Submitted:
10 April 2023
Posted:
11 April 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Integrative Medicine Assessment and Treatment Methods
Autonomic Response Testing (ART)
Low Dose Immunotherapy (LDI)
Low Nickel Diet
Supplementation with gamma linolenic acid (GLA)
EDTA
Case Reports

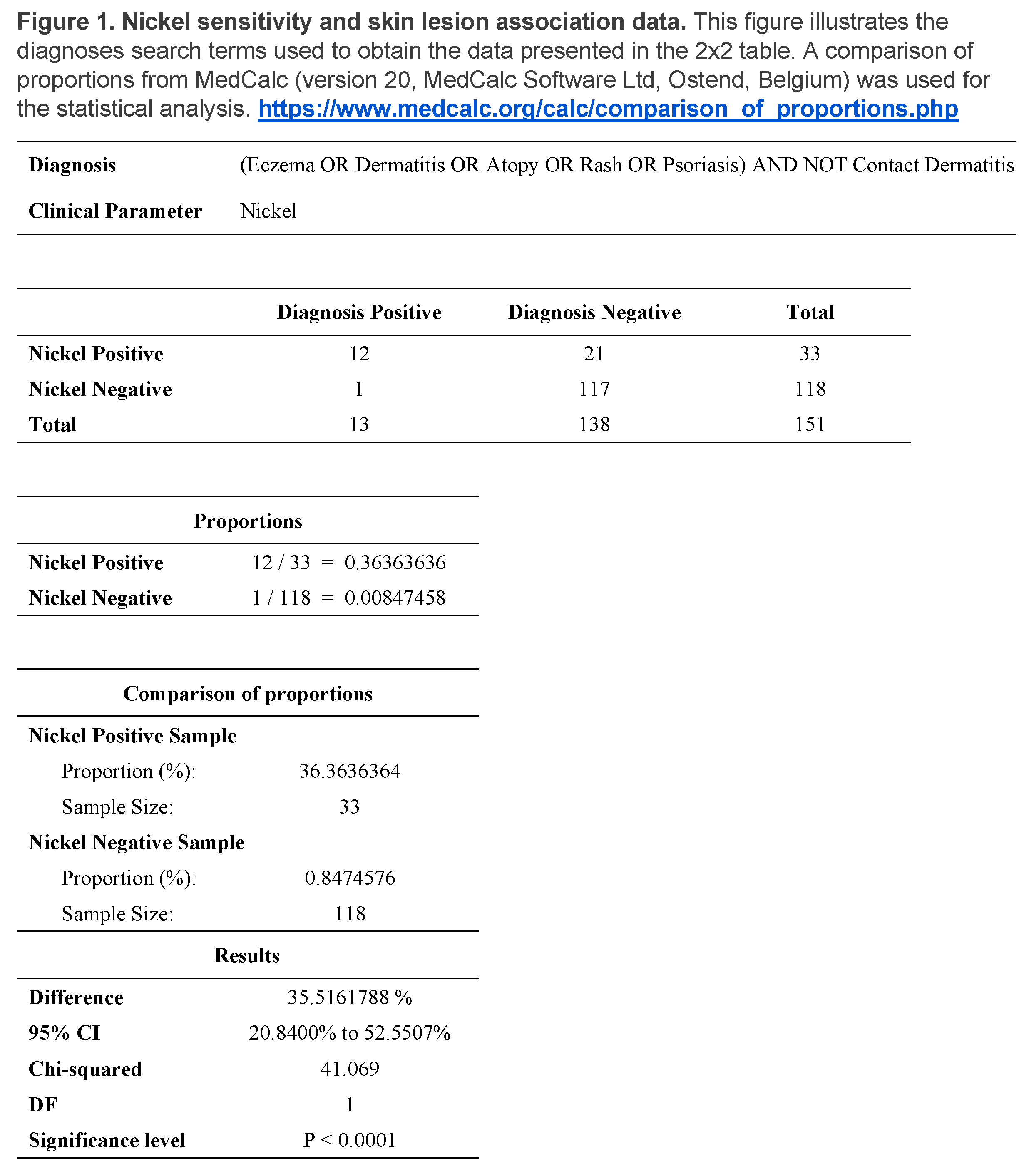
Clinical Practice Survey of association of nickel sensitivity with presence of skin lesions
Discussion
Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schmidt, M.; Goebeler, M. Immunology of metal allergies. J Dtsch Dermatol Ges 2015, 13, 653–660. [Google Scholar] [CrossRef]
- Jacob, S.E.; Goldenberg, A.; Pelletier, J.L.; Fonacier, L.S.; Usatine, R.; Silverberg, N. Nickel Allergy and Our Children's Health: A Review of Indexed Cases and a View of Future Prevention. Pediatric dermatology 2015, 32, 779–785. [Google Scholar] [CrossRef]
- Mukovozov, I.M.; Kashetsky, N.; de Gannes, G. Prevalence of Contact Allergy to Nickel: A Retrospective Chart Review. Dermatitis 2022, 33, 355–361. [Google Scholar] [CrossRef]
- Cattani, C.A.S.; Oppermann, K.; Perazzoli, S.; Guarda, N.H.; Baréa, P.; Bonamigo, R.R. Sensitizing agents found in children and adolescents with recalcitrant atopic dermatitis: a cross-sectional study with a pediatric battery. Anais brasileiros de dermatología 2022, 97, 307–314. [Google Scholar] [CrossRef]
- Mahlberg, S.; Scarberry, K.B.; Nedorost, S. Association Between Dyshidrotic Dermatitis and Metal Allergy: An Evaluation of 1,613 Patch Tests. Dermatitis 2022, 33, e37. [Google Scholar] [CrossRef]
- Yoshihisa, Y.; Shimizu, T. Metal Allergy and Systemic Contact Dermatitis: An Overview. Dermatology research and practice 2012, 2012, 749561–749565. [Google Scholar] [CrossRef]
- Hsu, J.W.; Matiz, C.; Jacob, S.E. Nickel Allergy: Localized, Id, and Systemic Manifestations in Children: Nickel Allergy Manifestations. Pediatric dermatology 2011, 28, 276–280. [Google Scholar] [CrossRef]
- Zirwas, M.J.; Molenda, M.A. Dietary nickel as a cause of systemic contact dermatitis. J Clin Aesthet Dermatol 2009, 2, 39–43. [Google Scholar]
- Hosoki, M.; Bando, E.; Asaoka, K.; Takeuchi, H.; Nishigawa, K. Assessment of allergic hypersensitivity to dental materials. Bio-medical materials and engineering 2009, 19, 53–61. [Google Scholar] [CrossRef]
