1. Introduction
Obesity has been a public health concern for several decades globally [
1]. It is projected that individuals living with obesity will reach up to one billion by 2030, particularly in low-and middle-income countries [
2]. In Thailand, the incidence rate of obesity increased by 10% within five-year period (2012-2018) [
3]. As obesity is widely recognized as a significant public health issue, numerous studies have shown that obesity is strongly associated with hypertension, type 2 diabetes mellitus, coronary heart disease, stroke, and poor cardiorespiratory fitness [
4]. In light of the evidence, poor cardiorespiratory fitness plays an important factor as a cardiovascular risk and is a strongest mortality predictor [
5,
6]. Peak oxygen uptake is an objective measure of cardiorespiratory fitness in individuals with and without health condition [
7]. Obesity has been negatively correlated with peak oxygen uptake [
8,
9,
10]. Moderate-intensity aerobic exercise, performing 30 minutes per day, 5 days a week or a total of 150 min per week) [
11] has provided positive effects on body fat reduction [
12,
13,
14] and oxygen uptake improvement [
13,
14] in obese individuals. However, reduction in movement efficiency as a consequence of excessive body fat results in decreased exercise efficiency and reduced fat oxidation due to multiorgan dysfunction (e.g., low adenosine triphosphate (ATP) synthesis and poor muscular blood flow [
15,
16,
17]. Hence, investigating the impact of obesity on oxygen uptake and fat oxidation during moderate-intensity aerobic exercise is essential for identifying health status and is likely to refer to cardiorespiratory fitness status.
The body mass index is widely adopted as an anthropometric marker to classify obesity and non-obesity [
18,
19]. Nevertheless, some evidence argues against the use of BMI on obesity classification as it does not distinguish fat mass and fat-free mass [
20]. Other obesity-related anthropometric markers including waist circumference (WC), waist – to – hip ratio (WHR), and waist – to – height ratio (WHtR) have been served as alternative markers. These markers are recognized as an indirect method for identifying body fatness, particularly abdominal or central obesity. A previous work has suggested that central obesity, known as abdominal fat, is likely to be more closely linked with total adiposity cumulation [
21]. However, the impact of obesity, as measured by these anthropometric markers, on oxygen uptake and fat oxidation during moderate-intensity aerobic exercise remains unknown. Enhancing our comprehension of how obesity affects oxygen uptake and fat oxidation can provide valuable insight into which anthropometric markers are responsible for obesity-related health risks. This information could potentially help reduce the burden on public health.
Physical activity is defined as “bodily movement produced by skeletal muscles that results in energy expenditure”. It can take in an exercise form (a planned, structured, and repetitive form) or a non-exercise form (e.g., work-related activity, housework-related activity, daily walking, etc.) [
22]. The literature clearly indicates that physical activity serves as a protective factor against cardiovascular disease [
23]. Previous studies have illustrated that physical activity could improve a prognosis of cardiovascular diseases in healthy individuals and those who were at risk of cardiovascular diseases [
24,
25]. The 2016 European Guidelines on cardiovascular disease prevention has also recommended a sufficient physical activity, as reflected by ≥ 150 min/week of moderate-intensity of physical activity or ≥ 75 min/week of vigorous-intensity of physical activity [
26]. Conversely, physical inactivity is a predictor of cardiovascular risk factors and is positively correlated with body fat [
27]. A previous systematic review ana meta-analysis has shown that individuals with sedentary lifestyle had a 1.9 times higher risk of type 2 diabetes, a 1.14 times higher risk of cardiovascular disease incidence, and a 1.15 times higher risk of cardiovascular mortality when compared to those with sufficient physical activity [
28].
Furthermore, evidence has revealed that obesity is associated with lower levels of physical activity [
29]. Among these contexts, it is suggested that obesity with high physical activity may exhibit higher oxygen uptake than those with low physical activity. This study aimed to investigate the impact of obesity, as measured by various anthropometric indicators (i.e., BMI, WC, WHR, and WHtR), and physical activity level on oxygen uptake and fat oxidation during moderate-intensity aerobic exercise in adults. We hypothesized that obese adults, as classified by at least one anthropometric indicator would have poorer oxygen uptake and lower fat oxidation than those with non-obesity. In addition, obese adults, as classified by at least one anthropometric indicator who were active had better results on these outcomes than obese adults who were inactive. The findings of this study would provide important indicators related to health risks in obese adults.
2. Materials and Methods
2.1. Study Design and Participants
The data of this study was obtained from our original research [
30]. Recruitment process was conducted via a public advertisement during November 2022 - February 2023. The current study investigated a total of 48 individuals with obesity classified by BMI. Participants who had BMI equal or above 25 kilometer per square meters (kg/m2) according to guideline for Asia-Pacific region [
31]; aged between 20 to 60 years; and could walk without walking aids were included. Any participants who met the following criteria: (i) presence in uncontrolled cardiovascular diseases (e.g., unstable angina and acute heart failure), (ii) having neurological conditions (e.g., severe spasticity and epilepsy), (iii) having musculoskeletal conditions (e.g., severe osteoarthritis and rheumatoid arthritis), (iv) having respiratory disorders (e.g., severe asthma and chronic obstructive pulmonary disease) which restricted to perform exercise, or refusing study participation were excluded. All participants provided written informed consent before data collection. The study was approved by the Research Ethics Committee of Research Institute for Health Sciences, Chiang Mai University (Approval number: 55/2022).
