1. Introduction
In humans, oxygen plays an important role in providing energy and maintaining life and function [
1]. Oxygen in the blood is divided into combined and dissolved oxygen. Since oxygen has low solubility at atmospheric pressure, most of the oxygen during respiration is combined with hemoglobin in the blood to become bound oxygen, and the remaining oxygen is released into the air through gas exchange or dissolved in plasma (dissolved oxygen) [
2]. In general, combined oxygen that is larger than dissolved oxygen passes smoothly through capillaries to each organ and cell that requires it. When blood vessels are abnormally narrowed due to unhealthy diet, smoking, drinking, obesity, etc., or when blood obesity increases due to diabetes or hyperlipidemia, the bound oxygen combined with hemoglobin cannot pass through capillaries. A variety of diseases and defects are associated with a lack of oxygen supply (hypoxia), which can lead to severe disability and even death [
3].
The first report on the therapeutic use of hyperbaric oxygen therapy (HBOT) was published in 1879 by Fontaine, a French surgeon who believed that pressurized oxygen chambers could help with anesthesia [
4]. HBOT is used to treat patients by supplying 100% oxygen at more than twice the atmospheric pressure. This therapy is commonly applied to treat cesarean disease, gas poisoning, wounds, and burns. It is known to be effective in decompression sickness (DCS), carbon monoxide (CO) poisonings, diabetic foot, etc. Research on indications is being actively conducted [
5,
6]. Also, the Undersea and Hyperbaric Medicine Society (UHMS) in the United States provides guidelines and recommendations for the use of HBOT in various medical conditions. For clinical efficacy, it was specified that the pressure must be greater than or equal to 1.4 atmosphere absolute (ATA), and in clinical practice, pressures applied usually range from 2.0 to 3.0 ATA [
7]. CO is a common worldwide poison and, thus, treatment options are an important subject for global health [
8]. CO poisonings vary from 14 to perhaps 160/100,000 people annually, with higher incidence in some developing countries [
9]. Intentional poisonings account for the majority of deaths, which are due to the cardiac insult arising from hypoxic stress mediated by carboxyhaemoglobin (COHb) and mitochondrial dysfunction [
10]. Accidental exposures represent the majority of non-fatal poisonings, and in the United States, it costs over
$1 billion annually for direct hospital care and lost earnings [
11]. Morbidity is related to neurological injuries. cognitive, vestibular and motor impairments occur in ~25–50% of survivors from severe poisoning [
12]. Sethuraman and Thom presented that HBOT at a dose of 2.5–3.0 atmospheres absolute (ATA) is a necessary treatment for acute CO poisoning with appropriate consideration for pathology and therapeutic mechanisms [
13].
Hyperbaric chambers are used in high-pressure environments where a pressure of at least two or more times atmospheric pressure is set and maintained. It is treated for 45 to 300 minutes in a pressurized environment with 1 atm or 2 atm pressure depending on the purpose or severity. According to recent studies on the indications of HBOT, it is expected to have positive effects in the treatment of hypoxia, oxidative stress, inflammation-induced brain damage, congenital cerebral palsy, stroke, autism, Alzheimer's disease, Parkinson's syndrome, and chronic Lyme disease, and cancers [
14]. Although no clear evidence for the effects and mechanism of HBOT on the treatment of intractable diseases has been discovered, it has shown favorable results in many clinical cases. According to the number of users, it was classified into monoplace and multiplace chamber [
15]. Monoplace chamber delivers oxygen to the patient's tissues through breathing, and multiplace chamber delivers oxygen to the patient's tissues through a breathing aid such as a mask. In the case of a monoplace chamber, gas monitoring inside the hyperbaric chamber is important because oxygen is consumed and carbon dioxide is increased because treatment is performed in a closed volume. Values may vary slightly depending on where the oxygen and carbon dioxide concentrations are measured in the hyperbaric chamber. In general, 100% oxygen is supplied during HBOT, but the oxygen concentration in the hyperbaric chamber may not be constant because a difference in oxygen partial pressure may occur according to a pressure change. The goal is to increase the effectiveness of HBOT by measuring the concentration change of these internal gases and supplying low carbon and high oxygen to the patient. In addition, the temperature and humidity are fluctuated together according to the change in pressure in the closed treatment device, and when the pressure rises, the temperature and humidity also rise together. It is important to measure the changing pressure and maintain the temperature and humidity according to the pressure change in order to provide the optimal treatment environment to the patient and to become an accurate HBOT.
