1. Introduction
Artificial intelligence (AI) has undergone rapid developments to transform business, society and healthcare practices [
1,
2]. Medical imaging (MI) is one of the healthcare areas that is being the most impacted by AI, with recent research showing that AI can perform as well as or better than humans in detecting, classifying and monitoring diseases [
1,
3,
4]. The advancements in AI have enabled the swift and simultaneous extraction and correlation of multiple imaging parameters, surpassing the limitations of human perception by identifying subtle findings that were previously undetectable to the naked eye [
4,
5]. As a result, MI is undergoing a transformative shift from a subjective, skill-based discipline to a more objective and scientifically led specialty. This evolution is marked by the use of accurate, efficient, and reproducible image analysis techniques [
4,
5]. Through the amalgamation of AI and advanced MI methods, healthcare professionals can now provide more precise diagnoses and significantly improve patients’ outcomes by adapting medicine to the patients’ needs [
4,
5,
6]. Healthcare information technology (IT) systems with AI technology hold promise to reduce personnel burden in healthcare institutions, by streamlining workflows and allocating resources more effectively and efficiently [
6,
7,
8,
9].
The radiographers’ clinical practice is becoming more automated with AI, which could result in a reduction on the current radiographer roles and responsibilities [
10]. However, this change is not without risks, since the AI’s potential liabilities are not yet fully understood or appropriately managed. Furthermore, the databases are often built-up without thorough validation processes, which require audits and evaluations to verify the decision-making process and to ensure optimal outcomes [
11,
12]. This change also means the radiographer’s role needs to be adapted and, consequently, with support of education and training to be better integrated in the transformed clinical practice. Recent studies [
7,
13] have reported the perspectives and attitudes of radiographers with regards to the integration of AI in medical imaging practice and education in other countries. Results showed a positive attitude but with concerns due to the lack of understanding of AI technologies and AI training, which can lead to insecurity in their workplace or even resistance to the implementation of these new technologies. To better prepare this transformation in clinical practice, meticulous follow up is required as well as the involvement of all key stakeholders involved in the process. To address this gap, this study aimed to explore the possible impact AI on radiographers’ practice and profession in Switzerland based on perspectives from clinical radiographers, teaching-staff, students and physicians (radiology, nuclear medicine and radiation oncology), to better adapt radiographers’ training for the market needs.
2. Materials and Methods
A cross-sectional survey was developed to collect data on perspectives from radiographers, teaching staff, students and physician (radiologists, nuclear medicine specialists and radiation oncologists) on the possible impact of AI on radiographers’ activities and profession in Switzerland.
2.1. Data Collection
Data was collected using an online survey on Microsoft Forms® and included 34 questions and sub-questions addressing participants’ demographics, AI-knowledge, skills, confidence, training in AI and their perceptions about the impact of AI on clinical practice. Snowball sampling was performed by distributing the survey through the Swiss Association of Radiographers (ASTRM), different professional bodies linked to the physicians and social media (Instagram®, Facebook® and LinkedIn®). To encourage more radiographers to participate in the study, the link was also sent out to the head of departments and clinical tutors that are in contact with the respective universities of applied sciences.
2.2. Survey
The survey collected medical imaging professionals’ AI-knowledge, skills, training, confidence in AI and their perceptions about the impact of AI on clinical practice. This tool was first developed by Rainey et al in 2021 [
14] who demonstrated internal consistency ranging from 0.736-0.777. The authors also ascertain the validity of this survey, grounded on AI expert reviews from Society of Radiographers (SCoR), other AI experts reviews, and key literature [
8,
14].
The original instrument was available in English and was translated to French and German as necessary, as well culturally adapted to the Swiss context and structures. A comprehensive translation process was conducted to ensure conceptual equivalence between both versions. The process involved several steps, including forward translation, expert panel back-translation, pre-testing and feedback [
15]. Forward translation was performed by two individuals ensuring conceptual and contextual equivalence and then two other individuals processed to translate back to English. The two English versions were then compared, with content equivalence determined to be adequate by the reviewer. To maintain face and content validity of the survey through its translation, and ensure the comprehension of the statements, a pilot study was conducted by sharing the survey with the Swiss AI steering committee of the ASTRM and three imaging physicians, each representing one specialty. Based on the results from the pilot study, suggestions were integrated when appropriate. Reliability of the scale was determined by calculating internal consistency for all Likert scale questions in the survey.
2.3. Data Analysis
Data management and data analysis was carried out using Stata, version 17.0 (StataCorp LP, College Station, Texas) and Microsoft Excel. Descriptive statistics were used to describe participants’ demographics in terms of percentages and frequency distribution. Qualitative data acquired through the three open questions of the survey was analysed using thematic analysis following the Braun & Clarke Framework (2006) [
16].
2.4. Ethics
Under Swiss Law, the current project/questionnaire does not fall under the regulations for research involving human subjects, and as such, does not require authorisation from any federal or cantonal ethics committee. A committee member (Arthur Zinn-Poget) of the Swiss Association of Research Ethics Committees gave exemption of this study. To comply with ethical standards (LRH, 2011) [
17] and the Swiss constitution, art. 118b (1999) [
18], an enclosure letter was presented on the first page of the online survey. This letter provided a clear explanation of the study’s purpose, context, and an estimation of the completion time. Participants were assured of the anonymous nature of the study and no associated risks or compensation for participating. Additionally, a letter including contact details, allowing participants to seek further information available to participants. Participants were notified that study findings may be shared publicly or presented in scientific conferences. To confirm their agreement to participate, participants were required to check a box to signify consent.
3. Results
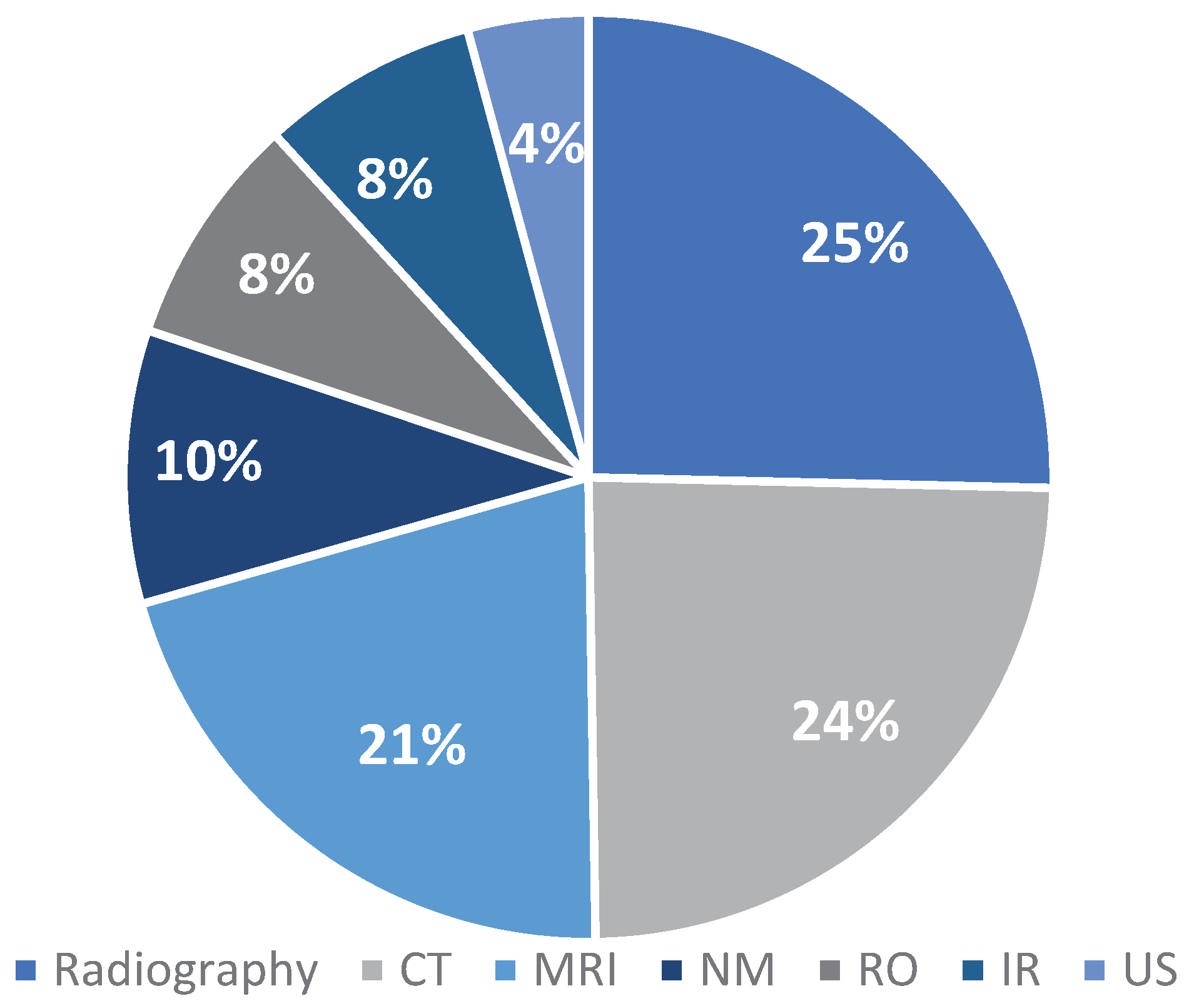
A total of 242 participants agreed to participate in the study. The demographic characteristics of these participants are presented in
Table 1. General radiography, CT and MRI were identified as the most performed by participants in this study (
Figure 1).