2.2. Aerobic Exercise Test
The exercise testing session contains three activities
— warm up, aerobic exercise test, and cool down. Eligible participants were instructed to perform aerobic exercise test with moderate intensity. Moderate-intensity aerobic exercise was done using a bicycle ergometer (Lode, Lode B.V., Groningen, Netherland). The aerobic exercise was done in the laboratory room environment, set at 50-55% relative humidity and a constant room temperature of 25℃. The moderate intensity of exercise was determined based on a percentage of predicted maximum heart rate (HRmax) (HRmax was calculated from 220 minus with age), which are ranging between 64-76% HRmax [
32]. The moderate intensity was obtained by workload adjusting within an initial 5 minutes of exercise, which was adjusted every minute until the moderate intensity of exercise was met. According to Wasserman’s formula, the workload (watt) was computed based on each participant’s VO2peak and VO2unloaded (workload = VO2peak ((height-age) x sex) - VO2unloaded (150 + (6 x weight)))/ 100) [
33]. Each participant was instructed to perform cycling for a total of 30 minutes, at a constant speed of 60 revolutions per minute (rpm). Lower limb stretching, carried out as warm up and cool down was performed before and after completed the aerobic exercise session. Hip flexor, knee flexor, and knee extensor muscle groups were statically stretched (15 seconds/ muscle/ side/ set) for 3 sets each.
2.3. Physical Activity Assessment
The physical activity level was evaluated using a short version of the International Physical Activity Questionnaire (IPAQ) [
34]. The short version of IPAQ is widely used across countries, and is valid and reliable [
35,
36]. Participants were interviewed and given verbal information about their physical activity over the last 7 days. During completed the questionnaire, all participants were also provided with a time to recall their physical activity. The IPAQ containing eight subitems encompasses questions relevant time spent vigorous activity, moderate activity, walking, and sitting. Metabolic equivalent in a minute per week (MET-minute/ week) was computed for each activity category, except for sitting. Formulas used to calculate the MET-minute/ week of each activity depend on its factor, number of minutes, and number of days: (a) vigorous MET-minute (8 x minutes of vigorous-intensity activity x days of vigorous-intensity activity); (b) moderate MET-minute (4 x minutes of moderate-intensity activity x days of moderate-intensity activity); (c) walking MET-minute (3.3 x minutes of walking activity x days of walking activity). The physical activity is interpreted as highly active, minimally active, and inactive. Criteria for these three categories are as follows.
Highly active level is classified based on either criteria: (a) ≥ 3 days of vigorous-intensity activity which obtain a minimum of an equal or above 1500 MET-minute/week; (b) ≥ 7 days of any combined walking, moderate- or vigorous-intensity activities which receive a minimum of at least 3000 MET-minute/week.
Minimally active level is considered based on either criteria: (a) ≥ 3 days of vigorous activity with a minimum of 20-minute/day; (b) ≥ 5 days of moderate-intensity activity or walking, with a minimum of 30-minute/day; (c) ≥ 5 days of any combined vigorous-intensity activity, moderate-intensity activity, or walking, with a minimum of 600 MET-minute/week.
Inactive level is categorized as participants who do not meet either highly active or minimally active levels.
2.4. Anthropometric Measurement
Anthropometric variables included BMI, WC, WHR, and WHtR. The measurement of anthropometrics are as follows;
2.4.1. Body Mass Index (BMI)
The Body Mass Index (BMI) is determined by taking into account an individual's weight and height. The BMI is computed using the following mathematical expression: BMI equals the weight in kilograms (kg) divided by the square of the height in meters (m^2). In the context of the participants in this study, who are in Asia-Pacific region, a BMI exceeding 25 kg/m^2 is categorized as obese individuals [
31].
2.4.2. Waist Circumference (WC)
The measurement of waist circumference (WC) involved the use of a non-elastic measuring tape, and this was conducted with participants in a standing position, barefoot. The participants were instructed to expose their waist area and fold their arms across their chest. The assessor positioned the non-elastic measuring tape horizontally, precisely at the midpoint between the lowest rib and the iliac crest [
37]. The assessor took the measurement of the waist circumference while participants were in an exhaled state. The measurement was recorded in centimeters (cm). Each participant's WC was measured twice, and the average of these two measurements was utilized for analysis. In case where the two measurements differed by more than 1 cm, a third measurement was taken to ensure accuracy. The WC that equals or exceeds 90 cm in men and 80 cm in women is considered as a key indicator of obesity [
38].
