Introduction
The introduction and refinement of primary percutaneous coronary intervention (pPCI) in the treatment of patients with acute myocardial infarction with ST segment elevation (STEMI) has significantly improved survival and reduced the occurrence of complications [
1]. Due to improved survival, patients with stable chronic coronary disease post STEMI represent an increasingly important and prevalent population [
2,
3,
4]. Non-cardiac comorbidities are frequent in patients with acute myocardial infarction (AMI) [
4,
5]. The presence of non-cardiac comorbidities in patients with AMI can be explained by the presence of the same risk factors for both AMI and non-cardiac comorbidity (e.g., smoking is also a risk factor for chronic obstructive pulmonary disease, peripheral artery disease, stroke, etc.), while some non-cardiac comorbidities are risk factors for coronary disease (e.g., diabetes mellitus, hypertension, chronic kidney disease, etc.) [
4]. The results of studies analyzing the prognostic significance of non-cardiac or non-cardiovascular comorbidities in patients with STEMI and/or non-STEMI have shown that the presence of at least one non-cardiac comorbidity has a negative impact on short-term and long-term prognosis [
2,
3,
4,
5,
6,
7,
8,
9,
10,
11].
Left ventricular ejection fraction (EF) is considered one of the most important predictors of prognosis after STEMI. The percentage of patients with reduced left ventricular systolic function (i.e., reduced EF) is smaller in the pPCI era than in the thrombolytic era, because the establishing of a normal blood flow through the infarcted artery leads to a reduction in the myocardial necrotic zone [
12]. It can be said that in the era of primary PCI, there is a higher percentage of patients with preserved systolic function than patients with reduced systolic function of the left ventricle. Patients with preserved EF generally have an excellent short- and long-term prognosis [
1]. Predictors of long-term prognosis, as well as the influence of non-cardiac comorbidities, may be different in patients with reduced and preserved left ventricular systolic function. To the best of our knowledge, the influence of non-cardiac comorbidities on the long-term prognosis of the patient in relation to the EF value after STEMI has not been analyzed as yet.
The aim of this study was to analyze the prevalence and long-term prognostic impact of non-cardiac co-morbidities in patients with reduced and preserved EF following ST-elevation myocardial infarction.
Method
Study Population, Data Collection and Definitions
The present study enrolled 3,115 consecutive patients hospitalized between December 2005 and January 2012, who were included in the prospective University Clinical Center of Serbia STEMI Register. The purpose of the prospective University Clinical Center of Serbia STEMI Register has been published elsewhere [
13].
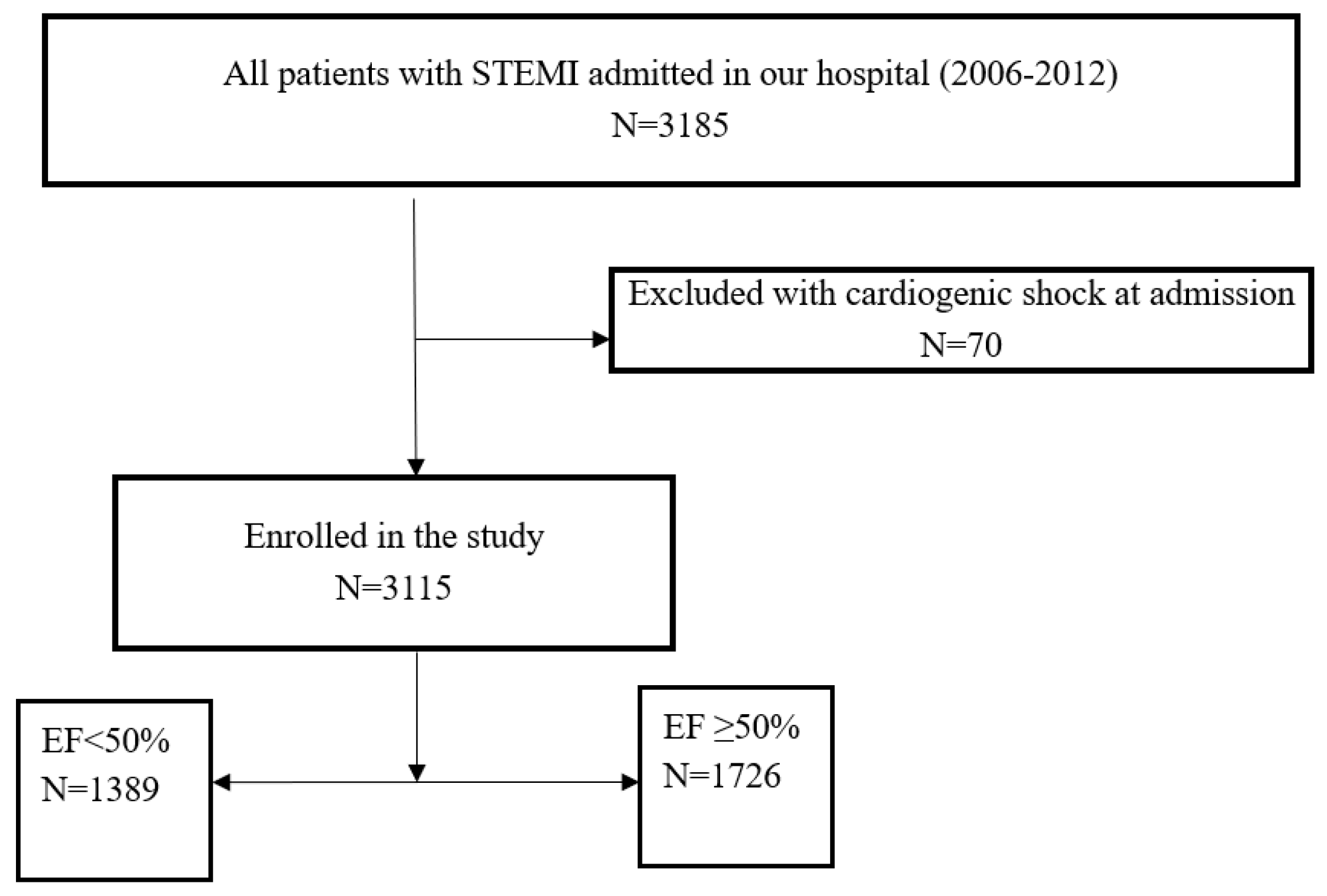
