1. Introduction
According to the World Health Organization, there have been more than 661 million confirmed cases of COVID-19 and more than 6.7 million deaths, as of January 15, 2023 [
1]. Recent studies show that 40% to 70% of patients have residual symptoms up to 3 months after infection [
2,
3]. Currently, the persistence or appearance of symptoms for more than 4 weeks after SARS-CoV-2 infection is defined as "post-COVID-19 condition" [
4]. The most commonly observed residual clinical manifestations of the post-COVID-19 condition or syndrome at 3- to 12-month follow-up are fatigue, dyspnea, sleep disturbances, difficulty concentrating, exertional intolerance, and myalgia [
5]. According to patient self-reported statistics in the United Kingdom, fatigue remains the most common symptom (70 %), followed by difficulty concentrating (45 %), difficulty breathing (42 %) and muscle pain (42 %) [
6]. Finally, neurocognitive symptoms and fatigue are described as the most limiting and seem to have the greatest impact on patients' quality of life [
7].
In young adults a prevalence of COVID-19 of 45.3% was found, and of these 10.8% reported long-term symptoms [
8]. In a study of university students, the most frequent symptoms were exercise intolerance, dyspnea, chest pain, chemosensory impairment, lymphadenopathy, rhinitis and loss of appetite. Despite persistent symptoms, a third of the post-COVID-19 syndrome group had not contacted any healthcare professional [
9]. Probably, the lack of consultation with a physician is due to the asymptomatic form and mild presentations of symptoms in this population [
10,
11].
On the one hand, pulmonary rehabilitation has been shown to be effective as non-pharmacological treatment in post-COVID-19 patients [
12]. Generally, treatment is administered to improve ventilatory mechanics and fatigue resistance. Thus, respiratory exercises (anaerobic/aerobic) and stretching have been used to recover pulmonary function, always considering the patient's condition and vital signs [
13]. Diaphragmatic pattern breathing exercises activate inspiratory flow and volume, favoring oxygenation and airway patency [
14]. In contrast, aerobic exercise activates the immune response, increases lung tissue flexibility, improves circulation and prevents oxidative damage [
15]. Recently, it was suggested that respiratory physiotherapy combined with aerobic exercises should be included in pulmonary rehabilitation to improve cardiorespiratory fitness in post-COVID-19 patients [
16].
On the other hand, the way and speed of transmission of the virus forced the confinement, which in turn allowed the massification of remote health services "telemedicine". Telemedicine uses information and communication technologies to offer health services outside health institutions. Several studies conducted in the acute and subacute stage demonstrate that respiratory physiotherapy performed remotely improves respiratory capacity [
17,
18]. Studies of moderate quality showed that telerehabilitation “TR” is a viable and effective option to allow continuity of care. Specifically, TR has allowed maintaining the quality of rehabilitation, reducing the risk of infection and avoiding displacement [
19].
Today, there is evidence that some programs have achieved the same or higher level of recovery than face-to-face pulmonary rehabilitation programs [
20,
21,
22]. In addition, patients who received TR were equally satisfied with the health service, than patients who received traditional musculoskeletal rehabilitation [
23]. However, most of these studies were conducted in adults and older adults; consequently, there is limited knowledge about the effects of a TR program on young patients with post-COVID-19 syndrome. Thus, the aim of this study was to analyze the effects of a pulmonary TR program in young adults with post-COVID-19 syndrome. We hypothesized that respiratory and aerobic exercises can modify vital parameters, dyspnea, physical and cardiorespiratory capacity. The TR program was developed on a web page designed for this purpose. This page was used as a follow-up guide to explain the correct techniques for performing the exercises included in the pulmonary rehabilitation program.
2. Materials and Methods
2.1. Design
A longitudinal, retrospective study was conducted on students of the University. The clinical practical protocol respected the stipulated in the Declaration of Helsinki. All participants signed an informed consent form accepting the treatment. The treatment included the techniques and exercises used in the current clinical practice of pulmonary rehabilitation.