2.4.3. Waist – to - Hip Ratio (WHR)
The waist – to – hip ratio (WHR) was calculated by dividing the waist circumference by the hip circumference. The hip circumference was measured in cm at its broadest point above the buttocks. Each participant underwent this measurement twice, and the average of these two values was employed in the computation of the waist – to – hip ratio. In situations where the two measurements exhibited a variance greater than 1 cm, a third measurement was taken to guarantee precision. As outlined in reference [
38], a WHR equal to or exceeding 0.9 for men and 0.85 for women is established as a significant marker for obesity.
Waist – to – height ratio (WHtR)
The waist – to – height ratio (WHtR) was determined by dividing the waist circumference by individual’s height in cm. In accordance with the criteria provided in reference [
39], a WHtR value that equal to or exceeding 0.51 for men and 0.53 for women is established as a significant indicator of obesity.
2.5. Oxygen Uptake Measurement
The measurement of oxygen uptake (VO2) was conducted during a 30-minute session of moderate exercise intensity. To capture a comprehensive profile of VO2, data points were recorded at 5 minutes intervals throughout the entire 30-minute aerobic exercise session. Subsequently, these VO2 values were adjusted based on the participants’ respective body weight to account for variations among individuals. The aggregate oxygen uptake for the full 30-minute duration, referred to as total VO2 (Vo2tot), was calculated as the sum of VO2 measurements taken over the course of the exercise, ensuring that it was adjusted for each 5 minutes segment of the session.
This approach allowed for a more precise evaluation of the participants’ oxygen consumption, taking into consideration both the intensity and duration of the exercise, while also accounting for differences in body weight. By normalizing the VO2 data, it provided a standardized way to compare and analyze the participants’ metabolic responses to the 30-minute moderate exercise, enhancing the accuracy and comprehensiveness of the assessment.
2.6. Fat Oxidation Measurement
Fat oxidation, an important component of metabolic analysis, was determined through the utilization of an indirect calorimetry method, with a stationary metabolic cart (Corival CPET, Lode B.V., Groningen, Netherland). This advanced equipment precisely measured oxygen consumption and carbon dioxide production, allowing for a comprehensive evaluation of the fat oxidation process. The calculation of fat oxidation involved a straightforward yet effective formula that subtracted the carbon dioxide production (VCO2) from the oxygen consumption (VO2). This formula denoted as [(1.695 x VO2) – (1.701 x VCO2)] [
40] and is a widely recognized approach for determining fat oxidation rates.
2.7. Procedures
After screening completed, all eligible participants were instructed to (i) avoid vigorous exercise or activity of at least 24 hr and (b) refrain from beverages and meals within 8 hr prior to data collecting day. On the data collecting day, participants were asked to record their general information (i.e., age, sex, weight, height, and underlying disease) and physical activity. The participants were then measured anthropometric parameters (i.e., BMI, WC, WHR, and WHR) by a well-trained assessor. All participants were asked to perform moderate-intensity aerobic exercise for 30 minutes. Prior to the moderate-intensity aerobic exercise testing, the participants were instructed to sit quietly on the bicycle seat test for 5 minutes in order to ensure a resting status. During the exercise test, oxygen uptake and fat oxidation were recorded. Vital sign (i.e., blood pressure, heart rate, and oxygen saturation) and adverse clinical symptoms were monitored throughout the test.
2.8. Statistical Analyses
Descriptive statistics were used to present baseline characteristics. The Shapiro-Wilk test was used to assess the normal distribution of data. For the outcome analysis, an independent t-test was carried out to compute the differences in VO2tot and fat oxidation between obese and non-obese groups, classified by WC, WHR, and WHtR. One-way analysis of variance (ANOVA) was used to compute the difference in VO2tot and fat oxidation among active obese (Ac-Ob), inactive obese (IAc-Ob), active non-obese (Ac-nOb), and inactive non-obese (IAc-nOb) groups, classified by BMI, WC, WHR, and WHtR. Subgroup analysis was performed by Bonferroni post-hoc adjustment. Dichotomous data (i.e., sex and underlying diseases) were presented as number and percentage while continuous data (i.e., age, weight, height, BMI, VO2tot, and fat oxidation) were expressed a mean ± 95% confidence interval (CI). The data were analyzed by SPSS statistics software (version 22.0, IBM Corp., Armonk, NY, USA) for windows. Significance level was set at p ≤ 0.05.
3. Results
Baseline characteristics are presented in
Table 1. Eligible participants, with a mean age of 28.94 years, were predominantly women (72.9%). Allergic diseases were identified as the most underlying condition, accompanied by dyslipidemia and hypothyroidism.
All participants in this study were classified as obese based on their BMI. Therefore, the classification of obese and non-obese groups in this study was determined solely using WC, WHR, and WHtR. Based on the factor of obesity, the total oxygen uptake (VO2tot) in the obese group, as classified by WC, WHR, and WHtR, was 6%, 6.5%, and 7.8% lower than in non-obese groups, respectively. However, no significant differences were observed (
Table 2). The obese group, as classified by WC, WHR, and WHtR had lower fat oxidation by 9.3%, 21.7%, and 9.3%, respectively, but the differences were not statistically significant (
Table 3).
