Submitted:
22 April 2023
Posted:
23 April 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Resources, Data Collection, and Sample Size
2.3. The Proposed Conceptual Model
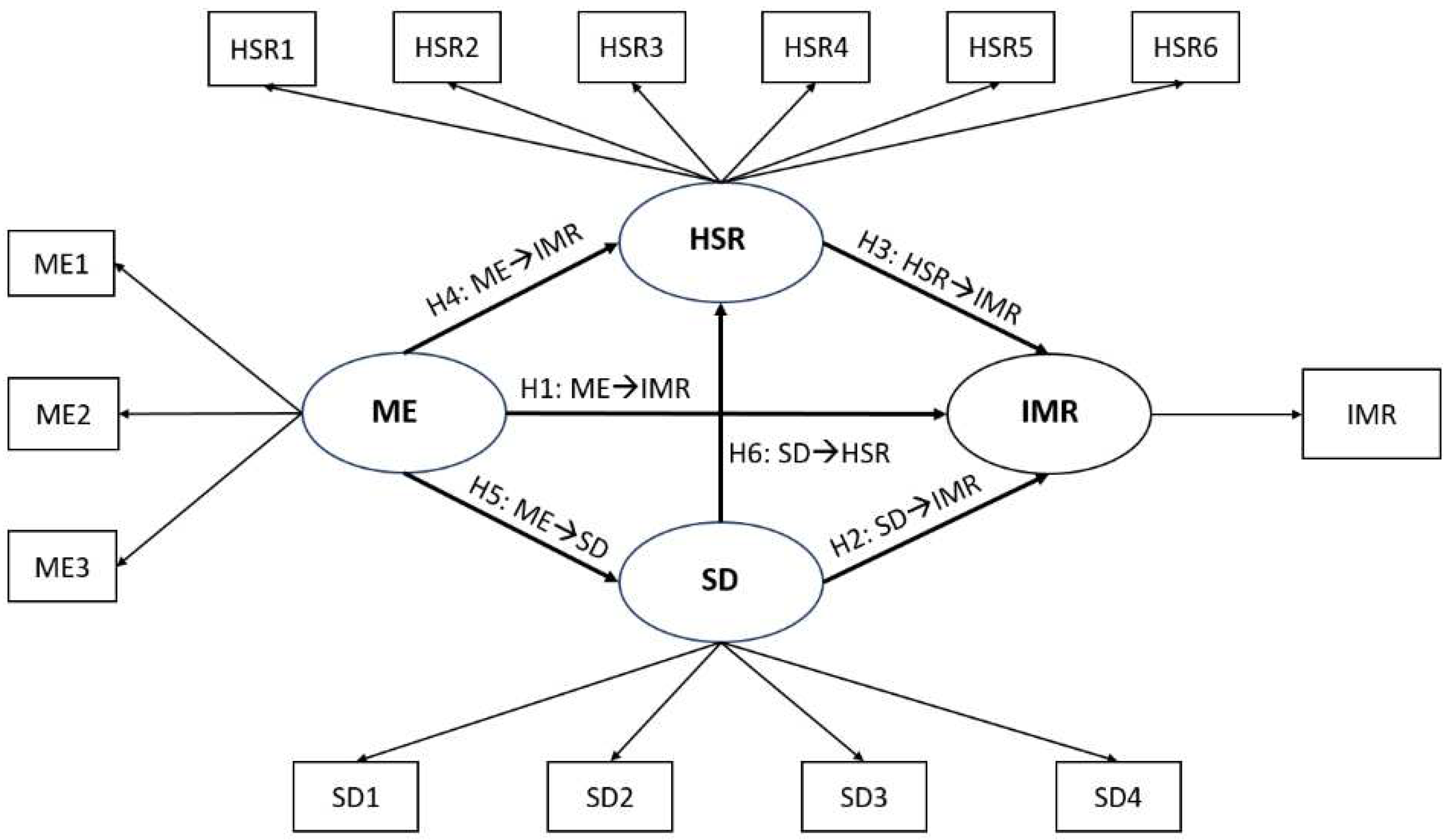
| Label | Variable | Definition | Source |
|---|---|---|---|
| IMR | Infant Mortality Rate | The infant mortality rate is the number of infants dying before one year per 1,000 live births yearly. | World Bank |
| SD variables | |||
| SD1 | Birth rate (crude) | Crude birth rate indicates the number of live births per 1,000 midyear population. | World Bank |
| SD2 | Adolescent fertility rate | Adolescent fertility rate is the number of births per 1,000 women aged 15-19. | World Bank |
| SD3 | Fertility rate (total, births per woman) | Total fertility rate represents the number of children that would be born to a woman if she were to live to the end of her childbearing years and bear children in accordance with age-specific fertility rates of the specified year | World Bank |
| SD4 | Percentages (%) of women married | Proportion of married or in-union women of reproductive-age (ages 15-49) in total population of women in the same age group, expressed in terms of percentage. | SESRIC |
| HSR variables | |||
| HSR1 | Newborns protected against tetanus (%) | Percentage of births by women of child-bearing age who are immunized against tetanus. I.e., newborns who achieved protection at birth from their mothers who received tetanus toxoid doses during the pregnancy. | World Bank |
| HSR2 | 1-Year-Olds Immunized with BCG (%) | One-year-olds who have received one dose of Bacille Calmette-Guérin (BCG) vaccine in a given year, expressed in terms of percentage. | SESRIC |