2.2. Participants
Participants were adult students (>18 years) diagnosed with post-COVID-19 syndrome by the occupational physician at the University. Thirty-seven students' medical files were analyzed. Five students did not have informed consent, two had no sequel, and 12 had persistent symptoms lasting between 4 and 12 weeks. Thus, eighteen students accomplished the inclusion criteria, but two of them did not complete the program. To be included in the study students had to: i) be aged between 18 and 30 years and ii) be diagnosed with Post-COVID-19 syndrome. Students with: i) COVID-19 in acute phase; ii) previous pulmonary diseases; iii) chronic diseases; iv) oxygen-dependent; and v) cardiological pathologies were excluded from the study. The subjects were assigned by convenience into a control group (CG) (8 subjects) and experimental groups (EG) (8 subjects), after their commitment to continue the program. The EG had access to the TR educational platform while the CG did not perform any activity, only was assessed in the same time intervals that the EG. In addition, neither patient participated in a pulmonary rehabilitation program prior to the study.
2.3. Assessments
The students were invited to complete a questionnaire conducted on Google Forms. Once the inclusion criteria verified, the students underwent a complete clinical examination by the University's Occupational Health Department. Finally, the retained participants were assessed (face to face) by a physical therapist trained in pulmonary rehabilitation, at the beginning and end of the program. Neither participants received any treatment information during the initial assessment.
The parameters assessed were: i) vital signs (oxygen saturation "SpO2", heart rate "HR", respiratory rate "RR" and blood pressure "BP"; ii) physical capacity; iii) cardiorespiratory capacity; and iv) perceived effort "dyspnea/fatigue". A finger pulse oximeter (GIMA, model XY-010, 2021) was used to measure SpO2 and HR.
Physical capacity was assessed through the number of times the subject can stand up and sit down, as quickly as possible during 1 minute (1-min Sit-to-stand Test). The test should be performed from a 46 cm high chair, without armrests, the participant's vital signs will be taken before and after the test, normal ranges are, 30 to 40 repetitions/minute [
24].
Cardiorespiratory capacity was assessed by the 6-Minute Walk Test “6MWT” using as unit the distance covered in meters. This test predicts through an equation the distance that a person should walk, taking into account gender, age and weight [
25]. Finally, the Borg Scale (0-10) was used to measure the perceived exertion during the 1-min Sit-to-stand Test and the 6MWT. This scale subjectively assesses effort (0=no effort and 10=extreme ef-fort) [
26]. All participants were assessed at two time points. The EG participants were evaluated before and after the intervention while the CG participants were evaluated at the same time periods as the EG subjects.
2.4. Intervention
A 4-week remote pulmonary rehabilitation program was developed to help the students to continue your academic program at home. Participants were required to perform three TR sessions per week until 12 sessions were completed. Each TR session was done remotely and asynchronously in students' homes. All students were assessed at the Centro de Atención y Rehabilitación en Fisioterapia “CARF” of the University, at the beginning and at the end of the program. The assessments were executed by a physical therapist trained in pulmonary rehabilitation. CARF is a university physiotherapy center that provides specialized care to the community.
Patients had to connect to a web page designed specifically for this CARF project between the two assessments. The home page contains user instructions and the therapy program spread over three links (HTTPS: //rehabilitacionpostcovid.wordpress.com/). In the first link, the instructions for the execution of the breathing exercises are presented; the aerobic exercises are in the second; and a combination of the previous exercises appears in the third. Each link contains a description of the starting position, execution, number of sets, and repetitions, as well as a video demonstration for each exercise. The use of both types of exercises is common in pulmonary rehabilitation clinical practice.
All subjects started the program at the same time, which allowed the links to be activated progressively as the treatment progressed. Selective activation prevented patients from performing exercises that did not correspond to that week. Thus, to start the program, participants had to perform only the exercises listed on the page.
The program included diaphragmatic pattern breathing exercises (4 sets of 10 repetitions, with a 1 min pause between each set) and active cycling (4 sets of 6 repetitions, with a 40 sg pause between each set), as well as aerobic and/or strength exercises (10 exercises, see
Table 1). The respiratory exercises were performed in order to re-educate the physiological breathing pattern, which in turn increases lung volumes, oxygenation and de-creases respiratory rate [
27]. Aerobic exercises were chosen because they can activate abdominal muscle synergy, leading to increased lung expansibility [
15]. The TR program was considered complete when participants accomplished the program (12 sessions).