In brief, the objective of the Register is to gather complete and representative data on the management and short- and long-term outcomes of patients with STEMI, undergoing primary PCI in the Center. All consecutive patients with STEMI, aged 18 or older, who were admitted to the Coronary Care Unit after undergoing pPCI in the Center, were included in the Register. All patients for whom data were entered into the Register received written information of their participation in the Register and the long-term follow up, and their verbal consent for enrollment was obtained. Patients with cardiogenic shock at admission were excluded. The flowchart of patient selection is shown in
Figure 1.
Coronary angiography was performed via the femoral approach. Primary PCI and stenting of the infarct-related artery (IRA) was performed according to the standard technique. Aspirin, 300 mg, and clopidogrel, 600 mg, were administered to all eligible patients before pPCI. Selected patients, with visible intracoronary thrombi, were also given the GP IIb/IIIa receptor inhibitor during pPCI. Flow grades were assessed according to the Thrombolysis in Myocardial Infarction (TIMI) criteria. After pPCI, patients were treated according to current guidelines.
Demographic, baseline clinical, angiographic, and procedural data were collected and analyzed. Echocardiographic examination was performed within the first three days after pPCI. The left ventricular ejection fraction (EF) was assessed according to the biplane method, in classical two- and four-chamber apical projections. Patients were divided in two groups: patients with preserved EF (EF ≥ 50%) and patients with reduced EF (EF < 50%).
Non-cardiac comorbidities were defined by means of hospital diagnoses or with the help of retrieved prescriptions that were issued before hospital admission (i.e., before the index event – STEMI). We considered the non-cardiac comorbidities included in the Charlson Comorbidity Index – CCI [
14]. On the basis of the CCI, we analyzed the following non-cardiac comorbidities: previous stroke, peripheral artery disease (PAD), chronic obstructive pulmonary disease (COPD), diabetes mellitus (DM), chronic kidney disease (CKD), (the value of the estimated glomerular filtration rate at admission < 60ml/min/m
2, using the Modification of Diet in Renal Disease equation), carcinoma, peptic ulcer disease, psychiatric disorders, and liver disease. We also analyzed anemia (according to the World Health Organization criteria baseline, defined as a hemoglobin level < 130g/L, in men, and a hemoglobin level < 120g/L, in women) and obesity (defined as body mass index ≥ 30kg/m
2). Anemia was included in the analysis due to its relatively frequent presence in our patients, its importance in the application and duration of application of dual antiplatelet therapy, and the known negative impact on the prognosis of patients with acute coronary syndrome [
15]. Obesity was analyzed because it represents a global health problem.
Patients were followed-up at eight years after enrolment. Follow-up data were obtained by scheduled telephone interviews and outpatient visits. We analyzed all-cause mortality.
Ethics
The study protocol was approved by the ethics committee of the University of Belgrade, Faculty of Medicine (approval number 470/II-4, February 21, 2008). The study was conducted in accordance with the principles set forth in the Helsinki Declaration. Written informed consent was obtained from all patients for their participation in the Register.
