Introduction
Suicide is a relatively rare event in pediatric population, but its prevalence increases during adolescence and it is highly lethal (1). The World Health Organization states that suicide is the fourth leading cause of death among 15- to 29-year-olds (2) and the United Nations International Children’s Emergency Fund in “The State of the World’s Children 2021” highlights that suicide is the second leading cause of death among 15 to 19-years-olds in Europe (3). Almost 1200 youth between the age of 10 and 19 years die by suicide every year in Europe (3). According to the Centers for Disease Control and Prevention (CDC) 2018 suicide is the second most common cause of death among 10-14 and 20 to 34-year-olds in USA (4). Suicide in youth is globally recognized as an important public health problem (2).
Poisoning by pesticides represents the 20% of suicides in low- and middle-income countries (2) but there are large differences between countries and genders in suicide attempt methods (5)(6). In a 15 European Countries analyses, Värnik et al. (6) claimed that hanging and jumping from height were respectively the first and the second suicide method for both genders in people between 15 and 24 years of age, followed by using moving vehicle for males and poisoning for females. According to Kolves at all, the most frequent suicide method in children and adolescent aged 10-19 years in different countries worldwide is hanging. In this last paper, jumping from height is also an important alternative method (5).
Many recent studies in literature confirm a significant increase in mental health disease in children and adolescent from the beginning of COVID-19 pandemic (7)(8)(9)(10)(11)(12)(13)(14)(15)(16)(17) with a rise of suicidal ideation and suicide attempts.
According to Mayne et al. pre and post pandemic study, suicide screeners show an increased risk from 6.1% to 7.1% (PR: 1.16, 95% CI: 1.08-1.26), with a 34% relative increase in reporting recent suicidal thoughts among female adolescents (PR: 1.34, 95% CI: 1.18-1.52). Study results underscore a major increase in depression and suicide concerns post pandemic (14).
From the beginning of COVID-19 pandemic, admission of patients with mood disorders, self-injurious behaviors and suicidal ideation significant increased also in our hospital (16). We noted a significative increase in suicidal attempts by jumping from height in adolescent patients, comparing data with pre covid situation. Many of these suicidal jumpers attempts resulted in vertebral fractures.
There are few studies on type of injuries associated with falls from heights in pediatric patients because it’s rare. In general, traumatic spinal injuries in pediatric population are uncommon and are frequently related to motor vehicle crash (18)(19). In patients younger than 4 years of age most of vertebral fractures involves the upper cervical spine (C0-C4) (20) and this is due to anatomical age related conditions. Thoracic spine is the most common localization of spine fractures in general pediatric population, followed by lumbar spine (21)(22). Conservative treatment, for 6 to 8 weeks with a thoraco-lumbo-sacral orthosis, is the gold standard for stable fractures (21)(23) and neurological impairment is reported in about 5% of cases (21) and it is considered a risk factor for progressive spinal deformity (23).
The care of vertebral fractures in suicidal jumpers is peculiar and must consider the issues of mental health of patients.
Material and Methods
In this retrospective study, we reviewed all patients treated at Bambino Gesù Children’s Hospital Emergency Department in Rome from April 1, 2017 to March 31, 2023 for suicidal attempt. We compared the three-year post COVID 19 pandemic beginning with the three-year period before pandemic. Italian government imposed a national lockdown on March 9, 2020 but in this study we decided to start the pandemic period from April 1, about 1 month after, to better highlights the effects. Only patients with vertebral fractures for a suicidal attempt were included. Fracture classification, treatment and mid-term follow up were analyzed.
Thoracolumbar, subaxial cervical and sacropelvic fractures were classified according to AO Spine (24)(25)(26) and cervical fractures were classified by Anderson-D’Alonso Classification (27). We decided treatment according to grade of fracture instability, neurological impairment and psychiatric treatment needed.
Usually, these patients require an immediate and prolonged psychiatric treatment with long hospitalization period in dedicated wards. The possibility of early mobilization of patient without orthosis is paramount to begin successful psychiatric rehabilitation treatment and in many “borderline” spine fractures we opted for percutaneous surgical treatment to avoid long bracing treatment. We defined as “borderline” the vertebral fractures without neurological impairment that in a patient without psychiatric issues could be treated with a prolonged orthosis or cast immobilization and instead we treated with a percutaneous internal stabilization in patients with a recent suicidal attempt.
Results
At Bambino Gesu’ Children Hospital there were 141 cases of suicidal attempts from April 1, 2017 to March 31, 2020 and 5 (2,8%) of these were suicidal jumpers; none of them reported vertebral fractures.