3.1. Internal Consistency
Cronbach alphas were calculated for all Likert scale variables for each population. The results showed adequate to low internal consistency with alpha’s ranging from 0.692 for the radiographers and 0.717 for the physicians.
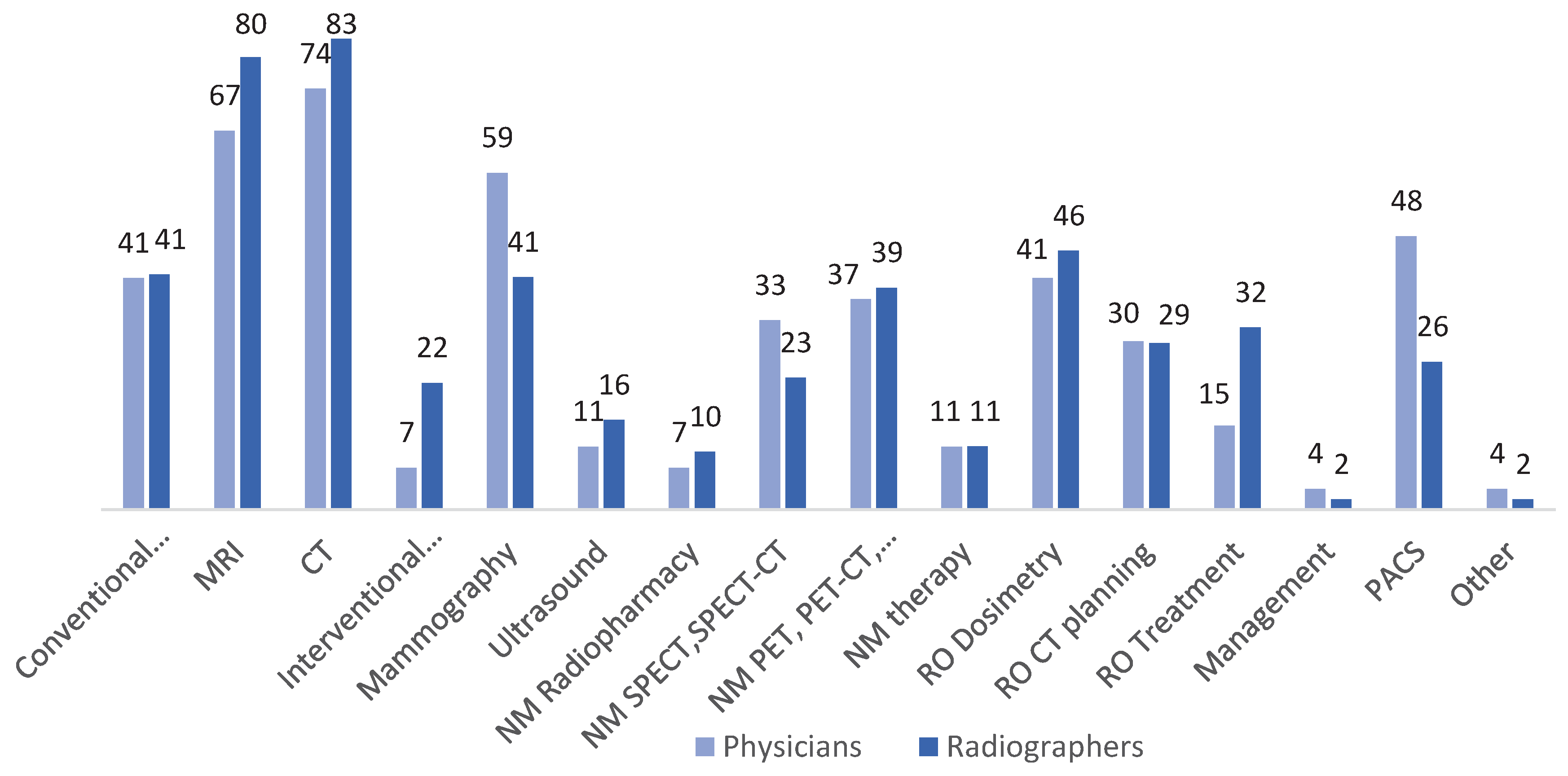
3.2. AI impact on Radiographers’ Activities
Radiographers indicated that CT (83%), MRI (80%), conventional radiology (41%), mammography (41%), radiotherapy dosimetry (46%) and PET (39%) examinations are the main activities impacted by AI. In contrast, RO treatment (32%), RO CT planning (29%), PACS (26%), SPECT examinations (23%), interventional radiology (22%), ultrasound (16%), NM therapy (11%), NM radiopharmacy (10%), and management (2%) are less impacted by AI intervention. Results were similar to those from the physicians except for a higher impact on mammography (59%) and PACS (48%) compared to radiographers’ perspective (
Figure 2).