Based on the physical activity factor in obese group as classified by BMI, there were two groups: active obesity (Ac-Ob) and inactive obesity (IAc-Ob). Based on two factors of obesity and physical activity, there were four groups categorized by WC, WHR, and WHtR: active obesity (Ac-Ob), inactive obesity (IAc-Ob), active non-obesity (Ac-nOb), and inactive non-obesity (IAc-nOb). Participants who met inactive category were described in the inactive group whereas those who met minimally active and highly active categories were classified in the active group. Of BMI classification, the result found that VO2tot in IAc-Ob group was 7.9% lower than Ac-Ob group, but not statistically different between groups (
Table 4).
Among the other three different anthropometric indicators of obesity, there were no differences in VO2tot among four different groups classified by WC and WHtR, except WHR. The result showed that VO2tot was significantly different among four different groups classified by WHR (p = .032). After the main analysis, post-hoc analysis was performed and found that IAc-Ob group had a 28.1% significantly lower VO2tot compared to Ac-Ob group (p = .050). IAc-Ob also had a 29.2% significantly lower VO2tot than Ac-nOb group (p = .021). (
Table 4).
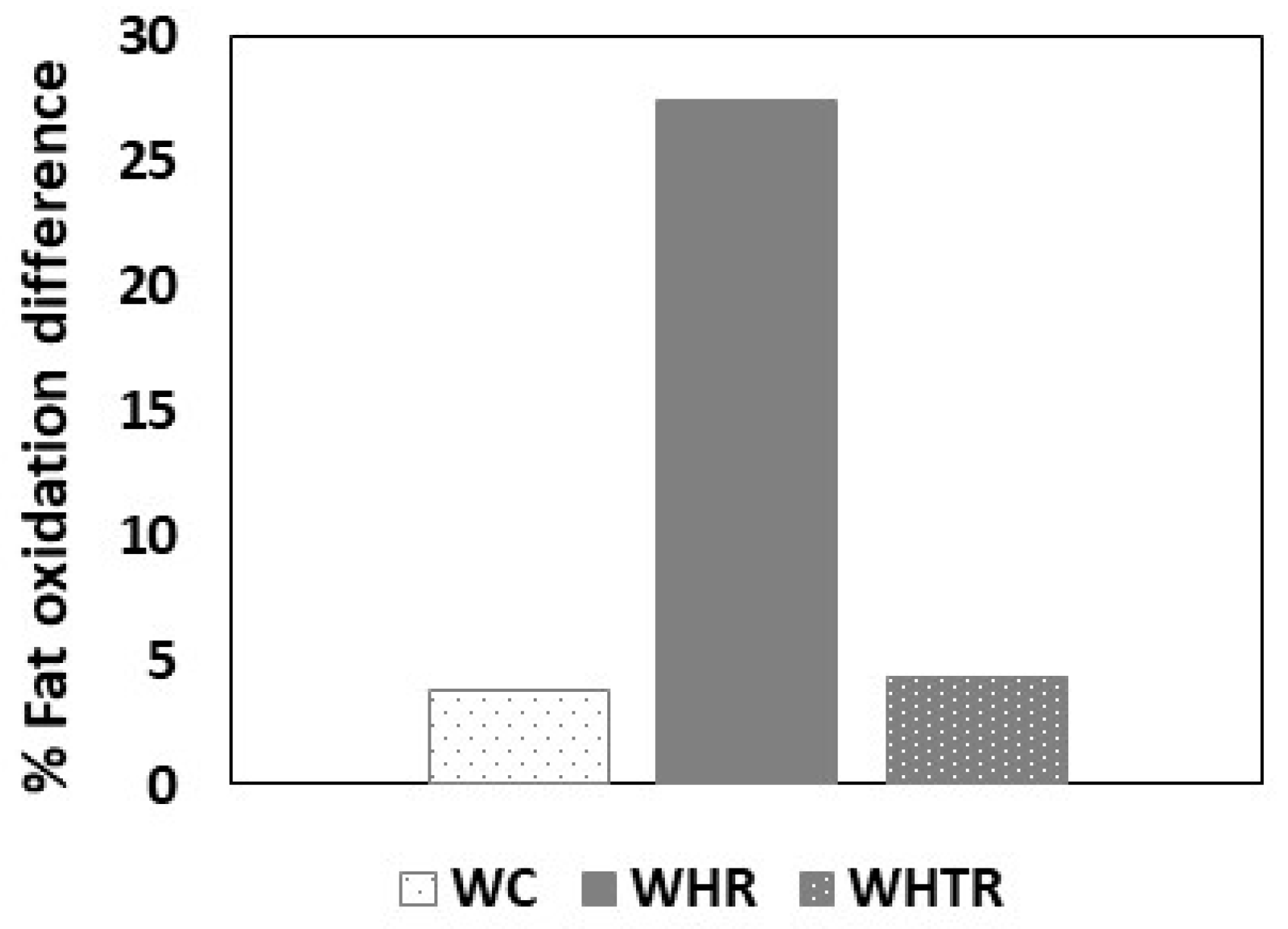
There were no differences of fat oxidation among groups, as classified by all anthropometric indicators (i.e., BMI, WC, WHR, and WHtR). Considering the percentage difference of fat oxidation between the worst-case participant (IAc-Ob) and best-case participant (Ac-nOb), the data could only be analysed based on WC, WHR, and WHtR. The result showed that the worst-case had a 3.8%, 27.4%, and 4.3% lower fat oxidation than the best-case participants, classified by WC (IAc-Ob vs Ac-nOb: 12.6 (7.3 - 17.9) vs 13.1 (5.4 - 20.7) g.min-1), WHR (IAc-Ob vs Ac-nOb: 9.8 (2.8 - 16.8) vs 13.5 (11.2 - 15.9) g.min-1), and WHtR (IAc-Ob vs Ac-nOb: 13.2 (8.4 - 18.0) vs 13.8 (8.2 - 19.4) g.min-1), respectively (
Figure 1).
