Submitted:
08 October 2023
Posted:
09 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
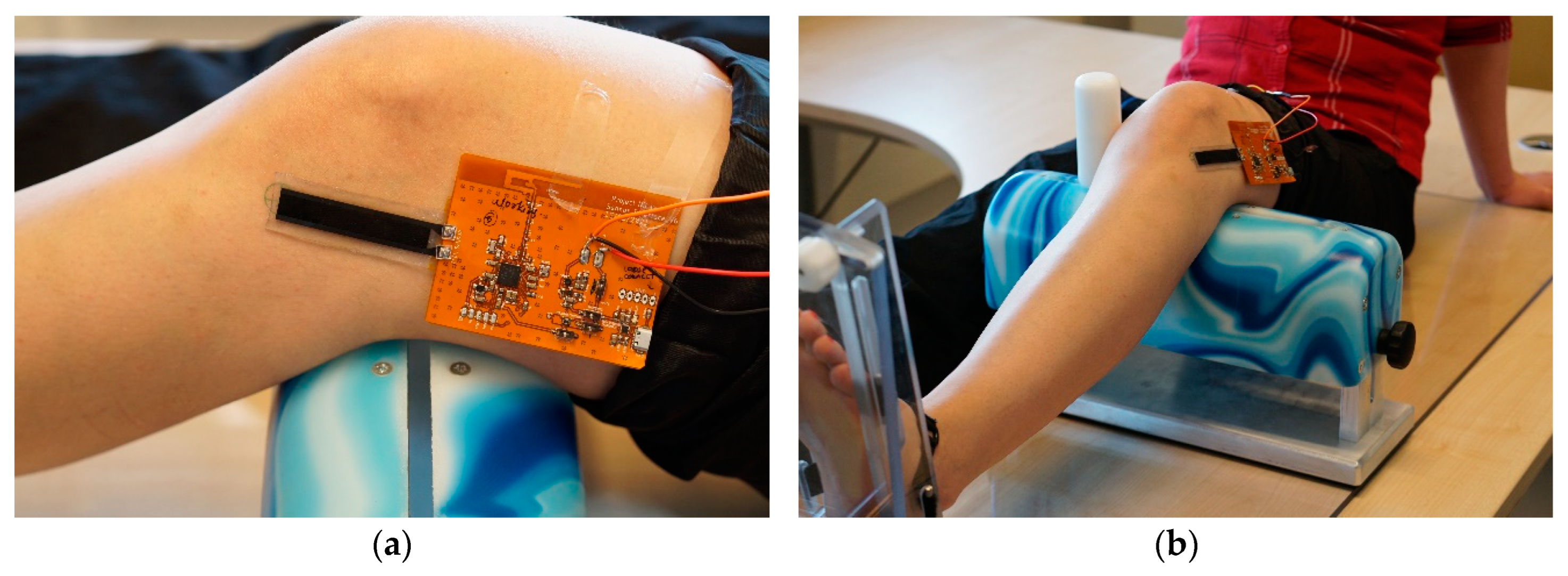
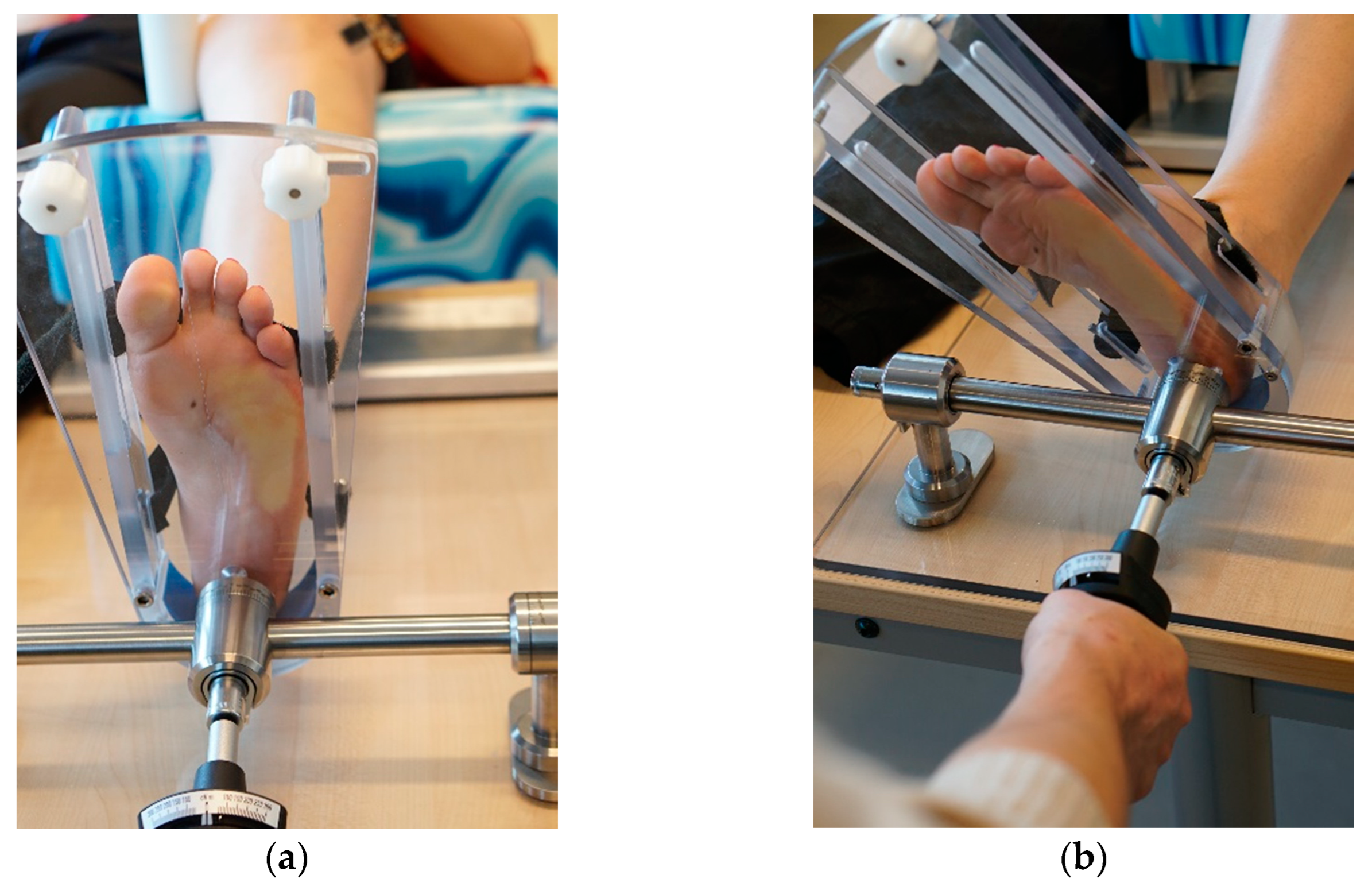
2. Materials and Methods
2.1. Materials
2.2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Boden, B.P.; Sheehan, F.T. Mechanism of non-contact acl injury: Oref clinical research award 2021. 2022, 40, 531–540. [CrossRef]
- destatis. Fallpauschalenbezogene krankenhausstatistik (drg-statistik) operationen und prozeduren der vollstationären patientinnen und patienten in krankenhäusern (4-steller) für 2021. Office, G.F.S., Ed. Wiesbaden, 2022.
- destatis. Fallpauschalenbezogene krankenhausstatistik (drg-statistik) diagnosen, prozeduren, fallpauschalen und case mix der vollstationären patientinnen und patienten in krankenhäusen für 2012. Wiesbaden, 2013.
- Evans, J.; Nielson, J.I. Anterior cruciate ligament knee injury. [updated 2022 may 5]. In: Statpearls [internet]. Treasure island (fl): Statpearls publishing; 2023 jan-. Available from: Https://www.Ncbi.Nlm.Nih.Gov/books/nbk499848/. https://www.ncbi.nlm.nih.gov/books/NBK499848/ (09-26).
