1. Introduction
Kümmell 's disease is a relatively rare disease that was first reported by Hermann Kümmell 's in 1895 [
1]. It is also known as post-traumatic vertebral osteonecrosis, which is characterized by vertebral avascular necrosis, dynamic instability, and progressive kyphosis with prolonged back pain or neurological deficits following an asymptomatic or mild period [
2,
3].
Percutaneous kyphoplasty (PKP) is a highly successful treatment option for Kümmell's disease (KD), offering several advantages such as rapid pain relief, vertebral height restoration, and minimal invasiveness [
4,
5]. Due to the fibrocartilaginous repair membrane formed around the vertebral body resulting from the failed healing of the intravertebral cleft (IVC) and its surrounding tissues [
6,
7], patients with Kümmell's disease (KD) undergoing percutaneous kyphoplasty (PKP) are susceptible to complications such as bone cement displacement, adjacent vertebral refracture,bone cement leakage [
8,
9,
10]. Many studies have proven that pre-existing bone fragility in osteoporotic patients, increased stiffness and strength in the treated vertebral body, as well as improved mobility may be the risk factors of adjacent vertebral refracture [
11,
12]. However, the exact mechanism and preferred treatment of adjacent vertebral refracture caused by premature bone cement displacement in Kümmell's disease (KD) patients remains controversial. We observed that premature bone cement displacement in Kümmell's disease patients can lead to adjacent vertebral fracture, and only a few reports on this matter have been published. We report a rare case of adjacent vertebra fracture caused by premature bone cement displacement within 3 days of surgery, which helps clinical doctors comprehend this complication’s pathophysiology and take necessary precautions to improve the safety and efficacy of surgery.
2. Case report
2.1. Medical History
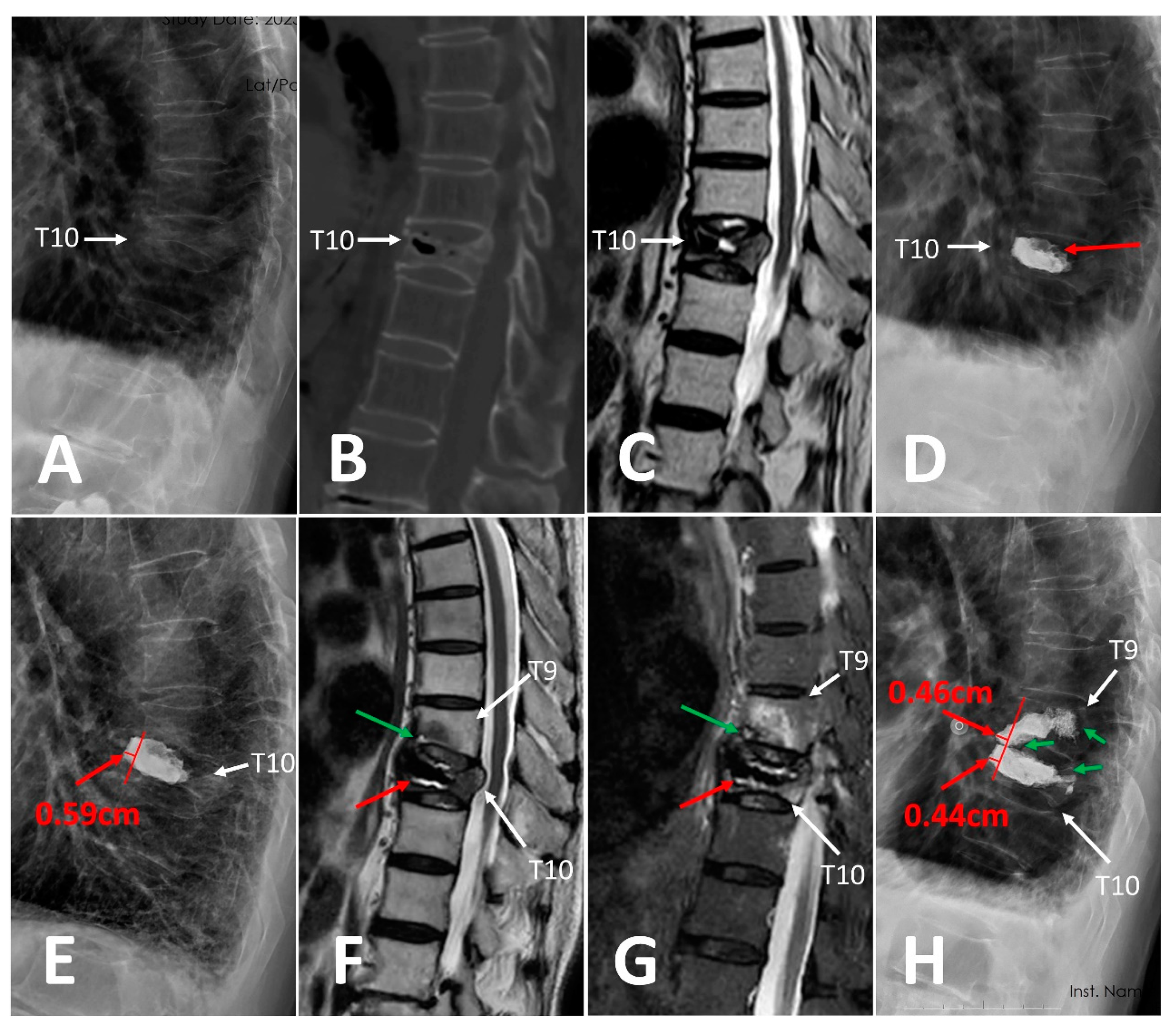
An eighty-year-old man experienced mild back pain after a fall six months ago. Physical examination revealed tenderness over the T10 spinous process and no neurological deficits. The patient's medical history includes a 20-year history of rheumatoid arthritis, with disease control achieved through the long-term use of prednisone acetate tablets. X-ray indicated de-creased height of T10 vertebral body (