According to the current status of hyperbaric chamber deployment investigated by the Korean Academy of Undersea and Hyperbaric Medicine, the number of medical institutions capable of HBOT in Korea increased from 21 to 50 in 2021 compared to the first survey in 2017. The details of number of medical institutions capable of HBOT increased from 8 to 13 for tertiary general hospitals, from 3 to 17 for general hospitals, and from 10 to 20 for hospitals and other medical institutions. The number of multiplace hyperbaric chambers increased from 12 to 30, and the number of monoplace hyperbaric chambers increased from 13 to 43 [
16].
However, to the best of our knowledge, there has been no study that has verified safety and effectiveness through evaluation of the pressure, oxygen concentration, etc. of a monoplace hyperbaric chamber during HBOT. This study aims to develop a gas monitoring system for safety evaluation of the monoplace hyperbaric chamber. In addition, it examined the clinical characteristics of the patients diagnosed with CO poisoning who performed HBOT using a monoplace hyperbaric chamber.
2. Materials and Methods
2.1. Monoplace Hyperbaric Chamber and Ethical Approval
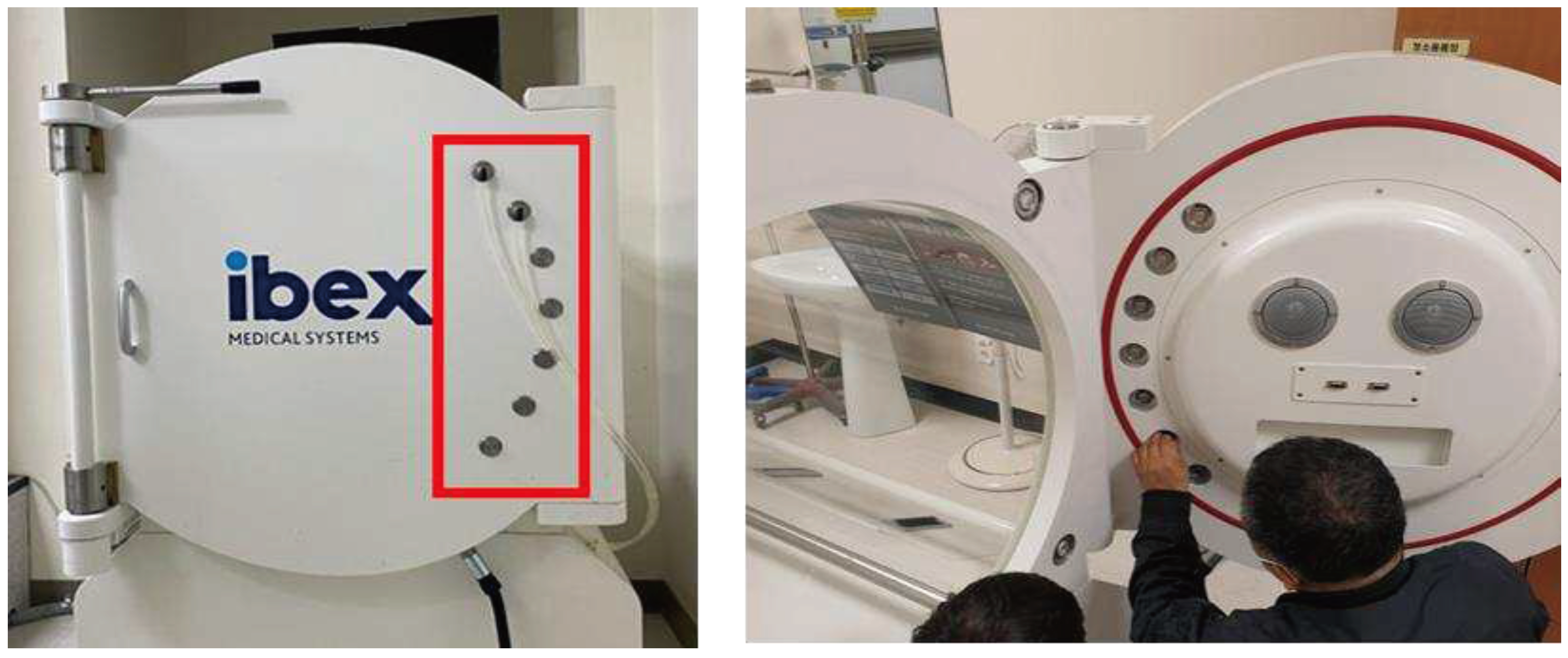
IBEX M2 (IBEX Medical systems, Wonju, Republic of Korea) was a newly developed and recently commercialized monoplace hyperbaric chamber as a medical device for testing (
Figure 1). It was applied the automatic control system including the anti-barotrauma technology. This study was approved by the Institutional Review Board of Wonju Christian Hospital (IRB Approval No. CR320074).