- Joseph, A.M.; Collins, C.L.; Henke, N.M.; Yard, E.E.; Fields, S.K.; Comstock, R.D. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. Journal of athletic training 2013, 48, 810–817. [Google Scholar] [CrossRef]
- Imhoff, A.; Linke, R.; Baumgartner, R. Checkliste orthopädie. Thieme: Stuttgart, Germany, 2021; Vol. 4. [CrossRef]
- Lam, M.H.; Fong, D.T.; Yung, P.; Ho, E.P.; Chan, W.Y.; Chan, K.M. Knee stability assessment on anterior cruciate ligament injury: Clinical and biomechanical approaches. Sports medicine, arthroscopy, rehabilitation, therapy & technology : SMARTT 2009, 1, 20. [Google Scholar] [CrossRef]
- Wiertsema, S.H.; van Hooff, H.J.; Migchelsen, L.A.; Steultjens, M.P. Reliability of the kt1000 arthrometer and the lachman test in patients with an acl rupture. Knee 2008, 15, 107–110. [Google Scholar] [CrossRef]
- Ahldén, M.; Samuelsson, K.; Fu, F.H.; Musahl, V.; Karlsson, J. Rotatory knee laxity. Clinics in sports medicine 2013, 32, 37–46. [Google Scholar] [CrossRef]
- Zens, M.; Niemeyer, P.; Bernstein, A.; Feucht, M.J.; Kühle, J.; Südkamp, N.P.; Woias, P.; Mayr, H.O. Novel approach to dynamic knee laxity measurement using capacitive strain gauges. Knee Surgery, Sports Traumatology, Arthroscopy 2015, 23, 2868–2875. [Google Scholar] [CrossRef]
- Mayr, H.O.; Stöhr, A. [current status of instrumental measurement of knee laxity]. Arthroskopie 2010, 23, 56–61. [Google Scholar] [CrossRef]
- Lange, T.; Freiberg, A.; Dröge, P.; Lützner, J.; Schmitt, J.; Kopkow, C. The reliability of physical examination tests for the diagnosis of anterior cruciate ligament rupture – a systematic review. Manual Therapy 2015, 20, 402–411. [Google Scholar] [CrossRef]
- Kuroda, R.; Hoshino, Y.; Kubo, S.; Araki, D.; Oka, S.; Nagamune, K.; Kurosaka, M. Similarities and differences of diagnostic manual tests for anterior cruciate ligament insufficiency:A global survey and kinematics assessment. 2012, 40, 91–99. [CrossRef]