From April 1, 2020 to March 31, 2023, there were 362 suicidal attempts with 19 (5,2%) suicidal jumpers. Twelve (63,2%) of the suicidal jumpers had a vertebral fracture (M: F=4:8) (
Table 1).
The mean age were 14 years (range 10 to 16). Only two patients had a neuropsychiatric diagnosis before the suicide attempt (16,6%). The most common level of fracture was L1 (6 cases). Thoracic spine was involved in four cases and lumbar spine in ten. Hospitalization period ranged from 12 to 210 days, with high variability mostly due to neuropsychiatric care.
According to AO-Spine Thoracolumbar Classification (24), there were: 5 A0, 10 A1, 3 A3 and 5 A4 vertebral fractures, alone or in association (
Table 1). Moreover, there were an “U shaped sacral fracture” (C3 AO-Spine) (26), a transforaminal sacral fracture (B3 AO-Spine) (26), a coccyx fracture (A1 AO-Spine) (26) and an Anderson-D’Alonso C2 type II fracture (27).
In the latter case, a burst C5 fracture (A4 AO-Spine) and a compression C6 fracture (A1 AO-Spine) (25) were associated with the C2 fracture and she was conservatively treated with a Halo-Vest for 3 months.
Only two patients with thoracolumbar A0 and A1 types of fractures (cases 4 and 5,
Table 1) were conservatively treated with a rigid thoracolumbar orthosis for 3 months with good compliance and results. Percutaneous pedicle fixation was applied in seven patients with an indirect decompression and to restore a better sagittal balance (images case 6 and 10,
Table 1). Only in two cases there were a neurological impairment. In both cases an open spinal decompression and posterior spinal fusion was performed open. All surgically treated patients used a soft spine orthosis for 1 month to facilitate early mobilization and to reduce muscular pain.
All patients had other appendicular fractures or other injuries that in some cases needed a surgical treatment. Eight patients underwent other procedures: seven orthopedic surgeries for appendicular fractures, one maxillofacial surgery for an orbital floor fracture, one vascular and one proctological surgery. Many different medical specialties were involved in these patients’ care.
Four patients had preoperative neurologic deficits: the first patient (case 1,
Table 1) presented with a diffuse axonal injury and a left hemiparesis that completely recovered in 4 months; the second one (case 3,
Table 1) had a transitory right peroneal nerve palsy; the third one (case 6,
Table 1) had a paraplegia and complete neurogenic bowel and bladder dysfunction; the latter had a complete neurogenic bowel and bladder dysfunction which improving in the last month (case 12,
Table 1).
At the last follow-up, the third patient has a persistent complete sphincter deficiency and a partial recovery of paraplegia. Nowadays, she can walk with crutches for short distances. Otherwise the latter patient only has a urinary retention.
One years after trauma, four patients underwent implant removal surgery (cases 1, 2, 3 and 8,
Table 1) with excellent clinical and radiological results. All these patients resumed their daily activities, including sports.
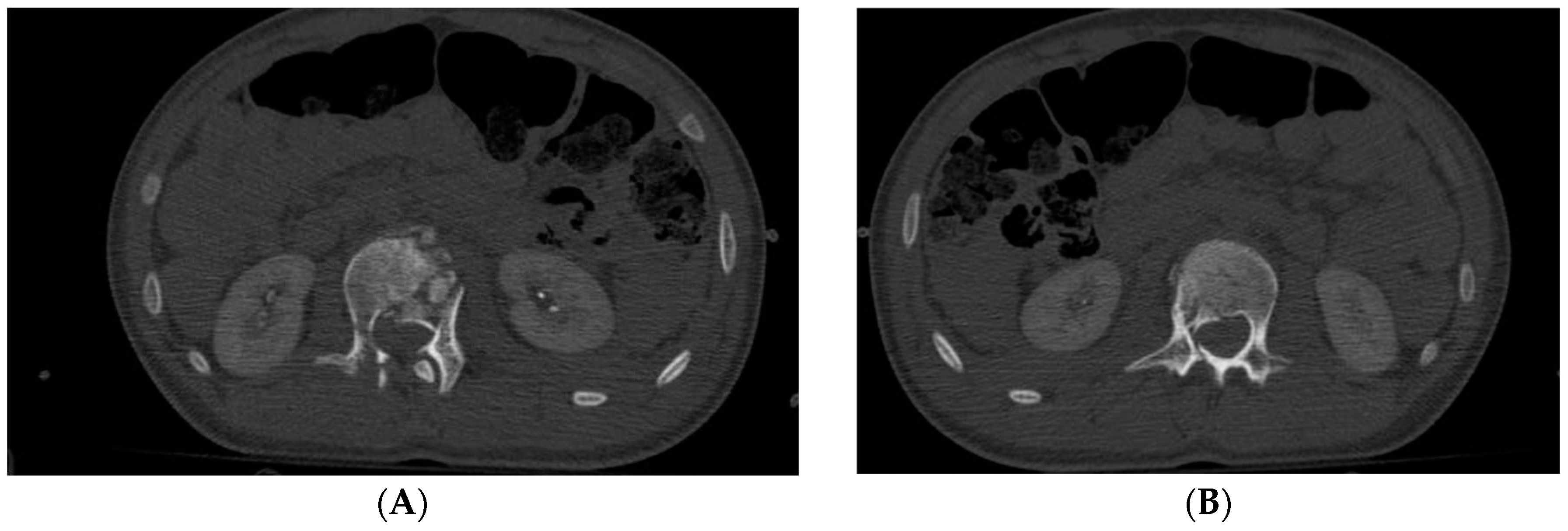
Figure 1.