| HSR3 | 1-Year-Olds Immunized with MCV1 (%) | One-year-olds who have received at least one dose of measles-containing vaccine (MCV1) in a given year, expressed in terms of percentage. | SESRIC |
| HSR4 | 1-Year-Olds Immunized with Pol3 (%) | One-year-olds who have received three doses of polio vaccine (Pol3) in a given year, expressed in terms of percentage | SESRIC |
| HSR5 | Births attended by skilled health personnel (%) | Birth attended by Skilled Health worker in a given period (as % of total birth) | IHME-GHDx |
| HSR6 | UHC service coverage index (0 to 100) | Coverage of essential health services | IHME-GHDx |
| ME variables | |||
| ME1 | GDP per capita (current US$) | GDP per capita is gross domestic product divided by midyear population | World Bank |
| ME2 | Employment to population ratio (15+, males) in % | Proportion of a country’s female population (with ages 15+) that is employed, expressed in terms of percentage. | World Bank |
| ME3 | Employment to population ratio (15+, females) in % | Proportion of a country’s male population (with ages 15+) that is employed, expressed in terms of percentage. | World Bank |
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Variables in the Final Model
| Label | N | Min | Max | Mean | SD | Skewness | Kurtosis |
|---|---|---|---|---|---|---|---|
| IMR | 43 | 9.50 | 78.90 | 24.09 | 19.53 | 1.44 | 1.08 |
| SD3 | 43 | 2.57 | 8.13 | 4.64 | 2.013 | 0.64 | -1.24 |
| SD4 | 43 | 55.21 | 69.47 | 61.884 | 5.89 | 0.28 | -1.76 |
| HSR1 | 43 | 29.00 | 99.00 | 83.77 | 21.22 | -1.84 | 1.94 |
| HSR2 | 43 | 51.00 | 99.00 | 94.07 | 10.74 | -3.14 | 9.69 |
| HSR3 | 43 | 10.00 | 99.00 | 88.26 | 23.30 | -2.41 | 4.66 |
