1. Introduction
Recently, clear aligners are highly demanded by patients, compared to fixed orthodontic braces, due to their comfort and their transparent esthetic appearance [
1,
2,
3]. From the time when the CAD/CAM process and the intraoral scanners found their way into aligner therapy, the manufacturing workflow of aligners became completely digital with less effort and time [
4]. The force system of orthodontic aligners is not fully understood yet, consequently, their clinical outcomes are less predictable [
5,
6,
7,
8]. However, it is postulated that force with aligners is generated via two mechanisms acting in the same time. The first mechanism is a returning force on the targeted tooth, which is created by the local elastic deformation of the part of the aligner that is in contact with this tooth. The second mechanism is another returning force caused by the elastic deformation of the entire aligner, which occurs when the tooth to be moved does not align properly with the rest of the teeth, and the aligner is held in place by friction against the other teeth. Additionally, the initial tooth mobility due to deformation of the periodontal ligament plays a prominent role [6, 9–11].
The performance of orthodontic aligners is strongly affected by the utilized material [5, 6, 8, 12, 13]. Optimally, orthodontic materials should exert continuous light force over time, and the material should always return to its original shape after removal from the mouth [7, 14]. For that, the ideal material should have some stiffness, enough to apply required light force, and with a high elastic limit, to avoid the permanent deformation [
15]. The commonly used aligner sheets are composed of viscoelastic thermoplastic polymers [4, 13, 16, 17]. The mechanical properties of the thermoformed sheets differ significantly from those of the raw ones [5, 18]. Moreover, viscoelastic materials show creep and stress relaxation phenomena, which means that their mechanical behavior varies significantly under loading over time [15, 19]. Common thermoforming sheets in orthodontics consist of ethylene vinyl acetate (EVA), polypropylene (PP), polystyrene (PS), polyethylene terephthalate (PET), polyethylene terephthalate glycol (PET-G), thermoplastic polyurethane (TPU), or polycarbonate (PC) [4, 13, 20].
Patients are instructed to wear their aligner splints for at least 22 hours a day, only removing them for eating and brushing their teeth. Each splint of the aligner series is worn for approximately two weeks before being replaced with the next one [
16]. As a result, the aligners experience intermittent thermal and mechanical loads. Short-term mechanical loads occur during insertion and removal of the aligners, while long-term loads are due to continuous contact between the aligners and the misaligned teeth, as well as the force of chewing [
11]. Thus, to accurately study the behavior of aligners, it is necessary to conduct an
in vivo study or replicate the clinical situation
in vitro [
21].
Experimental studies have shown that only storage in aging agent has no significant effect on force generation by aligners [11, 21, 22]. On the contrary, thermal and mechanical loading have a significant impact on the mechanical properties of aligner materials, resulting in increased hardness [
23,
24,
25], reduced elasticity, and decreased strength [26, 27]. Others [19, 28, 29] reported that aligner materials show a significant force-drop at the first few hours of use.
To our knowledge, to date, there are very few studies in the literature that report on the effect of the thermo-mechanical aging on the 3D force systems by aligners, and no study reported that on the upper premolar tooth. Therefore, the purpose of the current in vitro experiment is to investigate the impact of thermocycling and mechanical loading on thermoformed orthodontic aligners made from thermoplastic polyurethane (TPU) sheets and investigate their effects on force and torque generation.
2. Materials and Methods
Ten resin models of an upper jaw were produced made of a fast-curing cold-curing resin (Technovit 4004; Kulzer, Hanau, Germany). Five identical models were aligned, and the other identical five models were malaligned (to simulate a mechanical loading), in which the upper left second premolar (Tooth 25) was shifted bodily 0.2 mm towards the vestibular side.
Ten aligners were fabricated over one of the aligned models, by thermoforming ten thermoplastic sheets of a polyurethane material (Zendura™; Bay Materials, Fremont, USA) with a thickness of 0.75 mm. The thermoforming process was performed with a standard thermoforming device (Ministar S
®; Scheu-Dental, Iserlohn, Germany; code 132, temperature: 220 °C, heating time 35 seconds, pressure 4.8 Bar; manufacturer's guidelines). The thermoformed aligners were then trimmed in a scalloped form following the gingival margin (
Figure 1). All aligners were thermoformed and trimmed identically on the same model and by one well-trained technician, so that the influence of the aligner trimming design on the measurements should be negligible.