4. Discussion
This study aimed to examine the impact of obesity as measured by various anthropometric indicators and physical activity level on oxygen uptake and fat oxidation during moderate intensity aerobic exercise in adults. Main findings showed that inactive obese adults as classified by WHR had poorer oxygen uptake than active obese adults and active non-obese adults. We further found the promising impact of WHR on fat oxidation as indicated by the greatest difference of the percentage of fat oxidation between the best case (active non-obese adults) than the worst case (inactive obese adults).
Poor cardiorespiratory fitness, indicated by a low level of oxygen uptake has been well-established as a strong independent predictor of cardiovascular diseases [
5,
6,
7,
41], particularly obese individuals [
8]. Evidence suggests that reduced movement in obesity can lead to poor exercise efficiency, resulting in decreased oxygen uptake and reduced fat oxidation in this population [
15,
16,
17]. Our study fails to confirm lower oxygen uptake and reduced fat oxidation in obese individuals compared to non-obese individuals. While the evidence is not entirely supportive, fat oxidation in obese individuals, as classified by WHR, tended to be lower than in non-obese individuals. Various anthropometric indicators (i.e., WC, WHR, and WHtR) have been debated as suitable determinants of health status related to obesity [
18,
21]. The finding of our study is likely to support the use of WHR as an obesity indicator. WC has been proposed as an indicator closely to central fat accumulation and intra-abdominal adipose tissue which is greatly associated with the risk of cardiometabolic diseases [
42]. In addition, several studies have shown that lower oxygen consumption was associated with the increased WC [
43,
44,
45]. Notably, our study did not find poor oxygen uptake and fat oxidation in obese individuals based on WC but rather on WHR. The finding of the current study may have been predominantly influenced by women, as they comprised nearly three-fourths of our study participants (72.9%). Women tend to store fat not only in the abdominal region but also in the hip and buttock areas [
46]. Furthermore, WHR has also been reported as a good predictor of intra-abdominal adipose tissue [
47], which correlates with cardiorespiratory fitness and strongly predicts CVD [
48]. Thus, using WHR as a surrogate marker of body fat is likely more appropriate than using WC and other indicators, especially in women.
Physical activity is inversely associated with cardiovascular disease [
23]. Particularly, obese individuals are at risk of cardiovascular disease, as scientific literature has shown a positive association between inadequate physical activity and the accumulation of excess body fat [
27]. Our finding showed a significantly higher oxygen uptake during moderate-intensity aerobic exercise in active obese individuals, as measured by WHR, than inactive obese individuals. This finding suggests that, even in the presence of obesity, oxygen availability can be preserved in obese individuals with high fitness. Active obese individuals are likely to be described as metabolically healthy obesity, which has low burden of metabolic abnormality.
A previous study has demonstrated that a higher level of physical activity is linked with metabolically healthy obesity [
49]. Considering the compelling evidence, adipose tissue dysfunction generates low-grade inflammation, which, in turn, leads to impaired mitochondrial function [
15]. This phenomenon results in lower ATP synthesis, an important substance involved in oxygen consumption during exercise. It is possible that active obese individuals may have the potential to partly maintain a normal metabolic function, as expressed by higher oxygen uptake while performing the exercise than that of inactive obese individuals. This finding is also supported by a previous work, suggesting the implementing of a physical activity program to improve cardiorespiratory fitness in obesity [
50]. Thus, physical activity is necessary to be considered as an important characteristic to prevent a transition to unhealthy obesity. Obesity and physical inactivity independently affect poor oxygen uptake and decreased fat oxidation [
8,
9,
10,
15,
16,
17].
Coexistence between obesity and physical inactivity possibly reinforces greater negative impact on such outcomes. Finding of the current study confirms poor oxygen uptake, indicating by 29.1% lower oxygen uptake in inactive obese individuals than active non-obese individuals. Our study did not reveal a significant difference in fat oxidation between the inactive obese and active non-obese groups. Although the difference was not statistically significant, the descriptive data illustrated the most substantial difference in fat oxidation between inactive obese and active non-obese individuals, with obesity classified by WHR.