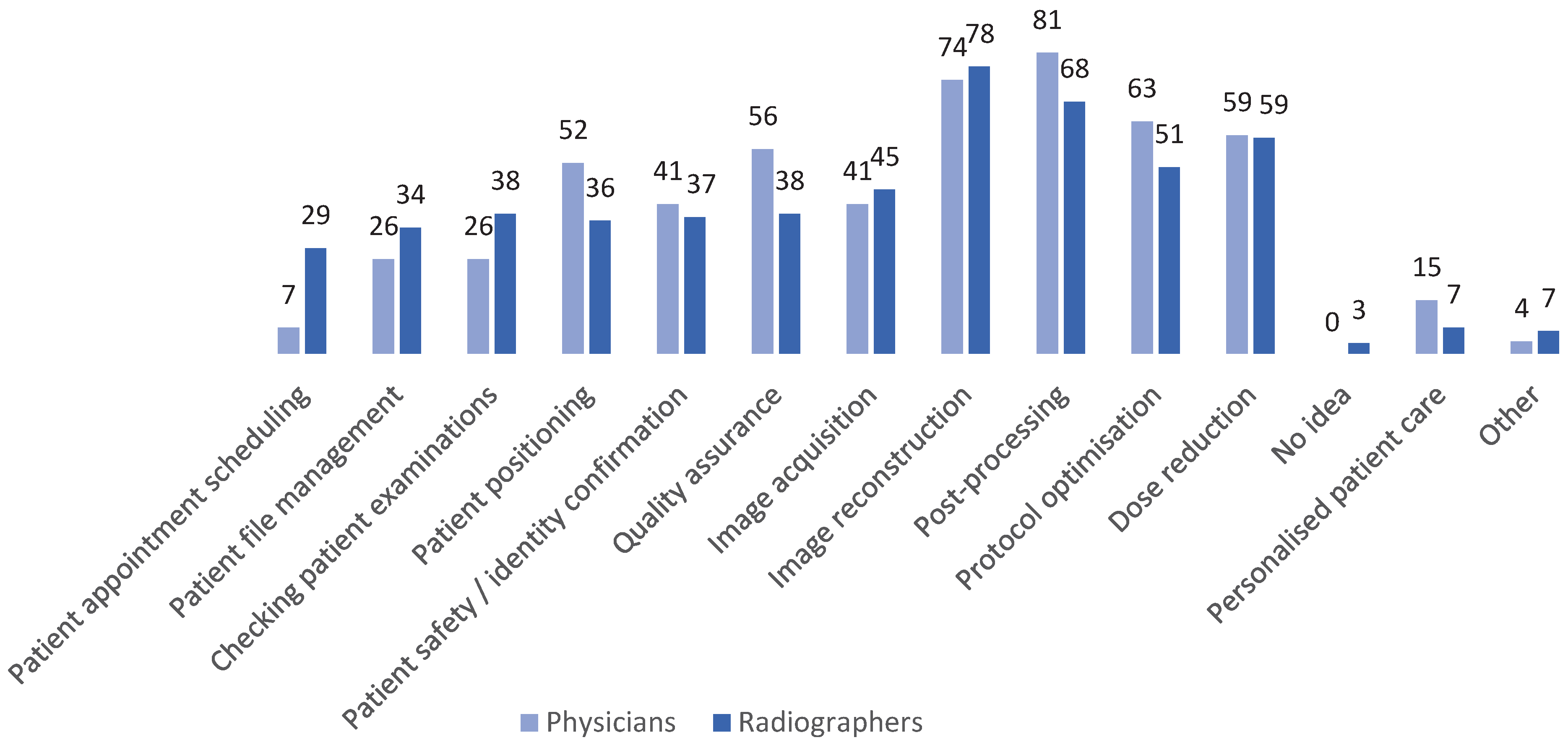
While data management (38%), quality assurance-related activities (38%), safety and identity check (37%), patient positioning (36%), file management (34%) and patient appointments scheduling (29%) are less impacted. Personalised patient care (7%) was presented as an area less impacted by AI in the radiographer’s daily routine (
Figure 3).
Physicians also provided their perceptions regarding the main radiographer activity areas that are affected by AI (
Figure 3).
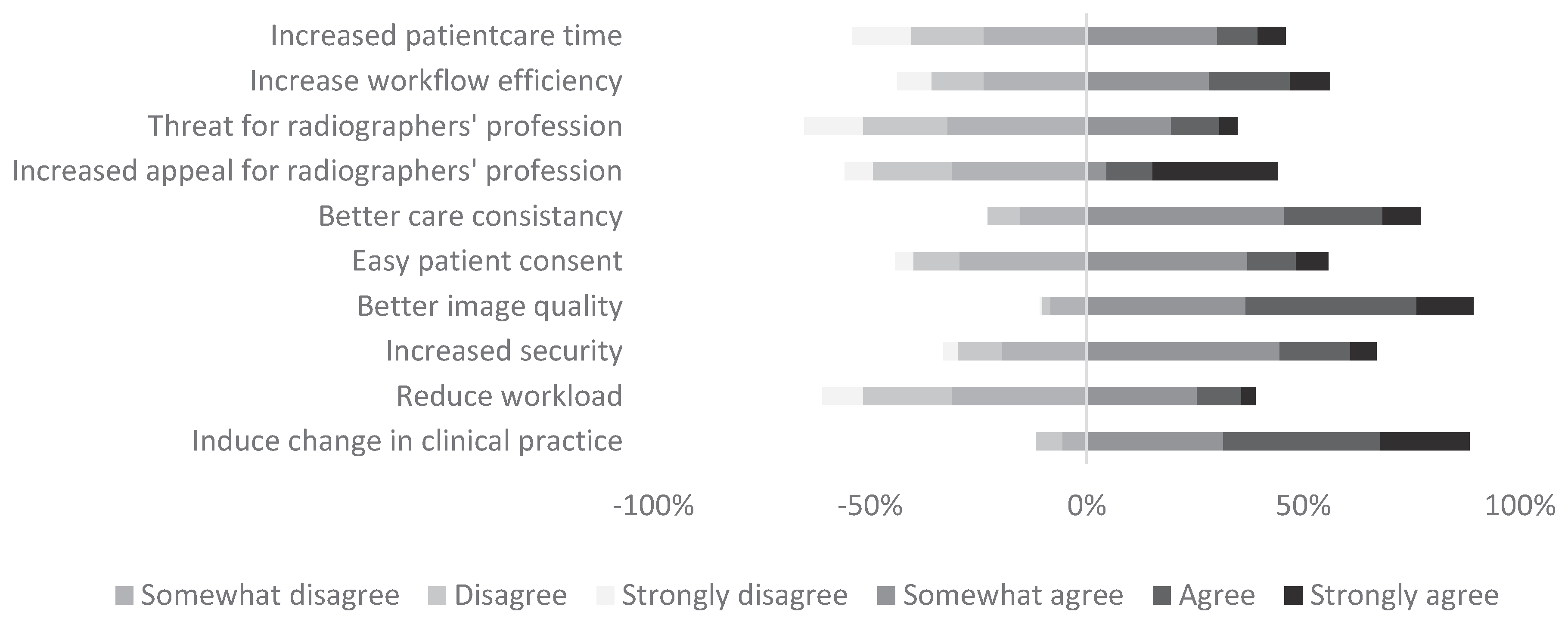
Radiographers mostly agree that the implementation of AI is going to induce change in their clinical practice or that it will improve image quality, where 80% and 90% respectively either expressed “somewhat agree” and “agree”/ “strongly agree”. On the other hand, 60% of them expressed “negative perspectives” when asked if AI will help reduce workload and 65% indicated that if AI was a threat to the profession. Appeal for the profession showed more divided opinions where 56% scored “somewhat disagree”, “disagree” or “strongly disagree” and 44% referred “positive feelings” (
Figure 4a).
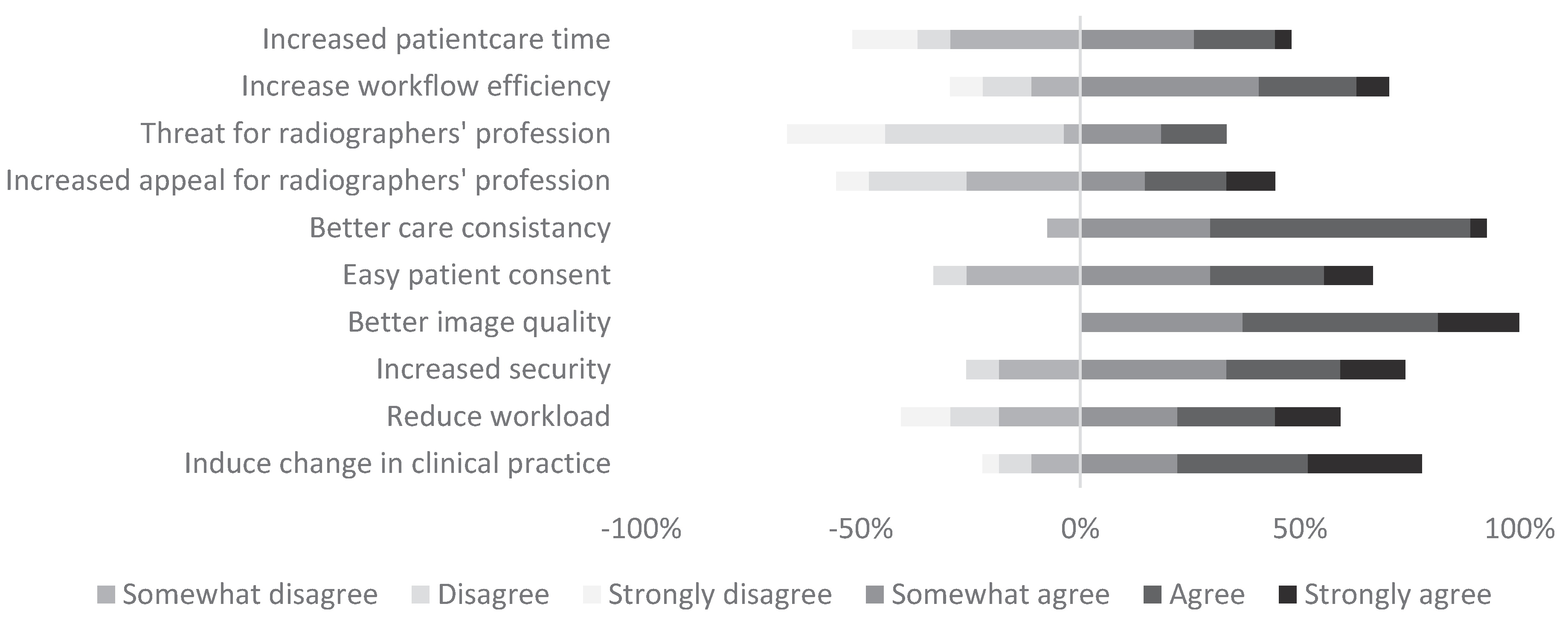
For all physicians (100%), image quality was also considered as something that would be improved by AI. They also agreed that better consistency on care would be found, where 93% “somewhat agree”, “agree” or “strongly agree”. However, as for radiographers 67% of physicians either “somewhat disagree”, “Disagree” or “Strongly disagree” when asked if AI was a threat for the profession (
Figure 4b).