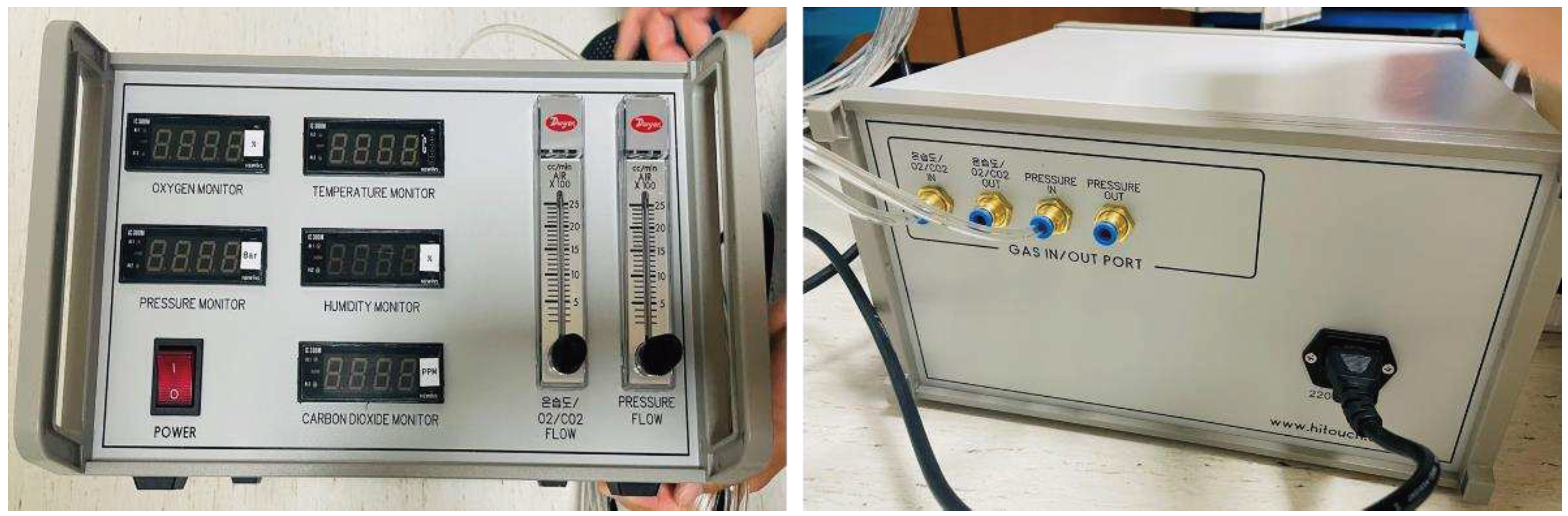
2.2. Development of the Gas Monitoring System and Its Connection to the Chamber
A sensor kit was developed by selecting a data recorder and a transmitter. The O2H-9903SD (LT Lutron Electronic Enterprise Co. Ltd., Taiwan) is the data recorder that was capable of O
2, Humidity, and Temperature detection into the SD memory card. Also, the CD-100 (ELT SENSOR Corp., Republic of Korea) is the one-board type transmitter that was capable of measuring CO
2 concentration (
Figure 2). The developed gas monitoring system was connected with a hose after installing a penetrator on the door side of the monoplace hyperbaric chamber. (
Figure 3).