This study has some limitations that should be considered. First, small sample size may not provide sufficient statistical power to detect differences in fat oxidation among the groups, as the sample size of this study was determined based on the sample size of the primary research project [
30]. Second, the finding of this study may be limited in their generalizability as the study primarily consisted of women. Third, a comparative analysis between obese and non-obese individuals based on BMI is limited. The participants of this study were obtained from our primary project which had a specific target population in obesity regarding BMI [
30]. Thus, the current study could not evaluate the impact of obesity on the outcomes of interest (i.e., oxygen uptake and fat oxidation), as classified by BMI. Further studies with more appropriate sample size, including men, and considering both obese and non-obese individuals using BMI are warranted to confirm the findings of this study.
5. Conclusions
In summary, we conclude that active obese individuals, as measured by WHR, exhibited higher oxygen uptake compared to inactive obese individuals. Moreover, inactive obese individuals showed poorer oxygen uptake than active non-obese individuals. This study suggests that measuring obesity using WHR and assessing physical activity level may provide valuable information in clinical practice for identifying health risks in adults.
Author Contributions
Conceptualization, S.N. and B.C.; methodology, S.N. and B.C.; investigation, S.N. and B.C.; data curation, S.N. and K.P.; writing—original draft preparation, S.N.; writing—review and editing, S.N., B.C. and K.P. supervision, B.C. All authors have read and agreed to the submitted version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Research Institute for Health Sciences, Chiang Mai University. (Approval number: 55/2022).
Informed Consent Statement
Written informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding authors.
Acknowledgments
This study was supported by CMU Junior Research Fellowship Program.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Obesity and overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 28 August 2021).
- The World Obesity Federation. World Obesity Atlas 2022. Available online: https://www.worldobesity.org/resources/resource-library/world-obesity-atlas-2022#:~:text=Call%20for%20Global%20Action%20Plan,living%20with%20obesity%20by%202030 (accessed on 28 August 2021).
- Sakboonyarat, B.; Pornpongsawad, C.; Sangkool, T.; Phanmanas, C.; Kesonphaet, N.; Tangthongtawi, N.; Limsakul, A.; Assavapisitkul, R.; Thangthai, T.; Janenopparkarnjana, P.; Varodomvitaya, P.; Dachoviboon, W.; Laohasara, J.; Kruthakool, N.; Limprasert, S.; Mungthin, M.; Hatthachote, P.; Rangsin, R. Trends, prevalence and associated factors of obesity among adults in a rural community in Thailand: serial cross-sectional surveys, 2012 and 2018. BMC public health. 2020, 20, 850. [CrossRef]
- Must, A.; Spadano, J.; Coakley, E.H.; Field, A.E.; Colditz, G.; Dietz, W.H. The disease burden associated with overweight and obesity. JAMA. 1999, 282, 1523–1529. [CrossRef]
- Kokkinos, P.; Faselis, C.; Samuel, I.B.H.; Pittaras, A.; Doumas, M.; Murphy, R.; Heimall, M.S.; Sui, X.; Zhang, J.; Myers, J. Cardiorespiratory fitness and mortality risk across the spectra of age, race, and sex. J Am Coll Cardiol. 2022, 80, 598–609. [CrossRef]
- Blair, S.N.; Kampert, J.B.; Kohl, H.W.; 3rd, Barlow, C.E.; Macera, C.A.; Paffenbarger, R.S.Jr.; Gibbons, L.W. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA. 1996, 276, 205–210. [CrossRef]
- Chakkera, H.A.; Angadi, S.S.; Heilman, R.L.; Kaplan, B.; Scott, R.L.; Bollempalli, H.; Cha, S.S.; Khamash, H.A.; Huskey, J.L.; Mour, G.K.; Sukumaran Nair, S.; Singer, A.L.; Reddy, K.S.; Mathur, A.K.; Moss, A.A.; Hewitt, W.R.Jr.; Qaqish, I.; Behmen, S.; Keddis, M.T.; Unzek, S.; Steidley, D.E. Cardiorespiratory fitness (peak oxygen uptake): safe and effective measure for cardiovascular screening before kidney transplant. J Am Heart Assoc. 2018, 7, e008662. [CrossRef]
- Green, S.; O'Connor, E.; Kiely, C.; O'Shea, D.; Egaña, M. Effect of obesity on oxygen uptake and cardiovascular dynamics during whole-body and leg exercise in adult males and females. Physiological reports. 2018, 6, e13705. [CrossRef]
- Drinkard, B.; McDuffie, J.; McCann, S.; Uwaifo, G.I.; Nicholson, J.; Yanovski, J. A. Relationships between walk/run performance and cardiorespiratory fitness in adolescents who are overweight. Phys Ther. 2001, 81, 1889–1896. [CrossRef]
