Introduction
Narcolepsy is a chronic neurological disorder affecting rapid eye movement (REM) sleep. It is characterized by extended daytime sleepiness, fragmented sleep, nightly hallucinations, and sleep paralysis [
1,
2]. A key symptom is cataplexy, a loss of muscle tone elicited by emotions, especially humor, and jocularity [
3]. Cognition is frequently affected and the condition has severe socioeconomic consequences [
4,
5,
6,
7]. Narcolepsy is categorized into two types. Narcolepsy with associated cataplexy is classified as narcolepsy type 1; narcolepsy without cataplexy is type 2 [
8]. Patients with narcolepsy type 1 have decreased hypocretin neurons in the lateral hypothalamus providing a pathogenetic explanation, as hypocretin plays an important role in the human sleep and metabolic system [
9,
10].
Publications on the prevalence of narcolepsy report diverse rates. A global review reported a mean prevalence of 30/100,000 with ranges between 4 and 56/100,000 inhabitants, even up to 160/100,000 in Japanese children [
11,
12]. The large variation is explained by the disparity of populations of different ethnicities, age groups, and methodologies. In Sweden, a recent study mentioned a crude prevalence restricted to healthcare-associated cases of 21.7/100,000 inhabitants in 2016, which only included patients retrieved in the National Patient Register (NPR) and pharmaceutical registries [
6]. Studies on the general incidence of narcolepsy show variable numbers as well with peaks in childhood/adolescence but also later in life [
13,
14]. A review estimated the incidence rate of narcolepsy as 0.3-0.6/100,000/year, suggesting an estimated number of 30-60/100,000/year presently [
15]. Another study describes the morbidity of narcolepsy in Europe before the influenza A (H1N1) pandemic, [
16]. Using some of the results in this article, we estimate that it corresponds to an incidence rate of 0.7/100,000/year in our country before the pandemic.
Sex ratio has shown varying distributions, a large international study that characterized clinical presentations of narcolepsy in different ethnicities, showed no difference in sex ratio across ethnicities [
17]. A US healthcare claims database from 2008 to 2010, showed a 50% greater prevalence and incidence among women compared to men across most age groups [
18]. Another population-based study of narcolepsy incidence from 2004 to 2013 in the US estimated a higher rate among women as well [
19]. Additionally, a Chinese study analyzing 162 patients with narcolepsy found that narcolepsy occurred 1.73 times more frequently in men than women [
20]. A recent study from the national narcolepsy registry found a sex ratio of 1.3 (women/men), i.e., a slight dominance of women in Sweden [
6].
The cause of narcolepsy is multifactorial with a genetic susceptibility through a strong association with the human leucocyte receptor (HLA) DR2 [
21,
22] and in addition several environmental factors of importance [
23]. Infections such as streptococcal infections and influenza A have been reported to precede the debut of narcolepsy [
24,
25]. There is subsequently strong evidence for narcolepsy being an autoimmune disorder, even though no useful auto-antibodies have been identified in clinical settings [
26,
27].
In the context of the H1N1 pandemic and the Pandemrix vaccination in 2009-2010, an increased number of narcolepsy cases were noted in several countries [
28]. Sweden had a high vaccination rate of around 60% of the population and the subsequent increase in narcolepsy was eventually interpreted as an effect of the extensive Pandemrix vaccinations [
29,
30,
31,
32]. Notably, in China, where no vaccinations were performed, studies indicated an increase in seasonal narcolepsy incidence as well, most probably due to the H1N1 infection [
33]. Furthermore, in Denmark, a country with a low vaccination rate, an increasing number of patients with narcolepsy during the period after the H1N1 infection was identified [
34]. Consequently, the correlation between the swine flu virus H1N1 infection and/or Pandemrix vaccination and the growing incidence rate of narcolepsy is of interest in both cases.
The background to this article was the neurologists' recent clinical impression that narcolepsy patients in the adult neurology outpatient clinics were getting steadily younger. This seemed to be supported by regional data in the Swedish Narcolepsy Registry, a sub-registry of the national Neuroregistry launched in 2012 that collects narcolepsy cases at clinics.
This paper aims to analyze the increase in narcolepsy cases in Sweden after the H1N1 pandemic and the Pandemrix vaccination, with a focus on age and sex distribution. Post hoc, we aimed to validate the origin of the excess cases.