| HSR4 | 43 | 18.00 | 99.00 | 88.51 | 23.62 | -2.31 | 3.92 |
| ME1 | 43 | 5073.85 | 24722.64 | 11899.81 | 6770.15 | 0.66 | -1.20 |
| ME2 | 43 | 43.88 | 87.80 | 73.93 | 11.06 | -1.19 | 1.34 |
| ME3 | 43 | 16.07 | 27.59 | 22.16 | 3.18 | -0.07 | -1.17 |
3.2. The Final Model Evaluation Indices
| LV | MV | FL | CA | Rho-A | CR | R2 | Q2 | AVE | HTMT (95% CI) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IMR | ME | SD | HSR | |||||||||
| IMR | IMR | 1.000 | 1.000 | 1.000 | 1.000 | 0.959 | 0.942 | 1.000 | - | - | - | 0.934 (0.854-0.970) |
| ME | ME1 | 0.893 | 0.938 | 0.963 | 0.960 | - | - | 0.889 | 0.851 (0.763-0.910) |
- | - | 0.728 (0.606-0.818) |
| ME2 | 0.946 | |||||||||||
| ME3 | 0.987 | |||||||||||
| SD | SD3 | 0.990 | 0.978 | 0.981 | 0.989 | 0.839 | 0.816 | 0.978 | 0.878 (0.833-0.928) |
0.954 (0.913-0.983) |
- | 0.698 (0.595-0.815) |
| SD4 | 0.988 | |||||||||||
| HSR | HSR1 | 0.944 | 0.978 | 0.979 | 0.984 | 0.521 | 0.474 | 0.940 | - | - | - | - |
| HSR2 | 0.953 | |||||||||||
| HSR3 | 0.992 | |||||||||||
| HSR4 | 0.988 | |||||||||||
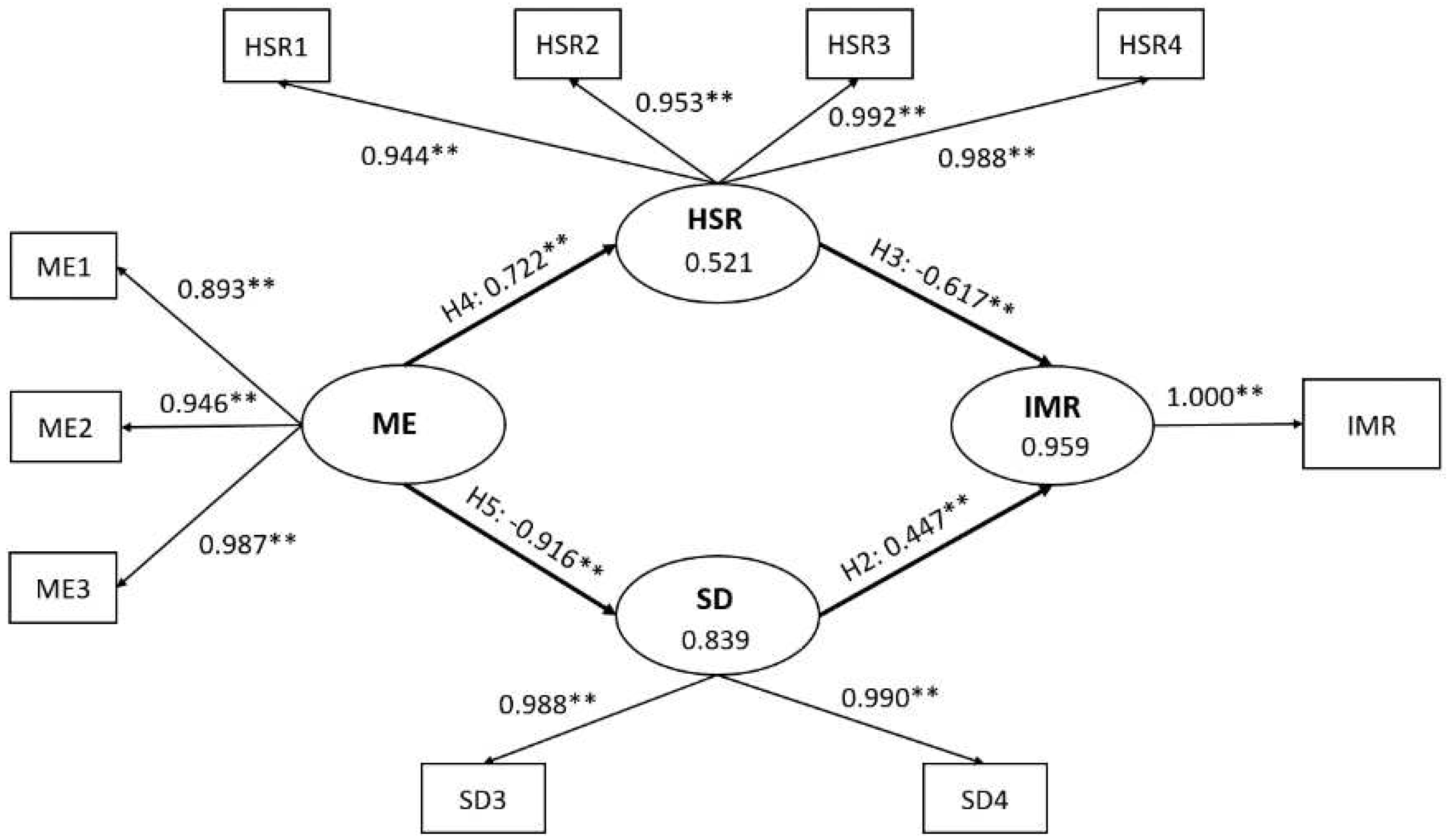
| Hypothesis | Pathway | Direct Effect (95% CI) | Indirect Effect (95% CI) | Total Effect (95% CI) | ƒ2 |
|---|---|---|---|---|---|
| H1 | ME→IMR | - | -0.854 (-0.898 to -0.790) | -0.854 (-0.898 to -0.790) | - |
| H2 | SD→IMR | 0.447 (0.327 to 0.601) | - | 0.447 (0.327 to 0.601) | 2.560 |
| H3 | HSR→IMR | -0.617 (-0.712 to -0.458) | - | -0.617 (-0.712 to -0.458) | 4.891 |
| H4 | ME→HSR | 0.722 (0.605 to 0.806) | - | 0.722 (0.605 to 0.806) | 1.087 |
| H5 | ME→SD | -0.916 (-0.945 to -0.880) | - | -0.916 (-0.945 to -0.880) | 5.193 |
| H6 | SD→HSR | - | - | - | - |
4. Discussion