2.5. Data analysis
The statistical analysis was performed with the SPSS, version 25.0 (IBM Corporation, Armonk, NY, USA). Quantitative variables were expressed as mean (M) and standard deviation (± SD). Qualitative variables were described as frequencies and percentages (N (%)). For the quantitative variables, the Shapiro Wilk test showed that the data set was normally distributed. An ANOVA analysis was employed (2 Groups x 2 Measures) to compare mean differences between groups. The student test was used to compare the age and persistent symptoms between the groups. Tukey's post hoc test was applied when an interaction between variables was found. Categorical data were analyzed using the Chi-square test. A value of p < .05 was considered statistically significant.
3. Results
Concerning the clinical and demographic characteristics, there were no statistically significant differences between patient groups for the variables age, sex, most important sequelae and duration of symptom persistence after overcoming COVID-19 (p > 0.05) (
Table 2).
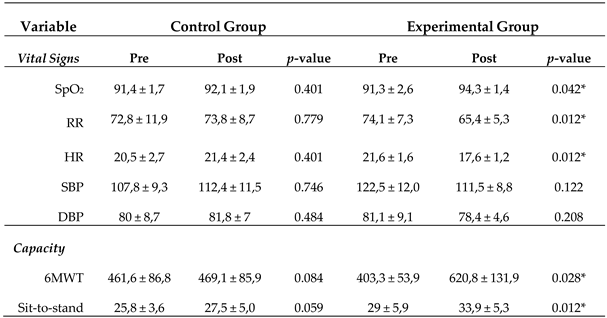
3.1. Vital signs
The Anova analysis (2 Groups X 2 Measures) did not reveal a significant interaction (F(1,14)=2.4128,
p > 0.143) for the SpO2 variable, nor for the blood pressure variable (F(1,14)=1.7527,
p > 0.207). On the contrary, a significant interaction was found for the heart (F(1,14)=7.9042,
p < 0.014) and respiratory rates (F(1,14)=18.262,
p < 0.001). Post hoc Tukey analysis showed a significant decrease in heart (
p < 0.001) and respiratory rates (
p < 0.031), after treatment in the EG. There were no significant differences between groups in any of the variables measured before treatment (
p > 0.05) (
Table 3).
3.2. Physical and cardiorespiratory capacity
A significant interaction (Group X Measurement) was found for the comparison of physical (F(1,14)=15.121,
p < 0.006) and cardiorespiratory capacities (F(1,14)=15.121,
p < 0.002). Tukey's test showed a significant increase in the number of times the subject sits on a chair for 1min, in the EG after treatment (