To mimic the typical two-week wear time of orthodontic aligners, the aligners were kept for 14 days in a thermocycler device (Thermocycler THE-1100; SD Mechatronik, Feldkirchen-Westerham, Germany). The two basins of the thermocycler were filled with deionized water (Ampuwa; Fresenius Kabi, Bad Homburg, Germany). Each thermo-cycle lasted for 94 seconds, 87 seconds of storage in a warm basin at 37 °C, one second of draining time, and one second of storage in a cold basin at 6 °C.
All the ten aligners were thermocycled while being kept in their position on a resin model, where half of them were kept on 5 aligned models (pure thermocycling), while the second half were stored on 5 malaligned models (thermocycling and mechanical loading because of the misalignment of tooth 25).
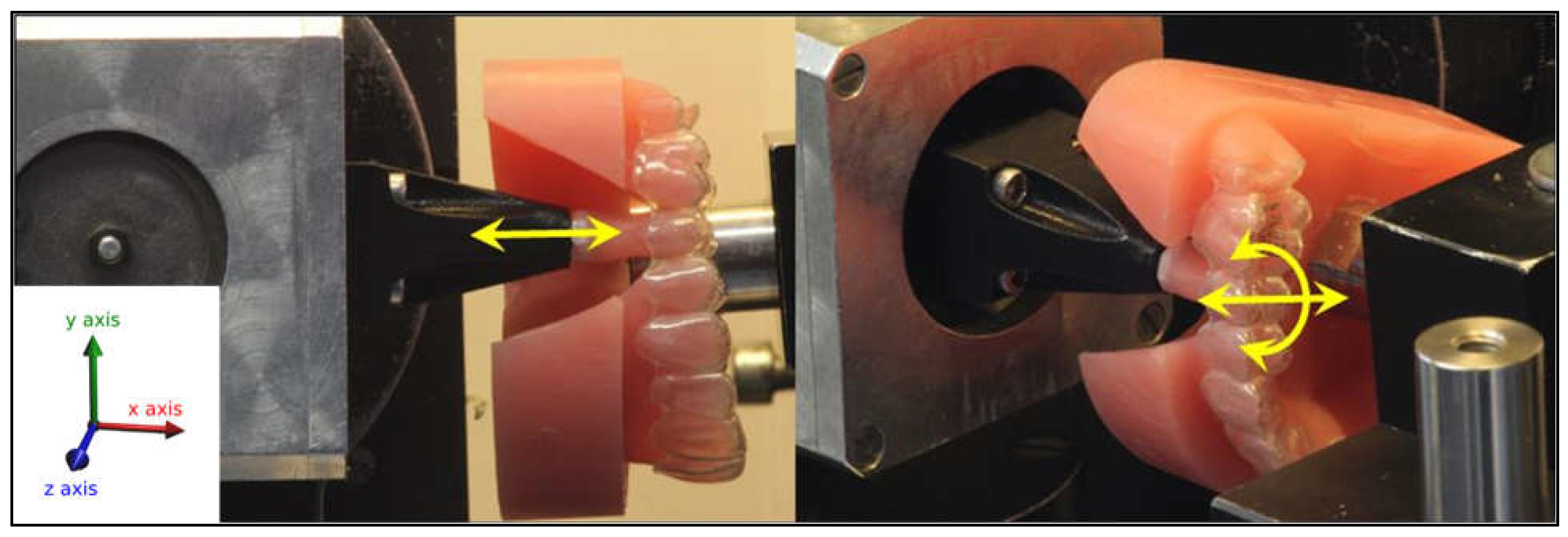
The orthodontic measurement and simulation system (OMSS) was used for the biomechanical measurements [11, 16, 30–32]. The OMSS is a custom-made mechanical device used to measure biomechanical characteristics. It is a software-controlled system that is used to perform virtual simulation of orthodontic movements. It consists of two sensors mounted on a 3D-mobilized platform that can measure forces and torques in three planes. Additionally, the set-up is housed in a temperature-controlled chamber (
Figure 1). In the current experiment, an additional resin model was created for the OMSS measurement, in which tooth 25 was sawn out and its surrounding teeth were slightly reduced to ensure a smooth movement of the tooth during simulation. Tooth 25 was then attached to one sensor of the OMSS and the resin model was fixed with the occlusal plane of the model parallel to the sensor axis. The tooth was positioned in its neutral position in the dental arch to eliminate any forces or torques on the tooth in its starting position (
Figure 1).