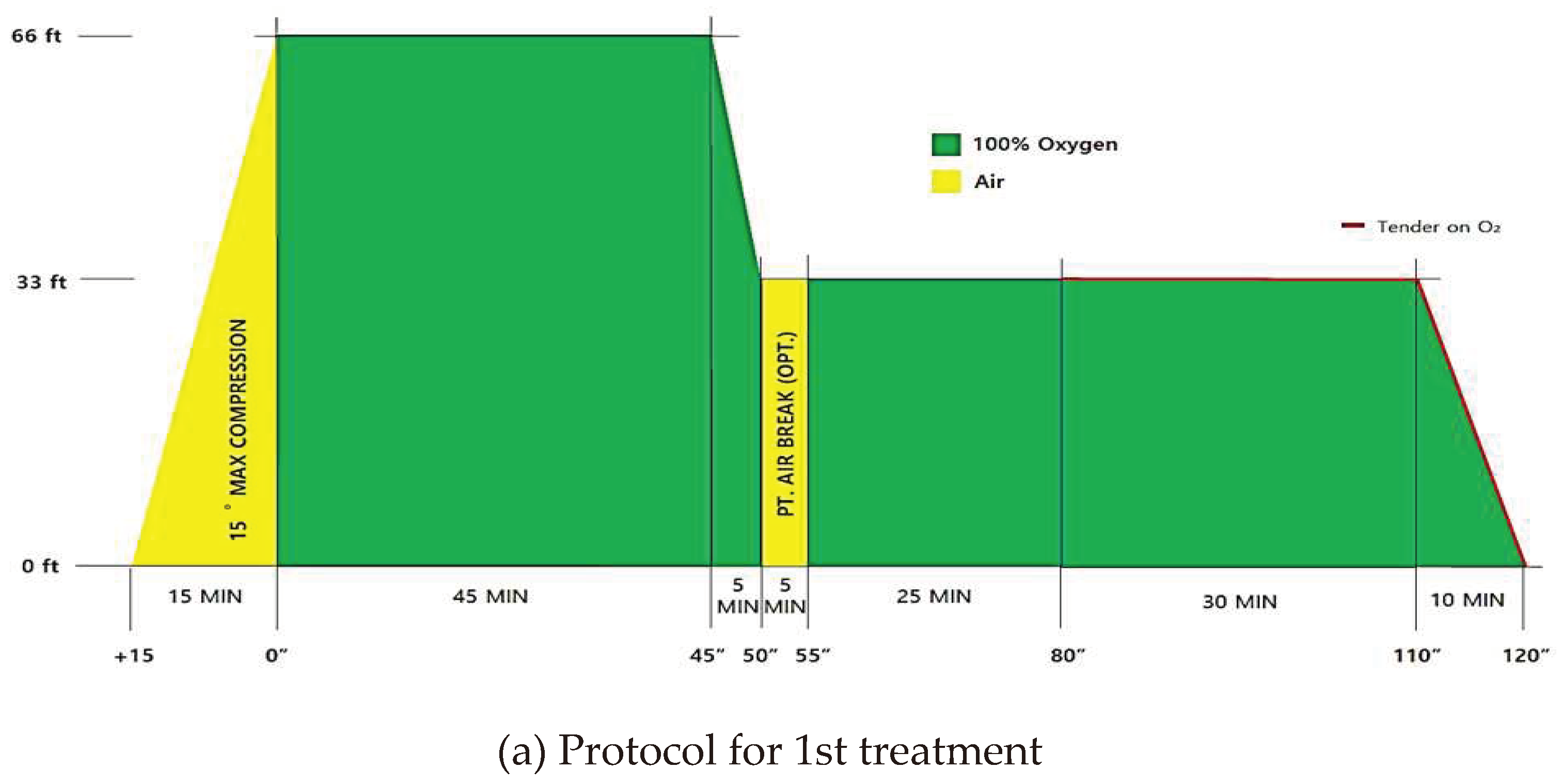
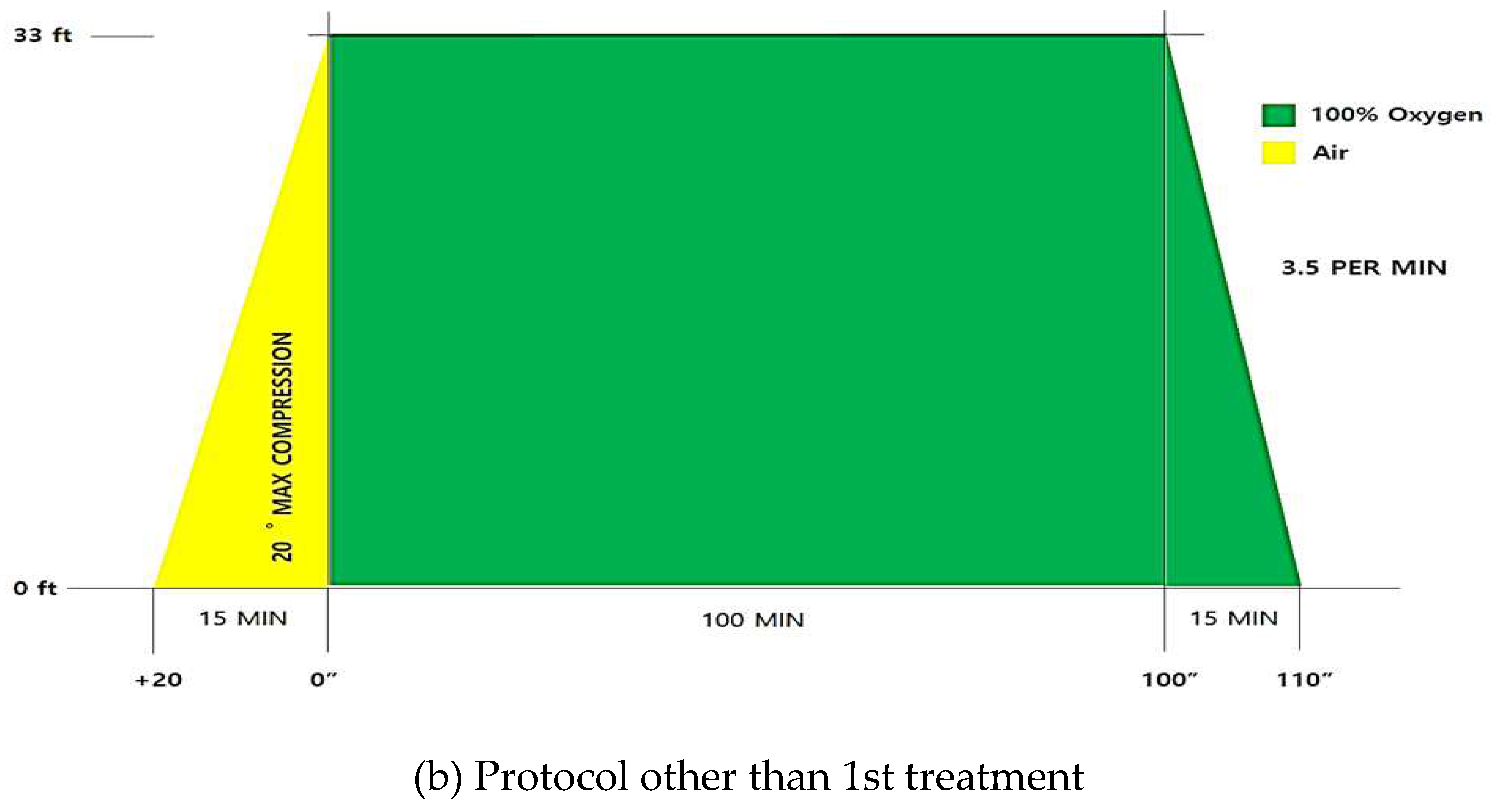
2.3. Pressure Value Settings Which Are Mostly Used in Hospital HBOT Protocols for the Safety and Effectiveness Evaluation of Monoplace Hyperbaric Chamber
The main symptoms and signs that require HBOT for CO poisoning are ECG abnormal findings, metabolic acidosis, abnormal blood test findings, when pregnancy is suspected, chest pain, coma, disorientation, personality change, and consciousness change. During the first HBOT session, initial compression was performed to 2.8 ATA for 45 minutes, followed by 2.0 ATA for 60 minutes [
17]. Similar to what Thom et al. reported,
Figure 4 showed the treatment protocol for acute CO poisoning in the HBOT center of Wonju Severance Christian Hospital. The 1st treatment was performed using both 3.0 ATA and 2.0 ATA for a total of 135 minutes. Before starting HBOT session, it was prepared for max compression for 15 minutes and then performed initial compression for 45 minutes to 3.0 ATA. Then, the pressure was reduced from 3.0 ATA to 2.0 ATA for 5 minutes, and air break was maintained for 5 minutes. Next, it was followed by 2 ATA for 55 minutes and ended with depressurization for 10 minutes. Other than the 1st treatment was performed using 2.0 ATA for a total of 110 minutes. Before starting HBOT session, it was prepared for max compression for 20 minutes and then performed initial compression for 100 minutes to 2.0 ATA. After that, it was decompressed for 15 minutes (
Figure 2). According to HBOT protocol for acute CO poisoning, the measured values between the hyperbaric chamber and the gas monitoring system were compared at two pressure conditions, 3.0 ATA and 2.0 ATA.
2.4. Study Design
When the monoplace hyperbaric chamber was operated at 3.0 ATA and 2.0 ATA, the values of oxygen, carbon dioxide, humidity, and temperature were measured in the chamber and gas monitoring system, respectively. In 2.0 ATA, the subject entered the chamber, but in 3.0 ATA, the subject did not enter the chamber to prevent a situation in which the subject could be in danger due to high pressure. The data has measured a total of three times during the chamber operating at 10 minutes, 20 minutes, and 30 minutes after pressurization, and this sequence was repeated five times. Finally, after improving the function of the chamber based on the measured data, the test was performed again in the same process.