Materials and Methods
Data on narcolepsy patients was extracted from the NPR (https:/socialstyrelsen.se Accessed May 2019). This dataset included the number of individuals with ICD code G47.4 annually from 2005 to 2017, categorized by sex and age groups spanning five years. Since 1968, the NPR has collected data on all inpatient visits to the hospital, and after 2001 it was expanded to include even all outpatient specialist care visits. However, primary health care is not included in this register.
The Swedish Total Population Register (TPR) collects and provides information on all persons born in 1932 or later in Sweden. For the prevalence calculation, the information obtained on the number of individuals was divided into sex and age groups annually from 2005 to 2017 in Sweden (
https://www.scb.se Accessed Mars 2021).
Stata v17 (StataCorp LLC, College Station, TX, USA) was used for the statistical analysis of the trend in the prevalence over the years by a score test to determine the trend of odds.
In a post hoc analysis, the excess cases were calculated using a stipulated incidence rate of 0.7/100,000/year, corresponding to a crude number of about 70 cases/year in Sweden, a natural incidence calculated from data published by Wijnans et al [
16].
The study was approved by the institutional review board in Linköping (Dnr 2014/129–31), (Dnr 2020–02594).
Results
The data extracted from the NPR showed that the number of narcolepsy cases in the study cohort in 2005 consisted of 637 individuals (375 women; 262 men), yielding a crude prevalence of 7.04 per 100,000 inhabitants (women 8.2; men 5.8). The number of narcolepsy patients increased significantly between 2009 and 2014 compared to the period before 2009. The most significant increase was seen in 2011, with 1341 patients (763 women; 578 men), corresponding to a prevalence of 14.1 per 100,000 inhabitants (women 17.8; men 13.9). In 2017, the total number of narcolepsy patients was 2044 (1169 women; 875 men), with a total prevalence of 20.2/100,000 (women 23.2; men 17.2), (Table 1).
The prevalence was higher among women than men. The sex ratio in the total cohort 2017 was 1.3 (w/m), p < 001. Notably, the sex ratio remained unchanged during the study period and was approximately the same after the H1N1 pandemic and the Pandemrix vaccination campaign (Table 1).
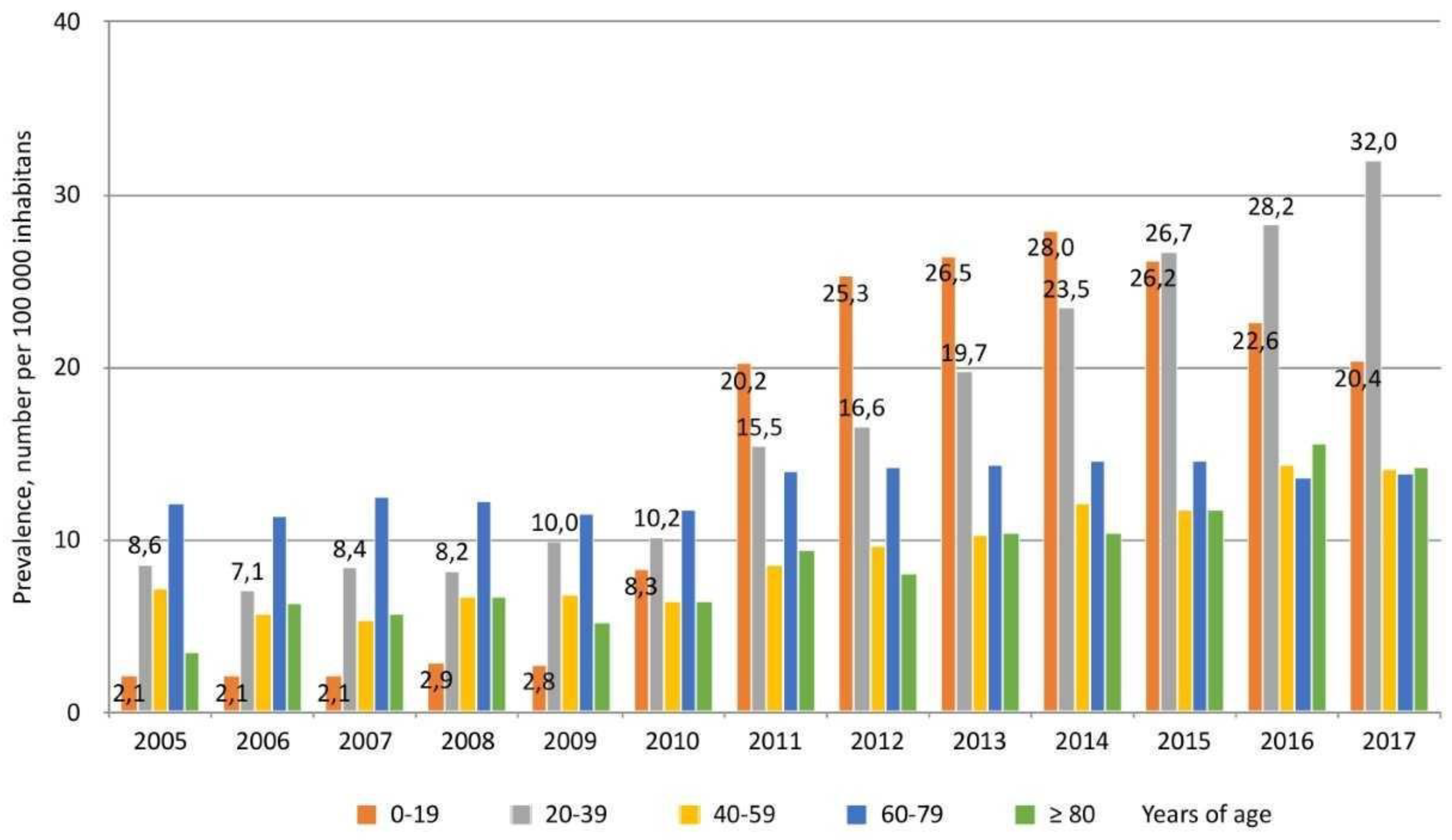
The overall prevalence of narcolepsy cases increased significantly between 2005 and 2017 (