Statistical Analysis
Categorical variables were expressed as frequency and percentage, while the continuous variables were expressed as the median (med), with 25th and 75th quartiles (IQR). Analysis for normality of data was performed using the Kolmogorov-Smirnov test. Baseline differences between groups were analyzed using the Man-Whitney test for continuous variables, and the Pearson X2 test for categorical variables. The Kaplan-Meier method was used for constructing the probability curves for eight-year survival, while the difference between patients with and without non-cardiac comorbidities was tested with the Log-Rank test. Multiple cox analysis (backward method, with p < 0.10 for entrance into the model) was used for identifying independent risk factors for the occurrence of eight-year all-cause mortality. Two-tailed p values of < 0.05 were considered to indicate a statistically significant difference. The SPSS statistical software, version 19, was applied (SPSS Inc, Chicago, IL).
Results
Out of the 3,115 patients analyzed, 1,389 (44.5%) patients had reduced EF, and 1,726 (55.4%) patients had preserved EF. Non-cardiac comorbidities at admission were present in a total of 1,014 (32.5%) patients. Amongst the patients with non-cardiac comorbidities 565 (18.1%) patients had one non-cardiac comorbidity, while 449 (14.4%) patients had two or more non-cardiac comorbidities. The most prevalent non-cardiac comorbidity was DM, followed by CKD, obesity, anemia, COPD, previous stroke and PAD. The prevalence of other comorbidities was less than 0.1%. As