In the current experiment, the force/torque measurements were carried out before the thermocycling (day 0, the reference measurement) and on the 2
nd, 4
th, 6
th, 10
th, and 14
th days (±2 hours) after the start of the thermocycling. The measuring unit with the tooth was moved in the X- (intrusion/extrusion) and Z- (oro-vestibular translation) axes by ±0.2 mm in 0.01 mm increments and rotated around the X-axis (rotation around the tooth axis) by ±2° in both directions in 0.1° increments, where positive (+) represents extrusion, vestibular, mesial movement, and vice versa (
Figure 1). After each measurement, the adjustment of the measurement setup was checked and corrected if necessary.
For each measurement, aligners were kept in the thermocycling system container and only removed briefly at the targeted time interval for assembly in the OMSS and then were returned back to the container immediately after the measurements were completed. The measurements of ten aligners lasted up to two hours. For each measurement, force/translation and torque/rotation curves were recorded and processed for subsequent data analysis.
Figure 1.
Resin model with aligner fitted into the orthodontic measurement and simulation system (OMSS): Tooth 25 was separated and adjusted in the neutral position in the aligner. Simulation of three tooth movements were carried out: intrusion/extrusion by 0.2 mm (X-axis) (left), oro-vestibular translation by 0.2 mm (Z-axis) and 2° rotation around the tooth axis in either direction (right).