Case 6 (
Table 1), (
A,
B) preoperative axial CT scan of L1 and L2, (
C) preoperative sagittal CT scan of lumbar spine, (
D,
E) anteroposterior and lateral Xray of lumbar spine after surgery, (
F) Sagittal CT scan of post traumatic cervical spine, (
G) Xray lateral view in Halo-Vest.
Figure 1.
Case 6 (
Table 1), (
A,
B) preoperative axial CT scan of L1 and L2, (
C) preoperative sagittal CT scan of lumbar spine, (
D,
E) anteroposterior and lateral Xray of lumbar spine after surgery, (
F) Sagittal CT scan of post traumatic cervical spine, (
G) Xray lateral view in Halo-Vest.
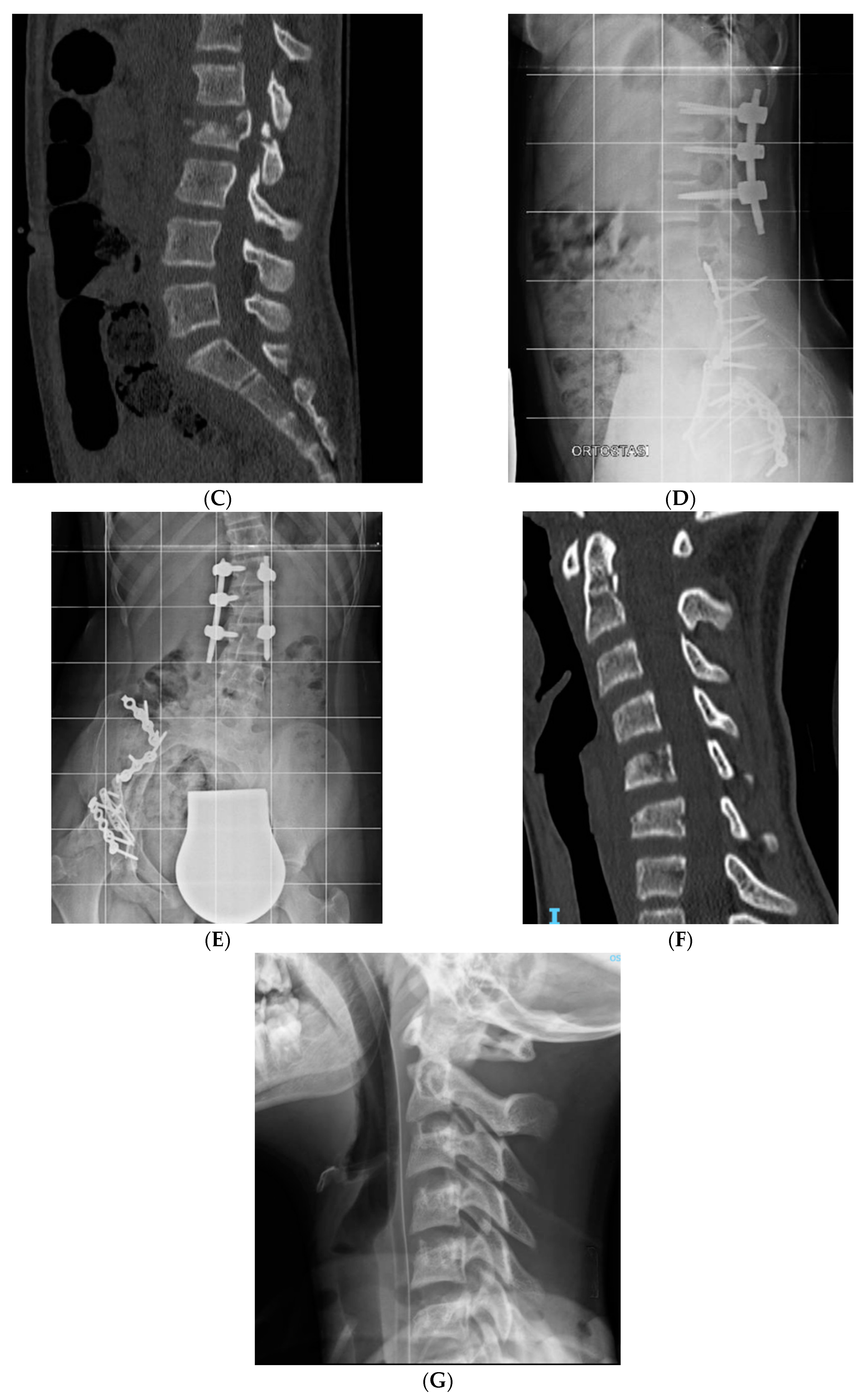
Figure 2.