p < 0.01). The increasing prevalence was particularly noted in the younger age groups (0-19 years), starting in 2010, with a prevalence of 8.3/100,000 inhabitants and an annual increase to 28.0 in 2014. In the age group 20-39 years, the prevalence was 15.5/100,000 inhabitants in 2011, with a further increase to 32/100,000 inhabitants in 2017, (
p < 0.01),
Figure 1.
Calculations from the Swedish narcolepsy registry in the period between 2005 and 2017 (n=950) showed a low mean age (37.4 years) and low median age (31 years).
Discussion
The number of patients diagnosed with narcolepsy in Sweden increased significantly after the H1N1 pandemic and the Pandemrix vaccination in 2009-2010, which is confirmed by our data. This was especially evident in children and teenagers, as visualized in
Figure 1, which has been demonstrated by previous studies and other methods, including our report on children in Östergötland County in Sweden. which showed an odds ratio as high as 17.7 (95% CI: 2.7- 147.5; p = 0.0036) [
29]. In Sweden, however, only an estimated number of 450 persons with narcolepsy have received economic compensation for the approved side effects of the Pandemrix vaccination. In addition, our clinical impression was that vaccinated narcolepsy cases tended to dominate in the Swedish narcolepsy polyclinic, with or without approved compensation. This prompted us to analyze the increase more thoroughly focusing on age and sex
The National Patient Register (NPR)
The observed increase in the number of narcolepsy patients starts from an unexpectedly low level, about 800 (2005-2009), which may be explained by the register´s recent inclusion of specialist open care. The NPR register did not include patients from open visits in neurology until 2001, i.e., only four years before the first data in the present study. Importantly, patients with a previous narcolepsy diagnosis who are neither actively seeking care nor using pharmacotherapy will be excluded. Patients attending primary health care will also be left out since these visits are not registered in the NPR. However, we believe that this number is small since general practitioners usually do not diagnose or treat patients with narcolepsy and typically do not possess the required license for prescribing the drugs that are used to treat narcolepsy. The rather stable baseline prevalence before the pandemic in 2009-2010 incentivized us to use the NPR data for comparison when analyzing the increase of narcolepsy patients.