Figure 1A). Sagittal CT scan showed T10 vertebra compression fracture with intervertebral vacuum cleft (
Figure 1B). Sagittal T2-weighted im-ages depicted acute vertebral compression fracture with an intravertebral vacuum cleft filled with fluid (
Figure 1C). Bone mineral density measurements confirmed severe osteoporosis (with a T sore of -4.5). It finally turns out to be the osteoporotic vertebral compression fracture with vertebral osteonecrosis of the T10 vertebra, then we performed PKP for him. The patient's back pain was relieved immediately after surgery. Postoperative X-ray showed resto-ration of vertebral height and blocky pattern of bone cement (
Figure 1D). After receiving systemic anti-osteoporosis therapy, the patient was discharged with brace protection on the second day after surgery.
On the third day of surgery, the patient presented again with back pain after bending over. Physical examination revealed tenderness over the T9 and T10 spinous process and no neurological deficits. X-ray showed T9 compression fracture and bone cement displacement of T10 (
Figure 1E). Sagittal T2-weighted images (
Figure 1F) and STIR MR sequences (
Figure 1G) revealed bone marrow edema in the T9 and T10 vertebrae, particularly at the site where the lower endplate of T9 met the displaced bone cement (green arrow in
Figure 1F, G). To prevent further bone cement displacement and remove the instability, we implemented percutaneous kyphoplasty with multi-point anchoring technique (A-PKP).
2.2. Percutaneous kyphoplasty (PKP) for the T10 vertebra
The first surgery was performed on the T10 vertebra using percutaneous kyphoplasty (PKP). After the puncture needle was advanced into the IVC of fractured vertebra through right unilateral transpedicular approach, a total of 5 mL of polymethyl methacrylate (PMMA) in late stage of wire drawing was then slowly injected through the needle to completely fill vacuum cleft. Unfortunately, there was a leakage of bone cement into the upper disc.