- Branch, T.P.; Mayr, H.O.; Browne, J.E.; Campbell, J.C.; Stoehr, A.; Jacobs, C.A. Instrumented examination of anterior cruciate ligament injuries: Minimizing flaws of the manual clinical examination. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2010, 26, 997–1004. [Google Scholar] [CrossRef]
- Sheeja Prakash, K.; Mayr, H.O.; Agrawal, P.; Agarwal, P.; Seidenstuecker, M.; Rosenstiel, N.; Woias, P.; Comella, L.M. Batch fabrication of a polydimethlysiloxane based stretchable capacitive strain gauge sensor for orthopedics. Polymers 2022, 14, 2326. [Google Scholar] [CrossRef]
- Mayr, H.O.; Hoell, A.; Bernstein, A.; Hube, R.; Zeiler, C.; Kalteis, T.; Suedkamp, N.P.; Stoehr, A. Validation of a measurement device for instrumented quantification of anterior translation and rotational assessment of the knee. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2011, 27, 1096–1104. [Google Scholar] [CrossRef]
- Mayr, H.O.; Hellbruegge, G.; Haasters, F.; Ipach, B.; Schmal, H.; Prall, W.C. Laxity measurement of internal knee rotation after primary anterior cruciate ligament rupture versus rerupture. Archives of Orthopaedic and Trauma Surgery 2022, 142, 2839–2847. [Google Scholar] [CrossRef] [PubMed]
- Sheeja Prakash, K.; Andersen, E.; von Einem, V.C.; Muthalagu, S.K.; Agarwal, P.; Mayr, H.O.; Seidenstuecker, M.; Rosenstiel, N.; Roundy, S.; Woias, P. , et al. Design and implementation of a wearable system based on a flexible capacitive sensor, monitoring knee laxity. Advanced Sensor Research 2023, n/a, 2300058. [Google Scholar] [CrossRef]