3.3. Confidence, Knowledge, and Training
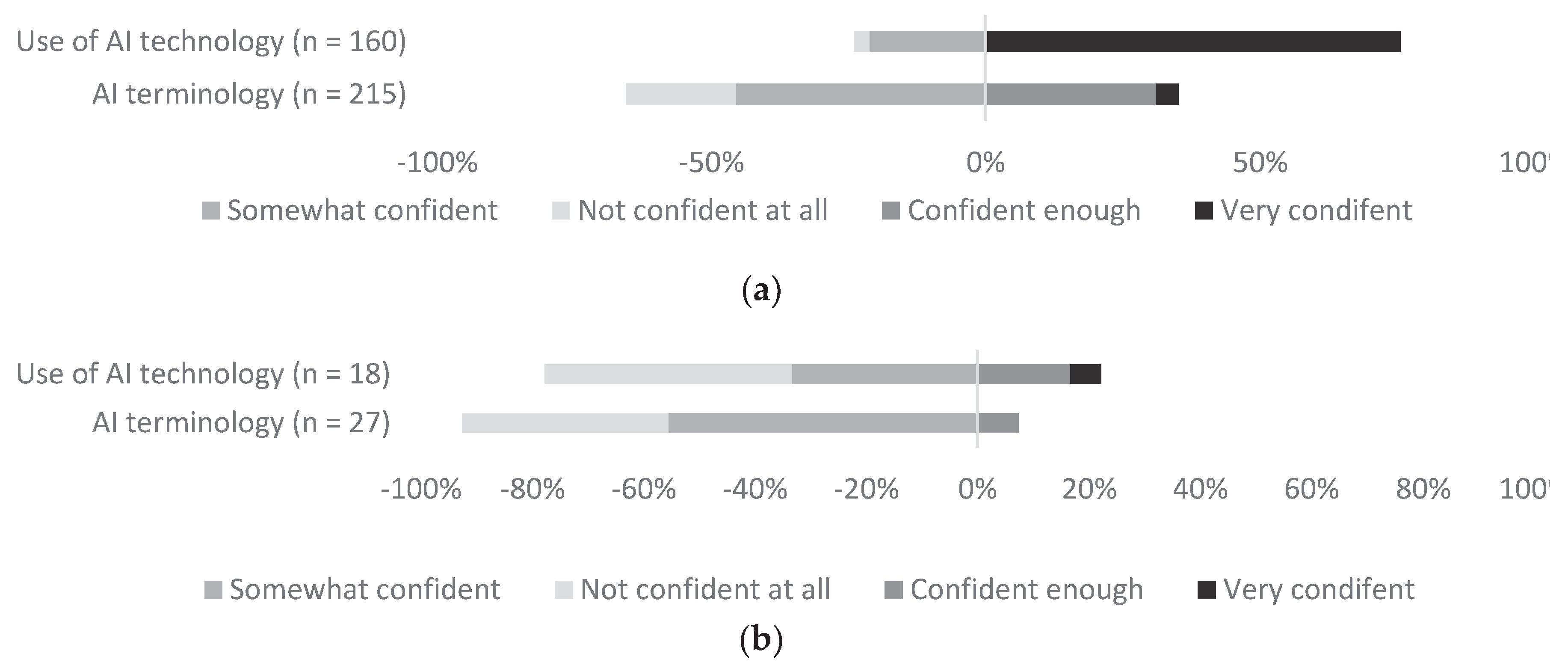
Radiographers were “very confident” or “confident enough” with the use of AI technology in clinical practice (76%) (
Figure 5a). However, when physicians where asked the same question about the radiographers’ profession, much fewer of them seem to feel “very confident” or “confident enough” with the use of AI technology (23%) (
Figure 5b). When asked how confident participants felt with the understanding of AI terminology, 66% of radiographers and 93% of physicians, expressed being “somewhat confident” or “not confident at all” (
Figure 5a and
Figure 5b).
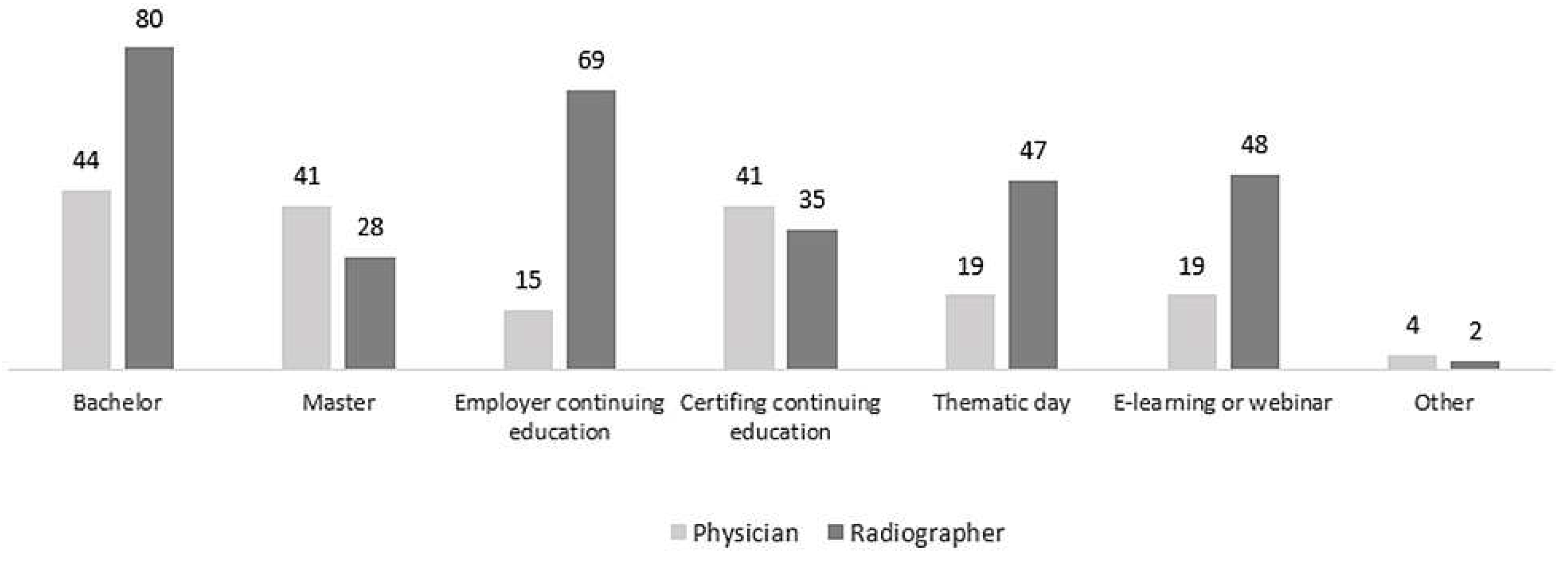
Radiographers and physicians all agree that AI training should be included in the Bachelor education programs with 93% of them indicating that they “somewhat agree”, “agree” or “strongly agree” with this statement. Majority of them did not agree (88%) with the fact that there are sufficient existing training programs for AI. Slightly more divided opinions were found when asked about if they felt that they had sufficient training, where 69% indicated not agreeing and 31% that they did. Radiographers indicated that AI education should be mainly delivered through Bachelor’s programmes (80%), continuing education offered by the employer (69%), while continuing professional development (CPD) (35%), thematic day (47%), e-learning or webinar (48%) were also indicated as useful resources. The survey participants indicated that Master’s programmes (27%) were less popular as a means of AI education. Physician perspectives were slightly different from radiographers’ opinions (
Figure 6).