4.1. The Effects of SD Determinants on IMR
4.2. The Effects of HSR Determinants on IMR
4.3. The Effects of ME Determinants on IMR
4.4. The Effects of ME Determinants on HSR
4.5. The Effects of ME Determinants on SD
4.6. Strengths and Limitations of this Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Infant Mortality Rate (between birth and 11 months per 1000 live births). Indicator Metadata Registry List 2022 [cited 2022 October 9]; Available from: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/1.
- CDC, Principles of Epidemiology in Public Health Practice. 2006: U.S. department of health and human services.
- Gonzalez, R.M. and D. Gilleskie, Infant mortality rate as a measure of a country’s health: a robust method to improve reliability and comparability. Demography, 2017. 54(2): p. 701-720. [CrossRef]
- World Health Organization, Millennium development goals, the health indicators: scope, definitions and measurement methods. 2003.
- United Nations. The 17 goals | sustainable development. 2022 [cited 2023 05/03]; Available from: https://sdgs.un.org/goals.
- 6. UN-IGME, Levels & Trends in Child Mortality, United Nations Inter-Agency Group for Child Mortality Estimation (UN IGME), Report 2021. 2022, UNICEF.
- World Health Organization. Infant Mortality. 2018 [cited 2022 26/09]; Available from: https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/infant-mortality.
- Salam, A.A. and R.M. Al-Khraif, Child Mortality Transition in the Arabian Gulf: Wealth, Health System Reforms, and Development Goals. Frontiers in public health, 2020. 7: p. 402. [CrossRef]
- National Centre for Statistics and Information. Data Portal - Population - Infant Mortality Rate. 2021.