Persisting Increase in the Prevalence of Narcolepsy
The increase in the prevalence of narcolepsy was most prominent between 2009 to 2014 but even later in 2017 the prevalence of narcolepsy in Sweden was slowly increasing and had not yet reached a plateau. Notably, to receive economic compensation from Swedish Pharmaceutical Insurance and the Swedish authorities, the onset of narcolepsy must have been documented within two years after the patient´s Pandemrix vaccination, i.e., around 2012. However, the prevalence has continued to increase long after that time. Delayed diagnosis, a well-known phenomenon, contributes to this trend. One example is that hypersomnia in teenagers is often mistaken as a natural phenomenon and a narcolepsy diagnosis therefore is not considered [
35]. This is well-known to occur and can explain many “late cases” [
30].
Ad Hoc Analysis
The observed increase in narcolepsy cases as seen in our data was greater than expected when considering the small number of patients receiving approved compensation due to the Pandemrix vaccination-related effects.
Considering the new evaluation from MPA we made a crude calculation on the possible excess cases taken from our data,
post hoc: Table 1 illustrates that more than 1000 new cases were registered between 2009 and 2014 (five years). With an estimated “natural” incidence of around 70/year as recalculated from data by Wijnans et al [
16], only 350 cases would be expected to occur. Subsequently, if deaths are not considered, a conservative estimation would indicate 600-700 excess cases in our data from this period. Thus, even if those 450 patients who have received compensation for vaccination side effects are subtracted, hundreds of excess cases remain.
A potential explanation may be that the H1N1 influenza also increased the risk of narcolepsy in line with the risk demonstrated by the wild-type H1N1 virus in China among people who did not receive the Pandemrix vaccination [
36]. The co-occurrence of subclinical infection and vaccination is also of interest in this respect. Such a phenomenon has been mentioned as a possible cause of the suspected geographic gradient of post-Pandemrix narcolepsy in Sweden: the vaccinations started from the north, and the infection entered the country from the south [
6]. This resulted in early infections and late vaccinations in the southern part of the country, where the majority of vaccinated cases seemed to be located. There may also have been a previous under-diagnosing of narcolepsy especially among children and teenagers. Narcolepsy among children was very rare before 2009, and poor knowledge may have diminished the chance of a correct diagnosis. The increased attention to narcolepsy supported by the media may finally raise the awareness of narcolepsy among the public, leading to more healthcare contacts in the affected group and introducing a bias into the study. However, the fact that children and teenagers mainly constitute the increased prevalence contradicts that overdiagnosing narcolepsy would be a major cause. Such a bias would most probably affect all age groups similarly.
Finally, the sex ratio deserves some attention, for example concerning the rapidly increasing women's quotient of the sex ratio in multiple sclerosis, another autoimmune disorder [
37]. Environmental factors such as obesity, smoking, and shortage of vitamin D have been mentioned as possible causes [
38]. In narcolepsy, on the other hand, we cannot yet state a similar sex-related development until a systematic evaluation of sex differences has been performed.
It is important to note that in the present study, there is no information on the vaccination rate among the narcolepsy cases, so the number of patients who did not receive the Pandemrix vaccination but were still diagnosed with narcolepsy is unknown. Additionally, there is no information on concurrent swine flu in our material.
Conclusions
Our retrospective analysis of the data extracted from the NPR register in 2019 confirms the increase in narcolepsy. Since the Pandemrix vaccination status of the patients is not known, we can only crudely estimate the impact of the vaccination. Regardless, the apparent escalation seems to be greater than the 450 cases approved for compensation due to the onset of narcolepsy within two years. This prompts the basis for looking for other reasons, for example, a prolonged latency before clinical onset, or narcolepsy cases initiated by the H1N1 virus itself, through overt or subclinical infection. Also, the impact of the infection and vaccination in combination should be considered. The prominent increase of children, adolescents, and young adults among the cases after 2009/2010 as demonstrated in our data fits well with the impression of the recent situation in the narcolepsy polyclinic, where young patients tend to dominate the panorama in, frequency, and often severity. This is of high concern since an early onset of such a disease, affecting energy, concentration ability, and cognition, may be an obstacle to future personal and social development.