2.3. Percutaneous Kyphoplasty with Multi-point Anchoring Technique (A-PKP) for the T10 and T9 Vertebrae
The second surgery was performed on the T9 and T10 vertebrae subsequently using percutaneous kyphoplasty with multi-point anchoring technique (A-PKP). The surgery of T9 was performed firstly. Choosing the puncture point 3mm laterally at 10 o’clock on the left pedicle. The bone cement was prepared into late-phase filiform shape and slowly infused through the defect of lower endplate of T9 vertebra to anchor at the displaced bone cement of T10. Then, an early-phase filiform shape and penetrated to trabecular bone to anchor at the previous mass cement of T9.
For the T10 vertebra, after the balloon inflated to restore the height of the vertebral body, a curved-tipped guide needle was placed through work cannula to the residual IVC of the posterior of the displaced bone cement. Then, controlling the curved-tipped guide needle to move up and down, which can destroy fibrocartilaginous membrane of IVC and allow bone cement penetrate freely into the trabecular bones. Early-phase filiform shaped bone cement was slowly infused to penetrate into trabecular bones and anchor at the displaced bone cement. Finally, the infused bone cement into two vertebrae distributed satisfactorily and formed a pattern of multi-point anchoring around the displaced bone cement.
2.4. Surgical Outcomes of Percutaneous Kyphoplasty with Multi-point Anchoring Tech-nique (A-PKP)
Postoperatively, the patient experienced prompt relief from back pain. X-ray showed the height of T9 and T10 restored, the displaced bone cement improved, the infused bone cement into two vertebrae distributed satisfactorily and formed a pattern of multi-point anchoring at the displaced bone cement. (
Figure 1H).
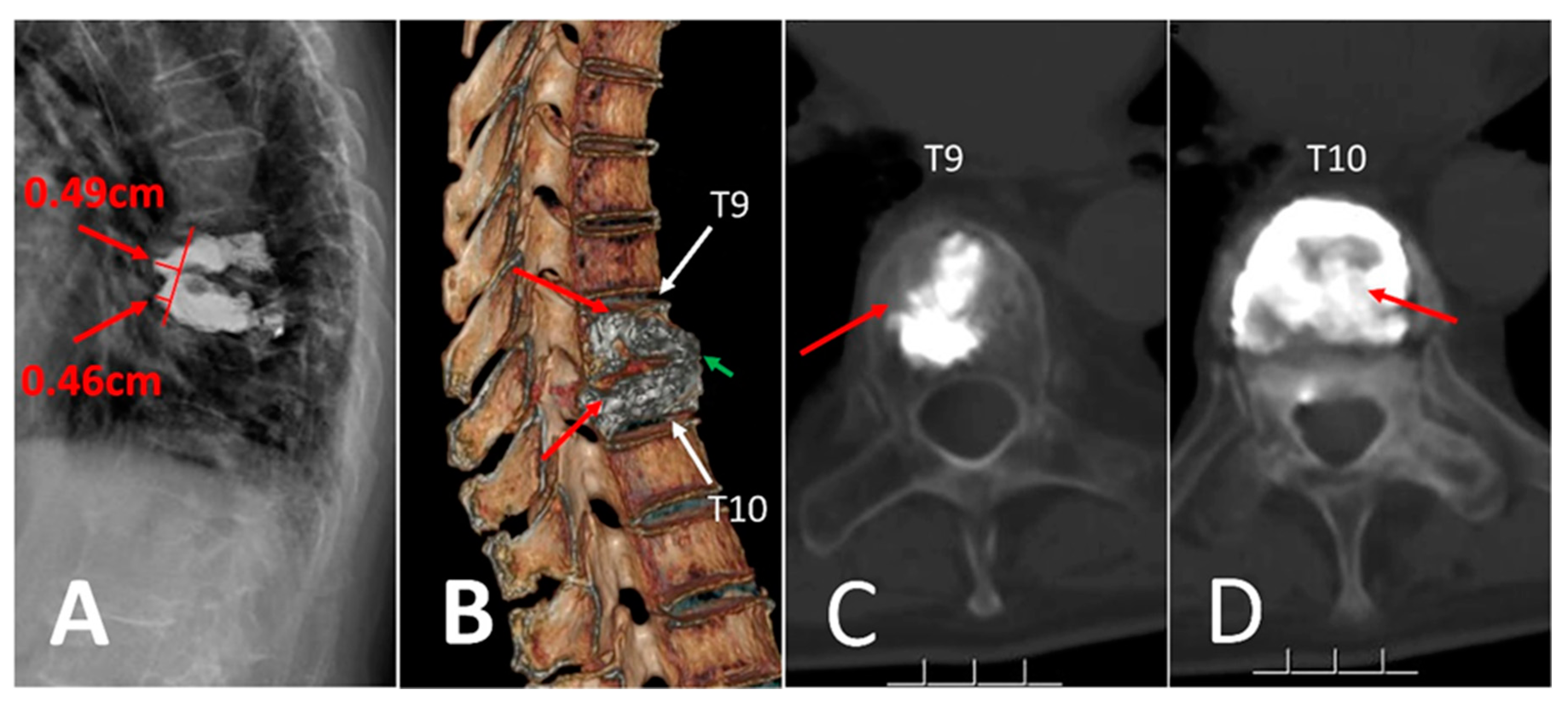
During a 10-month postoperative follow-up, the patient reported pain relief. X-ray (
Figure 2A) and three-dimensional CT (
Figure 2B) scan revealed no obvious progress of bone cement displacement and mild collapse of vertebrae. The later infused bone cement of two vertebrae still anchored at the previous bone cement tightly (