- Kim, D. and A. Saada, The social determinants of infant mortality and birth outcomes in Western developed nations: a cross-country systematic review. International Journal of environmental research and public health, 2013. 10(6): p. 2296-2335. [CrossRef]
- Bugelli, A., et al., The Determinants of Infant Mortality in Brazil, 2010–2020: A Scoping Review. International Journal of environmental research and public health, 2021. 18(12): p. 6464.
- Khadka, K.B., et al., The socioeconomic determinants of infant mortality in Nepal: analysis of Nepal Demographic Health Survey, 2011. BMC Pediatrics, 2015. 15(1): p. 1-11. [CrossRef]
- Kothari, C.L., et al., Race, Multiraciality, Income, and Infant Mortality: Markers of Racial Equity. Journal of Child & Family Studies, 2022. 31(3): p. 689-702. [CrossRef]
- Rezaei, S., K. Jamshidi, and K. Moradi, Impact of socioeconomic and health system factors on infant mortality rate in Organization of the Petroleum Exporting Countries (OPEC): evidence from 2004 to 2013. International Journal of Pediatrics, 2015. 3(2-2): p. 493-499.
- Tüzün, H., Factors Related to Infant Mortality Rate and Under-Five Mortality Rate in Turkey: An Ecological Study with Provincial Data. Türkiye’de Bebek Ölüm Hızı ve Beş Yaş Altı Çocuk Ölüm Hızıyla İlişkili Etmenler: İl Verileriyle Ekolojik Bir Araştırma., 2021. 21(3): p. 221-230. [CrossRef]
- Valcin, J., et al., Mortality, morbidity and clinical care in a referral neonatal intensive care unit in Haiti. PLoS ONE, 2020. 15(10). [CrossRef]
- Leal, M.d.C., et al., Determinants of infant mortality in the Jequitinhonha Valley and in the North and Northeast regions of Brazil. Revista de saude publica, 2017. 51.
- The Global Health Observatory. UHC service coverage index (3.8.1). n.d. [cited 2023; Available from: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/4834.
- Lozano, R., et al., Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 2020. 396(10258): p. 1250-1284. [CrossRef]
- G. B. D. Universal Health Coverage Collaborators, Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (British edition), 2020. 396(10258): p. 1250-1284.
- Tarekegn, W., S. Tsegaye, and Y. Berhane, Skilled birth attendant utilization trends, determinant and inequality gaps in Ethiopia. BMC Women’s Health, 2022. 22(1): p. 1-9. [CrossRef]
- Ayele, G.S., A.T. Melku, and S.S. Belda, Utilization of skilled birth attendant at birth and associated factors among women who gave birth in the last 24 months preceding the survey in Gura Dhamole Woreda, Bale zone, southeast Ethiopia. BMC public health, 2019. 19(1): p. 1-14. [CrossRef]
- 23. WHO. Vaccines and Immunization. 2022; Available from: https://www.who.int/health-topics/vaccines-and-immunization#tab=tab_1.
- Costa-Nobreid, D.T., et al., Clusters of cause specific neonatal mortality and its association with per capita gross domestic product: a structured spatial analytical approach. PLoS ONE, 2021. 16(8).