References
- Kornum BR, Knudsen S, Ollila HM, Pizza F, Jennum PJ, Dauvilliers Y, Overeem S. Narcolepsy. Nat Rev Dis Primers. 2017, 3, 16100. [CrossRef]
- Bassetti CLA, Adamantidis A, Burdakov D, Han F, Gay S, Kallweit U, et al. Narcolepsy - clinical spectrum, aetiopathophysiology, diagnosis and treatment. Nature reviews Neurology. 2019, 15, 519–539. [CrossRef] [PubMed]
- Schiappa C, Scarpelli S, D'Atri A, Gorgoni M, De Gennaro L. Narcolepsy and emotional experience: a review of the literature. Behav Brain Funct. 2018, 14, 19. [CrossRef] [PubMed]
- Witt ST, Drissi NM, Tapper S, Wretman A, Szakacs A, Hallbook T, et al. Evidence for cognitive resource imbalance in adolescents with narcolepsy. Brain Imaging Behav. 2018, 12, 411–424. [CrossRef] [PubMed]
- Drissi NM, Szakacs A, Witt ST, Wretman A, Ulander M, Stahlbrandt H, et al. Altered Brain Microstate Dynamics in Adolescents with Narcolepsy. Front Hum Neurosci. 2016, 10, 369. [CrossRef] [PubMed]
- Gauffin H, Fast T, Komkova A, Berntsson S, Bostrom I, Landtblom AM. Narcolepsy treatment in Sweden: An observational study. Acta Neurol Scand. 2022, 145, 185–192. [CrossRef] [PubMed]
- Jennum P, Ibsen R, Petersen ER, Knudsen S, Kjellberg J. Health, social, and economic consequences of narcolepsy: a controlled national study evaluating the societal effect on patients and their partners. Sleep Med. 2012, 13, 1086–1093. [CrossRef] [PubMed]
- Nishino S, Ripley B, Overeem S, Lammers GJ, Mignot E. Hypocretin (orexin) deficiency in human narcolepsy. Lancet 2000, 355, 39–40. [CrossRef] [PubMed]
- Thannickal TC, Moore RY, Nienhuis R, Ramanathan L, Gulyani S, Aldrich M, et al. Reduced number of hypocretin neurons in human narcolepsy. Neuron 2000, 27, 469–474. [CrossRef]
- Drissi NM, Warntjes M, Wessen A, Szakacs A, Darin N, Hallbook T, et al. Structural anomaly in the reticular formation in narcolepsy type 1, suggesting lower levels of neuromelanin. Neuroimage Clin. 2019, 23, 101875. [CrossRef]
- Partinen M, Kornum BR, Plazzi G, Jennum P, Julkunen I, Vaarala O. Narcolepsy as an autoimmune disease: the role of H1N1 infection and vaccination. Lancet Neurol. 2014, 13, 600–613. [CrossRef]
- Longstreth WT, Jr., Koepsell TD, Ton TG, Hendrickson AF, van Belle G. The epidemiology of narcolepsy. Sleep. 2007, 30, 13–26. [CrossRef]
- Ohayon MM, Thorpy MJ, Carls G, Black J, Cisternas M, Pasta DJ, et al. The Nexus Narcolepsy Registry: methodology, study population characteristics, and patterns and predictors of narcolepsy diagnosis. Sleep Med. 2021, 84, 405–414. [CrossRef]
- Silber MH, Krahn LE, Olson EJ, Pankratz VS. The epidemiology of narcolepsy in Olmsted County, Minnesota: a population-based study. Sleep. 2002, 25, 197–202. [CrossRef]
- Hallbook T SA, Bialek F, Feltelius N, Landtblom AM, Malmgren K. Narcolepsy-rare disease that has received increased attention. Pandemrix vaccination caused a higher incidence among children and adolescents. Lakartidningen 2014, 111, 1770–1773.