- Wei, M.; Gibbons, L.W.; Kampert, J.B.; Nichaman, M.Z.; Blair, S.N. Low cardiorespiratory fitness and physical inactivity as predictors of mortality in men with type 2 diabetes. Ann Intern Med. 2000, 132, 605–611. [CrossRef]
- Pate, R.R.; Pratt, M.; Blair, S.N.; Haskell, W.L.; Macera, C.A.; Bouchard, C.; Buchner, D.; Ettinger, W.; Heath, G.W.; King, A.C. (1995). Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995, 273, 402–407. [CrossRef]
- Ohkawara, K.; Tanaka, S.; Miyachi, M.; Ishikawa-Takata, K.; Tabata, I. A dose-response relation between aerobic exercise and visceral fat reduction: systematic review of clinical trials. Int J Obes (Lond). 2007, 31, 1786–1797. [CrossRef]
- Donnelly, J.E.; Honas, J.J.; Smith, B.K.; Mayo, M.S.; Gibson, C.A.; Sullivan, D.K.; Lee, J.; Herrmann, S.D.; Lambourne, K.; Washburn, R.A. Aerobic exercise alone results in clinically significant weight loss for men and women: midwest exercise trial 2. Obesity (Silver Spring, Md.). 2013, 21, E219–E228. [CrossRef]
- Al Saif, A.; Alsenany, S. Aerobic and anaerobic exercise training in obese adults. J Phys Ther Sci. 2015, 27, 1697–1700. [CrossRef]
- Holloway, G.P.; Bonen, A.; Spriet, L.L. Regulation of skeletal muscle mitochondrial fatty acid metabolism in lean and obese individuals. Am J Clin Nutr. 2009, 89, 455S–462S. [CrossRef]
- Woo, K.S.; Chook, P.; Yu, C.W.; Sung, R.Y.; Qiao, M.; Leung, S.S.; Lam, C.W.; Metreweli, C.; Celermajer, D.S. Overweight in children is associated with arterial endothelial dysfunction and intima-media thickening. Int J Obes Relat Metab Disord. 2004, 28, 852–857. [CrossRef]
- Galgani, J.E.; Fernández-Verdejo, R. Pathophysiological role of metabolic flexibility on metabolic health. Obes Rev. 2021, 22, e13131. [CrossRef]
- World Health Organization. Physical Status: the use and interpretation of anthropometry: report of a world health organization (WHO) expert committee; World Health Organization: Geneva, Switzerland, 1995;854:1-452. PMID 859-483-4.
- Flegal, K.M.; Carroll, M.D.; Kuczmarski, R.J.; Johnson, C.L. Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord. 1998, 22, 39–47. [CrossRef]
- Cotes, J.E.; Chinn, D.J.; Miller, M.R. lung function, physiology measurement and application in medicine. 6th ed.; Blackwell Publishing: USA, 2006; pp. 37–39, ISBN 063-206-493-5.
- Björntorp, P. Metabolic implications of body fat distribution. Diabetes Care. 1991, 14, 1132–1143. [CrossRef]
- Physical Activity Guidelines Advisory Committee. Physical activity guidelines advisory committee report; Department of Health and Human Services: Washington, D.C., USA, 2008; pp. A1-H14.
- Blair, S.N.; Morris, J.N. Healthy hearts--and the universal benefits of being physically active: physical activity and health. Ann Epidemiol. 2009, 19, 253–256. [CrossRef]
- Reddigan, J.I.; Ardern, C.I.; Riddell, M.C.; Kuk, J.L. Relation of physical activity to cardiovascular disease mortality and the influence of cardiometabolic risk factors. Am J Cardiol. 2011, 108, 1426–1431. [CrossRef]
- Claas, S.A.; Arnett, D.K. The Role of Healthy Lifestyle in the Primordial Prevention of Cardiovascular Disease. Curr Cardiol Rep. 2016, 18, 56. [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; Graham, I.; Hall, M.S.; Hobbs, F.D.R.; Løchen, M.L.; Löllgen, H.; Marques-Vidal, P.; Perk, J.; Prescott, E.; Redon, J.; Richter, D.J.; Sattar, N.; Smulders, Y.; Tiberi, M.; van der Worp, H.B.; van Dis, I.; Verschuren, W.M.M.; Binno, S; ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016, 37, 2315–2381. [CrossRef]
- World Health Organization. Global recommendations on physical activity for health. Available online: http://apps.who.int/iris/bitstream/10665/44399/1/9789241599979_eng.pdf. (accessed on 28 August 2021).
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015, 162, 123-132. [CrossRef]
- Singh, S.; Issac, R.; Benjamin, A.I.; Kaushal, S. Prevalence and association of physical activity with obesity: an urban, community-based, cross-sectional study. Indian J Community Med. 2015, 40, 103–107. [CrossRef]
- Nantakool, S.; Punturee, K.; Konghakote, S.; Sitthichoke, C.; Phirom, K.; Chuatrakoon, B. Immediate effects of aerobic exercise and whole-body vibration on fat metabolism and cardiovascular response in obesity. Obes Facts 2023, submitted.
- Pan, W.H.; Yeh, W.T. How to define obesity? Evidence-based multiple action points for public awareness, screening, and treatment: an extension of Asian-Pacific recommendations. Asia Pac J Clin Nutr. 2008, 17, 370–374.
- Riebe, D.; Ehrman, J.K.; Liguori, G.; Magal, M. ACSM's guidelines for exercise testing and prescription, 10th ed; Wolters Kluwer Health: Philadelphia, USA, 2018; Chapter 6 General principles of exercise prescription, 143-79, ISBN 978-149-633-906-5.