Case 10 (
Table 1), (
A) preoperative axial CT scan of L5, (
B) preoperative axial CT scan of L2, (
C) preoperative sagittal CT scan of lumbar spine, (
D) post operative Xray lateral view in sitting position.
Figure 2.
Case 10 (
Table 1), (
A) preoperative axial CT scan of L5, (
B) preoperative axial CT scan of L2, (
C) preoperative sagittal CT scan of lumbar spine, (
D) post operative Xray lateral view in sitting position.
Discussion
Recent literature highlights concern about the consequences of COVID-19 pandemic on pediatric population mental health (7)(8)(9)(10)(11)(12)(13)(14)(15)(16). In this study, the comparison between 3 years before and 3 after pandemic is sufficient to demonstrate a sharp increase of suicidal attempts. Comparing the two periods, after pandemic suicidal attempts increased by 61,1% and suicidal jumpers increased by 73,7%. In the 3 years before pandemic no vertebral fracture in suicidal jumpers were noted. Otherwise, in the other 3 years analyzed, during pandemic, 63,2% of suicidal jumpers reported vertebral fractures.
To our knowledge, this is the first study that shows a significant increase in suicide jumping attempts and a related increase of vertebral fractures in pediatric patients after pandemic.
Regarding the twelve patients included in the study and according to literature concerns about the increase in neuropsychiatric diseases, only 16,6% had a previous neuropsychiatric diagnosis. Even if it is not statistically significate, considering limited timeframe and low number of patients involved, in our opinion, this raw data shows the devastating effect of COVID-19 crisis on social environment and behavioral habits of youngest Italian population.
As personal consideration, by senior author (Marco Crostelli) experience in the previous 40 years before pandemic and also by younger authors more recent experience before COVID-19 spreading, authors cannot report a single case of spine fractures in suicidal attempts in young patient.
In this study, different types of vertebral fractures were found and most of them were surgically treated (83,3%). The pattern of fractures presented in this study were similar to high energy spine fractures due to other kind of injuries (i.e. motor vehicle crash), but their frequent recurrence in a relatively short period of time is a new finding. Some of fractures treated are rare in pediatric population (i.e. spinopelvic dissociation) and are more frequent in jumping from height in adult. Sacral fractures are about 0,16% of all pediatric trauma (28) and cervical fractures are also rare and different according to the age (29). Only 1.5% of pediatric trauma cause cervical spine injury but 60 to 80% of vertebral pediatric injuries involve cervical spine (29).
In literature, conservative treatment with orthosis for 6 to 8 weeks is suggested for stable vertebral fractures without neurologic impairment (21)(23). Nonsurgical treatment is also indicated in case of burst fractures without neurologic impairment (30)(31) as it seems not to be significant differences in functional outcomes compared to operative treatment.
Otherwise, in this study surgery was performed not only to decompress or to restore a better sagittal balance but also to achieve a faster recovery. Conservative spine treatment with rigid orthosis or casts for a long period following a suicide attempt could be an additional burden for these patients. Surgical percutaneous treatment for thoracolumbar fractures allows early mobilization, and this can ensure to the patient a quick resumption of daily activities. Suicidal jumper patients are usually adolescents, with multiple injuries and severe mental health diseases, who face long periods of psychiatric and multidisciplinary treatments. Surgery can be considered a temporary internal fixation as an alternative to conservative treatment with a rigid orthosis that could be a hitch to patient therapeutic path.