Also, the CO poisoning registry data used in this study were derived from a cohort at a single tertiary academic hospital. The HBOT records which was stored in the monoplace hyperbaric chamber and medical records were retrospectively analyzed for patients with CO poisoning. Clinical variables were evaluated in patients with CO poisoning as follows: age, sex, vital signs (systolic blood pressure, diastolic blood pressure, pulse rate, respiratory rate, and body temperature), CO source (charcoal, gas and oil, fire, or drug co-ingestion), maximal CO exposure time, time from rescue to ER arrival, Glasgow coma scale (GCS) at the time of rescue or ER arrival, comorbidities (diabetes mellitus, hypertension, dyslipidaemia, lung diseases, cardiovascular disorder, liver diseases, kidney diseases, stroke, cancer, or psychiatric diseases), and any interval of loss of consciousness, shock, seizure.
2.5. Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics Version 25.0 (IBM Corp., Armonk, NY, USA). In this study, the values measured in the monoplace hyperbaric chamber and a gas monitoring system were compared. Comparisons among the measured data were expressed as means with the standard deviations for continuous variables. Differences were assessed using the independent t-test or Mann-Whitney U test for continuous variables and the χ2 test or Fisher exact test for categorical variables. It was interpreted as statistically significant when the p-value was less than 0.05.
3. Results
3.1. Comparison between the Monoplace Hyperbaric Chamber and a Gas Monitoring System
In the air pressure condition at 3.0 ATA, the average carbon dioxide was higher in the hyperbaric chamber than in the gas monitoring system (447.22±7.85 PPM vs. 137.56±43.7 PPM, p<0.001). Also, the average humidity was higher in the hyperbaric chamber than in the gas monitoring system (22.69±13.14 % vs. 5.60±3.93 %, p=0.004). In the air pressure condition at 2.0 ATA, the average humidity was higher in the hyperbaric chamber than in the gas monitoring system (40.52±14.13 % vs. 12.79±7.31 %, p<0.001). Also, the average temperature was lower in the hyperbaric chamber than in the gas monitoring system (24.30±0.99 ℃ vs. 27.80±0.54 ℃, p<0.001) (
Table 1).
3.2. Clinical Characteristics of CO Poisoning Patients Who Treated with HBOT
1,006 patients with CO poisoning who performed HBOT were included in this study. The mean age of the patients who received HBOT was 44.93±19.78 years. According to the source of CO, 680 patients (67.6%) visited ER most commonly due to charcoal. The median maximal CO exposure time and time from rescue to ER were 4.0 hours [1.0-8.0] and 3.09 hours [1.37-5.47], respectively. The median GCS score at the scene or ER was 15. According to the underlying comorbidities, psychiatric diseases (19.5%) were the most common, followed by hypertension (18.1%) and diabetes mellitus (11.5%). In the emergency room, some patients had appeared symptoms such as loss of consciousness (59.8%), shock (6.7%), or seizure (8.3%) (
Table 2).
4. Discussion
4.1. Differences in Actual Pressure and Gas Concentration between Monoplace Hyperbaric Chamber and Gas Monitoring System
The safety evaluation of hyperbaric chambers for the treatment of CO poisoning has been a topic of ongoing discussion in the medical community. The difference in measured values between the hyperbaric oxygen chamber and gas monitoring system at 3.0 ATA and 2.0 ATA could be caused by a variety of factors. First, the difference in measured values could be caused by the pressure differences. The hyperbaric chamber was designed to operate at higher pressures than normal atmospheric pressure. Under the condition at 3.0 ATA, the increased pressure could cause the concentration of CO
2 to increase as the air became more saturated with CO
2. This would be explained by the higher CO
2 readings in the hyperbaric chamber compared to the gas monitoring system [
18]. On the other hand, under the condition at 2.0 ATA, the pressure was lower than 3.0 ATA, and the opposite effect might occur. Similarly, a study by Ay et al. found that increased pressure in hyperbaric chambers could lead to increased levels of humidity due to reduced ventilation and moisture from medical gases [
19]. Second, the difference in measured values could be caused by the ventilation differences. The hyperbaric chamber might have different ventilation settings than the gas monitoring system. At 3.0 ATA, the lower ventilation rate in the hyperbaric chamber might allow CO
2 to build up, which could contribute to the higher CO
2 readings. Similarly, the higher humidity readings might be due to a lower ventilation rate and the use of medical gases that could introduce moisture into the chamber. Lastly, the difference in measured values could be caused by the temperature differences. The hyperbaric chamber might be at a different temperature than the gas monitoring system, which could affect the readings of humidity and temperature. At 2.0 ATA, the lower average temperature readings in the hyperbaric chamber might be due to the lower ambient temperature in the chamber [
20].