- Shapira, G., D.d. Walque, and J. Friedman, How many infants may have died in low-income and middle-income countries in 2020 due to the economic contraction accompanying the COVID-19 pandemic? Mortality projections based on forecasted declines in economic growth. BMJ Open, 2021. 11(8). [CrossRef]
- Abdul Salam, A., et al., Components and public health impact of population growth in the Arab world. PloS one, 2015. 10(5): p. e0124944. [CrossRef]
- Bader, Y. and S. Ganguli, Analysis of the association between economic growth, environmental quality and health standards in the Gulf Cooperation Council during 1980-2012. Management of Environmental Quality, 2019. 30(5): p. 1050-1071. [CrossRef]
- Al-Azri, M., F. Al-Mamari, and S. Mondal, Healthcare expenditure and health outcome nexus: Exploring the evidences from Oman. Journal of Public Affairs, 2020. 20(4): p. e2329. [CrossRef]
- Eltayib, R.A.A., et al., The impact of sociodemographic, macroeconomic, and health status and resources determinants on infant mortality rates in the Gulf Cooperation Council (GCC) countries: A systematic review and meta-analysis. Journal of Neonatal Nursing, 2023. [CrossRef]
- Abu-Heija, A.T., M. Al-Bash, and M. Mathew, Gestational and Pregestational Diabetes Mellitus in Omani Women. مرض السكري خلال الحمل وما قبل الحمل عندالنساء العمانيات, 2015. 15(4): p. 496-500. [CrossRef]
- Patel, P.K., Profile of major congenital anomalies in the Dhahira region, Oman. Annals of Saudi Medicine, 2007. 27(2): p. 106-111.
- Rahman, A., et al., Changing Survival Rate of Infants Born Before 26 Gestational Weeks. تغير معدل البقاء للرضع المواليد قبل الأسبوع 26 من الحمل, 2015. 15(3): p. e351-e355. [CrossRef]
- Abdellatif, M., et al., The Patterns and Causes of Neonatal Mortality at a Tertiary Hospital in Oman. Oman Medical Journal, 2013. 28(6): p. 422-426. [CrossRef]
- Al-Haddabi, R., et al., Obstetric and perinatal outcomes of teenage pregnant women attending a tertiary teaching hospital in Oman. Oman Medical Journal, 2014. 29(6): p. 399-403. [CrossRef]
- Al Riyami, N., A. Al-Rusheidi, and M. Al-Khabori, Perinatal Outcome of Monochorionic in Comparison to Dichorionic Twin Pregnancies. Oman Medical Journal, 2013. 28(3): p. 173-177. [CrossRef]
- Al-Shukri, M., et al., Maternal and fetal outcomes of triplet gestation in a tertiary hospital in Oman. Sultan Qaboos University medical journal, 2014. 14(2): p. e204-e210.
- National Centre for Statistics and Information. Data Portal. 2021; Available from: https://data.gov.om/.
- The GCC Statistical Centre. Statistics. 2023; Available from: https://gccstat.org/en/statistic/statistics.
- The World Bank. World Bank Open Data. 2023 [cited 2023 05/03]; Available from: https://data.worldbank.org/.
- 40. SESRIC. OIC Statistics Database (OICStat). 2023; Available from: https://www.sesric.org/oicstat.php.
- Institute for Health Metrics and Evaluation (IHME). The Global Health Data Exchange (GHDx) data catalog. 2023 [cited 2023 05/03]; Available from: https://ghdx.healthdata.org/.
- Cohen, J., Statistical Power Analysis for the Behavioral Sciences. 2nd ed. 1988, New York: Routledge.
- Hair, J.F., et al., Multivariate data analysis. 8th ed. 2018: Cengage Learning EMEA.
- Chan, M.F., Factors affecting infant mortality rates: evidence from 1969–2008 data in Singapore. Journal of Public Health, 2011. 19: p. 15-22. [CrossRef]
- Wirayuda, A.A.B., et al., A structural equation model to explore sociodemographic, macroeconomic, and health factors affecting life expectancy in Oman. The Pan African Medical Journal, 2022. 41. [CrossRef]
- Wirayuda, A.A.B., A. Al-Mahrezi, and M.F. Chan, Factors Impacting Life Expectancy in Bahrain: Evidence from 1971 to 2020 Data. International Journal of Health Services, 2022: p. 00207314221129052. [CrossRef]
- Chan, M.F. and M. Kamala Devi, Factors affecting life expectancy: evidence from 1980-2009 data in Singapore, Malaysia, and Thailand. Asia Pacific Journal of Public Health, 2015. 27(2): p. 136-146.
