 meters and for near vision, suitable for reading printed material at approximately 30-40cm. However, with the evolving reading habits that involve the use of computers, smartphones, and tablets, the demands on MF-IOLs have changed [
1,
3]. These lenses have now been developed to diffract light and focus at different depths, resulting in varying levels of visual acuity at different distances [
4].
Cataract surgery with MF-IOL implantation is a common approach to addressing presbyopia and has shown promising outcomes. Although Snellen and Logarithm of the Minimum Angle of Resolution (LogMAR) acuity charts are widely used to assess visual results, they do not fully capture the demands of modern digital life. Fortunately, the MNREAD acuity chart (University of Minnesota) provides a comprehensive evaluation of visual performance on mobile devices [
5,
6]. This chart measures maximum reading speed (MRS), reading acuity (RA), reading accessibility index (ACC), and critical print size (CPS). The CPS represents the threshold print size at which reading speed significantly decreases, typically twice the size of the letters used for acuity measurement. In simpler terms, it can be considered as the comfortable print size for reading [
7,
8]. Studies comparing reading experiences on paper versus digital screens have shown that digital reading, which emits more light, can lead to increased visual fatigue. On the other hand, paper reading involves additional sensory aspects such as tactile sensations and physical interaction with the pages [
9,
10]. Therefore, digital reading may better reflect daily visual performance and patient satisfaction in the modern era.
Previous studies have demonstrated positive outcomes in patients who received bilateral implantation of non-toric diffractive MF-IOLs. These patients achieved favorable visual acuity at all distances, with a focus on uncorrected and intermediate visual acuity. Patient satisfaction was also high and spectacle dependence decreased following surgery [
11,
12]. These findings were further supported by larger studies, including Asian patients, which emphasized high satisfaction and reduced dependence on spectacles [
13,
14]. Furthermore, some studies explored a different approach by implanting different types of intraocular lenses in each eye, with diffractive MF-IOLs being one of the options [
15,
16]. However, none of these studies incorporated measurements on digital devices to assess visual outcomes in patients with bilaterally implanted diffractive MF-IOLs, regardless of whether they were toric or non-toric.
In our study, our aim was to evaluate the digital reading performance of patients who underwent bilateral implantation of AcrySof IQ PanOptix (Alcon Laboratories Inc., Fort Worth, Texas, USA) diffractive MF-IOL. We investigated the differences between digital reading and traditional paper reading, considering factors such as screen illumination, display polarity, glance-like reading, and the potential impact of digital eye strain. Our hypothesis was that reading on a digital screen, influenced by factors such as pupil constriction and improved visual acuity, would differ from reading on paper under the same lighting conditions5. Furthermore, we sought to determine the optimized CPS and reading speed and provide recommendations on display polarity for patients with MF-IOLs. By incorporating digital device measurements, our aim was to improve our understanding of visual outcomes in patients with bilateral diffractive MF-IOL and provide valuable insights for clinical practice.
2. Materials and Methods
This prospective, non-randomized, interventional case series obtained approval from the institutional review board (IRB #765/63) of the Faculty of Medicine, Chulalongkorn University and adhered to the principles outlined in the Declaration of Helsinki. The study recruited patients from the outpatient department of King Chulalongkorn Memorial Hospital. Before surgery, patients gave written informed consent and underwent various assessments, including tonometry (Nidek NT-530P), auto kerato-refractometer (Topcon KR800), and optical biometry (Zeiss IOLMaster700) on the same day. The surgeon (TS) conducted preoperative investigations, data collection and analysis, and made decisions regarding toric IOLs. Only the surgeon (TS) selected and implanted the diffractive MF-IOLs used in this study. Bilateral cataract surgery using the phacoemulsification technique was performed on the same day by the surgeon (TS). Intraoperative and postoperative complications were monitored, along with intraocular pressure measurements, for safety assessment. Patients underwent examinations on the day of surgery and at one day, one week, one month, and three months postoperatively, with additional examinations scheduled as needed. All procedures were performed at King Chulalongkorn Memorial Hospital between January 31 to October 31, 2021.
To be eligible for inclusion, the patients had to be 40 years or older, with or without corneal astigmatism that could be corrected using diffractive MF-IOL in both eyes. They also needed to use electronic devices, such as smartphones, daily and have proficiency in reading and understanding English. Exclusion criteria included prior refractive eye surgery and the presence of underlying diseases such as retinal disease, glaucoma, corneal disease, zonular weakness, or dehiscence that could potentially affect postoperative visual outcomes. Patients with intraoperative complications were also excluded from the study.
IOL calculations were performed using the Barrett Universal II formula (APACRS.org) and Barrett Toric Calculator (APACRS.org). The implanted IOLs in both eyes were AcrySof IQ PanOptix or AcrySof IQ PanOptix Toric, which are single-piece, aspheric, non-apodised diffractive trifocal IOLs. The alignment of the IOL axis was guided using the VERION image-guided system (Alcon Laboratories Inc., Fort Worth, Texas, United States) digital marker guiding system.
2.1. Data Collection
The recorded data included demographic information, frequency, and duration of daily use of digital devices, underlying diseases, and preoperative eye conditions such as lens status, refraction, intraocular pressure, keratometry, optical biometry, and surgical details. Efficacy measures included binocular uncorrected visual acuity measured using the LogMAR acuity chart and the MNREAD application on an iPad device (Apple Inc., Cupertino, California, USA) at different distances: 4 m (Uncorrected and corrected distance visual acuity; UCVA, CDVA), 60 cm (Uncorrected and distance-corrected intermediate visual acuity; UIVA, DCIVA), and 40 cm (Uncorrected and distance-corrected near visual acuity; UNVA, DCNVA) reported in LogMAR units. The reading acuity of the MNREAD application was measured only at 60 cm and 40 cm. The binocular uncorrected defocus curve was obtained from -4.00 D to +1.00 D in 0.5 D steps with the LogMAR chart at 4 meters under photopic light conditions. Postoperative manifest refraction at 3 months of follow-up was also recorded, including the spherical equivalent (SEQ) within ± 0.25 D, ± 0.50 D and ± 1.00 D of emmetropia, and the manifest cylinder. Reading acuity with positive display polarity (black on white background, BoW) and negative display polarity (white on black background, WoB) using a font size of 7 points or greater was measured at 40 cm and 60 cm one month and three months postoperatively. The mean digital CPS in logMAR unit and the mean reading speed (words per minute, WPM) with negative display polarity were collected one month and three months after surgery at 40 cm.
2.2. Statistical analysis
All data was collected using Microsoft Excel (Microsoft Inc, Redmond, Washington, USA). Statistical analysis was performed with STATA MP 16.0 (StataCorp LLC, College Station, Texas, USA). Visual acuity and reading acuity in logMAR were analyzed and presented as mean values with corresponding standard deviations (SD).
3. Results
3.1. Demographic Data
A total of 26 patients, corresponding to 52 eyes, underwent bilateral implantation of MF-IOL or Toric MF-IOL on the same day. The average age of the patients was 61.69 ± 5.96 years (mean ± SD). The distribution of IOL types used in the study was as follows: MF-IOL (48%) and Toric MF-IOL (52%). A detailed breakdown of the IOL types can be found in
Table 1.
3.2. Visual Acuity Using LogMAR Acuity Chart
Table 2 presents monocular and binocular UCVA, CDVA, UIVA, DCIVA, UNVA and DCNVA measured at 1 week, 1 month, and 3 months using the conventional LogMAR acuity chart.