Figure 2C,D).
3. Discussion
3.1. Potential Reasons of Premature Bone Cement Displacement
Percutaneous Kyphoplasty is an effective treatment for the I and II stage of Kümmell 's disease [
4,
5,
13,
14]. Bone cement displacement is a rare complication of PKP, which has cata-strophic consequences, and there were just a few case reports on this matter in previous literature [
15,
16,
17,
18,
19,
20]. Due to the poor osteointegration and biocompatibility of conventional PMMA, as well as fibrocartilaginous membrane at the periphery of IVC, the penetration of PMMA into the trabecular bone is often insufficient and forming a blocky diffusion [
6,
7,
21,
22]. Be-sides, because of the stress-shielding effect between osteoporotic trabecular bones and rigid PMMA cement, un-augmented trabecular bones compress and move slightly under long-term stress [
8,
23]. Consequently, the locking strength between bone and bone cement is not strong enough, which means the bone cement is easy to displace postoperatively [
24,
25,
26]. The potential risk factors of bone cement displacement have been proven to be uneven cement distribution, intervertebral cleft, and severe osteoporosis [
8]. Thoracolumbar junction is the stress concentration area of the spine, injection of conventional polymethyl methacrylate (PMMA) will increase the elastic modulus of cemented vertebra, change the mechanic transfer between vertebral body and the intervertebral disc, and increase the stress of adjacent vertebral body [
8,
22,
27]. Especially, the occurrence of bone cement displacement will aggravate the uneven stress distribution, thus increasing the chance of fractures of cemented and adjacent vertebrae. In our case, the responsible vertebra with IVC located at the conjunction of stress, and the bone cement distribution appeared blocky that means low locking strength and premature occurrence of bone cement displacement whin 3 days postoperatively. The displaced bone cement aggravated the uneven stress distribution, thus resulting in the adjacent vertebra fractured.