- Ibrahim, A., et al., Socioeconomic Risk Factors for Hospital-based Neonatal Death: A Population-based Study. Asploro Journal of Pediatrics and Child Health, 2021. 2020(3): p. 72.
- Almasi-Hashiani, A., et al., The correlation of human development index on fertility and mortality rate: a global ecological study. International Journal of Pediatrics, 2016. 4(12): p. 4071-4080.
- Awaidy, S., et al., Progress Towards Measles Elimination: Oman Experience. SM Vaccine Vaccin, 2015. 1(1): p. 1004-1009.
- Abuqamar, M., D. Coomans, and F. Louckx, Correlation between socioeconomic differences and infant mortality in the Arab World (1990-2009). International Journal of Sociology and Anthropology, 2011. 3(1): p. 15.
- Rahman, S., et al., SOCIODEMOGRAPHIC, OBSTETRIC AND FETAL DETERMINANTS OF NEONATAL MORTALITY. NEONATAL AND PERINATAL MORTALITY, 2017: p. 43.
- Hair Jr, J.F., et al., Partial least squares structural equation modeling (PLS-SEM) using R: A workbook. 2021, Springer Nature.
- Hair, J.F., et al., Mirror, mirror on the wall: a comparative evaluation of composite-based structural equation modeling methods. Journal of the academy of marketing science, 2017. 45(5): p. 616-632. [CrossRef]
- Chin, W., et al., Demystifying the role of causal-predictive modeling using partial least squares structural equation modeling in information systems research. Industrial Management & Data Systems, 2020. [CrossRef]
- Jöreskog, K.G. and D. Sörbom, PRELIS 2 user’s reference guide: A program for multivariate data screening and data summarization: A preprocessor for LISREL. 1996: Scientific Software International.
- Henseler, J., On the convergence of the partial least squares path modeling algorithm. Computational statistics, 2010. 25(1): p. 107-120. [CrossRef]
- Hair, J.F., C.M. Ringle, and M. Sarstedt, PLS-SEM: Indeed a silver bullet. Journal of Marketing theory and Practice, 2011. 19(2): p. 139-152.
- Henseler, J., C.M. Ringle, and M. Sarstedt, A new criterion for assessing discriminant validity in variance-based structural equation modeling. Journal of the academy of marketing science, 2015. 43(1): p. 115-135. [CrossRef]
- Franke, G. and M. Sarstedt, Heuristics versus statistics in discriminant validity testing: a comparison of four procedures. Internet Research, 2019. [CrossRef]
- Chin, W.W., How to write up and report PLS analyses, in Handbook of partial least squares. 2010, Springer. p. 655-690.
- Roemer, E., F. Schuberth, and J. Henseler, HTMT2–an improved criterion for assessing discriminant validity in structural equation modeling. Industrial management & data systems, 2021. [CrossRef]
- Hair, J.F., et al., A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM). Second ed. 2017: SAGE Publications, Inc.