compared to patients with preserved EF, patients with reduced EF were older, they had heart failure at admission more frequently, as well as previous hypertension, multivessel coronary artery disease at initial angiogram, and post-procedural flow TIMI<3. Non-cardiac comorbidities at hospital admission were more frequently present in patients with reduced EF, as compared to patients with preserved EF. Baseline characteristics, laboratory, angiographic and procedural characteristics, therapy at discharge, as well as comorbidities in the whole cohort and in patients with reduced and preserved EF, are shown in
Table 1.
During 8-year follow-up, the lethal outcome (all-cause mortality) was registered in a total of 244 (7.8%) patients; in the group with preserved EF, the lethal outcome was registered in 40 (2.3%) patients and in the group with reduced EF, lethal outcome was registered in 240 (17.2%) patients, p<0.001. Causes of mortality in all of the analyzed patients were predominantly cardiovascular (N = 228, 93.3% of all deaths). Cardiovascular causes included fatal re-infarction, progression of heart failure, sudden death, and stroke. Noncardiovascular causes of death (such as cancer, ileus, pneumonia) were registered in 16 patients (6.5% of all deaths).
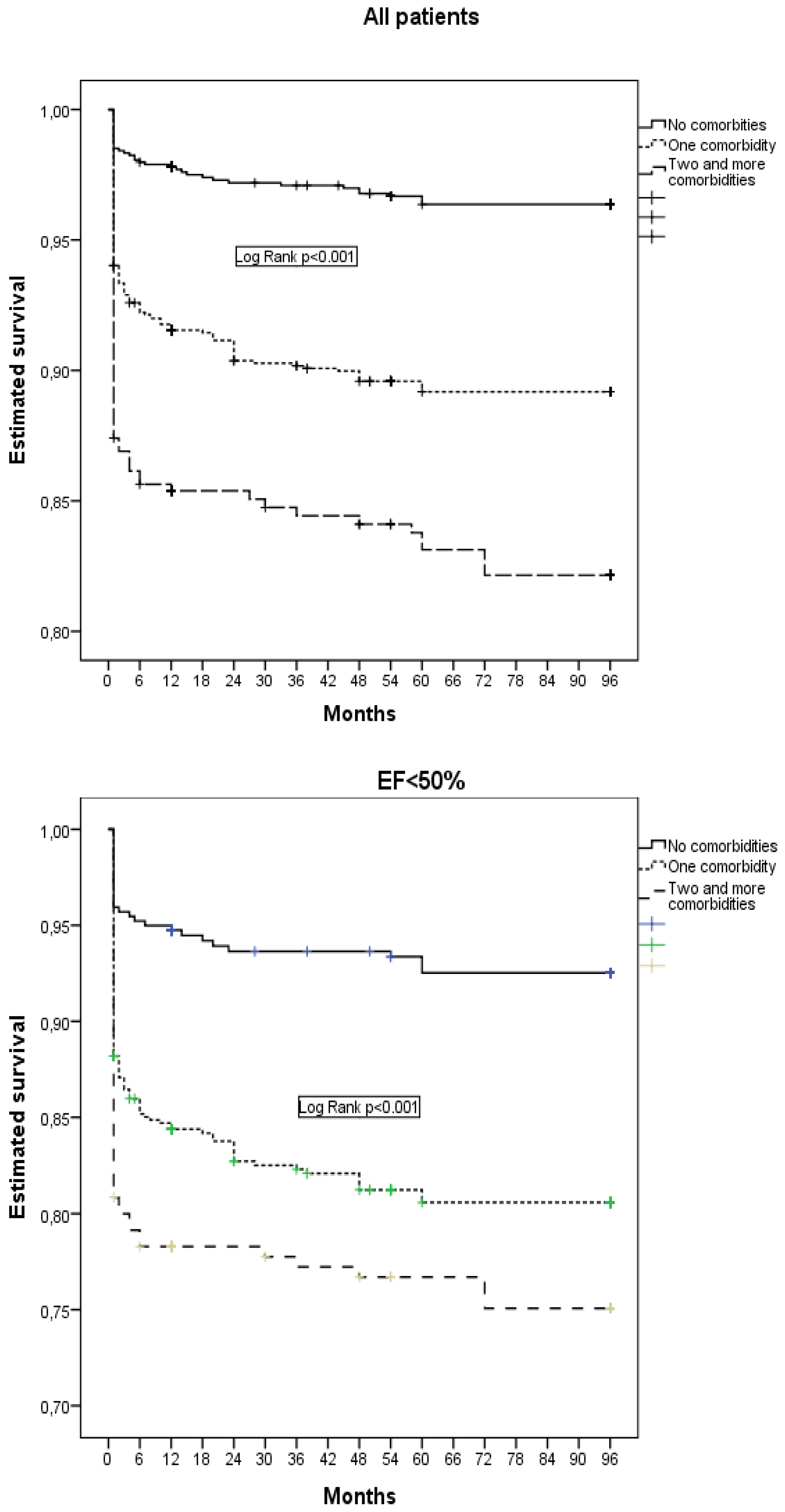
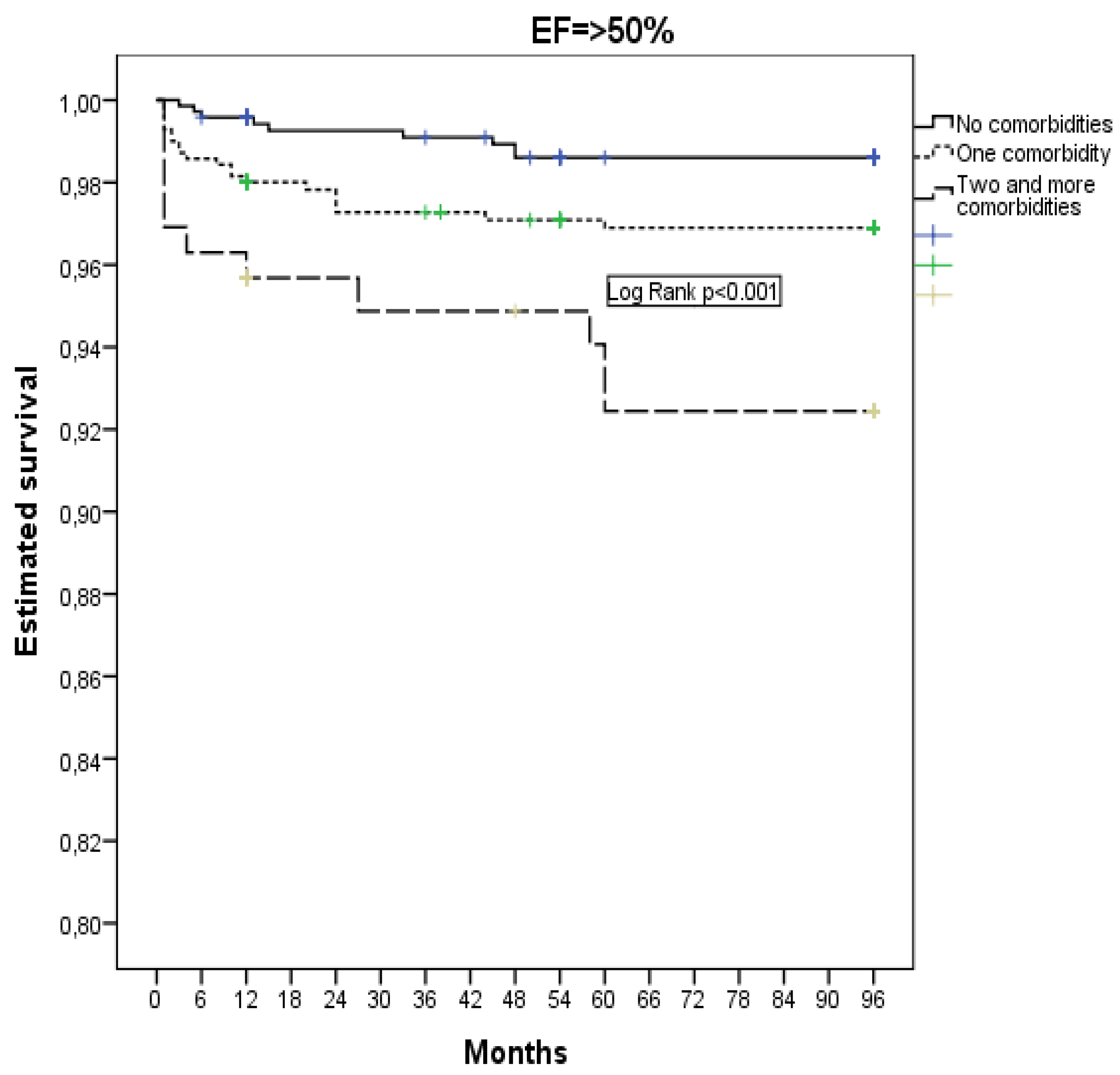
Patients with non-cardiac comorbidities had a higher 8-year all-cause mortality, as compared to patients without non-cardiac comorbidities, and mortality increased if two or more comorbidities were present at the same time.