4.2. Clinical Characteristics of CO Poisoning Patients Who Treated with HBOT
Additionally, the clinical characteristics of patients with CO poisoning can greatly impact the effectiveness of HBOT. The severity and duration of exposure, as well as the patient's overall health status, can play a significant role in determining the outcome of treatment. It is important for healthcare providers to consider these factors when deciding whether to use HBOT as a treatment option for CO poisoning. In this study, several comorbidities that might affect the outcomes of patients with CO poisoning were presented. According to the underlying comorbidities, psychiatric diseases were the most common, followed by hypertension and diabetes mellitus. Patients with psychiatric diseases might be at increased risk for CO poisoning due to impaired judgment, substance abuse, or living in suboptimal environments with poor ventilation. In addition, CO poisoning could cause neurological and psychiatric symptoms, which may exacerbate pre-existing mental illness or lead to new onset psychiatric disorders [
21]. Hypertension had been associated with increased susceptibility to CO poisoning and worse outcomes in CO poisoning patients, possibly due to increased vulnerability of blood vessels and tissues to hypoxia [
22]. Patients with diabetes mellitus might be at increased risk for CO poisoning and worse outcomes due to microvascular and macrovascular complications of diabetes, which could affect blood flow and oxygenation in tissues [
23].
5. Conclusions
In this study, it was developed a gas monitoring system and validated to evaluate the mechanical safety and effectiveness of a monoplace hyperbaric chamber. By developing a gas monitoring system and installing a penetrator for sensing on the chamber door, it was possible to measure more accurate values than the existing measurement method. In addition, it was confirmed that there were no problems by analyzing data from the monoplace hyperbaric chamber equipped with the developed gas monitoring system actually used to treat patients with carbon monoxide poisoning.
In conclusion, the safety evaluation of hyperbaric chambers and the clinical characteristics of patients with CO poisoning are crucial considerations in the management of CO poisoning. Based on the results of this study, it is possible to measure the gas concentration at the door in the direction of the head where the patient breathes, making it possible to analyze the gas at the position where breathing actually takes place. In the future, it can be expected that HBOT can be effectively performed by monitoring the gas concentration change inside the hyperbaric chamber.
Funding
This work was supported by the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Evergy, the Ministry of Health & Welfare, Republic of Korea, the Ministry of Food and Drug Safety) (Project Number: RS-2020-KD000247).
Institutional Review Board Statement
This study was conducted following approval from the research ethics committee of Wonju Severance Christian Hospital, Yonsei University (IRB Approval No.: CR320074).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets analyzed during the current study are not yet publicly available but are available from the corresponding author on reasonable request.
Acknowledgments
We thanks to thank the medical staff (doctors, nurses, and emergency medical technicians) who treated patients with CO poisoning and collected data at the Hyperbaric Oxygen Treatment Center at Wonju Severance Christian Hospital.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Clauss, W.; Clauss, C. Humanbiologie Kompakt, 2nd ed. Springer Spektrum: Berlin/Heidelberg, Germany, 2018.
- Widmaier, E.; Raff, H..; Strang, K.T. Vander's human physiology, McGraw-Hill US Higher Ed USE, 2022.
- Jain, K.K. Textbook of Hyperbaric Medicine, 6th ed. Springer International Publishing: Basel, Switzerland, 2017.
- Ii, J.H.J., Morsch, J.H., Rendell-Baker, L. The historical perspective of hyperbaric therapy. Ann N Y Acad Sci. 1965, 117(2), 651–670. [CrossRef]
- Leach, R.M.; Rees, P.J.; Wilmshurst, P. Hyperbaric oxygen therapy. BMJ. 1998, 317(7166), 1140–11433. [Google Scholar] [CrossRef] [PubMed]
- Tibbles, P.M.; Edelsberg, J.S. Hyperbaric-oxygen therapy. New England Journal of Medicine 1996, 334(25), 1642–1648. [Google Scholar] [CrossRef] [PubMed]
- Undersea and Hyperbaric Medical Society. Indications for hyperbaric oxygen therapy. https://www.uhms.org/resources/hbo-indications.html. Last accessed January 25, 2017.