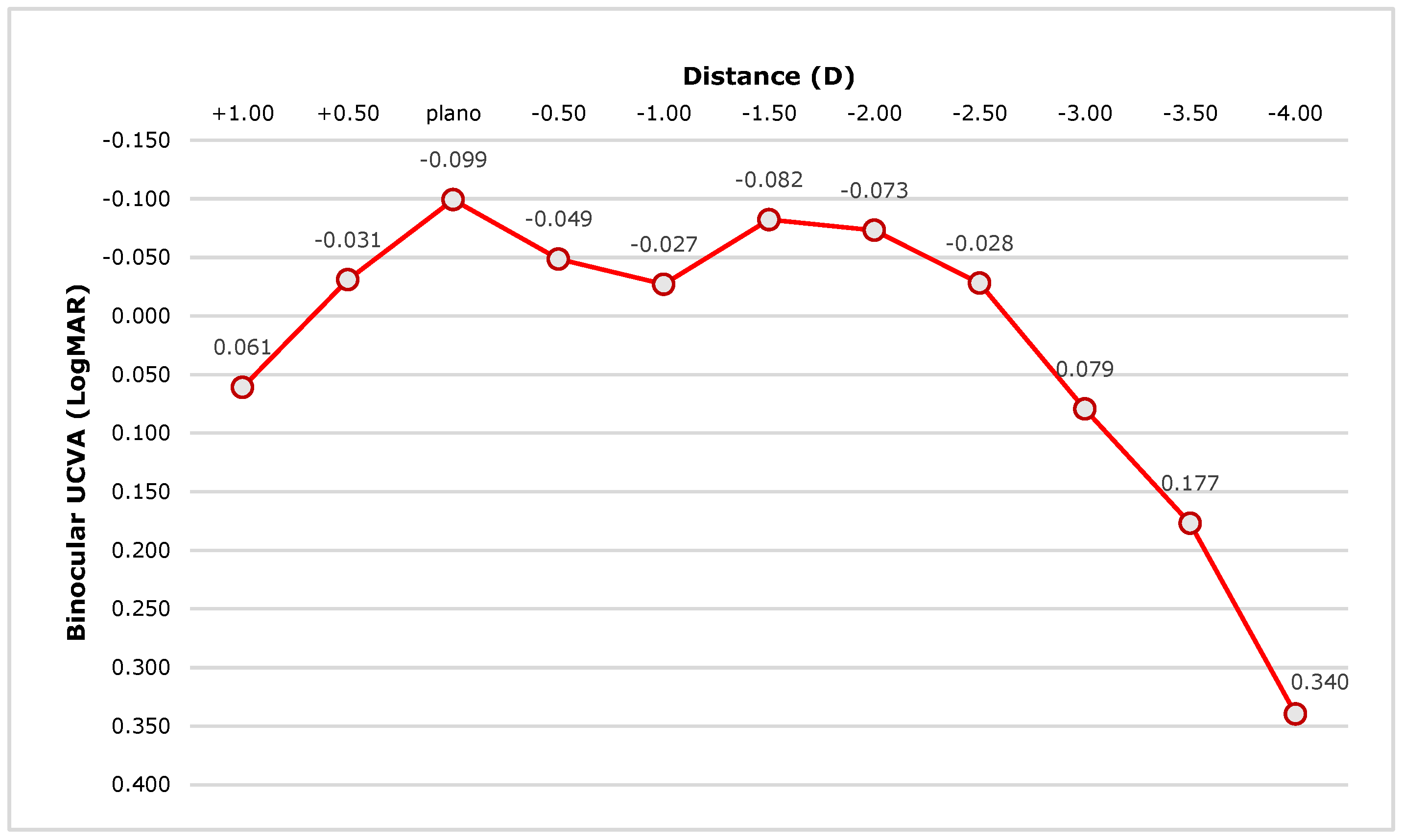
Figure 1 illustrates the defocus curve of the binocular UCVA measured with the LogMAR acuity chart, demonstrating the performance of the IOLs.
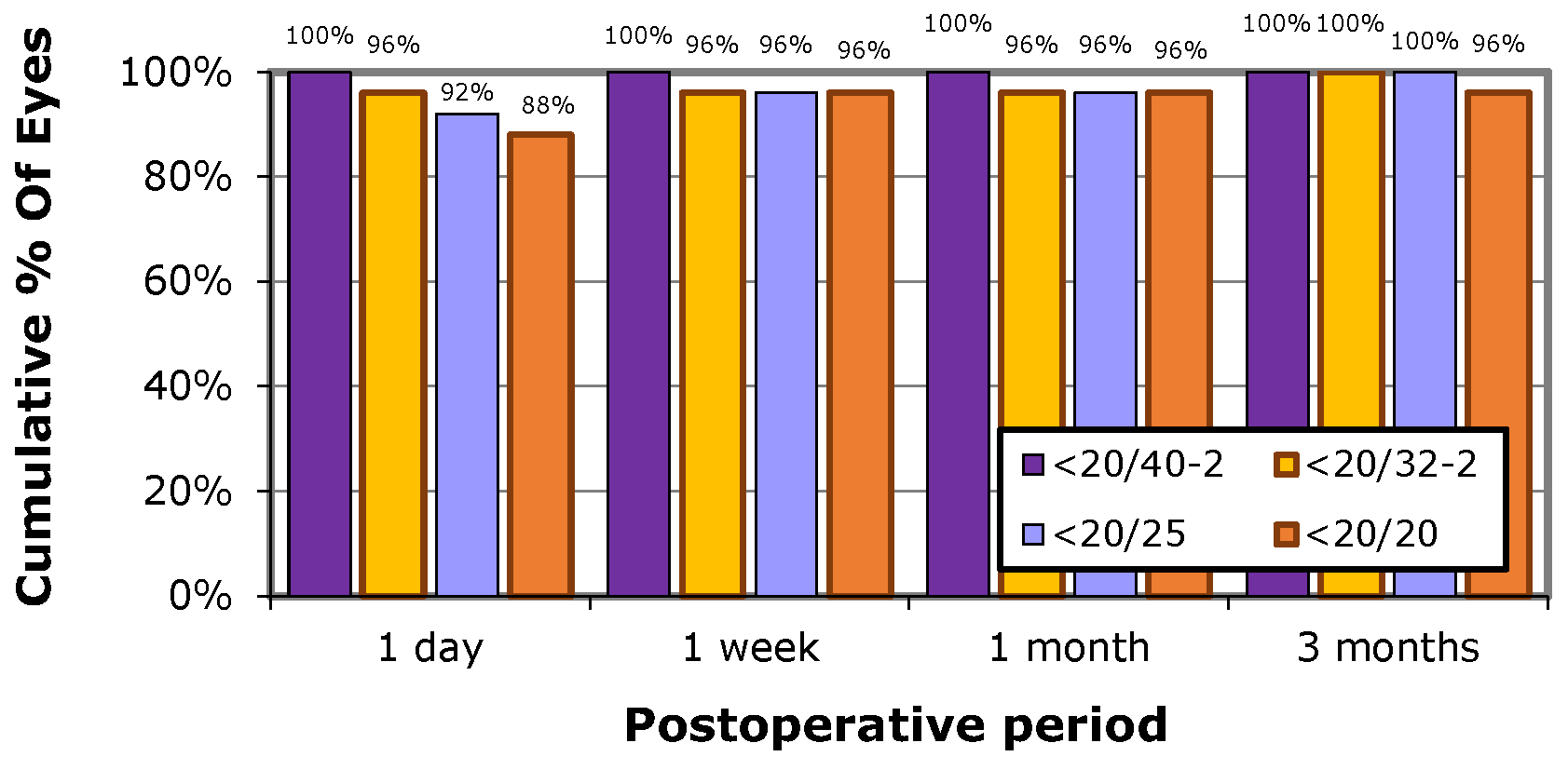
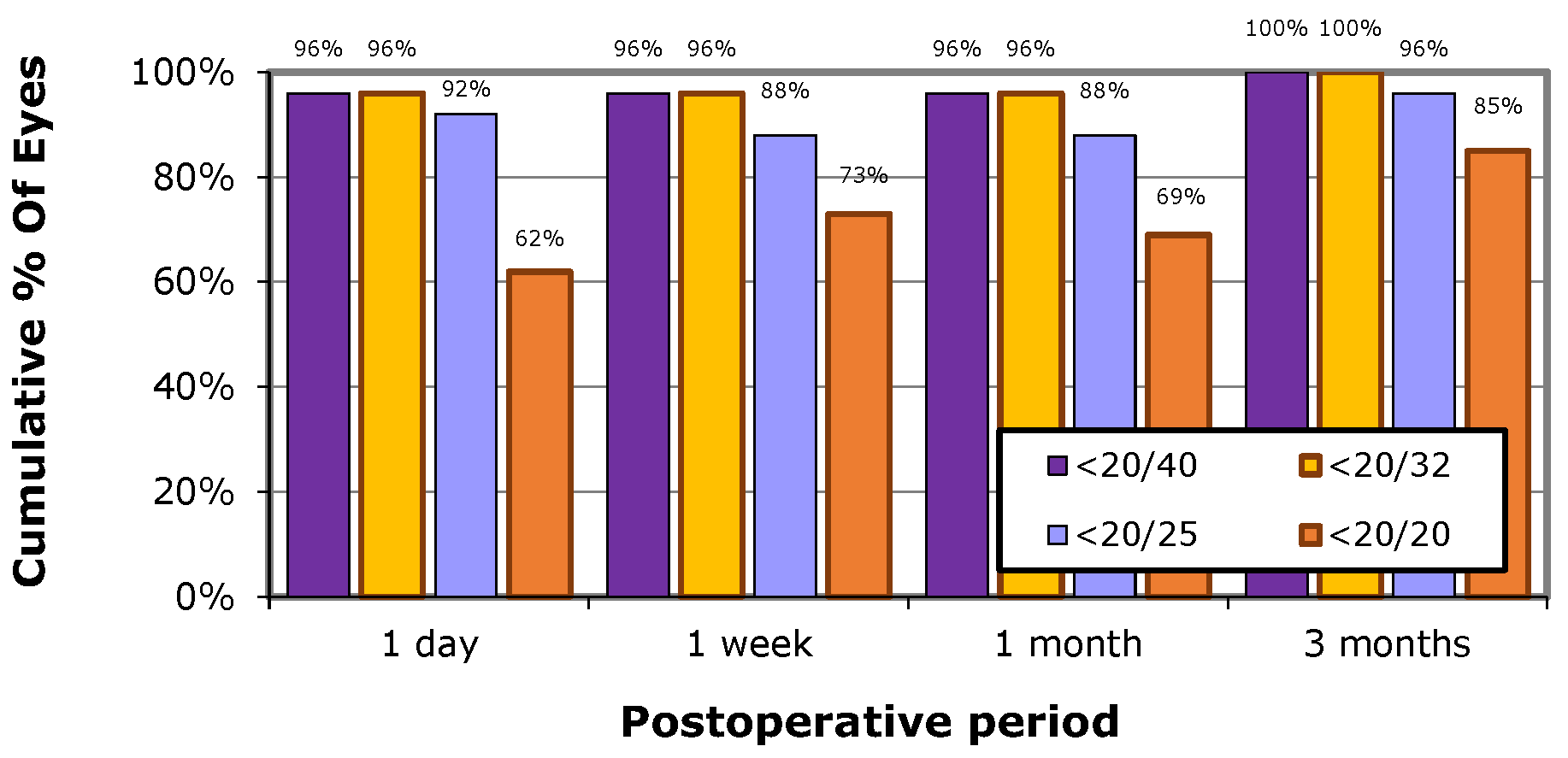
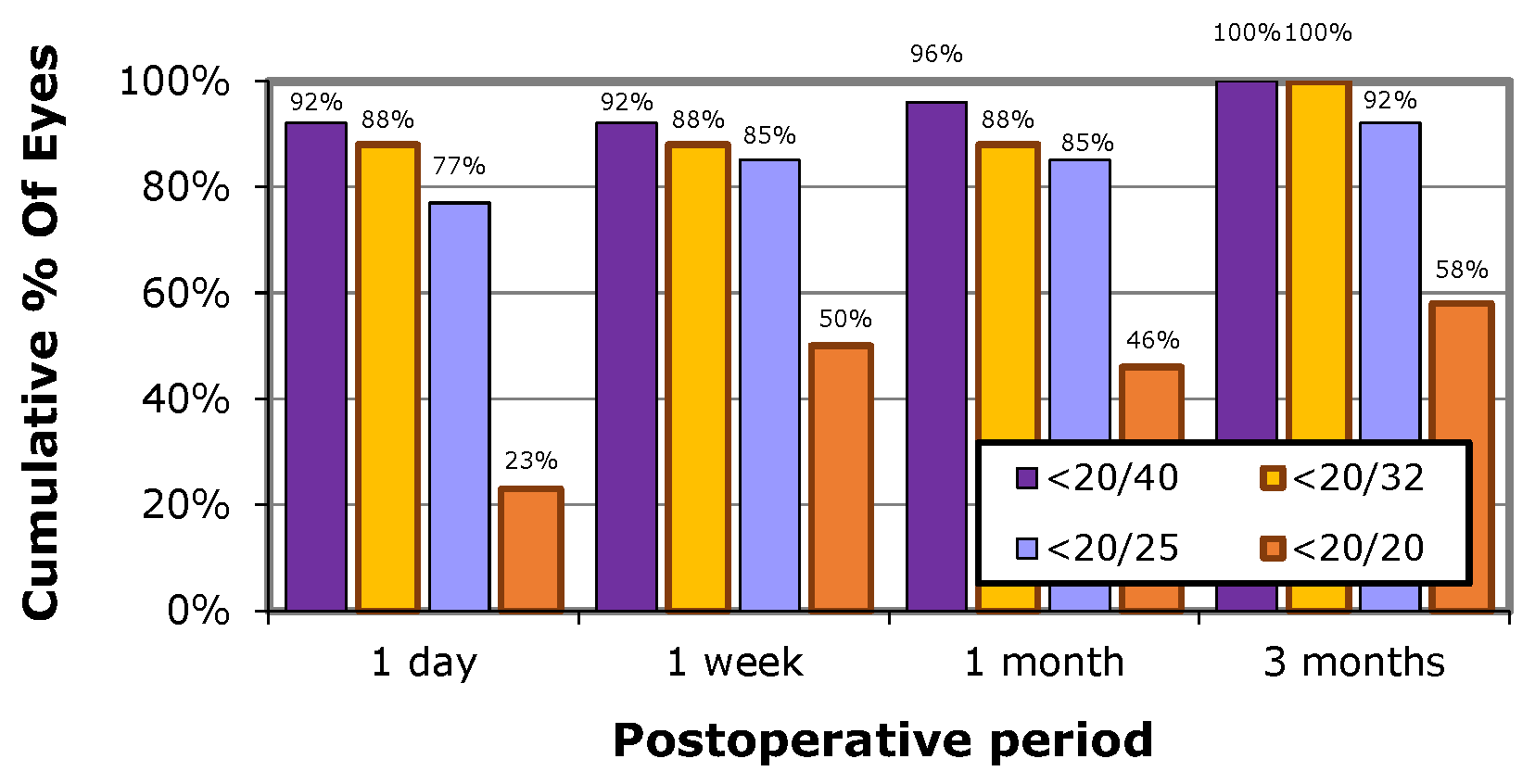