However cervical spine surgery is much more invasive and the only case with multiple cervical fractures was conservatively treated with a halo-vest with good results. In this case there wasn’t any neurological impairment, and a surgical treatment has no real advantage over conservative treatment to obtain better fractures reduction and stabilization. In this case, surgery would have a potential higher risk of complications (i.e., surgical site infection, vascular and nervous iatrogenic damage, blood loss) and an instrumentation spread on more levels. Patients and relatives have sometimes difficulty in comply with Halo vest treatment, even if Halo is somehow preferable to collar bracing or casting: in long treatment patient discomfort is lesser in Halo vest, particularly regarding alimentation and hygiene. In our case patient and parents showed good compliance with halo vest and the orthopedic treatment did not impair her psychiatric therapy.
In this study four patients had neurologic lesions and two with severe outcome albeit improving.
Treatment of these patients was challenging, especially during covid19 period when patient where isolated and they cannot have all their relatives and friend on their side. Moreover, spinal treatments had to be coordinated with the need for treatment of other associated injuries.
A multidisciplinary team is essential to optimize the management of these patients and avoid major complications.
Conclusions
This study shows an exponential increase in pediatric vertebral fractures due to suicide jumping attempt after COVID 19 pandemic. These are high energy fractures that are rather unusual in adolescent, and in some case rare (such as spinopelvic dissociation). The unusual high frequency of suicidal attempts with a not common modality in adolescent is a new epidemiological phenomenon after COVID-19 pandemic. The high number of complex vertebral fractures, in polytrauma pediatric patients who committed a self-harm act, could be a big issue for a spine surgeon. The choice of treatment must be guided by biological and biomechanical knowledge, but also by mental health condition of young patient and by other treatments needed. In our experience, percutaneous surgery was the most used treatment strategy and allowed a fast recovery. Suicidal jumper patients must be handled by a multidisciplinary team to optimize the management.
In future, we could expand this preliminary study, to see if this dramatic phenomenon and related injuries will remain as a grim result of post pandemic changes in social behavior or if suicidal jumper attempts in adolescents will return to pre pandemic incidence.
A multicenter study at European level, where there were similar pandemic conditions and restrictions, is desirable to better analyze these new data and to define the best treatment guidelines.
References
- Theodorou CM, Yamashiro KJ, Stokes SC, Salcedo ES, Hirose S, Beres AL. Pediatric suicide by violent means: a cry for help and a call for action. Inj Epidemiol (2022) 9:13. [CrossRef]
- (WHO) WHO. Preventing suicide: A global imperative. Prev suicide A Glob Imp (2014)92. https://www.who.int/publications/i/item/9789241564779.
- UNICEF UNICEF. The state of the world’s children 2021, On my mind: Promoting, protecting and caring for children’s mental health. (2021). https://www.unicef.org/reports/state-worlds-children-2021.
- CDC C for DC and PNC for HS. National Vital Statistics System, Mortality 2018-2021 on CDC WONDER Online Database, released in 2023. (2023). http://wonder.cdc.gov/mcd-icd10-expanded.html.