3.2. Clinical Practice Recommendations
There is currently no standard treatment strategy for symptomatic bone cement dis-placement. Chen [
28] et all thought that bone cement reperfusion surgery is a minimally invasive option for neurologically intact patients, which could ameliorate kyphosis and restore vertebral height. Kim [
18] et all found it would be better to inject a volume of bone cement that is greater than the volume the intravertebral cleft to prevent instability caused by non-union. Yang [
26] et al, Tsai [
17] et al and Ha et al [
20] considered that anterior reconstruction and posterior stabilization operation has some merits that theoretically reduce overall morbidity and mortality. To some extent, these open revision operations can rebuild the stability of spine and remove the displaced cement. However, it would be difficult for the elderly to tolerate the large blood loss and long operation time.
In our case, we utilized a curved-tipped guide needle to disrupt the fibrocartilaginous membrane of the T10 vertebra, enabling subsequent infusion of bone cement to penetrate freely into the trabecular bones and anchor at the posterior site of the previously displaced cement. Simultaneously, the injection of bone cement into the T9 vertebra passed through the defective cortex to anchor at the displaced cement of the T10 vertebra. The later infused cement from both vertebrae anchored at the anterior and posterior sites of the previously dis-placed cement, forming an effective multi-point locking system. This system prevents further movement, obviating the necessity for open surgery. Consequently, this process effectively fills the residual intervertebral vacuum cleft, eliminating instability and preventing further displacement of bone cement.
The patient in our case report had vertebral osteonecrosis of T10, where the premature bone cement displaced and resulted in adjacent vertebral fracture within 3 days after operation. After receiving percutaneous kyphoplasty with multi-point anchoring technique (A-PKP) for the second surgery, the patient’s pain alleviated significantly. Postoperative follow-up indicated that the bone cement displacement didn’t progress further.
4. Conclusions
Premature bone cement displacement leading to adjacent vertebral fracture is a rare complication following percutaneous kyphoplasty. The uneven distribution of bone cement patterns and cement leakage are potential contributing factors. Rather than opting for open revision operations, we advocate for the implementation of percutaneous kyphoplasty with a multi-point anchoring technique (A-PKP) in patients experiencing bone cement displacement without neurological deficits. This approach is crucial in preventing further displacement and offers patients an alternative to open surgery.
Author Contributions
Conceptualization, H.W. and S.W.; Operation S.X. and S.W.; Image processing, H.W, H.L. and J.B.H.; Writing—original draft preparation, H.W. and X.D.; Writing—review and editing, S.W.; All authors have read and agreed to the published version of the manuscript.
Funding
This work is jointly funded by the Sichuan Science and Technology Program (NO.2022-YFS0628) and Natural Science Foundation of Sichuan (NO.2023NSFSC0333).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki.
Informed Consent Statement
The patient was informed of the scientific and clinical interest of his treatment history, as well as that data from his case would be submitted to a professional peer-reviewed journal. In-formed consent was obtained from the patient for the publication of this case report.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