- Wijnans L, Lecomte C, de Vries C, Weibel D, Sammon C, Hviid A, et al. The incidence of narcolepsy in Europe: before, during, and after the influenza A(H1N1) pdm09 pandemic and vaccination campaigns. Vaccine 2013, 31, 1246–1254. [CrossRef] [PubMed]
- Kawai M, O'Hara R, Einen M, Lin L, Mignot E. Narcolepsy in African Americans. Sleep 2015, 38, 1673–1681. [CrossRef]
- Scheer D, Schwartz SW, Parr M, Zgibor J, Sanchez-Anguiano A, Rajaram L. Prevalence and incidence of narcolepsy in a US health care claims database, 2008-2010. Sleep. Sleep 2019, 42. [CrossRef]
- Lee RU, Radin JM. A population-based epidemiologic study of adult-onset narcolepsy incidence and associated risk factors, 2004-2013. J Neurol Sci. 2016, 370, 29–34. [CrossRef]
- Wu H, Zhuang J, Stone WS, Zhang L, Zhao Z, Wang Z, et al. Symptoms and occurrences of narcolepsy: a retrospective study of 162 patients during a 10-year period in eastern China. Sleep medicine. 2014, 15, 607–613. [CrossRef]
- Mignot E, Thorsby E. Narcolepsy and the HLA system. N Engl J Med. 2001, 344, 692. [CrossRef]
- Juji T, Satake M, Honda Y, Doi Y. HLA antigens in Japanese patients with narcolepsy. All the patients were DR2 positive. Tissue Antigens. 1984, 24, 316–319. [CrossRef]
- Mignot E. Genetic and familial aspects of narcolepsy. Neurology. 1998, 50, S16–22. [CrossRef]
- Aran A, Lin L, Nevsimalova S, Plazzi G, Hong SC, Weiner K, et al. Elevated anti-streptococcal antibodies in patients with recent narcolepsy onset. Sleep 2009, 32, 979–983. [CrossRef]
- Picchioni D, Hope CR, Harsh JR. A case-control study of the environmental risk factors for narcolepsy. Neuroepidemiology 2007, 29, 185–192. [CrossRef] [PubMed]
- Lind A, Salami F, Landtblom AM, Palm L, Lernmark A, Adolfsson J, Elding Larsson H. Immunocyte single cell analysis of vaccine-induced narcolepsy. Eur J Immunol. 2021, 51, 247–249. [CrossRef]
- Hallberg P, Smedje H, Eriksson N, Kohnke H, Daniilidou M, Ohman I, et al. Pandemrix-induced narcolepsy is associated with genes related to immunity and neuronal survival. EBioMedicine 2019, 40, 595–604. [CrossRef]
- Partinen M, Saarenpaa-Heikkila O, Ilveskoski I, Hublin C, Linna M, Olsen P, et al. Increased incidence and clinical picture of childhood narcolepsy following the 2009 H1N1 pandemic vaccination campaign in Finland. PLoS One. 2012, 7, e33723. [CrossRef]
- Boström I BS, Zheliba N, Gauffin H, Kristoffersson A, Nimelä V, Landtblom AM. Narcolepsy as a side effect of swine flu vaccination. 2017: Journal of neurological Sciences; 2017. p. 189.
- Boström I LO, Partinen M, Landtblom A-M. Vaccination against swine flu caused narcolepsy in several European countries. Health Risk Analysis. 2020, 3, 180–185. [CrossRef]
- Sarkanen T, Alakuijala A, Julkunen I, Partinen M. Narcolepsy Associated with Pandemrix Vaccine. Curr Neurol Neurosci Rep. 2018, 18, 43. [CrossRef]
- Szakacs A, Darin N, Hallbook T. Increased childhood incidence of narcolepsy in western Sweden after H1N1 influenza vaccination. Neurology 2013, 80, 1315–1321. [CrossRef] [PubMed]
- Han F, Lin L, Warby SC, Faraco J, Li J, Dong SX, et al. Narcolepsy onset is seasonal and increased following the 2009 H1N1 pandemic in China. Ann Neurol. 2011, 70, 410–417. [CrossRef] [PubMed]
- Thebault S, Vincent A, Gringras P. Narcolepsy and H1N1 vaccination: a link? Curr Opin Pulm Med. 2013, 19, 587–593. [CrossRef] [PubMed]
- Landtblom AM, Engstrom M. The sleepy teenager - diagnostic challenges. Front Neurol. 2014, 5, 140. [CrossRef]
- Wang X, Xiao F, Wang Y, Deng X, Chen Z, Dong X, et al. Changed epidemiology of narcolepsy before, during, and after the 2009 H1N1 pandemic: a nationwide narcolepsy surveillance network study in mainland China, 1990-2017. Sleep 2023, 46. [CrossRef]
- Dunn SE, Gunde E, Lee H. Sex-Based Differences in Multiple Sclerosis (MS): Part II: Rising Incidence of Multiple Sclerosis in Women and the Vulnerability of Men to Progression of this Disease. Curr Top Behav Neurosci. 2015, 26, 57–86. [CrossRef]
- Alfredsson L, Olsson T. Lifestyle and Environmental Factors in Multiple Sclerosis. Cold Spring Harb Perspect Med. 2019, 9. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).