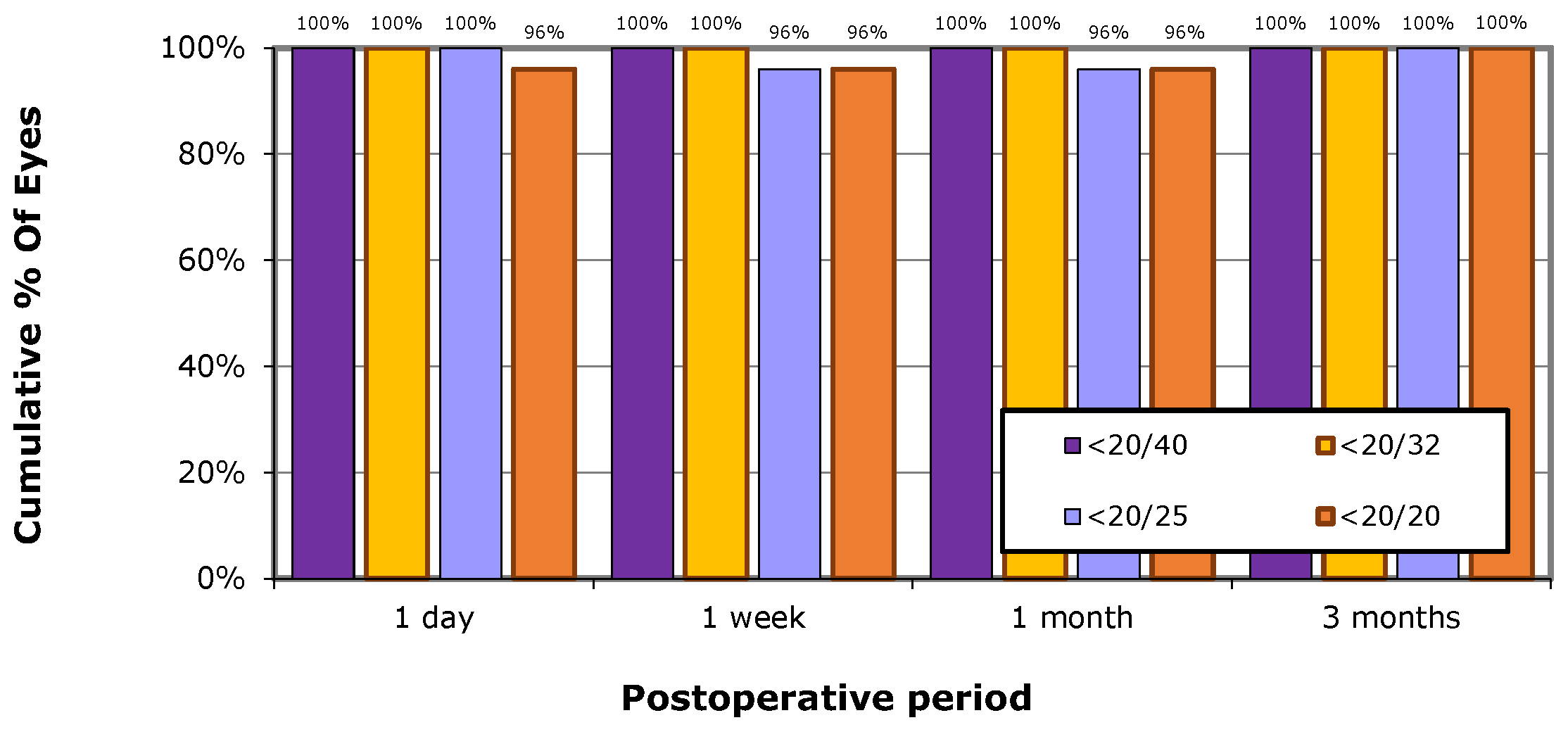
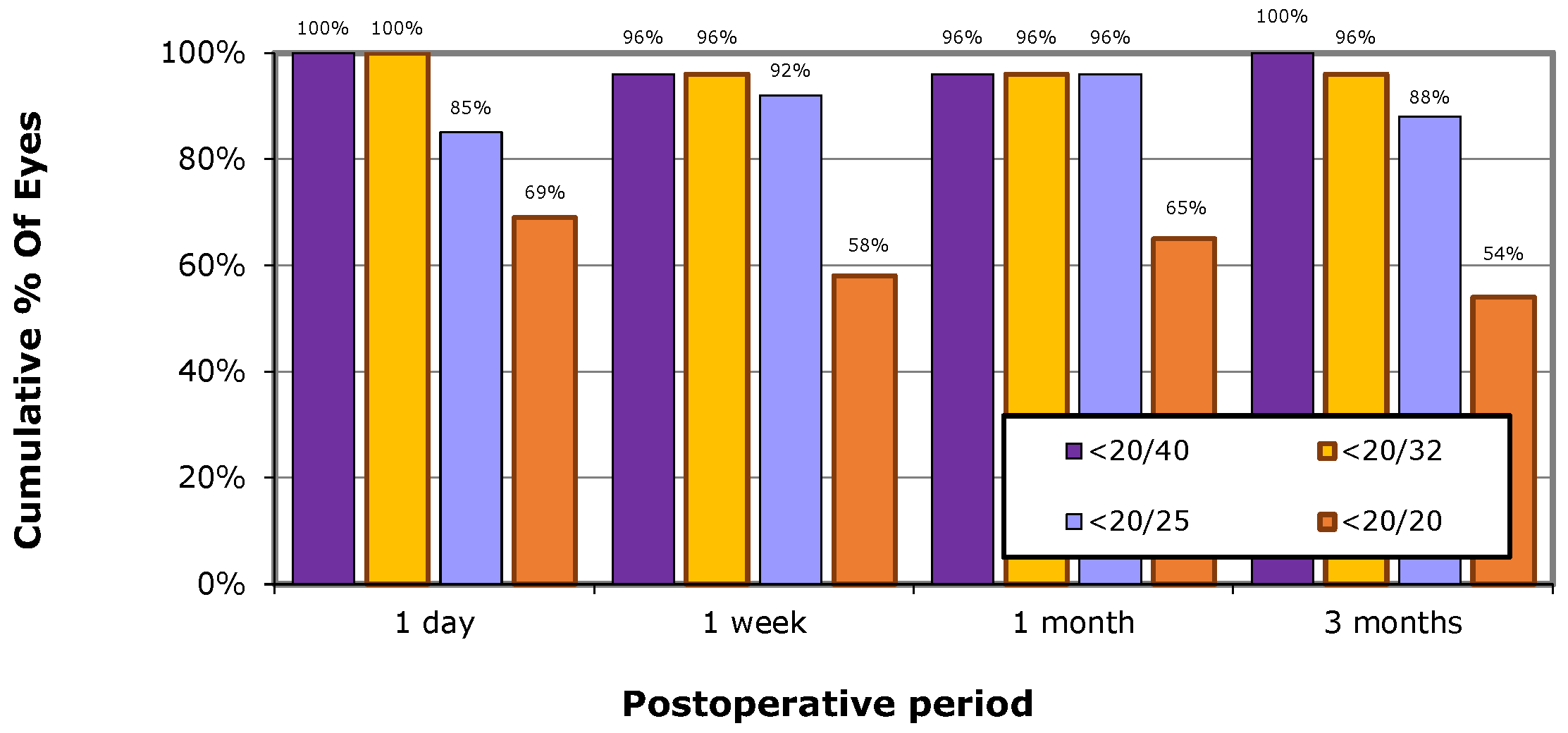
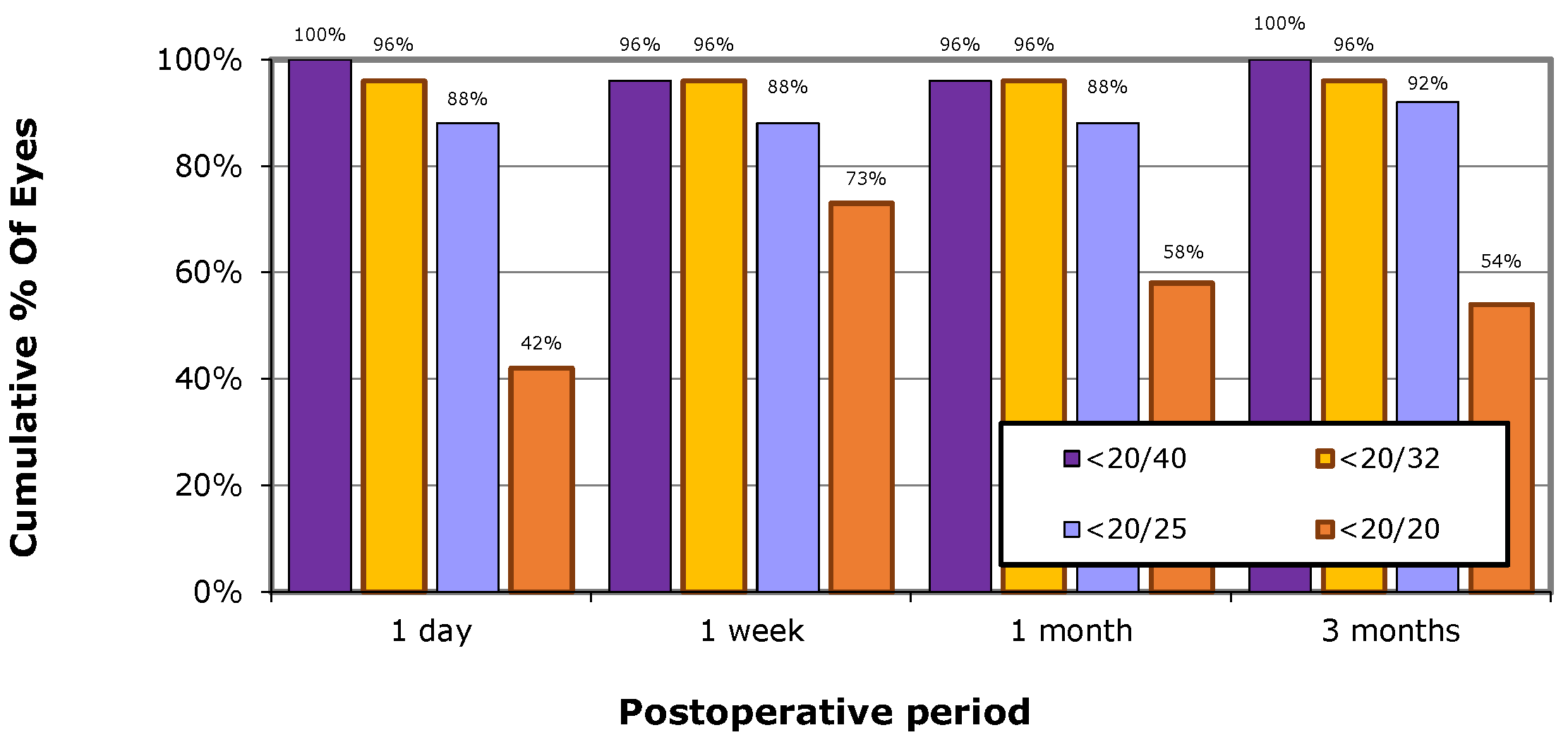
For binocular UCVA, all patients achieved visual acuity of 0.204 logMAR (20/25) or better after three months. In terms of the UIVA, 96% of patients achieved a reading acuity of 0.301 logMAR (20/32), with 96% achieving a reading acuity of 0.204 logMAR (20/25) and 85% achieving a reading acuity of 0.097 logMAR (20/20) at three months. Similarly, for UNVA, all patients achieved a reading acuity of 0.204 logMAR (20/32), 96% achieving a reading acuity of 0.204 logMAR (20/25) and 85% achieving a reading acuity of 0.097 logMAR (20/20) at three months.