We would like to thank all the staff in Department of Spine Surgery, Affiliated Hospital of Southwest Medical University for their contribution on our research.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Steel, H.H. Kummell's disease. Am J Surg 1951, 81, 161–167. [Google Scholar] [CrossRef]
- D'Oria, S.; Delvecchio, C.; Dibenedetto, M.; Zizza, F.; Somma, C. Case report of Kummell's disease with delayed onset myelopathy and the literature review. Eur J Orthop Surg Traumatol 2018, 28, 309–316. [Google Scholar] [CrossRef]
- Li, H.; Liang, C.Z.; Chen, Q.X. Kummell's disease, an uncommon and complicated spinal disorder: a review. J Int Med Res 2012, 40, 406–414. [Google Scholar] [CrossRef]
- Yu, H.; Li, Y.; Yao, X.; Lin, J.; Pan, Y.; Zhuang, H.; Wang, P. Application of percutaneous vertebroplasty and percutaneous kyphoplasty in treating Kümmell's patients with different stages and postural correction status. Expert Rev Med Devices 2020, 17, 357–364. [Google Scholar] [CrossRef]
- Chang, J.Z.; Bei, M.J.; Shu, D.P.; Sun, C.J.; Chen, J.B.; Xiao, Y.P. Comparison of the clinical outcomes of percutaneous vertebroplasty vs. kyphoplasty for the treatment of osteoporotic Kummell's disease:a prospective cohort study. BMC Musculoskelet Disord 2020, 21, 238. [Google Scholar] [CrossRef]
- Libicher, M.; Appelt, A.; Berger, I.; Baier, M.; Meeder, P.J.; Grafe, I.; Dafonseca, K.; Nöldge, G.; Kasperk, C. The intravertebral vacuum phenomen as specific sign of osteonecrosis in vertebral compression fractures: results from a radiological and histological study. Eur Radiol 2007, 17, 2248–2252. [Google Scholar] [CrossRef]
- Hasegawa, K.; Homma, T.; Uchiyama, S.; Takahashi, H. Vertebral pseudarthrosis in the osteoporotic spine. Spine (Phila Pa 1976) 1998, 23, 2201–2206. [Google Scholar] [CrossRef]
- Gao, X.; Du, J.; Zhang, Y.; Gong, Y.; Zhang, B.; Qu, Z.; Hao, D.; He, B.; Yan, L. Predictive Factors for Bone Cement Displacement following Percutaneous Vertebral Augmentation in Kümmell's Disease. J Clin Med 2022, 11. [Google Scholar] [CrossRef]
- Zhan, Y.; Jiang, J.; Liao, H.; Tan, H.; Yang, K. Risk Factors for Cement Leakage After Vertebroplasty or Kyphoplasty: A Meta-Analysis of Published Evidence. World Neurosurg 2017, 101, 633–642. [Google Scholar] [CrossRef]
- Wang, Y.T.; Wu, X.T.; Chen, H.; Wang, C.; Mao, Z.B. Adjacent-level symptomatic fracture after percutaneous vertebral augmentation of osteoporotic vertebral compression fracture: a retrospective analysis. J Orthop Sci 2014, 19, 868–876. [Google Scholar] [CrossRef]
- Lee, K.A.; Hong, S.J.; Lee, S.; Cha, I.H.; Kim, B.H.; Kang, E.Y. Analysis of adjacent fracture after percutaneous vertebroplasty: does intradiscal cement leakage really increase the risk of adjacent vertebral fracture? Skeletal Radiol 2011, 40, 1537–1542. [Google Scholar] [CrossRef]
- Frankel, B.M.; Monroe, T.; Wang, C. Percutaneous vertebral augmentation: an elevation in adjacent-level fracture risk in kyphoplasty as compared with vertebroplasty. Spine J 2007, 7, 575–582. [Google Scholar] [CrossRef]
- Yang, H.; Pan, J.; Wang, G. A review of osteoporotic vertebral fracture nonunion management. Spine (Phila Pa 1976) 2014, 39, B4–6. [Google Scholar] [CrossRef]
- Zhou, C.; Huang, S.; Liao, Y.; Zhang, F.; Meng, X.; Tang, Z.; Zhang, X.; Li, H.; Zhang, Y.; Zhao, S.; et al. Feasibility Analysis of the Bone Cement-Gelatine Sponge Composite Intravertebral Prefilling Technique for Reducing Bone Cement Leakage in Stage I and II Kummell's Disease: A Prospective Randomized Controlled Trial. Orthop Surg 2023, 15, 1763–1771. [Google Scholar] [CrossRef]