Figure 1.
Resin model with aligner fitted into the orthodontic measurement and simulation system (OMSS): Tooth 25 was separated and adjusted in the neutral position in the aligner. Simulation of three tooth movements were carried out: intrusion/extrusion by 0.2 mm (X-axis) (left), oro-vestibular translation by 0.2 mm (Z-axis) and 2° rotation around the tooth axis in either direction (right).
4. Results
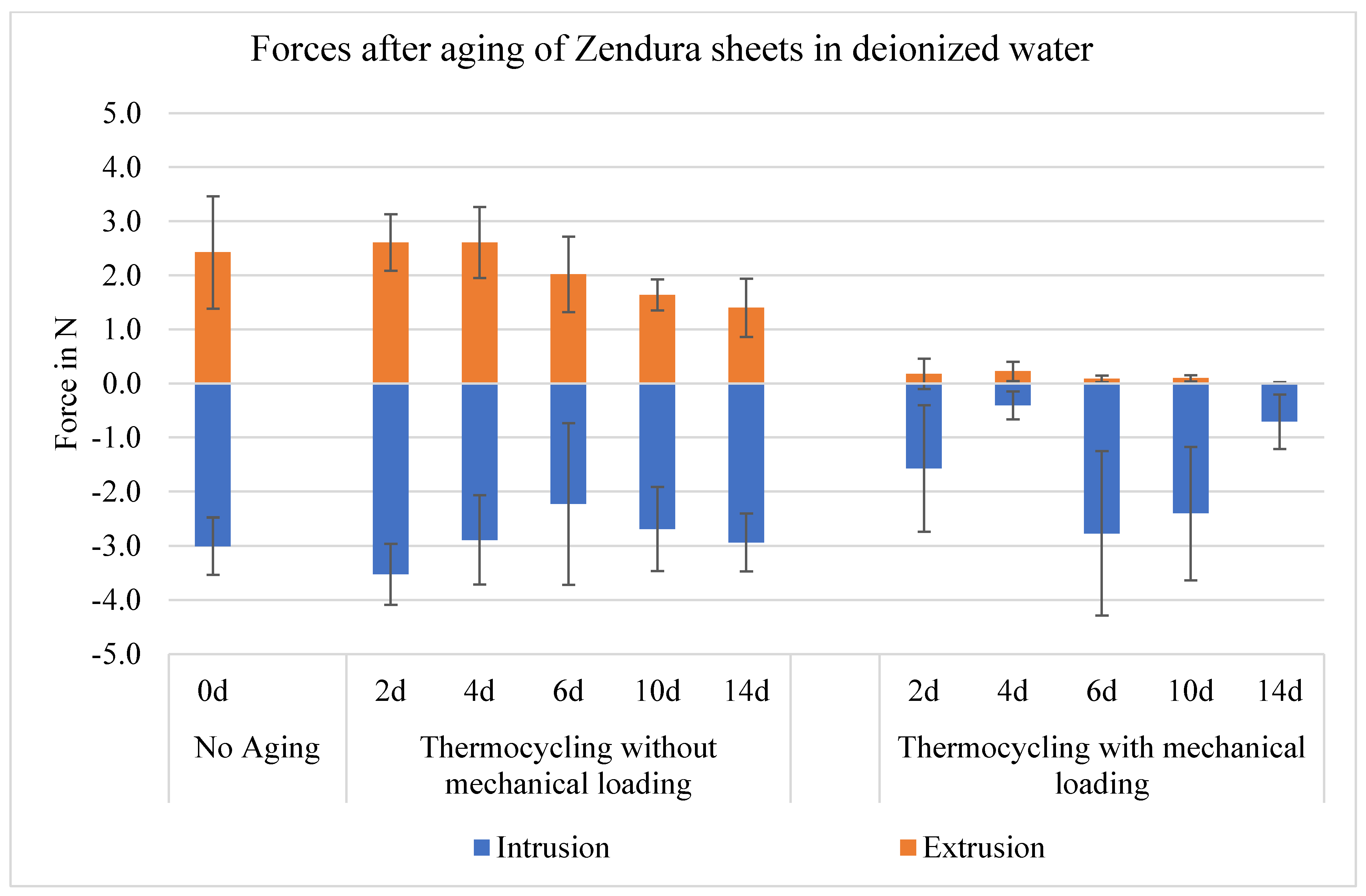
Regarding the vertical forces in the in-/extrusion movement, both groups of aging (without/with mechanical loading) showed an irregular asymmetrical expression of the forces with regard to the direction of movement. Pure thermocycling has no significant effect on force generation in both directions of vertical movement, however, aligners after both thermocycling and mechanical loading showed a significant decrease of force generation. The significant force drop occurred at the first 2 days, with insignificant difference from the force value after 14 days of aging. The mean force with intrusion was 3.0 N before aging, higher than with extrusion, which was 2.4 N. The average reduction in force due to mechanical loading after 14 days of aging was 76 % for intrusion (0.7 N) and 100 % on average for extrusion (0.0 N) (
Table 1 and
Figure 2).
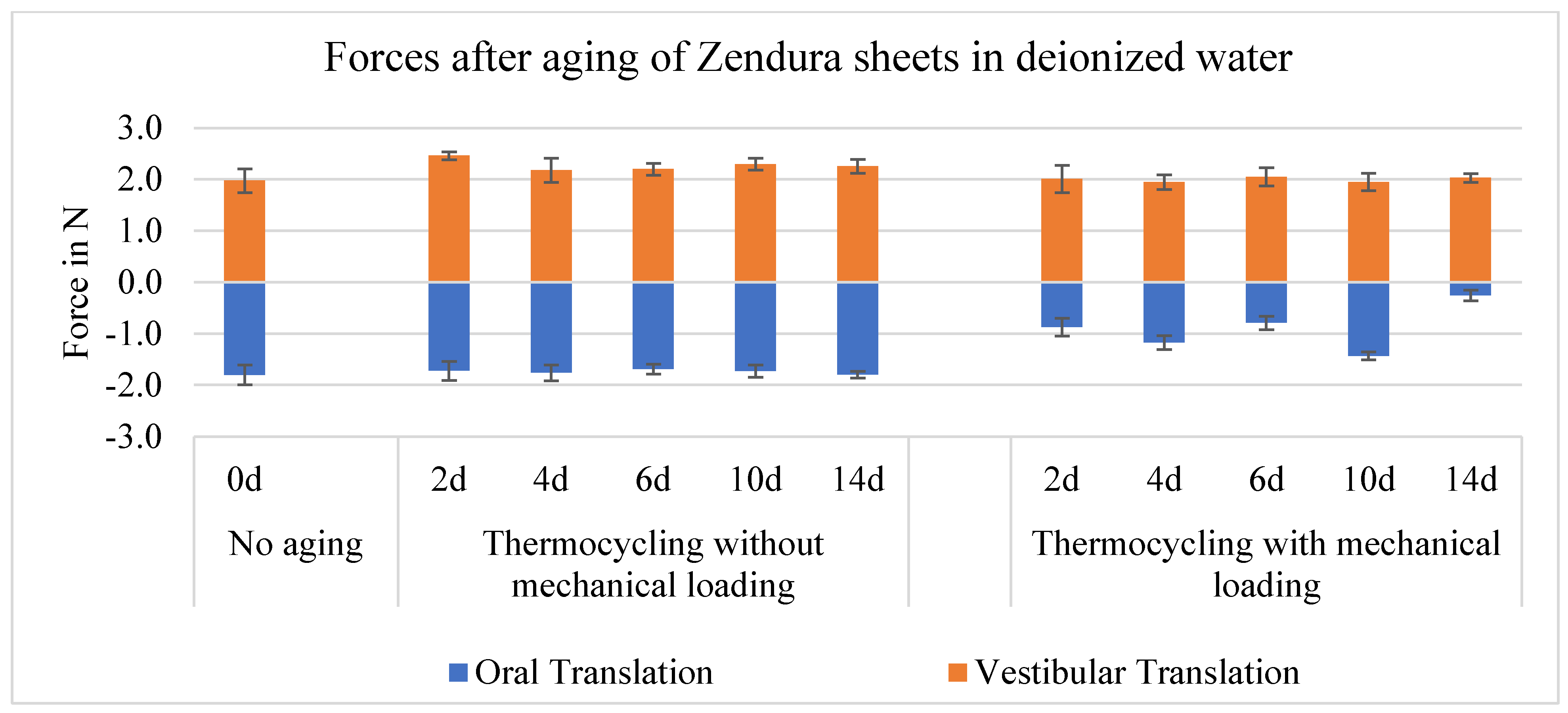