- Kõlves K, de Leo D. Suicide methods in children and adolescents. Eur Child Adolesc Psychiatry (2017) 26:155–164. [CrossRef]
- Värnik A, Kõlves K, Allik J, Arensman E, Aromaa E, van Audenhove C, Bouleau J-H, van der Feltz-Cornelis CM, Giupponi G, Gusmão R, et al. Gender issues in suicide rates, trends and methods among youths aged 15-24 in 15 European countries. J Affect Disord (2009) 113:216–226. [CrossRef]
- Bera L, Souchon M, Ladsous A, Colin V, Lopez-Castroman J. Emotional and Behavioral Impact of the COVID-19 Epidemic in Adolescents. Curr Psychiatry Rep (2022) 24:37–46. [CrossRef]
- Gracia R, Pamias M, Mortier P, Alonso J, Pérez V, Palao D. Is the COVID-19 pandemic a risk factor for suicide attempts in adolescent girls? J Affect Disord (2021) 292:139–141. [CrossRef]
- Yard E, Radhakrishnan L, Ballesteros MF, Sheppard M, Gates A, Stein Z, Hartnett K, Kite-Powell A, Rodgers L, Adjemian J, et al. Emergency Department Visits for Suspected Suicide Attempts Among Persons Aged 12-25 Years Before and During the COVID-19 Pandemic - United States, January 2019-May 2021. MMWR Morb Mortal Wkly Rep (2021) 70:888–894. [CrossRef]
- Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet (London, England) (2021) 398:1700–1712. [CrossRef]
- Sivertsen B, Knapstad M, Petrie K, O’Connor R, Lønning KJ, Hysing M. Changes in mental health problems and suicidal behaviour in students and their associations with COVID-19-related restrictions in Norway: a national repeated cross-sectional analysis. BMJ Open (2022) 12:e057492. [CrossRef]
- Gilsbach S, Herpertz-Dahlmann B, Konrad K. Psychological Impact of the COVID-19 Pandemic on Children and Adolescents With and Without Mental Disorders. Front public Heal (2021) 9:679041. [CrossRef]
- Carison A, Babl FE, O’Donnell SM. Increased paediatric emergency mental health and suicidality presentations during COVID-19 stay at home restrictions. Emerg Med Australas (2022) 34:85–91. [CrossRef]
- Mayne SL, Hannan C, Davis M, Young JF, Kelly MK, Powell M, Dalembert G, McPeak KE, Jenssen BP, Fiks AG. COVID-19 and Adolescent Depression and Suicide Risk Screening Outcomes. Pediatrics (2021) 148:. [CrossRef]
- Hill RM, Rufino K, Kurian S, Saxena J, Saxena K, Williams L. Suicide Ideation and Attempts in a Pediatric Emergency Department Before and During COVID-19. Pediatrics (2021) 147:. [CrossRef]
- Vicari S, Pontillo M. Developmental Psychopathology in the COVID-19 period. COVID-19 Pandemic Impact on Children and Adolescents’ Mental Health. Psychiatr Danub (2021) 33:33–35.
- Maina C, Cioffi SPB, Altomare M, Spota A, Virdis F, Bini R, Ragozzino R, Renzi F, Reitano E, Corasaniti L, et al. Increasing Trend in Violence-Related Trauma and Suicide Attempts among Pediatric Trauma Patients: A 6-Year Analysis of Trauma Mechanisms and the Effects of the COVID-19 Pandemic. J Pers Med (2023) 13:. [CrossRef]
- Cirak B, Ziegfeld S, Knight VM, Chang D, Avellino AM, Paidas CN. Spinal injuries in children. J Pediatr Surg (2004) 39:607–612. [CrossRef]
- Marco Crostelli, Osvaldo Mazza, Massimo Mariani, Pietro Persiani, Filippo Maria Ranaldi DM and CI. T7 vertebral burst fracture with left pedicle separated from vertebral body and displaced in vertebral canal without neurologic deficits in a 12 years old motorbike competition rider. Glob Surg (2018) 5(1): 1-5:. [CrossRef]
- Knox JB, Schneider JE, Cage JM, Wimberly RL, Riccio AI. Spine trauma in very young children: a retrospective study of 206 patients presenting to a level 1 pediatric trauma center. J Pediatr Orthop (2014) 34:698–702. [CrossRef]
- Payr S, Schuller A, Dangl T, Chocholka B, Binder H, Tiefenboeck TM. Spine Fractures in Children and Adolescents-Frequency, Causes, Diagnostics, Therapy and Outcome-A STROBE-Compliant Retrospective Study at a Level 1 Trauma Centre in Central Europe. Child (Basel, Switzerland) (2021) 8:. [CrossRef]
- Reddy SP, Junewick JJ, Backstrom JW. Distribution of spinal fractures in children: does age, mechanism of injury, or gender play a significant role? Pediatr Radiol (2003) 33:776–781. [CrossRef]
- Parisini P, Di Silvestre M, Greggi T. Treatment of spinal fractures in children and adolescents: long-term results in 44 patients. Spine (Phila Pa 1976) (2002) 27:1989–1994. [CrossRef]
- Vu C, Gendelberg D. Classifications in Brief: AO Thoracolumbar Classification System. Clin Orthop Relat Res (2020) 478:434–440. [CrossRef]
- Canseco JA, Schroeder GD, Paziuk TM, Karamian BA, Kandziora F, Vialle EN, Oner FC, Schnake KJ, Dvorak MF, Chapman JR, et al. The Subaxial Cervical AO Spine Injury Score. Glob spine J (2022) 12:1066–1073. [CrossRef]
- Kweh BTS, Tee JW, Oner FC, Schnake KJ, Vialle EN, Kanziora F, Rajasekaran S, Dvorak M, Chapman JR, Benneker LM, et al. Evolution of the AO Spine Sacral and Pelvic Classification System: a systematic review. J Neurosurg Spine (2022) 37:914–926. [CrossRef]
- Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am (1974) 56:1663–1674.