- Wasserman, K.; Hansen, J.E.; Sue, D.; Whipp, B.J.; Casaburi, R. Principles of exercise testing and interpretation, 4th ed; Lippincott Williams and Wilkins: Philadelphia, USA, 2004. ISBN 7-7817-4876-3.
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; Oja, P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003, 35, 1381–1395. [CrossRef]
- Oliveira, J.M.; Spositon, T.; Rugila, D.F.; Pitta, F.; Furlanetto, K.C. Validity of the international physical activity questionnaire (short form) in adults with asthma. PLoS One. 2023, 18, e0282137. [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; Oja, P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003, 35, 1381–1395. [CrossRef]
- Ma, W.Y.; Yang, C.Y.; Shih, S.R.; Hsieh, H.J.; Hung, C.S.; Chiu, F.C.; Lin, M.S.; Liu, P.H.; Hua, C.H.; Hsein, Y.C.; Chuang, L.M.; Lin, J.W.; Wei, J.N.; Li, H.Y. Measurement of waist circumference: midabdominal or iliac crest?. Diabetes Care. 2013, 36, 1660–1666. [CrossRef]
- Qiao, Q.; Nyamdorj, R. The optimal cutoff values and their performance of waist circumference and waist-to-hip ratio for diagnosing type II diabetes. Eur J Clin Nutr. 2010, 64, 23–29. [CrossRef]
- Jia, A.H.; Xu, S.Y.; Ming, J.; Zhou, J.; Zhang, W.C.; Hao, P.R.; Ji, Q.H. [The optimal cutoff value of waist-to-height ratio in Chinese: based on cardiovascular risk and metabolic disease]. Zhonghua nei ke za zhi. 2017, 56, 822–826. [CrossRef]
- Péronnet, F.; Massicotte, D. Table of nonprotein respiratory quotient: an update. Can J Sport Sci. 1991, 16, 23-29.
- Ross, R.; Blair, S.N.; Arena, R.; Church, T.S.; Després, J.P.; Franklin, B.A.; Haskell, W.L.; Kaminsky, L.A.; Levine, B.D.; Lavie, C.J.; Myers, J.; Niebauer, J.; Sallis, R.; Sawada, S.S.; Sui, X.; Wisløff, U.; American Heart Association Physical Activity Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Council on Cardiovascular and Stroke Nursing; Council on Functional Genomics and Translational Biology; Stroke Council. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement From the American Heart Association. Circulation. 2016, 134, e653–e699. [CrossRef]
- Miyawaki, T.; Abe, M.; Yahata, K.; Kajiyama, N.; Katsuma, H.; Saito, N. (2004). Contribution of visceral fat accumulation to the risk factors for atherosclerosis in non-obese Japanese. Intern Med. 2004, 43, 1138–1144. [CrossRef]
- Dyrstad, S.M.; Edvardsen, E.; Hansen, B.H.; Anderssen, S.A. Waist circumference thresholds and cardiorespiratory fitness. J Sport Health Sci. 2019, 8, 17–22. [CrossRef]
- Ortaglia, A.; McDonald, S.M.; Supino, C.; Wirth, M.D.; Sui, X.; Bottai, M. Differential relationships between waist circumference and cardiorespiratory fitness among people with and without type 2 diabetes. Prev Med Rep. 2020, 18, 101083. [CrossRef]
- Ross, R.; Katzmarzyk, P.T. Cardiorespiratory fitness is associated with diminished total and abdominal obesity independent of body mass index. Int J Obes Relat Metab Disord. 2003, 27, 204–210. [CrossRef]
- Lemieux, S.; Prud'homme, D.; Bouchard, C.; Tremblay, A.; Després, J.P. Sex differences in the relation of visceral adipose tissue accumulation to total body fatness. Am J Clin Nutr. 1993, 58, 463–467. [CrossRef]
- Ferland, M.; Després, J.P.; Tremblay, A.; Pinault, S.; Nadeau, A.; Moorjani, S.; Lupien, P.J.; Thériault, G.; Bouchard, C. Assessment of adipose tissue distribution by computed axial tomography in obese women: association with body density and anthropometric measurements. Br J Nutr. 1989, 61, 139–148. [CrossRef]
- Rhéaume, C.; Arsenault, B.J.; Dumas, M.P.; Pérusse, L.; Tremblay, A.; Bouchard, C.; Poirier, P.; Després, J.P. Contributions of cardiorespiratory fitness and visceral adiposity to six-year changes in cardiometabolic risk markers in apparently healthy men and women. J Clin Endocrinol Metab. 2011, 96, 1462–1468. [CrossRef]
- Murlasits, Z.; Kupai, K.; Kneffel, Z. Role of physical activity and cardiorespiratory fitness in metabolically healthy obesity: a narrative review. BMJ Open Sport Exerc Med. 2022, 8, e001458. [CrossRef]
- González-Gálvez, N.; Ribeiro, J.C.; Mota, J. Cardiorespiratory fitness, obesity and physical activity in schoolchildren: the effect of mediation. Int J Environ Res Public Health. 2022, 19. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).