- Aguirre-Urreta, M.I. and M. Rönkkö, Statistical inference with PLSc using bootstrap confidence intervals. MIS quarterly, 2018. 42(3): p. 1001-1020. [CrossRef]
- Streukens, S. and S. Leroi-Werelds, Bootstrapping and PLS-SEM: A step-by-step guide to get more out of your bootstrap results. European Management Journal, 2016. 34(6): p. 618-632. [CrossRef]
- Shmueli, G., et al., The elephant in the room: Predictive performance of PLS models. Journal of Business Research, 2016. 69(10): p. 4552-4564. [CrossRef]
- Hair, J.F., et al., When to use and how to report the results of PLS-SEM. European business review, 2019. 31(1): p. 2-24. [CrossRef]
- Hair, J.F., et al., The use of partial least squares structural equation modeling in strategic management research: a review of past practices and recommendations for future applications. Long range planning, 2012. 45(5-6): p. 320-340. [CrossRef]
- Subramaniam, T., et al., Determinants of infant mortality in older ASEAN economies. Social Indicators Research, 2018. 136: p. 397-415. [CrossRef]
- Neiger, R., Long-term effects of pregnancy complications on maternal health: a review. Journal of clinical medicine, 2017. 6(8): p. 76. [CrossRef]
- Hauspurg, A., et al., Adverse pregnancy outcomes and future maternal cardiovascular disease. Clinical cardiology, 2018. 41(2): p. 239-246. [CrossRef]
- Yang, W., et al., Relationship between gestational weight gain and pregnancy complications or delivery outcome. Scientific reports, 2017. 7(1): p. 12531. [CrossRef]
- Vilanova, C.S., et al., The relationship between the different low birth weight strata of newborns with infant mortality and the influence of the main health determinants in the extreme south of Brazil. Population health metrics, 2019. 17(1): p. 1-12. [CrossRef]
- Anele, C.R., et al., The influence of the municipal human development index and maternal education on infant mortality: an investigation in a retrospective cohort study in the extreme south of Brazil. BMC Public Health, 2021. 21(1): p. 1-12. [CrossRef]
- Munoz, F.M., Current challenges and achievements in maternal immunization research. Frontiers in Immunology, 2018. 9: p. 436. [CrossRef]
- David, J., Infant mortality and public health expenditure in Nigeria: Empirical explanation of the nexus. Timisoara Journal of Economics and Business (TJE&B), 2018. 11(2): p. 149-164. [CrossRef]
- Department of Surveillance & Disease Control, Manual on Expanded Program on Immunization. 2002, Directorate General of Health Affairs.
- Al-Abri, S.S., et al., Effective vaccine management and Oman’s healthcare system’s challenge to maintain high global standards. Journal of infection and public health, 2018. 11(5): p. 742-744. [CrossRef]
- Abbuy, K.E., Macroeconomic Determinants of Infant Mortality in WAEMU Countries: Evidence from Panel Data Analysis. 2018.
- Genowska, A., et al., Converging or diverging trajectories of mortality under one year of age in the Baltic States: a comparison with the European Union. Archives of Public Health, 2021. 79(76). [CrossRef]
- Ortigoza, A.F., et al., Characterising variability and predictors of infant mortality in urban settings: findings from 286 Latin American cities. J Epidemiol Community Health, 2021. 75(3): p. 264-270. [CrossRef]
- Jagrič, T., et al., Economic Impact of the Health Sector on the Regional Level-Case of a Small, Open Economy. Lex Localis, 2021. 19(3): p. 621-657.
- Naik, Y., et al., Going upstream–an umbrella review of the macroeconomic determinants of health and health inequalities. BMC Public Health, 2019. 19(1): p. 1-19. [CrossRef]
- Rezapour, A., et al., Factors affecting healthcare sector inflation rate in Iran’s provinces for 2004-2015. International Transaction Journal of Engineering, Management, & Applied Sciences & Technologies, 2020. 11(2).
- Finlay, J.E., I. Mejia-Guevara, and Y. Akachi, Inequality in total fertility rates and the proximate determinants of fertility in 21 sub-Saharan African countries. PloS one, 2018. 13(9): p. e0203344. [CrossRef]
- Pezzulo, C., et al., Geographical distribution of fertility rates in 70 low-income, lower-middle-income, and upper-middle-income countries, 2010–16: a subnational analysis of cross-sectional surveys. The Lancet Global Health, 2021. 9(6): p. e802-e812. [CrossRef]
- Furstenberg, F.F., Family change in global perspective: How and why family systems change. 2019, Wiley Online Library. p. 326-341. [CrossRef]
- Islam, M.M., Demographic transition in Sultanate of Oman: emerging demographic dividend and challenges. Middle East Fertility Society Journal, 2020. 25(1): p. 1-14. [CrossRef]
- Schrecker, T. and C. Bambra, How politics makes us sick: Neoliberal epidemics. 2015.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