- Hart DJ, Wang MY, Griffith P, Gordon McComb J. Pediatric sacral fractures. Spine (Phila Pa 1976) (2004) 29:667–670. [CrossRef]
- Montalbano M, Fisahn C, Loukas M, Oskouian RJ, Chapman JR, Tubbs RS. Pediatric Hangman’s Fracture: A Comprehensive Review. Pediatr Neurosurg (2017) 52:145–150. [CrossRef]
- Vander Have KL, Caird MS, Gross S, Farley FA, Graziano GA, Stauff M, Segal LS. Burst fractures of the thoracic and lumbar spine in children and adolescents. J Pediatr Orthop (2009) 29:713–719. [CrossRef]
- Siebenga J, Leferink VJM, Segers MJM, Elzinga MJ, Bakker FC, Haarman HJTM, Rommens PM, ten Duis H-J, Patka P. Treatment of traumatic thoracolumbar spine fractures: a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976) (2006) 31:2881–2890. [CrossRef]
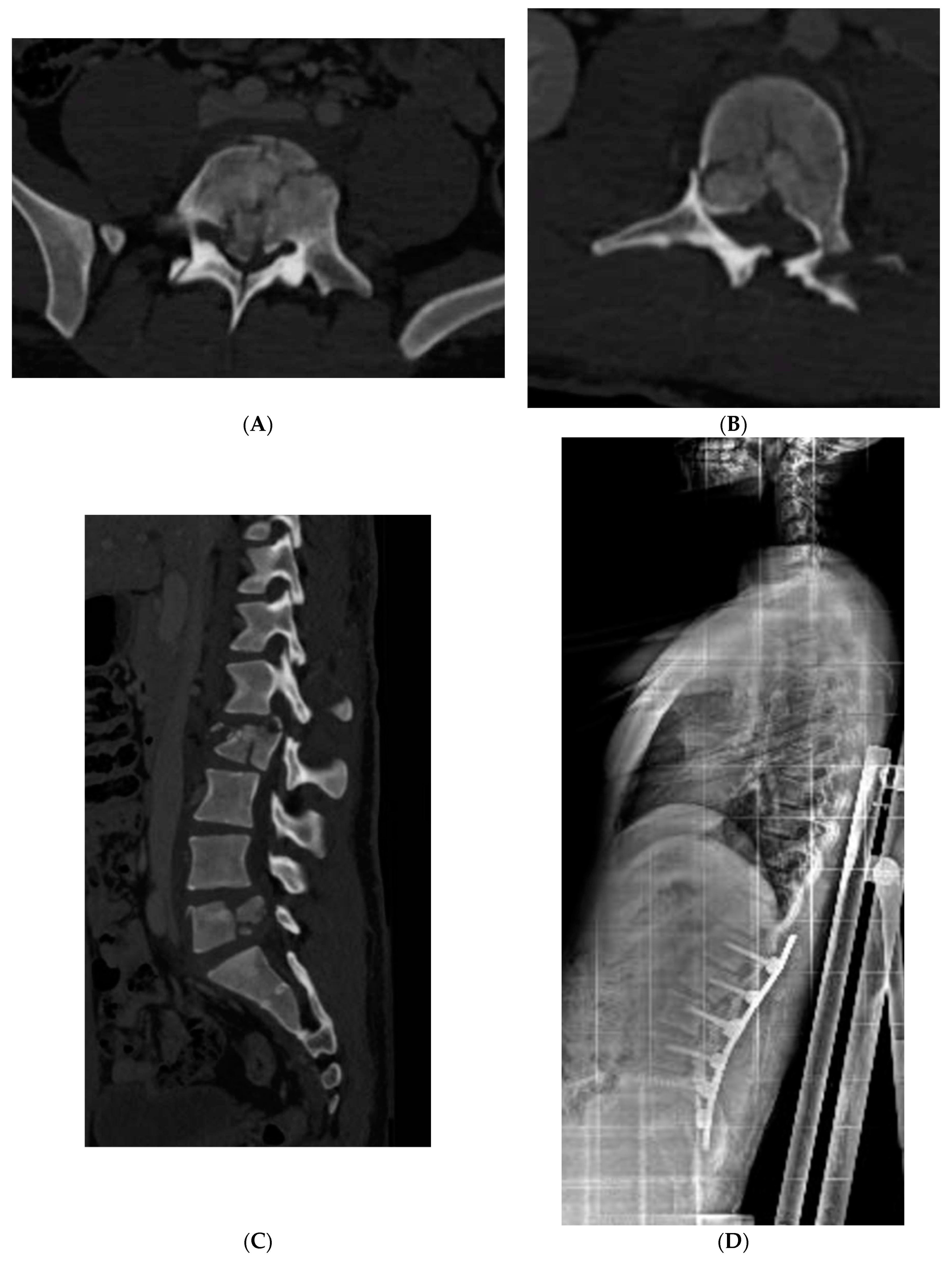
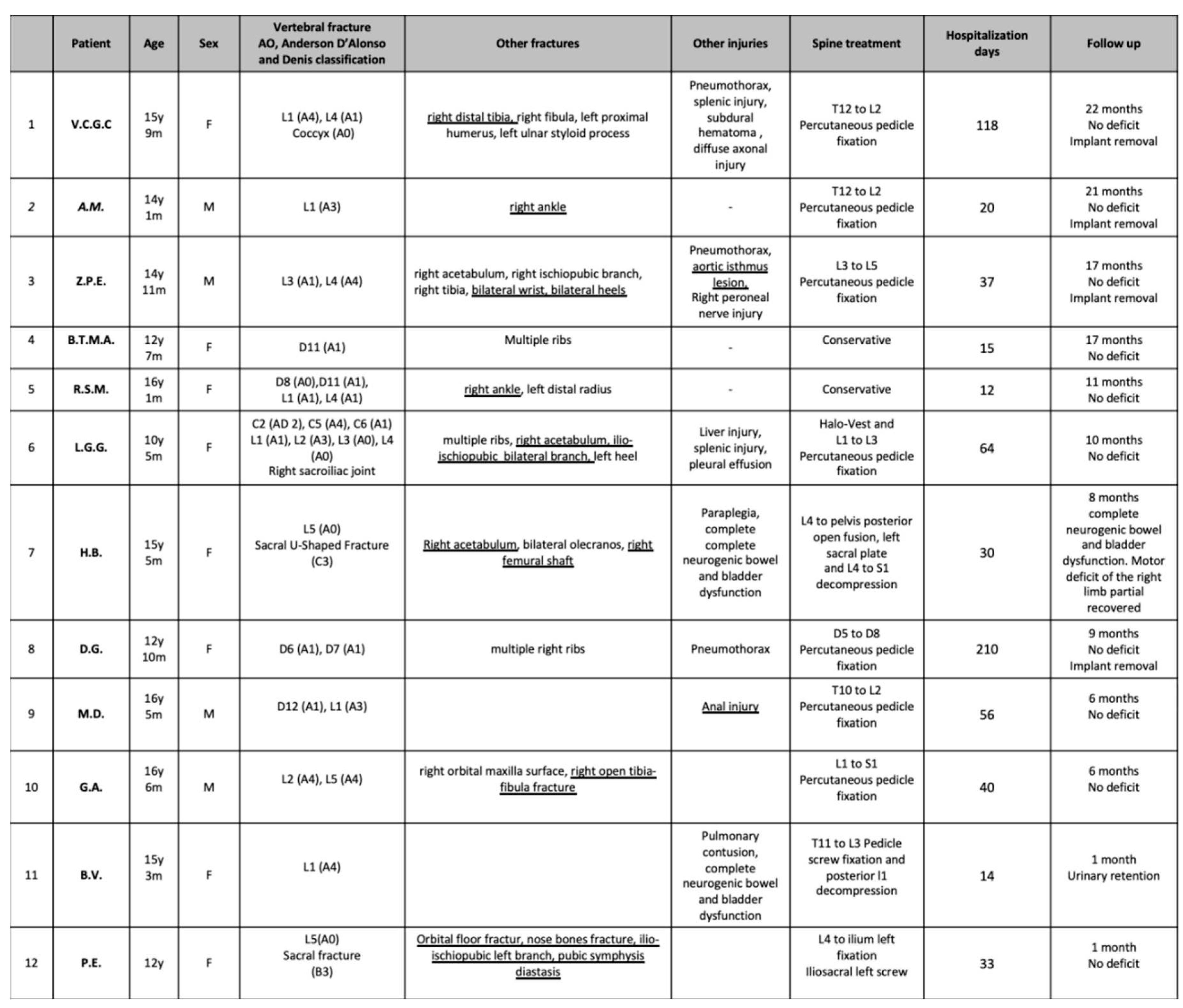
Table 1.
Patients involved in the study.
Table 1.
Patients involved in the study.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).