p < 0.002). This significant increase was also observed in the distance traveled by the EG patients (
p < 0.001). There was no significant difference between the groups before treatment (
p > 0.05) (
Table 3).
Table 3.
Pre- and post-treatment values for vital signs and physical capacity.
Table 3.
Pre- and post-treatment values for vital signs and physical capacity.
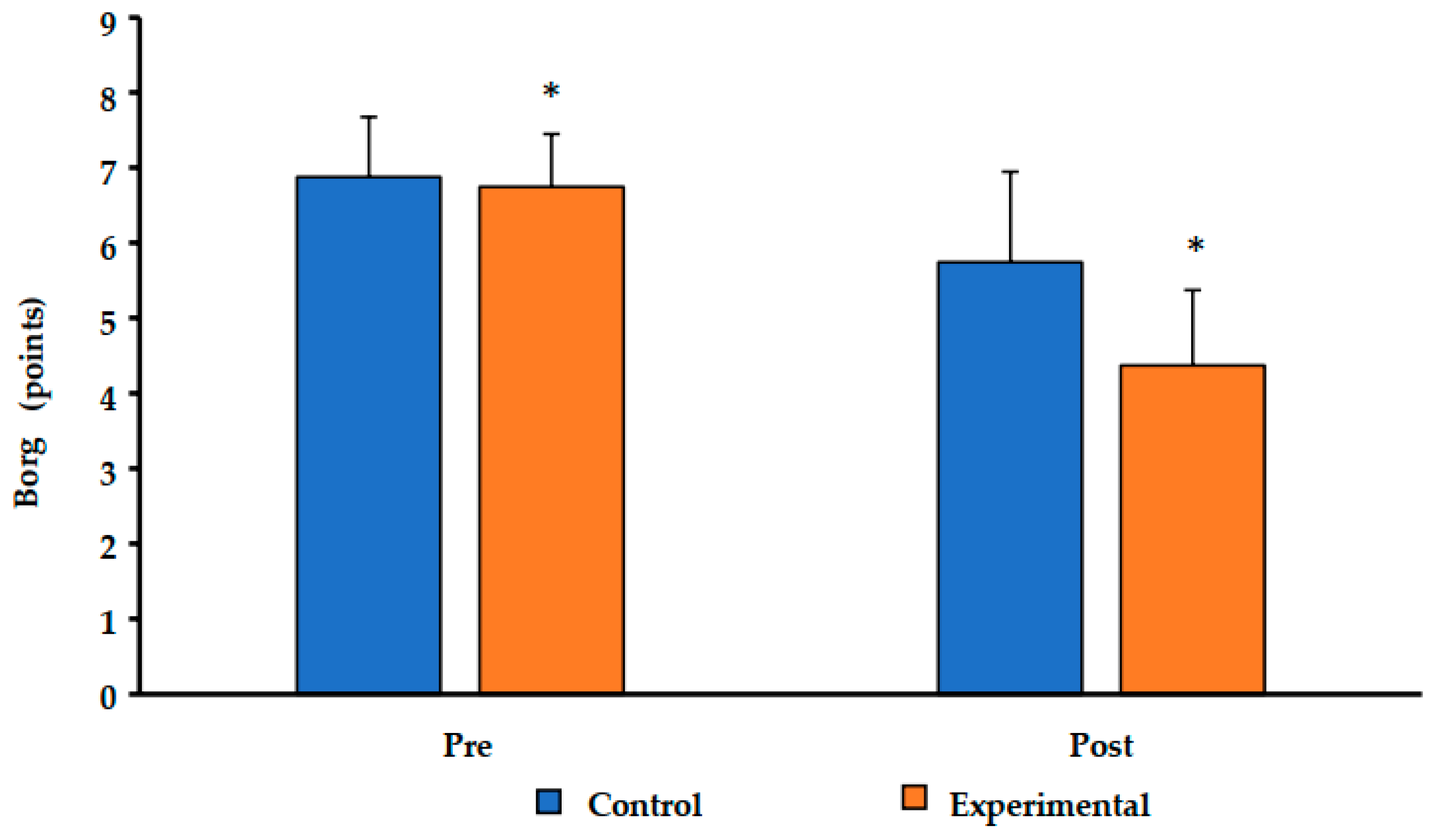
3.3. Perceived effort
The Borg Scale showed a significant interaction (Group X Measurement) to assess perceived exertion after performing the 1-min Sit-to-stand Test (F(1,14)=10.000,
p < 0.007). The post hoc test showed a significant difference between pre- and post-treatment within the groups (CG:
p < 0.006; EG
p < 0.001, respectively) (
Figure 1).
Regarding the Borg scale applied before and after the 6MWT did not show any significant interaction (F(1,14)=2,9929, p > 0.106).
4. Discussion
The aim of this pilot study was to analyze the effects of a respiratory TR program in young adults with post-COVID-19 syndrome. The results showed that respiratory together with aerobics exercises applied through a TR program decrease RF and HR improving physical and respiratory capacity in young adult patients with post-COVID-19 syndrome.
The percentage of oxygen saturation increased in both groups at the end of treatment (CG: 0.7%; EG: 2.3%). Systolic and diastolic blood pressure decreased in the EG (11; 2.7 mmHg), while it increased in the CG (4.6; 1.8 mmHg). However, none of these changes was significant. This result is consistent with a recent study that measured blood pressure continuously, showing that there are no changes in this parameter in young patients [
28]. With respect to HR and RR, these increased in the CG after treatment (HR=0.9; RR=1), whereas they decreased significantly in the EG (HR=4; RR=8.7). The decrease in these parameters in the EG could have been due to improved voluntary breathing control. Specifically, controlled breathing exercises produce a decrease in RR and HR, as well as an increase in lung volume [
29].