- Zens, M.; Niemeyer, P.; Ruhhammer, J.; Bernstein, A.; Woias, P.; Mayr, H.O.; Südkamp, N.P.; Feucht, M.J. Length changes of the anterolateral ligament during passive knee motion: A human cadaveric study. The American Journal of Sports Medicine 2015, 43, 2545–2552. [Google Scholar] [CrossRef]
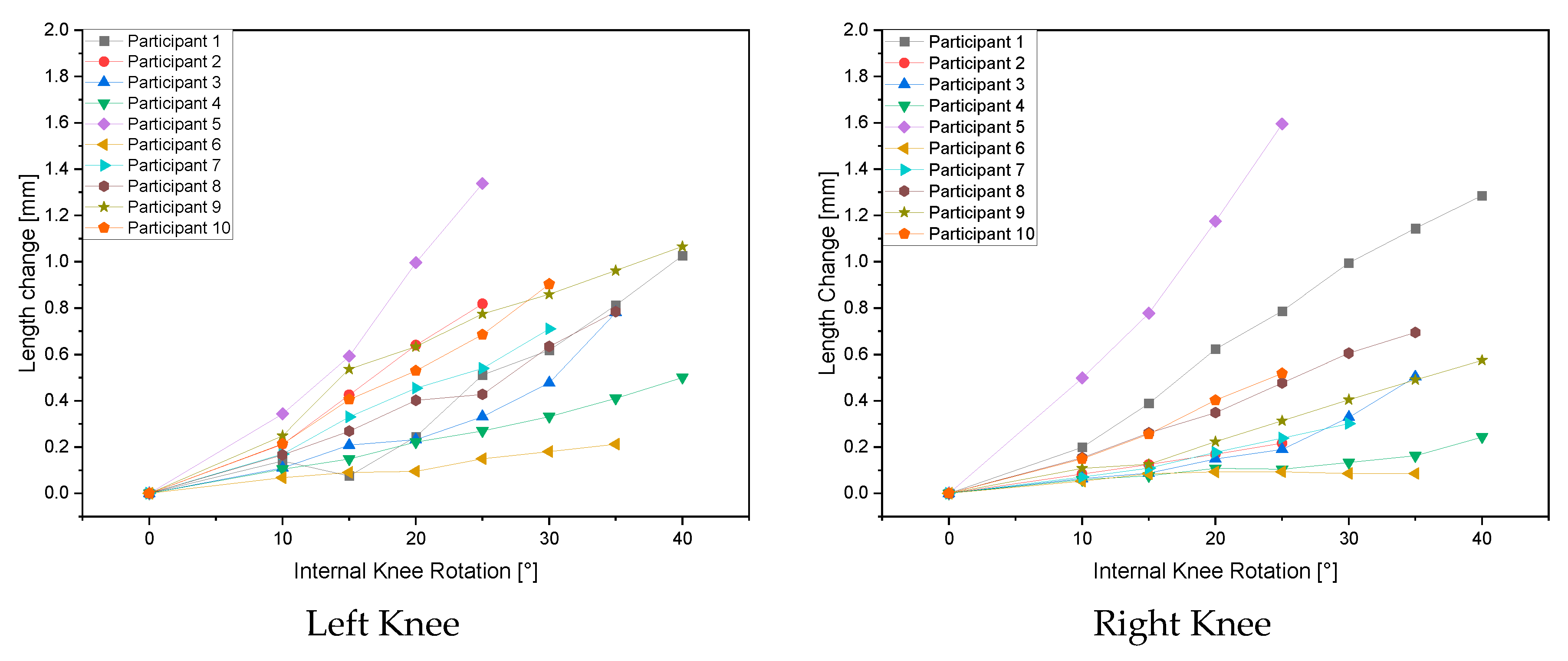
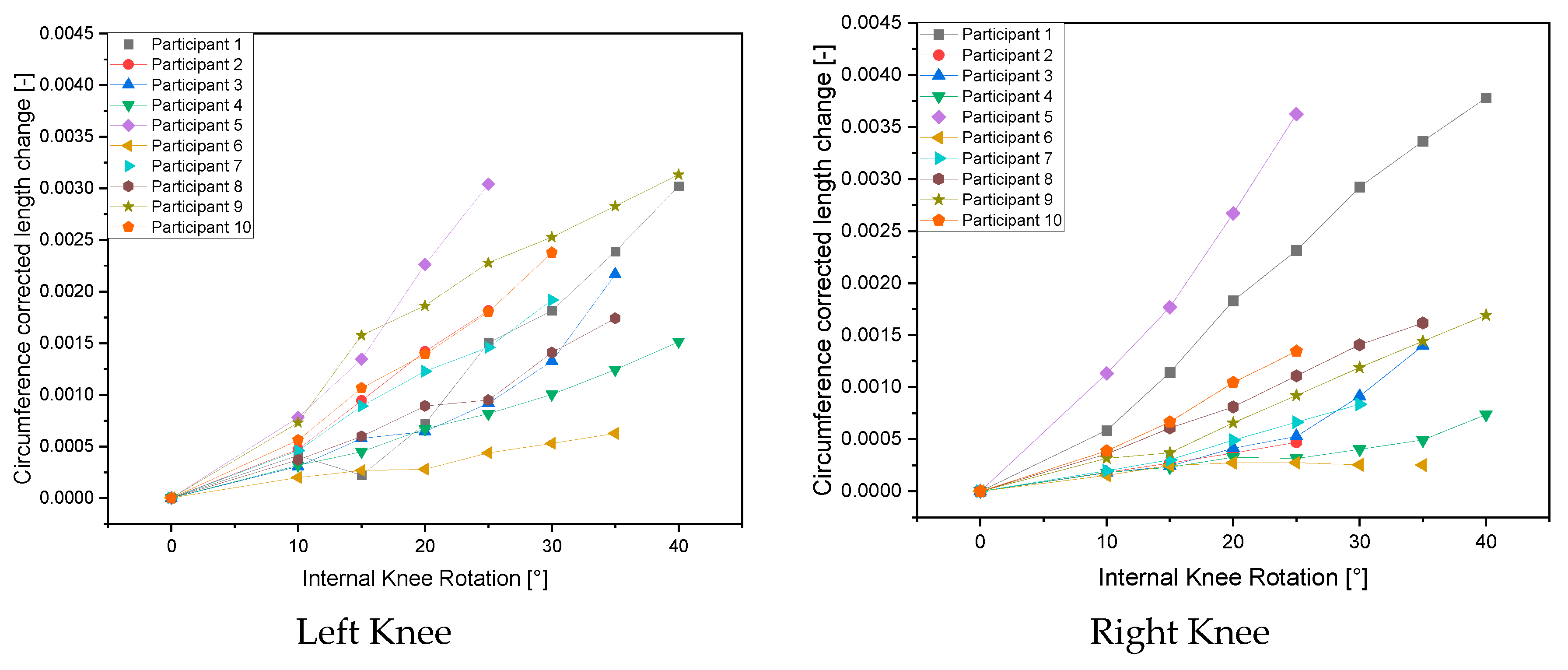
| Length Change [mm] | ||||||||
| Internal Knee Rotation | 0° | 10° | 15° | 20° | 25° | 30° | 35° | 40° |
| Left Knee Females | ||||||||
| Female 1 | 0 | 0.140 | 0.076 | 0.245 | 0.512 | 0.618 | 0.813 | 1.028 |
| Female 2 | 0 | 0.110 | 0.208 | 0.232 | 0.331 | 0.478 | 0.781 | |
| Female 3 | 0 | 0.104 | 0.148 | 0.222 | 0.270 | 0.332 | 0.410 | 0.500 |
| Female 4 | 0 | 0.166 | 0.269 | 0.402 | 0.428 | 0.635 | 0.784 | |
| Female 5 | 0 | 0.249 | 0.536 | 0.634 | 0.775 | 0.859 | 0.961 | 1.066 |
| Left Knee Males | ||||||||
| Male 1 | 0 | 0.212 | 0.426 | 0.640 | 0.818 | |||
| Male 2 | 0 | 0.344 | 0.592 | 0.996 | 1.338 | |||
| Male 3 | 0 | 0.068 | 0.091 | 0.095 | 0.149 | 0.180 | 0.213 | |
| Male 4 | 0 | 0.170 | 0.330 | 0.454 | 0.540 | 0.710 | ||
| Male 5 | 0 | 0.213 | 0.405 | 0.530 | 0.686 | 0.904 | ||
| Right Knee Females | ||||||||
| Female 1 | 0.000 | 0.199 | 0.388 | 0.623 | 0.787 | 0.994 | 1.144 | 1.285 |
| Female 2 | 0.000 | 0.064 | 0.087 | 0.149 | 0.190 | 0.329 | 0.503 | |
| Female 3 | 0.000 | 0.059 | 0.076 | 0.108 | 0.104 | 0.133 | 0.163 | 0.244 |
| Female 4 | 0.000 | 0.154 | 0.261 | 0.349 | 0.477 | 0.605 | 0.695 | |
| Female 5 | 0.000 | 0.108 | 0.126 | 0.223 | 0.313 | 0.404 | 0.490 | 0.575 |
| Right Knee Males | ||||||||
| Male 1 | 0 | 0.084 | 0.124 | 0.169 | 0.217 | |||
| Male 2 | 0 | 0.499 | 0.778 | 1.175 | 1.594 | |||
| Male 3 | 0 | 0.052 | 0.084 | 0.093 | 0.093 | 0.086 | 0.085 | |
| Male 4 | 0 | 0.071 | 0.109 | 0.177 | 0.239 | 0.301 | ||
| Male 5 | 0 | 0.149 | 0.256 | 0.402 | 0.518 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