- Raub, J.A.; Mathieu-Nolf, M.; Hampson, N.B.; Thom, S.R. Carbon monoxide poisoning—a public health perspective. Toxicology 2000, 145(1), 1–14. [Google Scholar] [CrossRef] [PubMed]
- Mattiuzzi, C.; Lippi, G. Worldwide epidemiology of carbon monoxide poisoning. Hum Exp Toxicol. 2020, 39(4), 387–392. [Google Scholar] [CrossRef] [PubMed]
- Rose, J.J.; Wang, L.; Xu, Q.; McTiernan, C.F.; Shiva, S.; Tejero, J.; Gladwin, M.T. Carbon monoxide poisoning: pathogenesis, management, and future directions of therapy. Am J Respir Crit Care Med 2017, 195(5), 596–606. [Google Scholar] [CrossRef] [PubMed]
- Hampson, N.B. U.S. mortality due to carbon monoxide poisoning, 1999–2014: accidental and intentional deaths. Ann Am Thorac Soc. 2016, 13(10), 1768–1774. [Google Scholar] [CrossRef] [PubMed]
- Hampson, N.B.; Piantadosi, C.A.; Thom, S.R.; Weaver, L.K. Practice recommendations in the diagnosis, management and prevention of carbon monoxide poisoning. Am J Respir Crit Care Med. 2012, 186(11), 1095–1101. [Google Scholar] [CrossRef] [PubMed]
- Sethuraman, K.; Thom, S.R. Hyperbaric oxygen should be used for carbon monoxide poisoning. Br J Clin Pharmacol. 2022, 89(3), 939–941. [Google Scholar] [CrossRef] [PubMed]
- Al-Waili, N.S.; Butler, G.J.; Beale, J.; Abdullah, M.S.; Hamilton, R.B.; Lee, B.Y.; Lucas, P.; Allen, M.W.; Petrillo, R.L.; Carrey, Z.; Finkelstein, M. Hyperbaric oxygen in the treatment of patients with cerebral stroke, brain trauma, and neurologic disease. Advances in therapy 2005, 22, 659–678. [Google Scholar] [CrossRef] [PubMed]
- Mayer, R., Hamilton-Farrell, M.R., van der Kleij, A.J., Schmutz, J., Granström, G., Sicko, Z., ... & Ditri, L. Hyperbaric oxygen and radiotherapy. Strahlentherapie und Onkologie. 2005, 181(2), 113. [CrossRef]
- Lee, S.M.; Heo, T.; Kim, G.W.; Kim, H. Current status and development direction of hyperbaric medicine in Korea. J Korean Med Assoc. 2022, 65(4), 232–238. [Google Scholar] [CrossRef]
- Thom, S.R; Taber, R.L.; Mendiguren, I.I.; Clark, J.M.; Hardy, K.R.; Fisher, A.B. Delayed neuropsychologic sequelae after carbon monoxide poisoning: prevention by treatment with hyperbaric oxygen. Ann Emerg Med. 1995, 25(4), 474–480. [Google Scholar] [CrossRef]
- Weaver, L.K. Hyperbaric oxygen therapy for carbon monoxide poisoning. Undersea Hyperb Med. 2014, 41(4), 339–354. [Google Scholar]
- Ay, H.; Salihoglu, M.; Altundag, A.; Tekeli, H.; Memis, A.; Cayonu, M. The effect of hyperbaric conditions on olfactory functions. Undersea Hyperb Med 2014, 41(3), 203–207. [Google Scholar]
- American Society of Heating Refrigerating and Air-Conditioning Engineers. 2017 Ashrae Handbook. Fundamentals. Inch-pound ed. Atlanta GA: ASHRAE 2017; 2017.
- Helffenstein, D.A. Neuropsychological evaluation of the carbon monoxide-poisoned patient. Carbon monoxide toxicity. CRC Press, 2000. 459-482.
- Shank, E.S.; Muth, C.M. Decompression illness, iatrogenic gas embolism, and carbon monoxide poisoning: the role of hyperbaric oxygen therapy. Int Anesthesiol Clin 2000, 38(1), 111–138. [Google Scholar] [CrossRef] [PubMed]
- White, S.R. 11 Update on the Clinical Treatment of Carbon Monoxide Poisoning. Carbon Monoxide Toxicity, 2000, 261-290.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).