Estimated survival during 8-year follow-up, according to the presence of comorbidities, is shown in
Figure 2.
Predictors for the occurrence of all-cause mortality during 8-year patient follow-up are presented in
Table 2.
Discussion
The results of our study showed that non-cardiac comorbidities were present in about a third of the analyzed patients. In patients who had reduced EF after STEMI, the prevalence of non-cardiac comorbidities was higher, as compared to patients who had preserved EF after STEMI. Regardless of the EF value, 8-year mortality was higher in patients with the presence of at least one non-cardiac comorbidity, as compared to patients without any non-cardiac comorbidities. In a multivariate analysis we found that diabetes mellitus and chronic kidney disease were independent predictors of 8-year all-cause mortality in patients with preserved EF, with the effect of DM being significantly greater than the prognostic impact of CKD. In patients with reduced EF, CKD was a strong independent predictor and the only comorbidity that had an independent prognostic impact on 8-year all-cause mortality.
Non-Cardiac Comorbidities in Patients with Myocardial Infarction
The prevalence of non-cardiac comorbidities in our patients is mostly in accordance with the data from literature, bearing in mind, however, the data found in literature depend on the design of the study, the population of analyzed patients, and the selected comorbidities for analysis [
2,
7,
10,
16]. In a systematic review by Breen et al., it was found that the prevalence of non-cardiac comorbidity in different studies ranged from 33% to 69%, with a mean of 56% [
16]. Despite the high prevalence of multimorbidity in the ACS population, there was a lack of consistency in the way multimorbidity was measured and characterized. Currently there is no gold standard for comorbidity measuring [
16].
The lack of studies analyzing the prognostic impact of non-cardiac comorbidities in patients with STEMI treated with pPCI (as well as in relation to left ventricular systolic function) limits direct comparison of our results with data from literature. On the other hand, the unfavorable impact of non-cardiac comorbidities on the prognosis of patients with AMI (STEMI and non-STEMI) has been analyzed in numerous studies, bearing in mind, however, that the prognostic impact was analyzed in a shorter follow-up, as compared to our study [
2,
4,
8,
9,
16,
17,
18,
19]. All studies show that the presence of a greater number of comorbidities is associated with higher mortality or more frequent occurrence of other complications, and also, in almost all studies, there is a significant prognostic impact of DM and/or CKD on the patient's prognosis.
A review by Rashid et al, showed that an increase in the value of the Charlson comorbidity index (CCI) increases the mortality of patients with acute coronary syndrome by 30%, and the mortality of patients treated with primary PCI by 20%. This review also showed that a CCI score value of above two increases the risk of mortality by 2.5 times in patients with acute coronary syndrome, and by about three times in patients undergoing PCI [
17]. In two Swiss cohort studies of patients with acute coronary syndrome, 8,330 patients with ST-segment elevation myocardial infarction (STEMI) undergoing percutaneous coronary intervention were analyzed, during the period 2005 – 2012 [
18]. It was shown that CCI scores ≥ 2 increased the one-year risk of major adverse cardiovascular and cerebrovascular events by 40% [
18]. In a nationwide cohort study by Schmidt et al., the impact of comorbidities on the prognosis of patients with AMI was analyzed, as well as the interaction between comorbidities and AMI. It was shown that the interaction effect was the greatest within the first 30 days of follow-up, but similar dose-response patterns were also observed between 31 and 365 days of follow-up, as well as during 1 to 5 years of follow-up [
9]. The results were independent by sex, but influenced by age; the percentage of the rate explained by interaction was highest in younger patients. The interaction effect for non-cardiac comorbidity was most pronounced for dementia, liver disease and DM [
9]. In the study by Rapsomaniki et al., mortality and the occurrence of bleeding in patients with AMI after one year were analyzed. In this study, a strong predictor of three-year all-cause death was CKD, along with heart failure, COPD and a history of cancer. Unlike our study, the aforementioned studies analyzed patients with STEMI and NSTEMI, and revascularization was not performed in all STEMI patients [
8]. A systematic review by Johanson et al. included studies analyzing all-cause death up to 5 years after AMI. Compared with the general population, MI survivors remain at high risk, particularly older patients and those with comorbidities such as hypertension, DM, CKD, PAD, or history of stroke [
11].