As with the in-/extrusion, the oro-vestibular forces of the aligners (with and without mechanical loading) were asymmetrical with respect to their direction of movement, and no trends with increasing aging can be identified, however, forces are overall less than with the in-/extrusion by about 20-40 %. The mean value of the vestibular force was 2.0 N before aging, higher than the oral force, which was 1.8 N. In oral translation, pure thermocycling has no significant effect, but both thermocycling and mechanical loading resulted in significant force decrease from the first 2 days of aging. Mechanical loading resulted in a 83 % decrease in forces in oral translation after 14 days of aging (0.3 N). Deviating from the trend, in vestibular translation, the force values increased significantly after pure thermocycling, but stayed unchanged after both thermocycling and mechanical loading (
Table 1 and
Figure 3).
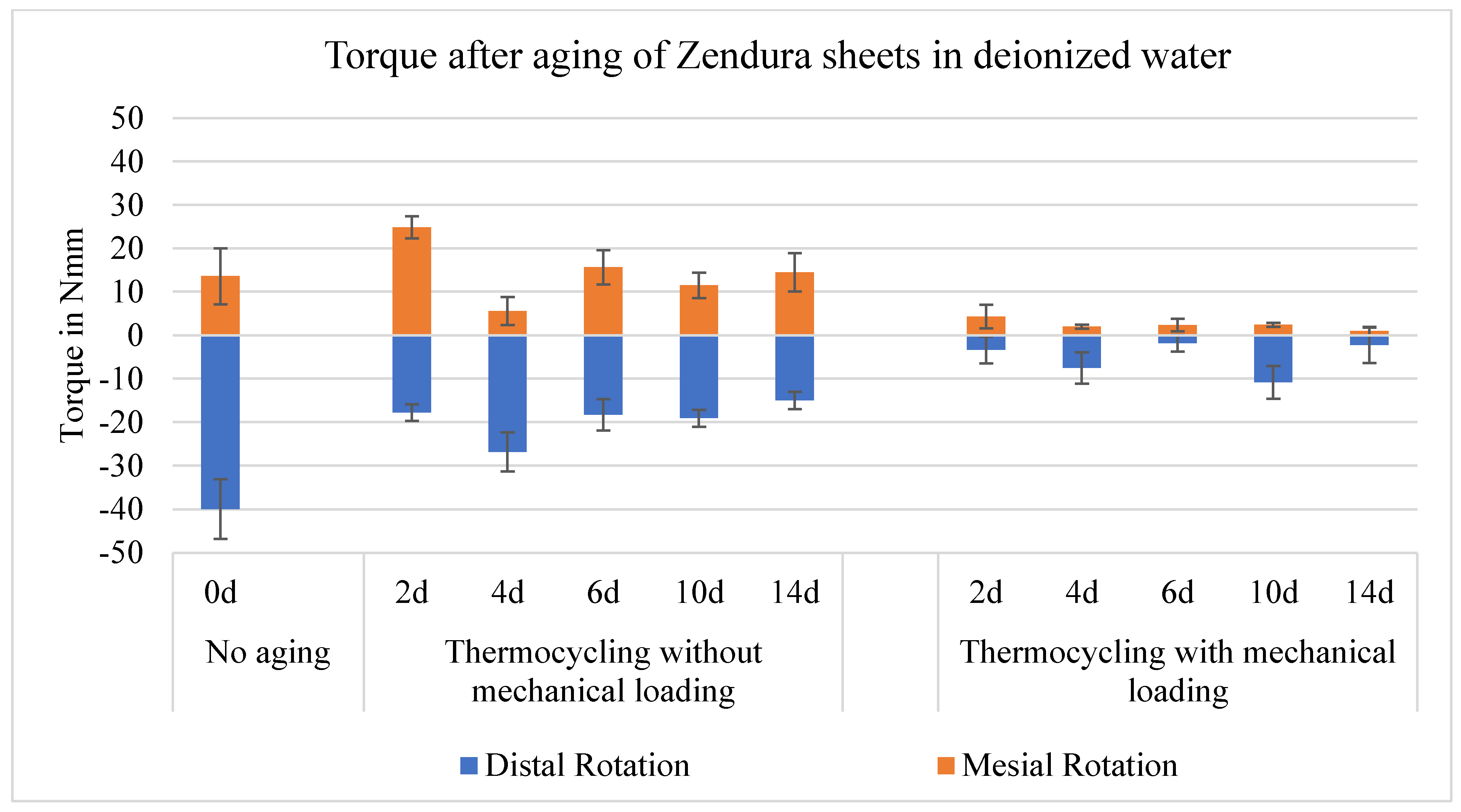
Both the aligners without mechanical loading and those with mechanical loading showed an symmetric development of the torque with respect to the direction of movement. In distal rotation, both the pure thermocycling and the thermocycling with mechanical loading caused a significant drop of the torque generation. While, in mesial rotation, torque decay occurred only after both thermocycling and mechanical loading. Mean values of torque with distal rotation was 40.0 Nmm before aging, higher than with mesial rotation (13.6 Nmm). Aging for 14 days by thermocycling with mechanical loading resulted in a 94 % decrease in torque for distal rotation (2.3 Nmm) and a 93 % decrease for mesial rotation (0.9 Nmm) (
Table 1 and
Figure 4).
Both groups of aging (without/with mechanical loading) showed an irregular asymmetrical expression of the forces and torques with regard to the direction of movement.
Pure thermocycling has no significant effect on force and torque generation, except with the distal rotation.
Mechanical loading has a significant influence on force and torque generation, except with vestibular translation.
Force and torque significant drop occurs at the first 2 days of aging, with no following significant decay in the following days, up to 14 days of aging.
Force and torque generation is direction dependent, where the intrusion force, vestibular force, and distal torque are higher than extrusion force, oral force, and mesial torque, respectively.
Table 1.
Mean values of forces (in N) with in-/extrusion and oro-/vestibular movements and torques (in Nmm) with mesio-/distal rotation generated by aligners made from Zendura™ sheets on tooth 25, after 0 (No aging), 2, and 14 days of artificial aging by thermocycling with and without mechanical loading.
Table 1.
Mean values of forces (in N) with in-/extrusion and oro-/vestibular movements and torques (in Nmm) with mesio-/distal rotation generated by aligners made from Zendura™ sheets on tooth 25, after 0 (No aging), 2, and 14 days of artificial aging by thermocycling with and without mechanical loading.