3.4. AI: Opportunity or Threat to Radiographers?
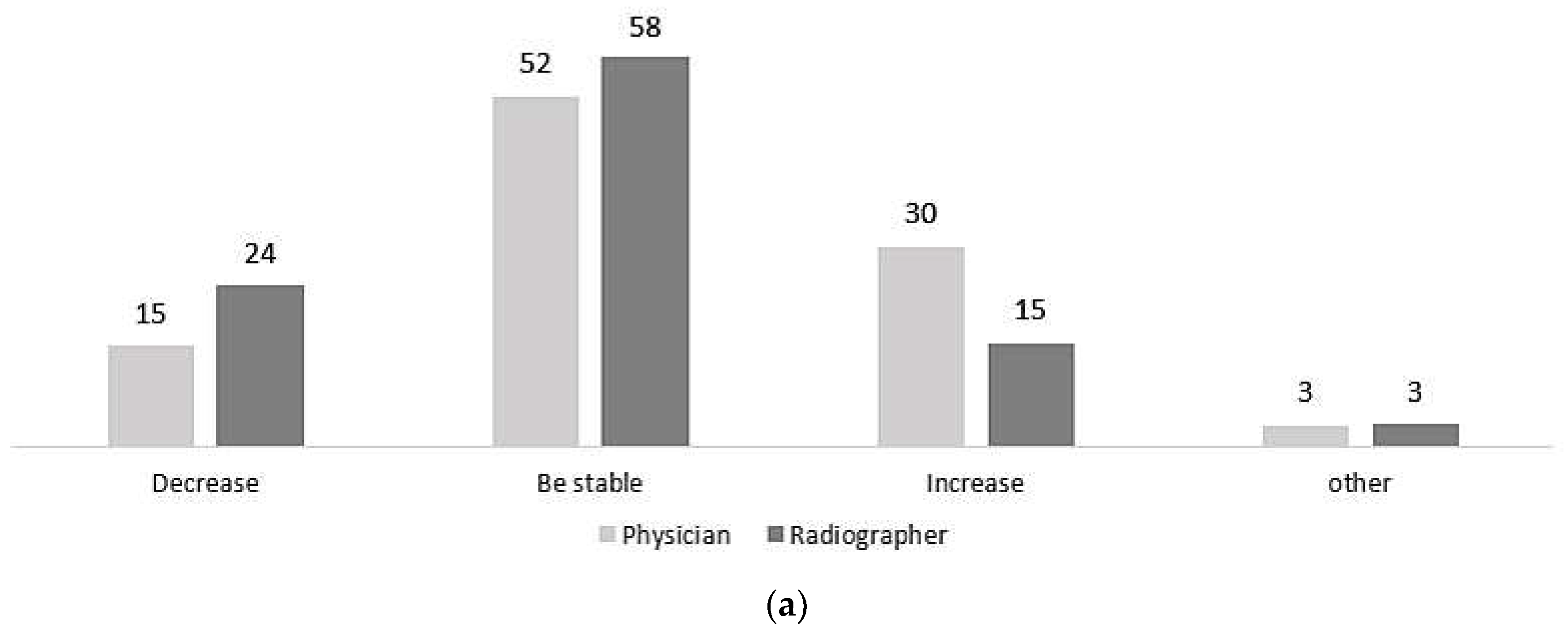
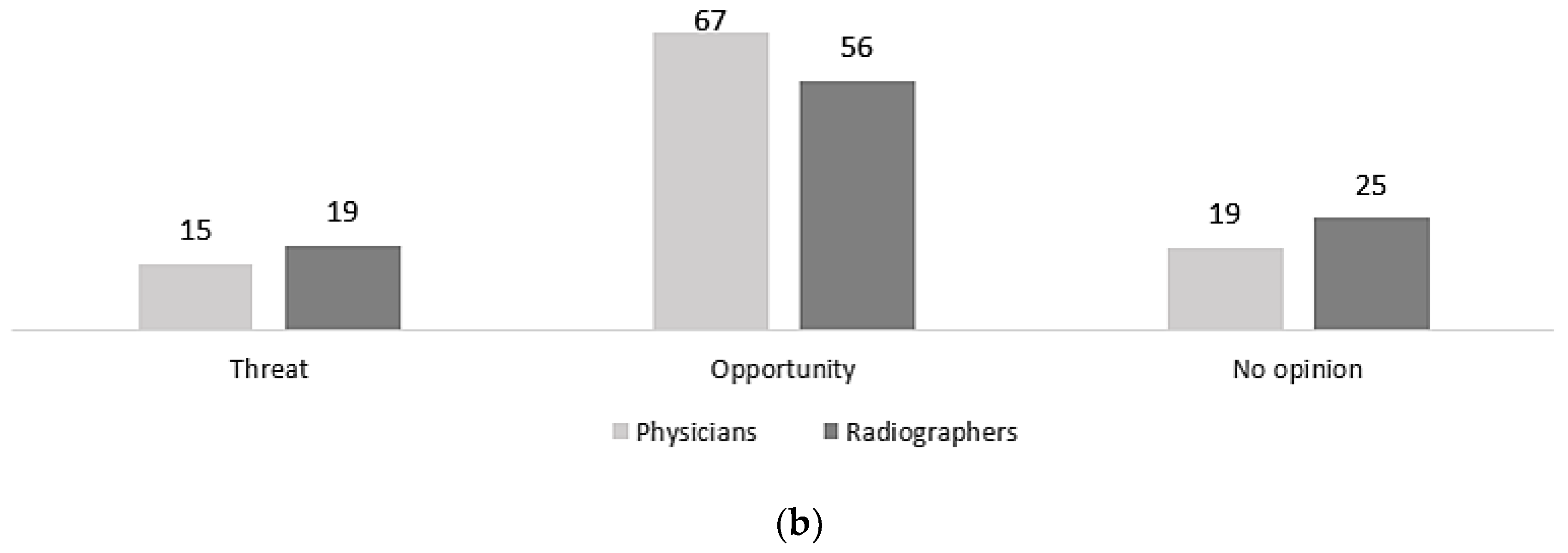
More than half of the radiographers (58%) and physicians (52%) indicated that the number of workplaces will remain stable in the future, some of radiographers (15%) and physicians (30%) believed that workplaces would increase, while others (15% physicians; 24% radiographers) considered that job opportunities will decrease (
Figure 7a). For both surveyed populations (radiographers: 56% (n=120/215); physicians: 67% (n=18/27)), AI is perceived more as an opportunity that a threat for the radiography profession (
Figure 7b).
3.5. Qualitative Data
Open-ended questions were used to explore respondents’ perception of the implementation of AI in practice (medium/long-term changes) and whether it is considered as a threat or an opportunity.