Non-Cardiac Comorbidities in Relation to EF
The prognostic impact of comorbidities in relation to the EF value in patients with heart failure has been analyzed in literature. In a study by Iorio et al., a similar prevalence and similar negative prognostic impact of non-cardiac comorbidities was found in patients with heart failure and reduced EF (HFrEF) as well as in patients with heart failure and preserved EF (HFpEF). In this study, CKD, anemia, COPD, and PAD had the strongest and most significant association with mortality [
20]. In a study by van Deursen et al., comorbidities in patients with chronic heart failure were analyzed and it was found that CKD, anemia, and diabetes mellitus were independent predictors of mortality and heart failure hospitalization [
21]. CKD showed the greatest prognostic significance, i.e., 41% of all-cause mortality in the analyzed population was attributable to CKD comorbidity [
21]. Also, in a study by Yang et al., it was found that the association between DM and 5-year all-cause mortality in patients with heart failure and reduced EF existed only if CKD was also present [
22].
Possible Mechanisms of the Negative Impact of Comorbidities on the Prognosis of Patients with AMI
Non-cardiac comorbidities may be risk factors for coronary disease, which is why secondary prevention is extremely important in these patients. This particularly applies to the coexistence of DM and CKD [
22]. Also, non-cardiac comorbidities reduce the possibility of taking the guideline-recommended treatment after AMI [
4,
9,
10]. There is also a known treatment-risk paradox with regard to the provision of invasive coronary procedures. It is known that, in patients with ACS and one or more comorbidities, revascularization procedures are generally performed less often [
10,
16]. In our study, this was not the case, because all our patients were treated with pPCI. In the study by Yadegarfar et al., it was found that the presence of each analyzed comorbidity, with the exception of hypertension, renal failure, and PAD, was associated with a reduced chance of receiving optimal care [
10]. On the other hand, the receipt of optimal AMI care was associated with reduced mortality, however, in patients with AMI and chronic heart failure, cerebrovascular disease, or with two or more comorbidities, there was no significant improvement in survival despite receiving optimal guideline-indicated AMI care [
10]. This finding may indicate that, in some situations, comorbidities may reduce the effectiveness of optimal or guideline-recommended treatment in patients with AMI [
10]. Also, rehabilitation after AMI is usually performed less often in patients with comorbidities [
16], which can affect the prognosis, but also the quality of life.
Clinical Significance of Our Study
We feel that our findings add to the existing knowledge on the prevalence of non-cardiac comorbidities among unselected STEMI patients and their influence of mortality in the primary PCI era. The frequent presence of non-cardiac comorbidities in patients with STEMI represents a significant challenge in the treatment of these patients, both during hospitalization and upon discharge from the hospital [
23,
24]. Multidisciplinary efforts to better manage cardiovascular risk factors may have an additional secondary preventive role, since the most common causes of death in our patients were cardiovascular [
5]. Even in patients who have preserved EF, who are without complications after STEMI, and have CKD and/or DM, prolonged dual antiplatelet therapy should be considered, taking into account the hemorrhagic risk. Attention should also be focused on therapy for non-cardiac comorbidities due to possible drug interactions, but also the possible effects on cardiac function and the occurrence of adverse events after AMI [
8,
10,
16].
Study Limitations
A number of limitations to our study warrant being mentioned. The study is unicentric, observational, but it is controlled, prospective and has included consecutive patients, thus limiting possible selection bias. Patients enrolled in the study were hospitalized between 2006 and 2012. We did not use other measures for determining systolic function, such as myocardial deformation imaging. However, many cornerstone clinical trials conducted so far have used EF to stratify patients [
25,
26]. The longitudinal measurement of EF was not performed for the purpose of evaluating the improvement in left ventricular function after STEMI [
27]. Some comorbidities were present in less than 0.1% of our patients, so their prognostic impact cannot be ruled out with certainty. Patients were treated with clopidogrel as there were no patients treated with more recently developed antithrombotic drugs (ticagrelor was not available for routine administration to patients at the time of their entry into the Register), which could have influenced the prognosis of the patients. The study was not designed to evaluate whether changing pharmacological treatment would have an impact on the long-term outcome in the analyzed patients.
Conclusions
About a third of the analyzed patients with STEMI had at least one non-cardiac comorbidity. Patients with reduced, as well as those with preserved EF after STEMI and the presence of at least one non-cardiac comorbidity had a higher 8-year all-cause mortality, as compared to patients without non-cardiac comorbidities. However, only diabetes mellitus and chronic kidney disease had an independent prognostic impact on 8-year all-cause mortality in patients with preserved EF, while in patients with reduced EF, CKD was the only non-cardiac comorbidity that was an independent predictor of 8-year all-cause mortality.