In relation to physical capacity (strength) and cardiorespiratory capacity (endurance), both groups increased their performance, but only the EG significantly. The EG increased the number of times it could stand up and sit down from a chair by 1.7 and the distance covered after 6 minutes by 7.5 meters. The improvement in physical and cardiorespiratory capacity in the CG may be due to the spontaneous recovery experienced by the young subjects. The EG significantly increased physical (4.9) and cardiorespiratory (217.5 mts) capacity to perform these activities. This increase in physical capacity is consistent with the results found by Dalbosco-Salas et al. [
13] in an observational study consisting of 24 TR treatment sessions. However, our average difference was higher (+ 3.2 times), this could be due to the age of the subjects (21.7 vs. 55.6 years), as the treatment was similar. Age has an impact on the process of transcriptional variability of immune cells (T, B, NK) and inflammatory mediators (TNF)-α (IL)-8. Specifically, with age the function and efficacy of immune cells is affected, generating inflammation in tissues, despite the absence of infection. Young people have fewer inflammatory markers and more functional immune cells, thus contributing to a faster recovery. An example is the radiological sign "ground glass" characteristic of COVID-19. This sign is associated with the accumulation of inflammatory exudate, which in the elderly remained after the acute phase, while in the young disappeared [
30]. In any case, increased cardiorespiratory capacity has already been reported in post-COVID-19 patients in the acute phase after respiratory and aerobic exercise [
31].
Finally, perceived exertion (fatigue) decreased in both groups after the evaluation of physical and respiratory capacities. However, this decrease was statistically significant only after performing the 1-min Sit-to-stand Test (CG: 1.1; EG 2.4 points). Probably, the 6MWT it is not sufficiently demanding enough to cause fatigue during exertion or the respiratory and aerobic exercises improved fatigue tolerance. The 6MWT and Sit-to-stand are generally used as the primary tests to quantify physical and cardiorespiratory fitness. However, a recent study that used a spirometer to quantify respiratory function in isolation found no significant differences between two groups, despite the fact that the 6MWT and Sit-to-stand Tests presented significant differences. The authors suggested that 6MWT and Sit-to-stand provide more information on cardiovascular response than respiratory response. Therefore, to assess respiratory function in isolation and reliably, the use of a spirometer is essential [
32].
This is one of the first studies in young adults considering post-COVID-19 syndrome by TR. However, this study is not without limitations. The sample of positive students is small, although consistent with positivity rates on the college campus. Given the low specificity rates of PCR testing, we cannot say with confidence that all students who tested negative for COVID-19 and were never diagnosed by a physician did not have the disease. In addition, the population may not be representative because students belong to a higher socio-economic status. Individuals with higher status are less affected by COVID-19 [
33]. Finally, the lack of objective information on COVID-19 in this age group also constitutes a limit to the study.
This study contributes with preliminary data about the physical and functional characteristics of young patients with post-COVID-19. It also confirms the Silva-Santos et al., suggestion [
16] to implement a pulmonary rehabilitation program that includes pulmonary physiotherapy and aerobic exercises at the same time. Moreover, we can point out that the variety of exercises included in this TR program allows patients to maintain their interest. This adherence to the program means that the training sessions are not perceived as repetitive. Additionally, the design and configuration of the platform is user-friendly and easy to access. Further studies recruiting a larger and more representative population are needed to verify our findings.
5. Conclusion
The application of respiratory and aerobic exercises in a TR program can lead to improvements in SpO2, physical and cardiorespiratory capacities in young patients with post-COVID-19 syndrome. Convergently, parameters such as HR, RR and dyspnea were reduced. It seems that the 6MWT is not a reliable indicator of perceived effort in young patients. The current study suggests that a TR program that involves breathing and aerobics exercises is feasible and effective in treating post-COVID-19 syndrome in young patients.
References
- “WHO Coronavirus (COVID-19) Dashboard | WHO Coronavirus (COVID-19) Dashboard “With Vaccination Data.” https://covid19.who.int/. (accessed on 29 January 2023).
- De-las-Peñas, C. F., Palacios-Ceña, D., Gómez-Mayordomo, V., Cuadrado, M. L., & Florencio, L. L. Defining post-covid symptoms (Post-acute covid, long covid, persistent post-covid): An integrative classification. Int J Environ Res Public Health. 2021, 18(5), 1-9. [CrossRef]
- Chen, C., Haupert, S. R., Zimmermann, L., Shi, X., Fritsche, L. G., & Mukherjee, B. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: A meta-analysis and systematic review. J Infect Dis. 2022, 226(9), 1593-1607. [CrossRef]
- Soriano, J. B., Murthy, S., Marshall, J. C., Relan, P., & Diaz, J. V. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2022, 22(4), e102-e107. [CrossRef]
- Alkodaymi, M. S., Omrani, O. A., Fawzy, N. A., Abou Shaar, B., Almamlouk, R., Riaz, M., .. & Tleyjeh, I. M. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: A systematic review and meta-analysis. Clin Microbiol Infect. 2022, 28(5), 657-666. [CrossRef]
- UK Office for National Statistics, “Prevalence of ongoing symptoms following coronavirus (COVID-19) infection.” https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/3november2022 (accessed 11 July 2023).