Figure 2,
Figure 3 and
Figure 4 depict the analysis of visual recovery through postoperative binocular UCVA, UIVA, and UNVA at different time intervals.
Regarding the best-corrected visual acuity, all participants achieved a CDVA of 0.097 logMAR (20/20) after three months. For DCIVA, 88% achieved a reading acuity of 0.204 logMAR (20/25), and 54% achieved a reading acuity of 0.097 logMAR (20/20) at three months. As for DCNVA, 100% achieved a reading acuity of 0.301 logMAR (20/40), 92% achieved a reading acuity of 0.204 logMAR (20/25), but only 54% achieved a reading acuity of 0.097 logMAR (20/20) at three months.
Figure 5,
Figure 6 and
Figure 7 provide further analysis of best-corrected visual acuity recovery through postoperative binocular CDVA, DCIVA, and DCNVA in different time intervals.
3.3. Manifest Refraction
At 3-month follow-up, the postoperative manifest refraction indicated a spherical equivalent of 0.111 ± 0.368 D. Among the 52 eyes, 28 (53.8%) achieved a SEQ within ±0.25 D of emmetropia, 44 (84.6%) achieved a SEQ within ±0.50 D, and all 52 eyes (100%) achieved a SEQ within ±1.00 D. Furthermore, the 52 eyes had an average manifest cylinder of -0.490 ± 0.367 D at the 3-month mark.
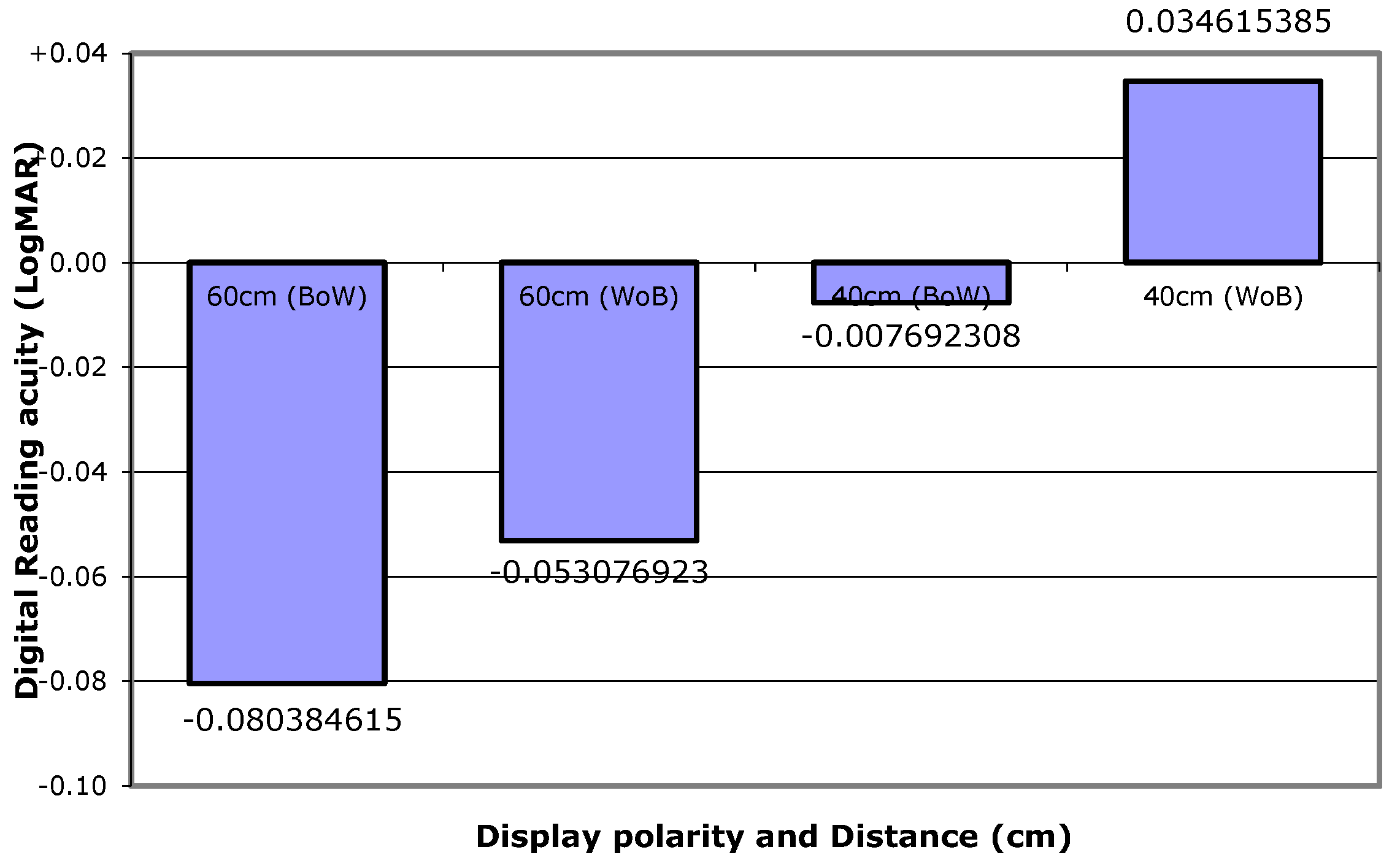
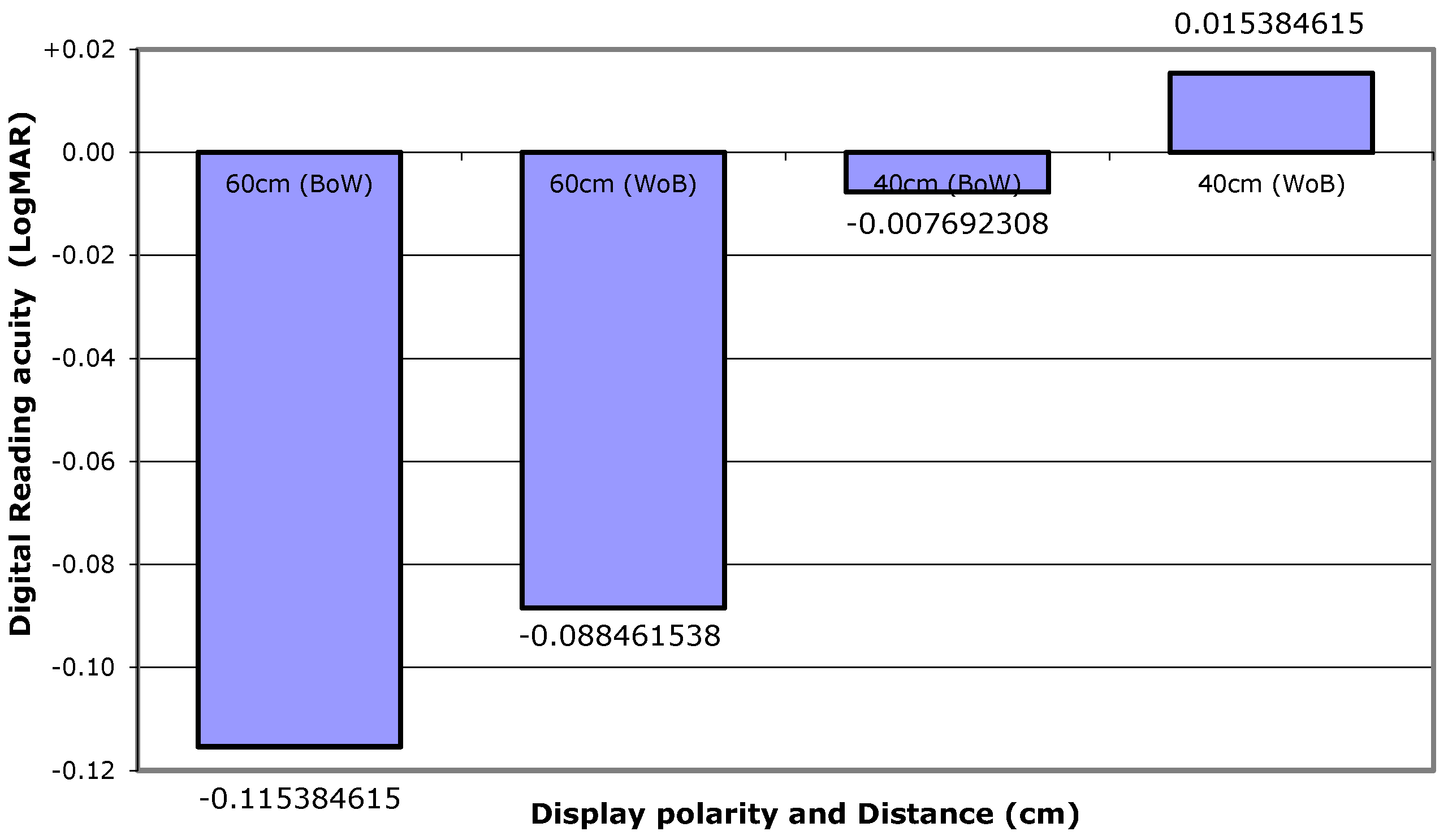
3.4. Polarity Display, Critical Print Size and Reading Speed
All patients participated in binocular reading acuity measurements at 40 cm and 60 cm using the MNREAD application at one month and three months after surgery. At 3 months, the reading acuity of BoW was -0.008 ± 0.083 at 40 cm and -0.115 ± 0.102 at 60 cm. For WoB, the values were -0.015 ± 0.086 at 40 cm and -0.088 ± 0.113 at 60 cm.
Figure 8 and
Figure 9 show the binocular reading acuity for both polarity displays at 40 cm and 60 cm, respectively, at one month and three months. The mean digital CPS with WoB at 40 cm was 0.173 ± 0.0168 logMAR at one month and 0.238 ± 0.100 logMAR at three months. The mean reading speed at one month and three months postoperatively was 84.63 ± 27.46 WPM and 101.89 ± 72.62 WPM, respectively.
Discussion
Our study aimed to evaluate the visual outcomes and quality of patients who received bilateral diffractive MF-IOL implantation. To minimize bias, we established inclusion and exclusion criteria and conducted thorough preoperative evaluations. The same surgeon performed all implantations using a consistent technique, reducing investigator bias. We followed up with patients at four time points to assess visual acuity recovery, with a focus on binocular CDVA as a measure of IOL performance and binocular UCVA for patient satisfaction and spectacle independence [
17,
18,
19,
20,
21].
Incorporating digital devices allowed us to gain a better understanding of the visual outcomes of the current time. Traditional LogMAR acuity charts, designed before the widespread use of digital devices, may not fully capture patients’ visual performance and satisfaction when seeking spectacle-free vision [
22,
23]. Factors such as screen illumination, display format, polarity, glance-like reading, and digital eye strain come into play with digital devices [
24].
Previous studies have shown that digital reading correlates well with patient satisfaction after cataract surgery and IOL implantation, regardless of IOL type [
25,