Author Contributions
LS and IM devised the study and participated in its design, acquisition of data and coordination. LS performed statistical analysis. MA, SS, GK, RL, DM, and DS participated in the design of the study and helped draft the manuscript. All of the authors have read and approved the final manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the ethics committee of the University of Belgrade, Faculty of Medicine (approval number 470/II-4, February 21, 2008).
Informed consent statement
All patients for whom data were entered into the Register received written information of their participation in the Register and the long-term follow up, and their verbal consent for enrollment was obtained.
Acknowledgments
The authors would like to express their gratitude to the physicians and nurses of the Coronary Unit and the Catheterization Laboratory who participated in the primary PCI program.
Conflicts of Interest
The authors report there are no competing interests to declare.
References
- Savic, L.; Mrdovic, I.; Asanin, M.; Stankovic, S.; Krljanac, G.; Lasica, R. Prognostic impact of renal dysfunction on long-term mortality in patients with preserved, moderately impaired, and severely impaired left ventricular systolic function following myocardial infarction. Anatol J Cardiol 2018, 20, 21–8. [Google Scholar] [CrossRef]
- Christensen, D.M.; Schjerning, A.M.; Smedegaard, L.; Charlot, M.G.; Ravn, P.B.; Ruwald, A.C.; et al. Long-term mortality, cardiovascular events, and bleeding in stable patients 1 year after myocardial infarction: a Danish nationwide study. Eur Heart J 2023, 44, 488–98. [Google Scholar] [CrossRef]
- Gili, M.; Sala, J.; López, J.; Carrión, A.; Béjar, L.; Moreno, J.; et al. Impact of comorbidities on in-hospital mortality from acute myocardial infarction, 2003-2009. Rev Esp Cardiol 2011, 64, 1130–7. [Google Scholar] [CrossRef]
- Schmidt, M.; Horváth-Puhó, E.; Ording, A.G.; Bøtker, H.E.; Lash, T.L.; Sørensen, H.T. The interaction effect of cardiac and non-cardiac comorbidity on myocardial infarction mortality: A nationwide cohort study. Int J Cardiol 2020, 308, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Munyombwe, T.; Dondo, T.B.; Aktaa, S.; Wilkinson, C.; Hall, M.; Hurdus, B.; et al. Association of multimorbidity and changes in health-related quality of life following myocardial infarction: a UK multicentre longitudinal patient-reported outcomes study. BMC Med 2021, 19, 227. [Google Scholar] [CrossRef] [PubMed]
- Ofori-Asenso, R.; Zomer, E.; Chin, K.L.; Markey, P.; Si, S.; Ademi, Z.; et al. Prevalence and impact of non-cardiovascular comorbidities among older adults hospitalized for non-ST segment elevation acute coronary syndrome. Cardiovasc Diagn Ther 2019, 9, 250–61. [Google Scholar] [CrossRef] [PubMed]
- Sundaram, V.; Rothnie, K.; Bloom, C.; Zakeri, R.; Sahadevan, J.; Singh, A.; et al. Impact of comorbidities on peak troponin levels and mortality in acute myocardial infarction. Heart 2020, 106, 677–85. [Google Scholar] [CrossRef] [PubMed]
- Rapsomaniki, E.; Thuresson, M.; Yang, E.; Blin, P.; Hunt, P.; Chung, S.C.; et al. Using big data from health records from four countries to evaluate chronic disease outcomes: a study in 114 364 survivors of myocardial infarction. Eur Heart J Qual Care Clin Outcomes 2016, 2, 172–83. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Jacobsen, J.B.; Lash, T.L.; Bøtker, H.E.; Sørensen, H.T. 25 year trends in first time hospitalisation for acute myocardial infarction, subsequent short and long term mortality, and the prognostic impact of sex and comorbidity: a Danish nationwide cohort study. BMJ 2012, 344, e356. [Google Scholar] [CrossRef] [PubMed]
- Yadegarfar, M.E.; Gale, C.P.; Dondo, T.B.; Wilkinson, C.G.; Cowie, M.R.; Hall, M. Association of treatments for acute myocardial infarction and survival for seven common comorbidity states: a nationwide cohort study. BMC Med 2020, 18, 231. [Google Scholar] [CrossRef] [PubMed]
- Johansson, S.; Rosengren, A.; Young, K.; Jennings, E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord 2017, 17, 53. [Google Scholar] [CrossRef] [PubMed]
- Ng, V.G.; Lansky, A.J.; Meller, S.; Witzenbichler, B.; Guagliumi, G.; Peruga, J.Z.; et al. The prognostic importance of left ventricular function in patients with ST-segment elevation myocardial infarction:the HORIZONS-AMI trial. Eur Heart J Acute Cardiovasc Care. 2014, 3, 67–77. [Google Scholar] [CrossRef]