- Halpin, S. J., McIvor, C., Whyatt, G., Adams, A., Harvey, O., McLean, L., .. & Sivan, M. Postdischarge symptoms and reha-bilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J Med Virol. 2021, 93(2), 1013-1022. [CrossRef]
- Ekström, S., Andersson, N., Lövquist, A., Lauber, A., Georgelis, A., Kull, I., .. & Bergström, A. COVID-19 among young adults in Sweden: Self-reported long-term symptoms and associated factors. Scand J Public Health. 2022, 50(1), 85-93. [CrossRef]
- Walsh-Messinger, J., Manis, H., Vrabec, A., Sizemore, J., Bishof, K., Debidda, M., .. & Greenspan, N. The kids are not al-right: A preliminary report of post-COVID syndrome in university students. J Am Coll Health. 2021, 71(5), 1367-1373. [CrossRef]
- Hageman, J.R. Long COVID-19 or post-acute sequelae of SARS-CoV-2 infection in children, adolescents, and young adults. Pediatr Ann. 2021, 50(6), e232–e233. [Google Scholar] [CrossRef]
- Guan, W. J., Ni, Z. Y., Hu, Y., Liang, W. H., Ou, C. Q., He, J. X., .. & Zhong, N. S. Clinical characteristics of coronavirus dis-ease 2019 in China. N Engl J Med. 2020, 382(18), 1708-1720. [CrossRef]
- Chandan, J. S., Brown, K., Simms-Williams, N., Camaradou, J., Bashir, N., Heining, D., .. & Haroon, S. Non-pharmacological therapies for postviral syndromes, including Long COVID: A systematic review and meta-analysis proto-col. BMJ open. 2022, 12(4), e057885. [CrossRef]
- Dalbosco-Salas, M., Torres-Castro, R., Rojas Leyton, A., Morales Zapata, F., Henriquez Salazar, E., Espinoza Bastias, G., .. & Vilaro, J. Effectiveness of a primary care telerehabilitation program for post-COVID-19 patients: A feasibility study. Journal of clinical medicine. J Clin Med. 2021, 10(19), 4428. [CrossRef]
- Niro, F., Dubuc, B., Sodeifi, K. G., & Jensen, D. Effect of end-inspiratory lung volume and breathing pattern on neural acti-vation of the diaphragm and extra-diaphragmatic inspiratory muscles in healthy adults. J Appl Physiol, 2021, 131(6), 1679-1690. [CrossRef]
- Alawna, M., Amro, M., & Mohamed, A. A. Aerobic exercises recommendations and specifications for patients with COVID-19: A systematic review. Eur Rev Med Pharmacol Sci. 2020, 24(24), 13049-13055. [CrossRef]
- Silva-Santos, S., Monteiro, A. M., Barbosa, T. M., Teixeira, J. E., Branquinho, L., Ferraz, R., & Forte, P. Associations between Coronavirus and Immune Response, Cardiorespiratory Fitness Rehabilitation and Physical Activity: A Brief Report. Int J Environ Res Public Health. 2023, 20(5), 4651. [CrossRef]
- Martin, I., Braem, F., Baudet, L., Poncin, W., Fizaine, S., Aboubakar, F., .. & Reychler, G. Follow-up of functional exercise capacity in patients with COVID-19: It is improved by telerehabilitation. Respir Med. 2021, 183, 106438. [CrossRef]
- Pastora-Bernal, J. M., Estebanez-Pérez, M. J., Molina-Torres, G., García-López, F. J., Sobrino-Sánchez, R., & Martín-Valero, R. Telerehabilitation intervention in patients with covid-19 after hospital discharge to improve functional capacity and quality of life. Study protocol for a multicenter randomized clinical trial. Int J Environ Res Public Health. 2021, 18(6), 1-12. [CrossRef]
- Brigo, E., Rintala, A., Kossi, O., Verwaest, F., Vanhoof, O., Feys, P., & Bonnechère, B. Using telehealth to guarantee the continuity of rehabilitation during the COVID-19 pandemic: A systematic review. Int J Environ Res Public Health. 2022, 19(16), 10325. [CrossRef]