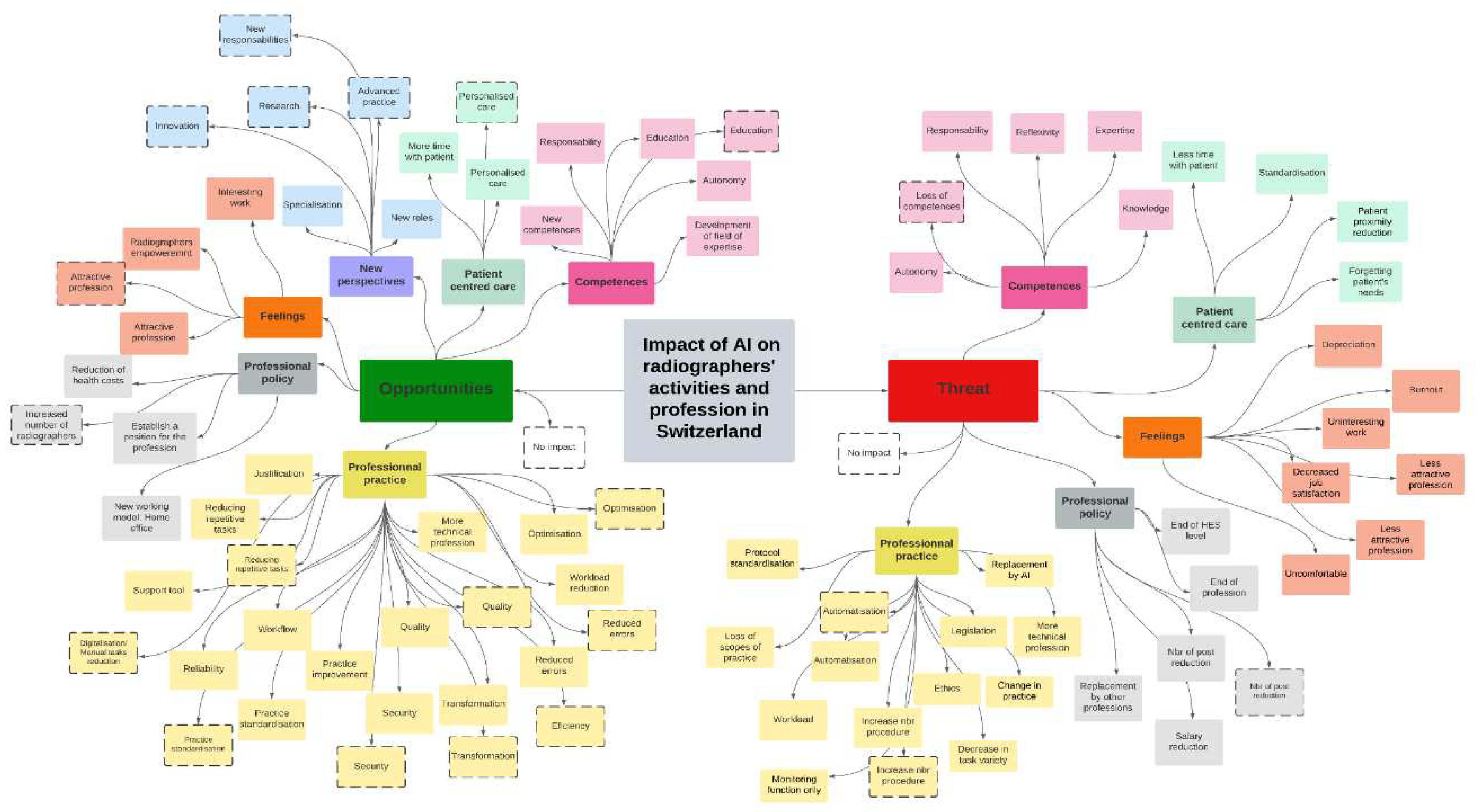
Five themes emerged from the thematic analysis: (i) competences, (ii) patient centred care, (iii) feelings, (iv) professional policy and (v) professional practice. All themes covered both negative and positive aspects in relation to AI, as expressed by the participants. However, an additional theme appeared as uniquely an opportunity and was titled (vi) new perspectives. This theme contained more codes coming from physicians namely innovation, research, advanced practice, and new responsibilities (
Figure 8). Thirty codes for radiographers and 15 for physicians were identified on the positive implications of AI, including 9 identical codes (education, personalised-care, attractive profession, reduction repetitive tasks, practice standardization, security, transformation, reduced errors, and optimisation). Thirty-two codes were identified for radiographers and 4 for the physicians on the negative implications of AI, 3 of which were identical (number of post reduction, increase number of procedures and automatisation) (
Figure 8).
3.5.1. Medium/Long Term Changes from the Development and Implementation of AI on the Profession
Content and quotes from the 6 themes are described below, as well as more detailed codes in
Supplementary Materials. Some codes were similar (autonomy, responsibility, time with patient, attractiveness of the profession) for opportunities and threats, meaning that what is seen as an opportunity for some participants was also seen as a threat by others.
Radiographers acknowledged several benefits that AI could provide for professional practice. For instance, they highlighted wordings linked to “quality“, “security“, “ergonomy“, “justification“ and “optimisation” as aspects that could be improved by AI tools. The physicians also identified positive impacts, similar to those identified by the radiographers. Some examples of radiographers and physicians’ responses are shown in
Supplementary Materials.
Radiographers indicated mainly a negative future repercussion over their activities with a “reduction of the number of job positions”, “hiring unqualified and cheaper professionals”, “fewer resources”, “salary reduction”, and even the “possible disappearance of the radiographer profession “.
While some participants pointed out a potential negative impact of AI, others viewed it as a chance to expand patient care by reaching more individuals. They also saw it as a positive development with the potential to reshape the healthcare system, possibly leading to changes in the role of radiographers in the future. Some examples of radiographers and physicians’ responses are shown in
Supplementary Materials.
Radiographers expressed rather negative feelings about the development of AI in their clinical practice, mentioning for example the increase of “panic”, “stress”, “burn out”, “pressure”, “divestment”, “disempowerment” and “boredom”. Some examples of radiographers and physicians’ responses are shown in
Supplementary Materials.
Radiographers’ opinion was balanced between negative and positive statements concerning the implementation of AI for patient-centred care and how it could improve this area. Positive impacts, such as “more time with the patient”, “more personalized examinations tailored to the patient”, or the “development of new skills or responsibilities”, increasing the patient experience and satisfaction. Some examples of radiographers and physicians’ responses are shown in
Supplementary Materials Radiographers raised concerns about a possible negative impact in their competences due to the implementation of AI in the clinical practice, compromising their “expertise, reflexivity and decision-making ability in protocol adaptation”.
"[...] Additionally, there will be power outages, and we won’t be able to use AI, and we’ll feel sorry for ourselves about not knowing how to function without it." (radiographer)
Other radiographers stated AI use as an opportunity to acquire “new competences, responsibility, knowledge, skills”, leading to an increase in “autonomy”, highlighting the need of a better “education, CPD and specific AI training”. Some examples of radiographers and physicians’ responses are shown in
Supplementary Materials.
Participants emphasised also the possibility of a positive impact of AI implementation in advancing practice in different fields such as “complex tasks accessibility, diagnostic tasks development with AI assistance or pre-reporting, medical tasks delegation, AI data/quality manager position, research, increased autonomy, diversification of profession either in patient related task or equipment related task”. Some examples of radiographers and physicians’ responses are shown in
Supplementary Materials.
Figure 8.
Physicians extracted themes concerning impact of AI as threat or opportunity for radiographers’ activities and profession in Switzerland.Note: Codes in the boxes that have the border highlighted by (- - -) are the codes given by physicians participating in the study, while the non-highlighted boxes are the codes emerging from radiographers’ response.
Figure 8.
Physicians extracted themes concerning impact of AI as threat or opportunity for radiographers’ activities and profession in Switzerland.Note: Codes in the boxes that have the border highlighted by (- - -) are the codes given by physicians participating in the study, while the non-highlighted boxes are the codes emerging from radiographers’ response.
4. Discussion
The study aimed to explore the perspectives of radiographers and physicians regarding the impact of AI on radiographers’ profession in both fields of medical imaging and radiation therapy. Our results, based on 242 responses (89% radiographers, 11% physicians), indicate that while 43% use AI in clinical practice, 63.8% lack confidence in AI terminology. Participants predominantly view AI as an opportunity (57.2%) but also as a threat (18.5%), with concerns about job reduction (22.6%) and automation bias (16.4%). A significant majority (68.3%) feel unprepared for AI implementation due to the absence of specific training (87.6%), and 93% believe AI education should be integrated into undergraduate programs.