26]. The defocus curve of our study aligns with previous research on bilateral diffractive MF-IOL implantation, demonstrating positive IOL performance [
11,
12,
13,
14]. Our figures illustrate rapid visual recovery in patients with bilateral diffractive MF-IOL or toric MF-IOL implantation at one month and three months, with encouraging distance UCVA and satisfactory binocular UCVA at various distances.
To evaluate binocular reading acuity, we used the MNREAD application on digital devices. The disparity between conventional VA and reading acuity highlights the importance of using digital devices to assess postoperative satisfaction in patients with bilateral MF-IOL implantation. Our findings are consistent with a previous study that emphasizes the effectiveness of digital devices over conventional methods [
26].
The polarity of the screen and the CPS significantly affect the performance of digital reading. Positive display polarity, which emits more light from the white background, enhances digital reading by reducing spherical aberration and creating a pupil constriction effect [
9,
10]. Our study found that using a font size of 7 points or larger on a positive display polarity significantly increased digital reading satisfaction in patients with bilateral diffractive MF-IOLs. Additionally, we observed excellent CPS at 40 cm in patients with bilateral diffractive MF-IOLs or toric MF-IOLs for 1 to 3 months. To enhance reading comfort, we recommend adjusting the text size on digital devices to be approximately twice as large as the acuity letter, with a suggested minimum of 6-7 points or J3-J4. The reading speed at 1 and 3 months yielded acceptable results, although the high standard deviation was influenced by variations in the patient’s English proficiency.
We acknowledge the limitations of our study, including the relatively small sample size and the lack of evaluation on factors such as digital eye strain and glance-like reading. Conducting a larger study that compares digital reading with conventional reading and comprehensively assesses satisfaction with digital reading is necessary for more comprehensive information. Evaluating digital reading performance in patients with other types of IOL implantation would provide a greater understanding of its impact on visual outcomes. Furthermore, using other digital reading evaluation methods alongside the MNREAD application would contribute to a more conclusive assessment of daily use of digital devices. These further investigations will improve our understanding of digital reading and its implications, leading to better patient satisfaction.
Conclusion
In summary, patients who undergo bilateral implantation of diffractive MF-IOLs achieve satisfactory postoperative outcomes at various distances. The use of digital reading on digital devices for outcome measurements provides additional visual benefits compared to traditional methods. Factors such as screen polarity, font size, and CPS are crucial to enhance digital reading. Our research contributes to understanding the impact of digital devices on bilateral intraocular lens implantation. Future studies should incorporate digital device measurements to comprehensively assess the effectiveness and patient satisfaction associated with digital reading and visual outcomes.