- Cancino-López, J., Vergara, P. Z., Dinamarca, B. L., Contreras, P. F., Cárcamo, L. M., Ibarra, N. C., & Soto-Sánchez, J. Tele-rehabilitation is effective to recover functionality and increase skeletal muscle mass index in COVID-19 survivors. Int J Telereha-bil. 2021, 13(2) e6415. [CrossRef]
- Dalbosco-Salas, M., Torres-Castro, R., Rojas Leyton, A., Morales Zapata, F., Henriquez Salazar, E., Espinoza Bastias, G., .. & Vilaro, J. Effectiveness of a primary care telerehabilitation program for post-COVID-19 patients: A feasibility study. J Clin Med. 2021, 10(19) 4428. [CrossRef]
- Pehlivan, E., Palalı, İ., Atan, S. G., Turan, D., Çınarka, H., & Çetinkaya, E. The effectiveness of POST-DISCHARGE telereha-bilitation practices in COVID-19 patients: Tele-COVID study-randomized controlled trial. Ann Thorac Med. 2022, 17(2), 110–117. [CrossRef]
- Cieślik, B., Kuligowski, T., Cacciante, L., & Kiper, P. The Impact of Personality Traits on Patient Satisfaction after Telere-habilitation: A Comparative Study of Remote and Face-to-Face Musculoskeletal Rehabilitation during COVID-19 Lockdown.Int J Environ Res Public Health. 2023, 20(6), 5019. [CrossRef]
- Strassmann, A., Steurer-Stey, C., Lana, K. D., Zoller, M., Turk, A. J., Suter, P., & Puhan, M. A. Population-based reference values for the 1-min sit-to-stand test. Int J Public Health. 2013, 58(6), 949–953. [CrossRef]
- Guyatt, G. H., Sullivan, M. J., Thompson, P. J., Fallen, E. L., Pugsley, S. O., Taylor, D. W., & Berman, L. B. The 6-minute walk: A new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985, 132(8), 919.
- Borg, G. A. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982. 14(5), 377-381. [CrossRef]
- Mendes, L. P., Moraes, K. S., Hoffman, M., Vieira, D. S., Ribeiro-Samora, G. A., Lage, S. M., .. & Parreira, V. F. Effects of diaphragmatic breathing with and without pursed-lips breathing in subjects with COPD. Respir Care. 2019, 64(2), 136–144. [CrossRef]
- Nandadeva, D., Skow, R. J., Grotle, A. K., Stephens, B. Y., Young, B. E., & Fadel, P. J. Impact of COVID-19 on ambulatory blood pressure in young adults: A cross-sectional analysis investigating time since diagnosis. J Appl Physiol. 2022, 133(1), 183–190. [CrossRef]
- Nicolò, A., Massaroni, C., Schena, E., & Sacchetti, M. The importance of respiratory rate monitoring: From healthcare to sport and exercise. Sensors, 2020, 20(21), 1–45. [CrossRef]
- Zheng, Y., Liu, X., Le, W., Xie, L., Li, H., Wen, W., .. & Su, W. A human circulating immune cell landscape in aging and COVID-19. Protein & Cell, 2020, 11(10), 740–770. [CrossRef]
- Barman, A., Sinha, M. K., Sahoo, J., Jena, D., & Patel, V. (2022). Respiratory rehabilitation in patients recovering from se-vere acute respiratory syndrome: A systematic review and meta-analysis. Heart & Lung, 2022, 53, 11–24. [CrossRef]
- Bernal-Utrera, C., Montero-Almagro, G., Anarte-Lazo, E., Gonzalez-Gerez, J. J., Rodriguez-Blanco, C., & Saa-vedra-Hernandez, M. Therapeutic Exercise Interventions through Telerehabilitation in Patients with Post COVID-19 Symptoms: A Systematic Review. J Clin Med. 2022, 11(24), 7521. [CrossRef]
- Lancaster, E., Byrd, K., Ai, Y., & Lee, J. Socioeconomic status correlations with confirmed COVID-19 cases and SARS-CoV-2 wastewater concentrations in small-medium sized communities. Environ Res. 2022, 215, 114290. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).