4.1. AI Application and its Impact On Medical Imaging Modalities and Specialties
Participants believe that AI will mainly have an impact on CT and MRI, the two modalities in which participants had the most experience. When asked about their expectations regarding the impact of AI on various aspects of their daily activities, radiographers as well as physicians, believed that the technical part of their job, such as image reconstruction, post-processing, and protocol optimisation, would be the main areas impacted by this technology. Both populations surveyed agree that AI will induce changes in clinical practice, with positive aspects such as better image quality and stronger security.
However, radiographers and physicians do not agree on the impact of AI on workload, with physicians being more positive and believing that AI will reduce the workload. This discrepancy can be due to the payment system applied in Switzerland, considering that physicians are paid per “act”, while radiographers receive a salary that does not take in account the work volume [
19]. Other studies [
20,
21] have also indicated a positive attitude towards AI among physicians, most likely due to the AI support in reducing the interpretation time. However, this increase in workload can impact on the accuracy of radiologists. According to Alexander at al. [
22], a minimum time should be required to avoid the detection and interpretation errors since it is one of the main issues in lawsuits currently in USA for malpractice in Radiology. The authors advocate that studies must be conducted to identify how many examinations or images radiologists can review in any period of time (number of studies per day or images per unit time) while maintaining accuracy not to compromise the medical imaging outcome. The aim is to provide an examination that supports adequately the choices made regarding follow up and treatment for the patient to achieve the best outcome and quality of life.
4.2. Confidence, Knowledge & Training
Radiographers exhibited a comparatively high level of confidence in the practical application of AI technology (76%), yet they experienced lower confidence levels when it came to comprehending AI terminology (66%). In contrast, physicians showed lower confidence levels in both aspects using AI technology (23%). This may be linked to the access to education and training, participation in conferences or closer contacts with industry, which is more limited for radiographers [
21].
Regarding education, participants considered that it should be mainly delivered through the Bachelor’s program, 69% of radiographers indicated that their employers should offer them a specific training program, and 15% of physicians agree to this. This discrepancy can be explained by the fact that in Switzerland, clinicians are the heads of department who are responsible for making decisions of where training should be provided to the radiographers. Similar observations were identified in other countries [
13,
14,
23,
24,
25,
26,
27,
28,
29] when compared to the Swiss context. Switzerland also faces a deficiency of AI training programs. This has been included in the design of the new Bachelor’s degree program being offered in Western Switzerland, and the AI steering committee is already planning to offer a continuing development program to radiographers who are currently practicing in clinical centres. Similar programmes have now started to begin in Europe for radiographers [
7]. This aligns with The Society and College of Radiographers guidance for AI [
30,
31] and recommendations available in the literature [
32], showing a tendency in Switzerland to evolve in this direction.
4.3. Opportunity & Threats for Future
Both populations (radiographers: 56%; physicians: 67%) considered AI as an opportunity for the radiography profession, but also mentioned fears. Physicians were more positive than radiographers about its impact on the profession. They even suggested that the implementation of AI would induce a possible increase in the number of workplaces for radiographers (physicians 30% versus radiographers 15%). In comparison to 56% of radiographers, 67% of physicians thought that AI represents an opportunity for the radiographer profession as the development of new responsibilities, involvement in research and innovation, and advanced practice. This view corresponds to what radiographers should be doing in the future according to the various recommendations already published [
30,
31,
32]. Swiss radiographers need to position themselves, with the support of professional associations and medical doctors, in taking a proactive, collaborative role in the deployment, evaluation and monitoring of AI in clinical practice with the specific competences in image analysis, quality, and safety that are part of the radiographer’s roles [
33].
The thematic analysis revealed a striking duality in radiographers’ perceptions since certain aspects were identified as both opportunities and threats. One illustrative example is the person-centred care. Radiographers suggested that the introduction of AI holds the promise of relieving the burden of repetitive and time-consuming tasks, enabling professionals to allocate more time and attention to patients. On the other hand, radiographers’ perception about AI’s potential to expedite examinations could lead to a reduction on the interaction with patients, driven by higher workload and promoting impersonalised healthcare within the profession. This workload, which is already present in the departments, intimidates radiographers who fear that it will increase even more, leading to burnout or to quit the job [
34]. In addition, the fear that less qualified people will be hired was highlighted, devaluing the level of radiographers’ profession, for both technical and human competences and skills. These concerns emphasise the importance of ongoing discussion and collaboration among stakeholders, including radiographers, physicians, educators and policymakers. This collective effort will be essential in harnessing AI’s potential to elevate clinical practice, ensuring patient-centred care, and navigating in the evolution of healthcare landscape.
4.4. Internal Consistency
The assessment of the internal consistency of this survey was low, according to According to Tavakol & Dennick (2011) [
35], an insufficient number of questions, inadequate inter-item correlations or the presence of heterogeneous constructs can potentially have an impact on Cronbach’s alpha coefficient. In addition, the translation of the survey resulted in responses in different languages, and some participants responded in a non-native language, which may affect the consistency of the scale. The lower score compared with the study by Rainey et al, [
14] which used the same questionnaire could be due to differences in stratification (physicians and all modalities and disciplines radiographers versus diagnostic & therapeutic radiographers) or to differences in level of training, given that in Switzerland only one region has Bachelor’s level training.
4.5. Study Limitations
Despite the valuable information it provides, this study is subject to certain limitations. The fact that the survey was conducted in several languages, while could introduce variability into the responses owing to not fully covering the country’s four official languages. Variations in response rates, particularly among physicians, could introduce biases and affect the generalisability of the results. Moreover, relying on self-reported scales has potential limitations related to respondent understanding and bias. However, the credibility of our study is enhanced by the pilot study that was conducted before dissemination, involving both radiographers and physicians from a variety of backgrounds taking into account these limitations to improve the validity of the results.
4.6. Implications for Practice and Future Research
To maximize the potential of AI in healthcare, several key recommendations emerge. Alongside, the integration of AI into the Bachelor’s curriculum and offering CPD, there is a strong emphasis on promoting interdisciplinary collaboration. This collaboration should be extended by involving radiographers, physicians, patients, and engineers. By fostering joint educational initiatives, particularly between radiographers and physicians, a deeper understanding of perspectives can be achieved, enhancing teamwork within AI-driven healthcare environments. This approach ensures a holistic implementation of AI, aligning with patient-centric care and overall healthcare improvement.
Exploring the patient perspective on AI could be a domain fully explored by future research. This exploration could shed light on patients’ perceptions and expectations of AI in healthcare, providing valuable insights into potential benefits and concerns from an end-user perspective and by applying explainable AI tools.
5. Conclusions
The impact of AI on radiographers’ profession and activities is multifaceted and presents both opportunities and challenges. The study highlights the need for comprehensive AI training to be integrated into radiography/medical radiation science education, collaboration between stakeholders to adapt to the roles that are changing, and proactive measures to address concerns around job stability, competences and skills retention. By leveraging this knowledge, radiographers can better prepare for the changing healthcare landscape driven by AI technology.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on
Preprints.org.