- Jensen, C.S.; Menné, T.; Duus Johansen, J. Systemic contact dermatitis after oral exposure to nickel: a review with a modified meta-analysis. Contact dermatitis 2006, 54, 79–86. [Google Scholar] [CrossRef]
- Hadasik, K.; Bergler-Czop, B.; Miziołek, B.; Salwowska, N.; Skrzypek-Salamon, A. Pruritus ani and perianal eczema as a manifestation of systemic contact dermatitis. Postȩpy dermatologii i alergologii 2017, 34, 174–176. [Google Scholar] [CrossRef]
- Alanko, K.; Kanerva, L.; Jolanki, R.; Kannas, L.; Estlander, T. Oral mucosal diseases investigated by patch testing with a dental screening series. Contact dermatitis 1996, 34, 263–267. [Google Scholar] [CrossRef]
- Muris, J.; Feilzer, A. Micro analysis of metals in dental restorations as part of a diagnostic approach in metal allergies. Neuro endocrinology letters 2007, 27 Suppl 1, 49–52. [Google Scholar]
- Forsell, M.; Marcusson, J.A.; Carlmark, B.; Johansson, O. Analysis of the metal content of in vivo-fixed dental alloys by means of a simple office procedure. Swed Dent J 1997, 21, 161–168. [Google Scholar]
- Pigatto, P.D.; Brambilla, L.; Ferrucci, S.; Zerboni, R.; Somalvico, F.; Guzzi, G. Systemic allergic contact dermatitis associated with allergy to intraoral metals. Dermatol Online J 2014, 20. [Google Scholar] [CrossRef]
- Brera, S.; Nicolini, A. Respiratory manifestations due to nickel. Acta Otorhinolaryngol Ital 2005, 25, 113–115. [Google Scholar]
- Altsushi, M. [A case report of a metal allergy patient whose prosthesis was identified allergenic by non-destructive metal element analysis and a dermatological patch test]. Nihon Hotetsu Shika Gakkai Zasshi 2006, 50, 276–279. [Google Scholar] [CrossRef]
- Chung, M.; Richmond, J.; LaRiccia, P. Successful Integrative Medicine Assessment and Treatment of Chronic Allergic Rhinitis, Asthma and Eczema Related to a Metal Dental Crown: Case Report. Chronicity 2019, 11, 11–16. [Google Scholar]
- Walther, D. Applied Kineseology, Synopsis 2nd Edition, 2nd ed.; Triad of Health Pulishing: Shawnee Mission, KS 66202, 2016. [Google Scholar]
- Klinghardt, D.; Williams, L. Autonomic Response Testing (workshop manual). self-Published: Woodinville, WA, 1996.