- Mrdovic, I.; Savic, L.; Lasica, R.; et al. Efficacy and safety of tirofiban-supported primary percutaneous coronary intervention in patients pretreated with 600 mg clopidogrel: results of propensity analysis using the clinical center of serbia STEMI register. Eur Heart J Acute Cardiovasc Care. 2014, 3, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987, 40, 373–83. [Google Scholar] [CrossRef]
- Lawler, P.R.; Filion, K.B.; Dourian, T.; et al. Anemia and mortality in acute coronary syndromes: a systematic review and meta-analysis. Am Heart J 2013, 165, 143–53.e5. [Google Scholar] [CrossRef]
- Breen, K.; Finnegan, L.; Vuckovic, K.; Fink, A.; Rosamond, W.; DeVon, H.A. Multimorbidity in Patients With Acute Coronary Syndrome Is Associated With Greater Mortality, Higher Readmission Rates, and Increased Length of Stay: A Systematic Review. J Cardiovasc Nurs 2020, 35, E99–E110. [Google Scholar] [CrossRef]
- Rashid, M.; Kwok, C.S.; Gale, C.P.; Doherty, P.; Olier, I.; Sperrin, M.; et al. Impact of co-morbid burden on mortality in patients with coronary heart disease, heart failure, and cerebrovascular accident: a systematic review and meta-analysis. Eur Heart J Qual Care Clin Outcomes 2017, 3, 20–36. [Google Scholar] [CrossRef]
- Jeger, R.; Jaguszewski, M.; Nallamothu, B.N.; Lüscher, T.F.; Urban, P.; Pedrazzini, G.B.; Erne, P.; Radovanovic, D.; AMIS Plus Investigators. Acute multivessel revascularization improves 1-year outcome in ST-elevation myocardial infarction: a nationwide study cohort from the AMIS Plus registry. Int J Cardiol 2014, 172, 76–81. [Google Scholar] [CrossRef]
- Sanchis, J.; Núñez, J.; Bodí, V.; Núñez, E.; García-Alvarez, A.; Bonanad, C.; Regueiro, A.; Bosch, X.; Heras, M.; Sala, J.; Bielsa, O.; Llácer, A. Influence of comorbid conditions on one-year outcomes in non-ST-segment elevation acute coronary syndrome. Mayo Clin Proc 2011, 86, 291–6. [Google Scholar] [CrossRef]
- Iorio, A.; Senni, M.; Barbati, G.; Greene, S.J.; Poli, S.; Zambon, E.; Di Nora, C.; Cioffi, G.; Tarantini, L.; Gavazzi, A.; Sinagra, G.; Di Lenarda, A. Prevalence and prognostic impact of non-cardiac co-morbidities in heart failure outpatients with preserved and reduced ejection fraction: a community-based study. Eur J Heart Fail 2018, 20, 1257–66. [Google Scholar] [CrossRef]
- van Deursen, V.M.; Urso, R.; Laroche, C.; Damman, K.; Dahlström, U.; Tavazzi, L.; et al. Co-morbidities in patients with heart failure: an analysis of the European Heart Failure Pilot Survey. Eur J Heart Fail 2014, 16, 103–11. [Google Scholar] [CrossRef]
- Yang, Y.; Huang, Z.; Wu, B.; Lu, J.; Xiu, J.; Tu, J.; Chen, S.; Pan, Y.; Bao, K.; Wang, J.; Chen, W.; Liu, J.; Liu, Y.; Chen, S.; Chen, K.; Chen, L. Predictors of mortality in heart failure with reduced ejection fraction: interaction between diabetes mellitus and impaired renal function. Int Urol Nephrol 2023. [CrossRef]
- Jernberg, T.; Hasvold, P.; Henriksson, M.; Hjelm, H.; Thuresson, M.; Janzon, M. Cardiovascular risk in post-myocardial infarction patients: nationwide real world data demonstrate the importance of a long-term perspective. Eur Heart J 2015, 36, 1163–70. [Google Scholar] [CrossRef] [PubMed]
- Bonaca, M.P.; Bhatt, D.L.; Cohen, M.; Steg, P.G.; Storey, R.F.; Jensen, E.C.; et al. Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med 2015, 372, 1791–1800. [Google Scholar] [CrossRef]
- Moukarbel, G.V.; Yu, Z.F.; Dickstein, K.; Hou, Y.R.; Wittes, J.T.; McMurray, J.J.; et al. The impact of kidney function on outcomes following high risk myocardial infarction:findings from 27 610 patients. Eur J Heart Fail 2014, 16, 289–99. [Google Scholar] [CrossRef]
- Meta-analysis Global Group in Chronic Heart Failure (MAGGIC) The survival of patients with heart failure with presserved or reduced left ventricular ejection fraction;an individual patient data meta-analysis. Eur Heart J. 2012, 33, 1750–7. [CrossRef]
- Søholm, H.; Lønborg, J.; Andersen, M.J.; et al. Repeated echocardiography after first ever ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention–is it necessary? Eur Heart J Acute Cardiovasc Care 2015, 4, 528–536. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).