Author Contributions
UK Survey Conceptualization, S.T., R.K., and C.M.; Swiss survey adaptation: M.C., L.M., I.G., and S.D.; methodology, M.C., L.M.,S.G., S.D, and C.S.R; dissemination, M.C., L.M.,S.G., I.G., S.D, and C.S.R.; formal analysis, M.C., S.D., and S.G.; data curation, M.C., S.D., and S.G.; writing—original draft preparation, M.C., S.D., S.G. and C.S.R; writing—review and editing, C.S.R, C.M. and Z.S.; supervision, C.S.R., C.M., and Z.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study. Under Swiss Law, the current project/questionnaire does not fall under the regulations for research involving human subjects, and as such, does not require authorisation from any federal or cantonal ethics committee. A committee member of the Swiss Association of Research Ethics Committees gave exemption of this study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data that support the findings of this study are available from the first author, M.C. upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Davenport, T.; Kalakota, R. The potential for artificial intelligence in healthcare. Futur. Healthc. J. 2019;6:94–8. [CrossRef]
- Kulkarni, S.; Seneviratne, N.; Baig, M.S.; Khan, A.H.A. Artificial Intelligence in Medicine: Where Are We Now? Acad. Radiol. 2020;27:62–70. [CrossRef]
- Champendal, M.; Marmy, L.; Malamateniou, C.; Sá dos Reis, C. Artificial intelligence to support person-centred care in breast imaging - A scoping review. J. Med. Imaging. Radiat Sci. 2023;19. [CrossRef]
- Bitencourt, A.; Daimiel Naranjo, I.; Lo Gullo, R.; Rossi Saccarelli, C.; Pinker, K. AI-enhanced breast imaging: Where are we and where are we heading? Eur. J. Radiol. 2021;142:109882. [CrossRef]
- Pianykh, O.S.; Langs, G.; Dewey, M.; Enzmann, D.R.; Herold, C.J.; Schoenberg, S.O.; et al. Continuous Learning AI in Radiology: Implementation Principles and Early Applications. Radiology. 2020;297:6–14. [CrossRef]
- Syed, A.; Zoga, A. Artificial Intelligence in Radiology: Current Technology and Future Directions. Semin. Musculoskelet. Radiol. 2018;22:540–5. [CrossRef]
- van de Venter, R.; Skelton, E.; Matthew, J.; Woznitza, N.; Tarroni, G.; Hirani, S.P, et al. Artificial intelligence education for radiographers, an evaluation of a UK postgraduate educational intervention using participatory action research: a pilot study. Insights. Imaging. 2023;14:25. [CrossRef]
- Malamateniou, C.; Knapp, K.M.; Pergola, M.; Woznitza, N.; Hardy, M. Artificial intelligence in radiography: Where are we now and what does the future hold? Radiography. 2021;27:S58–62. [CrossRef]
- Potočnik, J.; Foley, S.; Thomas, E. Current and potential applications of artificial intelligence in medical imaging practice: A narrative review. J. Med. Imaging. Radiat. Sci. 2023;54:376–85. [CrossRef]
- Hardy, M.; Harvey, H. Artificial intelligence in diagnostic imaging: impact on the radiography profession. Br. J. Radiol. 2020;93:20190840. [CrossRef]
- Xue, H.; Hu, G.; Hong, N.; Dunnick, N.R.; Jin, Z.. How to keep artificial intelligence evolving in the medical imaging world? Challenges and opportunities. Sci. Bull. 2023;68:648–52. [CrossRef]
- Saw, S.N.; Ng, K.H. Current challenges of implementing artificial intelligence in medical imaging. Phys. Medica. 2022;100:12–7. [CrossRef]
- Coakley, S.; Young, R.; Moore, N.; England, A.; O’Mahony, A.; O’Connor, O.J.; et al. Radiographers’ knowledge, attitudes and expectations of artificial intelligence in medical imaging. Radiography. 2022;28:943–8. [CrossRef]
- Rainey, C.; O’Regan, T.; Matthew, J.; Skelton, E.; Woznitza, N.; Chu, K.Y.; et al. Beauty Is in the AI of the Beholder: Are We Ready for the Clinical Integration of Artificial Intelligence in Radiography? An Exploratory Analysis of Perceived AI Knowledge, Skills, Confidence, and Education Perspectives of UK Radiographers. Front. Digit. Heal. 2021;3. [CrossRef]
- World Health Organization. Process of translation and adaptation of instruments. WHO guidelines on translation and adaptation of instruments. Man WHO Disabil Assess Sched WHODAS 20 2022:1–8.
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006;3:77–101. [CrossRef]
- La, B. Loi fédérale relative à la recherche sur l ’ être humain 2011;2011:3215–40.
- Constitution fédérale de la Confédération suisse. 1999.
- Jeanrenaud, P.C. Ode de rémunération des médecins et coûts de la santé en 2003:1–18.
- Huisman, M.; Ranschaert, E.; Parker, W.; Mastrodicasa, D.; Koci, M.; Pinto de Santos, D.; et al. An international survey on AI in radiology in 1,041 radiologists and radiology residents part 1: fear of replacement, knowledge, and attitude. Eur. Radiol. 2021;31:7058–66. [CrossRef]
- Chen, Y.; Stavropoulou, C.; Narasinkan, R.; Baker, A.; Scarbrough, H. Professionals’ responses to the introduction of AI innovations in radiology and their implications for future adoption: a qualitative study. BMC. Health. Serv. Res. 2021;21:1–9. [CrossRef]
- Alexander, R.; Waite, S.; Bruno, M.A.; Krupinski, E.A.; Berlin, L; Macknik, S.; et al. Mandating Limits on Workload, Duty, and Speed in Radiology. Radiology. 2022;304:274–82. [CrossRef]
- Alelyani, M.; Alamri, S.; Alqahtani, M.S.; Musa, A.; Almater, H.; Alqahtani, N.; et al. Radiology community attitude in saudi arabia about the applications of artificial intelligence in radiology. Healthc. 2021;9:1–10. [CrossRef]
- Akudjedu, T.N.; Torre, S.; Khine, R.; Katsifarakis, D.; Newman, D.; Malamateniou, C. Knowledge, perceptions, and expectations of Artificial intelligence in radiography practice: A global radiography workforce survey. J. Med. Imaging. Radiat. Sci. 2022. [CrossRef]
- Botwe, B.O. ; Akudjedu, T.N. ; Antwi, W.K. ; Rockson, P. ; Mkoloma, S.S. ; Balogun, E.O. ; et al. The integration of artificial intelligence in medical imaging practice: Perspectives of African radiographers. Radiography. 2021;27:861–6. [CrossRef]
- Ng, C.T. ; Roslan, S.N.A. ; Chng, Y.H. ; Choong, D.A.W. ; Chong, A.J.L. ; Tay, Y.X. ; et al. Singapore radiographers’ perceptions and expectations of artificial intelligence - A qualitative study. J. Med. Imaging. Radiat. Sci. 2022;53:554–63. [CrossRef]
- Botwe,, B.O. ; Antwi, W.K. ; Arkoh, S. ; Akudjedu, T.N. Radiographers’ perspectives on the emerging integration of artificial intelligence into diagnostic imaging: The Ghana study. J. Med. Radiat. Sci. 2021;68:260–8. [CrossRef]
- Ryan, M.L. ; O’Donovan, T. ; McNulty, J.P. Artificial intelligence: The opinions of radiographers and radiation therapists in Ireland. Radiography. 2021;27:S74–82. [CrossRef]
- Currie, G. ; Nelson, T. ; Hewis, J. ; Chandler, A. ; Spuur, K. ; Nabasenja, C. ; et al. Australian perspectives on artificial intelligence in medical imaging. J. Med. Radiat. Sci. 2022;69:282–92. [CrossRef]
- Malamateniou, C.; McFadden, S.; McQuinlan, Y.; England, A.; Woznitza, N.; Goldsworthy, S.; et al. Artificial Intelligence: Guidance for clinical imaging and therapeutic radiography professionals, a summary by the Society of Radiographers AI working group. Radiography. 2021;27:1192–202. [CrossRef]
- Woznitza, N., International Society of Radiographers, The European Federation of Radiographer Societies. Artificial Intelligence and the Radiographer/Radiological Technologist Profession: A joint statement of the International Society of Radiographers and Radiological Technologists and the European Federation of Radiographer Societies. Radiography. 2020;26:93–5. [CrossRef]
- Chamunyonga, C.; Edwards, C.; Caldwell, P.; Rutledge, P.; Burbery, J. The Impact of Artificial Intelligence and Machine Learning in Radiation Therapy: Considerations for Future Curriculum Enhancement. J. Med. Imaging. Radiat. Sci. 2020;51:214–20. [CrossRef]
- European Federation of Radiographers Societies. RERP - Radiographer Education, Research, and Practice: 2021–2031. 2021.
- de Labouchere, S.; Metsälä, E.; Jorge, J. Radiographers ’ perceived workload and its association to work well-being factors in Western Switzerland 2020.
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011;2:53–5. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).