Author Contributions
Conceptualization, T.S., N.S., W.S., T.W. and T.P.; Methodology, T.S., N.S. and T.P.; Formal Analysis, T.S., N.S. and T.P.; Investigation, T.S., N.S., W.S. and T.W.; Resources, T.S.; Data Curation, T.S., N.S. and T.P.; Writing – Original Draft Preparation, T.S., N.S. and T.P.; Writing – Review & Editing, T.S., N.S., W.S., T.W. and T.P.; Funding Acquisition, T.S
Funding
Financial support was received for this investigator-initiated trial from Alcon Laboratories (Thailand) Ltd. The funding source had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; the preparation of the version manuscript; or the decision to submit the manuscript for publication.
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of the Faculty of Medicine, Chulalongkorn University (IRB #765/63, approved November 26, 2020). Informed consent was obtained from all subjects involved in the study. Restrictions apply to the availability of these data. Data was obtained from the faculty of medicine, Chulalongkorn University and King Chulalongkorn Memorial Hospital and are available from the authors with the permission of from the faculty of medicine, Chulalongkorn University and King Chulalongkorn Memorial Hospital.
Acknowledgments
We acknowledge Dr.Tanavadee Rattanaphong for her dedication to facilitating the project process in the operating theatre.
Conflicts of Interest
The authors declare no conflict of interest. The sponsors had no role in the design, execution, interpretation, or writing of the study.
Abbreviation
| ACC |
reading accessibility index |
| BoW |
black on white |
| CDVA |
Corrected distance visual acuity |
| CPS |
critical print size |
| D |
Diopters |
| DCIVA |
Distance-corrected intermediate visual acuity |
| DCNVA |
Distance-corrected near visual acuity |
| IOLs |
intraocular lenses |
| IRB |
institutional review board |
| LogMAR |
Logarithm of the Minimum Angle of Resolution |
| MF-IOLs |
multifocal intraocular lenses |
| MRS |
maximum reading speed |
| RA |
reading acuity |
| SEQ |
spherical equivalent |
| SD |
standard deviations |
| TFNT |
trifocal natural toric |
| UCVA |
Uncorrected distance visual acuity |
| UIVA |
Uncorrected intermediate visual acuity |
| UNVA |
Uncorrected near visual acuity |
| WoB |
white on black |
References
- Mencucci, R.; Favuzza, E.; Caporossi, O.; Rizzo, S. Visual performance, reading ability and patient satisfaction after implantation of a diffractive trifocal intraocular lens. Clin Ophthalmol 2017, 11, 1987–1993. [Google Scholar] [CrossRef]
- Alio, J. L.; Plaza-Puche, A. B.; Férnandez-Buenaga, R.; Pikkel, J.; Maldonado, M. Multifocal intraocular lenses: An overview. Survey of Ophthalmology 2017, 62, 611–634. [Google Scholar] [CrossRef] [PubMed]
- Mangen, A.; Olivier, G.; Velay, J. L. Comparing Comprehension of a Long Text Read in Print Book and on Kindle: Where in the Text and When in the Story? Front Psychol 2019, 10, 38. [Google Scholar] [CrossRef] [PubMed]
- Shen, Z.; Lin, Y.; Zhu, Y.; Liu, X.; Yan, J.; Yao, K. Clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses: a systematic review and meta-analysis. Sci Rep 2017, 7, 45337. [Google Scholar] [CrossRef]
- Domínguez-Vicent, A.; Esteve-Taboada, J. J.; Del Águila-Carrasco, A. J.; Ferrer-Blasco, T.; Montés-Micó, R. In vitro optical quality comparison between the Mini WELL Ready progressive multifocal and the TECNIS Symfony. Graefes Arch Clin Exp Ophthalmol 2016, 254, 1387–1397. [Google Scholar] [CrossRef]
- Rasp, M.; Bachernegg, A.; Seyeddain, O.; Ruckhofer, J.; Emesz, M.; Stoiber, J.; Grabner, G.; Dexl, A. K. Bilateral reading performance of 4 multifocal intraocular lens models and a monofocal intraocular lens under bright lighting conditions. J Cataract Refract Surg 2012, 38, 1950–1961. [Google Scholar] [CrossRef] [PubMed]
- Gill, K.; Mao, A.; Powell, A. M.; Sheidow, T. Digital reader vs print media: the role of digital technology in reading accuracy in age-related macular degeneration. Eye (Lond) 2013, 27, 639–643. [Google Scholar] [CrossRef]
- Lin, Y.-T.; Lin, P.-H.; Hwang, S.-L.; Jeng, S.-C.; Liao, C.-C. Investigation of legibility and visual fatigue for simulated flexible electronic paper under various surface treatments and ambient illumination conditions. Applied Ergonomics 2009, 40, 922–928. [Google Scholar] [CrossRef]
- Plaza-Puche, A. B.; Alio, J. L. Analysis of defocus curves of different modern multifocal intraocular lenses. Eur J Ophthalmol 2016, 26, 412–417. [Google Scholar] [CrossRef]
- Cillino, G.; Casuccio, A.; Pasti, M.; Bono, V.; Mencucci, R.; Cillino, S. Working-age cataract patients: visual results, reading performance, and quality of life with three diffractive multifocal intraocular lenses. Ophthalmology 2014, 121, 34–44. [Google Scholar] [CrossRef]
- Kohnen, T.; Herzog, M.; Hemkeppler, E.; Schönbrunn, S.; De Lorenzo, N.; Petermann, K.; Böhm, M. Visual Performance of a Quadrifocal (Trifocal) Intraocular Lens Following Removal of the Crystalline Lens. American Journal of Ophthalmology 2017, 184, 52–62. [Google Scholar] [CrossRef]
- Kohnen, T.; Marchini, G.; Alfonso, J. F.; Bala, C.; Cochener, B.; Martinez, A.; Carreño, E. Innovative trifocal (quadrifocal) presbyopia-correcting IOLs: 1-year outcomes from an international multicenter study. J Cataract Refract Surg 2020, 46, 1142–1148. [Google Scholar] [CrossRef]
- Kim, T.-i.; Chung, T.-Y.; Kim, M. J.; Lee, K.; Hyon, J. Y. Visual outcomes and safety after bilateral implantation of a trifocal presbyopia correcting intraocular lens in a Korean population: a prospective single-arm study. BMC ophthalmology 2020, 20, 1–11. [Google Scholar] [CrossRef]
- Carreño, E.; Carreño, E. A.; Carreño, R.; Carreño, M.; López, V.; Potvin, R. Refractive and visual outcomes after bilateral implantation of a trifocal intraocular lens in a large population. Clinical Ophthalmology 2020, 369–376. [Google Scholar] [CrossRef]
- Tarib, I.; Kasier, I.; Herbers, C.; Hagen, P.; Breyer, D.; Kaymak, H.; Klabe, K.; Lucchesi, R.; Teisch, S.; Diakonis, V. F. Comparison of visual outcomes and patient satisfaction after bilateral implantation of an EDOF IOL and a mix-and-match approach. Journal of Refractive Surgery 2019, 35, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Sandoval, H. P.; Potvin, R.; Solomon, K. D. Visual Acuity, Defocus Curve, Reading Speed and Patient Satisfaction with a Combined Extended Depth of Focus Intraocular Lens and Multifocal Intraocular Lens Modality. Clin Ophthalmol 2020, 14, 2667–2677. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Vega, L.; Madrid-Costa, D.; Alfonso, J. F.; Montés-Micó, R.; Poo-López, A. Optical and visual performance of diffractive intraocular lens implantation after myopic laser in situ keratomileusis. Journal of Cataract & Refractive Surgery 2009, 35, 825–832. [Google Scholar] [CrossRef]
- Ortiz, D.; Alió, J. L.; Bernabéu, G.; Pongo, V. Optical performance of monofocal and multifocal intraocular lenses in the human eye. Journal of Cataract & Refractive Surgery 2008, 34, 755–762. [Google Scholar] [CrossRef]
- Palomino Bautista, C.; Carmona González, D.; Castillo Gómez, A.; Cristóbal Bescos, J. A. Evolution of Visual Performance in 250 Eyes Implanted with the Tecnis ZM900 Multifocal IOL. European Journal of Ophthalmology 2009, 19, 762–768. [Google Scholar] [CrossRef]
- Baudu, P.; Penin, F.; Arba Mosquera, S. Uncorrected Binocular Performance After Biaspheric Ablation Profile for Presbyopic Corneal Treatment Using AMARIS with the PresbyMAX Module. American Journal of Ophthalmology 2013, 155, 636–647. [Google Scholar] [CrossRef]
- Rementería-Capelo, L. A.; García-Pérez, J. L.; Gros-Otero, J.; Carrillo, V.; Pérez-Lanzac, J.; Contreras, I. Real-world evaluation of visual results and patient satisfaction for extended range of focus intraocular lenses compared to trifocal lenses. International Ophthalmology 2021, 41, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Bailey, I. L.; Lovie, J. E. New design principles for visual acuity letter charts. American journal of optometry and physiological optics 1976, 53, 740–745. [Google Scholar] [CrossRef] [PubMed]
- Hussaindeen, J. R. Commentary: A novel miniaturized visual acuity chart design. Indian Journal of Ophthalmology 2021, 69, 51–52. [Google Scholar] [CrossRef] [PubMed]
- Dobres, J.; Chahine, N.; Reimer, B. Effects of ambient illumination, contrast polarity, and letter size on text legibility under glance-like reading. Applied Ergonomics 2017, 60, 68–73. [Google Scholar] [CrossRef]
- Spadea, L.; Giannico, M. I.; Formisano, M.; Alisi, L. Visual Performances of a New Extended Depth-of-Focus Intraocular Lens with a Refractive Design: A Prospective Study After Bilateral Implantation. Ther Clin Risk Manag 2021, 17, 727–738. [Google Scholar] [CrossRef]
- Calabrèse, A.; To, L.; He, Y.; Berkholtz, E.; Rafian, P.; Legge, G. E. Comparing performance on the MNREAD iPad application with the MNREAD acuity chart. J Vis 2018, 18, 8. [Google Scholar] [CrossRef]
Figure 1.