- Healing, K.I.-t.H.o. https://klinghardtinstitute.com/. Available online: (accessed on 3/30/23).
- Klinghardt, D; with editing Derksen, A. Klinghardt D; with editing Derksen, A. ART I Autonomic Response Testing (Workshop Manual). 2009.
- Frandsen, A.; McClure, M.; Chung, M.K.; Lariccia, P.J. Autonomic response testing compared with immunoglobulin e allergy panel test results: Preliminary report. Alternative therapies in health and medicine 2018, 24, 10–14. [Google Scholar]
- Couture, D.C.; Chung, M.K.; Shinnick, P.; Curzon, J.; McClure, M.J.; Lariccia, P.J. Integrative Medicine Approach to Pediatric Obsessive-Compulsive Disorder and Anxiety: a Case Report. Global advances in health and medicine 2016, 5, 117–121. [Google Scholar] [CrossRef]
- Brobyn, T.L., P. J. Successful Treatment of Chronic Edema, Recurrent Cellulitis and Leg Pain using Autonomic Response Testing Assessment: Case Report. Journal of the Science of Healing Outcomes 2017, 9, 10. [Google Scholar]
- Chung, M.K.; LaRiccia, P.J. Successful Integrative Medicine Assessment and Treatment of Chronic Pain Associated With Breast Surgery: A Report of 3 Cases. Holist Nurs Pract 2017, 31, 21–29. [Google Scholar] [CrossRef]
- Brobyn, T.L.; Chung, M.K. Clinical Roundup: Selected Treatment Options for Mood Disorders—Part 2 The use of autonomic response testing and the 5 phases paradigm to identify unresolved feelings in patients with mood disorders. Alternative and Complementary Therapies 2015, 21, 182–188. [Google Scholar] [CrossRef]
- Chung, M.; LaRiccia, P. How Do You Deactivate Painful Scars in Your Practice? Medical acupuncture 2016, 28, 162–167. [Google Scholar] [CrossRef]
- Vincent, T. Low Dose Immunotherapy (LDI) for Autoimmune Diseases and Chronic Inflammatory Disorders (providers manual). 2018.
- Global Immunotherapy LLC. Available online: https://globalimmunotherapy.com/ (accessed on 3/30/23).
- Shrader, W.A. Low dose allergen immunotherapy (LDA): the allergy treatment of the future - here now. Townsend letter 2012, 46. [Google Scholar]
- Santa Fe Center for Allergy and Environmental Medicine. Available online: http://drshrader.com/ (accessed on 3/30/23).
- Da Mata Perez, L.; Franca, A.T.; Zimmerman, J.R. Systemic nickel allergy syndrome. The World Allergy Organization journal 2015, 8, A89–A89. [Google Scholar] [CrossRef]
- Sharma, A. Low nickel diet in dermatology. Indian journal of dermatology 2013, 58, 240–240. [Google Scholar] [CrossRef]
- Horrobin, D.F. Fatty acid metabolism in health and disease: the role of Δ-6-desaturase. The American journal of clinical nutrition 1993, 57, 732S–737S. [Google Scholar] [CrossRef]
- Allergy Research Group. Available online: https://www.allergyresearchgroup.com/content/97.pdf (accessed on 2/28/23).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