- Wagner, A.L.; Baskurt, E. Refracture with cement extrusion following percutaneous vertebroplasty of a large interbody cleft. AJNR Am J Neuroradiol 2006, 27, 230–231. [Google Scholar]
- Jeong, Y.H.; Lee, C.J.; Yeon, J.T.; Bae, J.; Choi, E.; Lee, P.B.; Nahm, F.S. Insufficient Penetration of Bone Cement Into the Trabecular Bone: A Potential Risk for Delayed Bone Cement Displacement After Kyphoplasty? Reg Anesth Pain Med 2016, 41, 616–618. [Google Scholar] [CrossRef]
- Tsai, T.T.; Chen, W.J.; Lai, P.L.; Chen, L.H.; Niu, C.C.; Fu, T.S.; Wong, C.B. Polymethylmethacrylate cement dislodgment following percutaneous vertebroplasty: a case report. Spine (Phila Pa 1976) 2003, 28, E457–460. [Google Scholar] [CrossRef]
- Kim, J.E.; Choi, S.S.; Lee, M.K.; Lee, D.K.; Cho, S.I. Failed Percutaneous Vertebroplasty Due to Insufficient Correction of Intravertebral Instability in Kummell's Disease: A Case Report. Pain Pract 2017, 17, 1109–1114. [Google Scholar] [CrossRef]
- Wang, H.S.; Kim, H.S.; Ju, C.I.; Kim, S.W. Delayed bone cement displacement following balloon kyphoplasty. J Korean Neurosurg Soc 2008, 43, 212–214. [Google Scholar] [CrossRef]
- Ha, K.Y.; Kim, Y.H.; Yoo, S.R.; Molon, J.N. Bone Cement Dislodgement: One of Complications Following Bone Cement Augmentation Procedures for Osteoporotic Spinal Fracture. J Korean Neurosurg Soc 2015, 57, 367–370. [Google Scholar] [CrossRef]
- Zhu, J.; Yang, S.; Yang, Y.; Yao, T.; Liu, G.; Fan, S.; Zhao, H.; Cui, F.; Wang, X.; Jiang, G.; et al. Modified poly(methyl methacrylate) bone cement in the treatment of Kümmell disease. Regen Biomater 2021, 8, rbaa051. [Google Scholar] [CrossRef]
- Chen, J.B.; Xiao, Y.P.; Chen, D.; Chang, J.Z.; Li, T. Clinical observation of two bone cement distribution modes of percutaneous vertebroplasty in the treatment of thoracolumbar Kummell's disease. J Orthop Surg Res 2020, 15, 250. [Google Scholar] [CrossRef]
- Niu, J.; Zhou, H.; Meng, Q.; Shi, J.; Meng, B.; Yang, H. Factors affecting recompression of augmented vertebrae after successful percutaneous balloon kyphoplasty: a retrospective analysis. Acta Radiol 2015, 56, 1380–1387. [Google Scholar] [CrossRef]
- Chen, L.; Dong, R.; Gu, Y.; Feng, Y. Comparison between Balloon Kyphoplasty and Short Segmental Fixation Combined with Vertebroplasty in the Treatment of Kummell's Disease. Pain Physician 2015, 18, 373–381. [Google Scholar]
- Yang, C.C.; Chien, J.T.; Tsai, T.Y.; Yeh, K.T.; Lee, R.P.; Wu, W.T. Earlier Vertebroplasty for Osteoporotic Thoracolumbar Compression Fracture May Minimize the Subsequent Development of Adjacent Fractures: A Retrospective Study. Pain Physician 2018, 21, E483–e491. [Google Scholar]
- Yang, S.C.; Chen, W.J.; Yu, S.W.; Tu, Y.K.; Kao, Y.H.; Chung, K.C. Revision strategies for complications and failure of vertebroplasties. Eur Spine J 2008, 17, 982–988. [Google Scholar] [CrossRef]
- Trout, A.T.; Kallmes, D.F.; Layton, K.F.; Thielen, K.R.; Hentz, J.G. Vertebral endplate fractures: an indicator of the abnormal forces generated in the spine after vertebroplasty. J Bone Miner Res 2006, 21, 1797–1802. [Google Scholar] [CrossRef]
- Chen, T.; Lin, C.; Wang, Y.; Yang, H.; Li, X.; Chu, G.; Jiang, W.; Liu, Y. Bone Cement Reperfusion Revision Surgery for Symptomatic Recurrence of Kummell's Disease After Percutaneous Kyphoplasty. Global Spine J 2023, 21925682231174189. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).