Binocular UCVA defocus curve in LogMAR three months postoperatively showed values of -0.099 LogMAR at 0.00 defocus, and -0.082, -0.073, -0.028, and 0.079 LogMAR for defocus levels of -1.50, -2.00, -2.50, and -3.00, respectively, corresponding to simulated distances of 66 cm, 50 cm, 40 cm, and 33 cm. D = Dioptres; UCVA = uncorrected distance visual acuity.
Figure 1.
Binocular UCVA defocus curve in LogMAR three months postoperatively showed values of -0.099 LogMAR at 0.00 defocus, and -0.082, -0.073, -0.028, and 0.079 LogMAR for defocus levels of -1.50, -2.00, -2.50, and -3.00, respectively, corresponding to simulated distances of 66 cm, 50 cm, 40 cm, and 33 cm. D = Dioptres; UCVA = uncorrected distance visual acuity.
Figure 2.
Binocular UCVA postoperatively on day 1, 1 week, 1 month and 3 months UCVA = Uncorrected distance visual acuity.
Figure 2.
Binocular UCVA postoperatively on day 1, 1 week, 1 month and 3 months UCVA = Uncorrected distance visual acuity.
Figure 3.
Binocular UIVA (60 cm) postoperatively on day 1, 1 week, 1 month and 3 months UIVA = Uncorrected intermediate visual acuity.
Figure 3.
Binocular UIVA (60 cm) postoperatively on day 1, 1 week, 1 month and 3 months UIVA = Uncorrected intermediate visual acuity.
Figure 4.
Binocular UNVA (40 cm) postoperatively on day 1, 1 week, 1 month and 3 months UNVA = Uncorrected near visual acuity.
Figure 4.
Binocular UNVA (40 cm) postoperatively on day 1, 1 week, 1 month and 3 months UNVA = Uncorrected near visual acuity.
Figure 5.
CDVA at post-operative at day one, one week, one month, and three months. CDVA = Corrected distance visual acuity
Figure 5.
CDVA at post-operative at day one, one week, one month, and three months. CDVA = Corrected distance visual acuity
Figure 6.
DCIVA (60cm) at post-operative at day one, one week, one month, and three months DCIVA = Distance-corrected intermediate visual acuity.
Figure 6.
DCIVA (60cm) at post-operative at day one, one week, one month, and three months DCIVA = Distance-corrected intermediate visual acuity.
Figure 7.
DCNVA (40cm) at post-operative at day one, one week, one month, and three months DCNVA = Distance-corrected near visual acuity.
Figure 7.
DCNVA (40cm) at post-operative at day one, one week, one month, and three months DCNVA = Distance-corrected near visual acuity.
Figure 8.
One month postoperative of intermediate (60 cm) and near (40 cm) reading acuity comparing the positive display polarity and the negative display polarity in the MNREAD application. BoW = black on white background; UCVA = Uncorrected Visual Acuity; WoB = white on black background.
Figure 8.
One month postoperative of intermediate (60 cm) and near (40 cm) reading acuity comparing the positive display polarity and the negative display polarity in the MNREAD application. BoW = black on white background; UCVA = Uncorrected Visual Acuity; WoB = white on black background.
Figure 9.
Three months postoperative of intermediate (60 cm) and near (40 cm) reading acuity comparing the positive display polarity and the negative display polarity in the MNREAD application. BoW = black on white background; UCVA = Uncorrected Visual Acuity; WoB = white on black background.
Figure 9.
Three months postoperative of intermediate (60 cm) and near (40 cm) reading acuity comparing the positive display polarity and the negative display polarity in the MNREAD application. BoW = black on white background; UCVA = Uncorrected Visual Acuity; WoB = white on black background.
Table 1.
Types and number of IOL models used in this study.
Table 1.
Types and number of IOL models used in this study.
| AcrySof Model |
N of the IOLs used |
% of the total IOLs used |
| TFNT00 |
25 |
48.07% |
| TFNT20 |
13 |
25% |
| TFNT30 |
8 |
15.38% |
| TFNT40 |
4 |
7.69% |
| TFNT50 |
0 |
0% |
| TFNT60 |
2 |
3.84% |
Table 2.
Post-operative VA at 1 week, 1 month and 3 months (mean ± SD) CDVA = Corrected distance visual acuity, DCIVA = Distance-corrected intermediate visual acuity, DCNVA = Distance-corrected near visual acuity DCNVA, LogMAR = Logarithm of the Minimum Angle of Resolution, UCVA = Uncorrected distance visual acuity, UIVA = Uncorrected intermediate visual acuity, UNVA = Uncorrected near visual acuity.
Table 2.
Post-operative VA at 1 week, 1 month and 3 months (mean ± SD) CDVA = Corrected distance visual acuity, DCIVA = Distance-corrected intermediate visual acuity, DCNVA = Distance-corrected near visual acuity DCNVA, LogMAR = Logarithm of the Minimum Angle of Resolution, UCVA = Uncorrected distance visual acuity, UIVA = Uncorrected intermediate visual acuity, UNVA = Uncorrected near visual acuity.
Measurement
(logMAR) |
1 week |
1 month |
3 months |
Monocular
N=52 eyes |
Binocular
N=26 subjects |
Monocular
N=52 eyes |
Binocular
N=26 subjects |
Monocular
N=52 eyes |
Binocular
N=26 subjects |
| UCVA 4 m |
-0.040±0.101 |
-0.069±0.107 |
-0.015±0.107 |
-0.078±0.108 |
-0.036±0.093 |
-0.084±0.079 |
| CDVA 4 m |
-0.086±0.085 |
-0.120±0.108 |
-0.071±0.091 |
-0.095±0.089 |
-0.091±0.067 |
-0.139±0.079 |
| UIVA 60 cm |
0.065±0.124 |
0.032±0.109 |
0.089±0.149 |
0.035±0.131 |
0.051±0.087 |
-0.014±0.078 |
| DCIVA 60 cm |
0.067±0.098 |
0.051±0.091 |
0.078±0.144 |
0.028±0.117 |
0.091±0.092 |
0.048±0.089 |
| UNVA 40 cm |
0.104±0.122 |
0.079±0.131 |
0.111±0.129 |
0.084±0.126 |
0.104±0.088 |
0.040±0.081 |
| DCNVA 40 cm |
0.085±0.108 |
0.053±0.098 |
0.089±0.130 |
0.066±0.113 |
0.087±0.085 |
0.048±0.073 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).