| |
Intrusion |
p-value |
Extrusion |
p-value |
| Aging |
0 days |
2 days |
14 days |
|
0 days |
2 days |
14 days |
|
| Thermocycling without mechanical loading |
-3.0±0.5a
|
-3.5±0.6 a
|
-2.9±0.5 a
|
0.899 |
2.4±1.0 a
|
2.6±0.5 a
|
1.4±0.5 a
|
0.0898 |
| Thermocycling with mechanical loading |
-3.0±0.5 a
|
-1.6±1.2 b
|
-0.7±0.5 b
|
*<0.05 |
2.4±1.0 a
|
0.2±0.3 b
|
0.0±0.0 b
|
*<0.05 |
| |
Oral translation |
|
Vestibular translation |
|
| Thermocycling without mechanical loading |
-1.8±0.2 a
|
-1.7±0.1 a
|
-1.8±0.1 a
|
0.899 |
2.0±0.2 b
|
2.5±0.2 a
|
2.3±0.1 a
|
*<0.05 |
| Thermocycling with mechanical loading |
-1.8±0.2 a
|
-0.9±0.3 b
|
-0.3±0.1 b
|
*<0.05 |
2.0±0.2 a
|
2.0±0.2 a
|
2.0±0.1 a
|
0.899 |
| |
Distal rotation |
|
Mesial rotation |
|
| Thermocycling without mechanical loading |
-40.0±6.8 a
|
-17.8±1.9 b
|
-15.0±2.0 b
|
*<0.05 |
13.6±6.4 b
|
24.8±2.5 a
|
14.5±4.4 b
|
*<0.05 |
| Thermocycling with mechanical loading |
-40.0±6.8 a
|
-3.4±3.1 b
|
-2.3±4.1 b
|
*<0.05 |
13.6±6.4 a
|
4.3±2.7 b
|
0.9±1.0 b
|
*<0.05 |
Figure 2.
Change in the mean value of intrusive/extrusive forces generated by aligners made from Zendura™ sheets on tooth 25, after 0 (without thermocycling and mechanical loading), 2, 4, 6, 10 and 14 days, which corresponds to the abbreviations 0d, 2d, 4d, 6d, 10d and 14d in the diagrams.
Figure 2.
Change in the mean value of intrusive/extrusive forces generated by aligners made from Zendura™ sheets on tooth 25, after 0 (without thermocycling and mechanical loading), 2, 4, 6, 10 and 14 days, which corresponds to the abbreviations 0d, 2d, 4d, 6d, 10d and 14d in the diagrams.
Figure 3.
Change in mean oro-vestibular forces generated by aligners made from Zendura™ sheets on Tooth 25, after 0 (without thermocycling and mechanical loading), 2, 4, 6, 10 and 14 days, which corresponds to the abbreviations 0d, 2d, 4d, 6d, 10d and 14d in the diagrams.
Figure 3.
Change in mean oro-vestibular forces generated by aligners made from Zendura™ sheets on Tooth 25, after 0 (without thermocycling and mechanical loading), 2, 4, 6, 10 and 14 days, which corresponds to the abbreviations 0d, 2d, 4d, 6d, 10d and 14d in the diagrams.
Figure 4.
Change in the mean value of the torque generated by aligners made from Zendura™ sheets when tooth 25 rotates around tooth axis, after 0 (without thermocycling and mechanical loading), 2, 4, 6, 10 and 14 days, which corresponds to the abbreviations 0d, 2d, 4d, 6d, 10d and 14d in the diagrams.
Figure 4.
Change in the mean value of the torque generated by aligners made from Zendura™ sheets when tooth 25 rotates around tooth axis, after 0 (without thermocycling and mechanical loading), 2, 4, 6, 10 and 14 days, which corresponds to the abbreviations 0d, 2d, 4d, 6d, 10d and 14d in the diagrams.
5. Discussion
As an orthodontic appliance used for tooth movement, aligners should basically have the property of exerting continuous forces over time [4, 16, 25]. However, they are exposed
in vivo to various mechanical and thermal stresses that can impact their physical properties and effectiveness [
21]. Mechanical stresses include the brief insertion and removal of the aligner, as well as prolonged contact with teeth [
15]. Additionally, factors such as water absorption and temperature changes in the oral cavity can also affect the mechanical properties of aligners [
34]. In the current study, the impact of simulated aging on the force and torque levels of orthodontic aligners made from Zendura™ thermoplastic polyurethane (TPU) sheets was investigated. The aging simulation was done either through pure thermocycling, or through combined thermocycling and mechanical loading caused by a pre-designed 0.2 mm vestibular translation of the targeted tooth.
Thermocycling is a method of simulating aging by repeatedly exposing test specimens to alternating temperatures of water storage, which can cause changes in the material [
11]. When plastic is stored in water, water molecules can diffuse into the plastic and move between the polymer chains, increasing their mobility. Additionally, as the temperature increases, the mobility of the polymer molecules also increases, leading to changes in the material [11, 27, 35–37]. To simulate a more clinically relevant situation, artificial saliva could be used, but since the thermocycling device does not allow its use, deionized water was used instead. Nevertheless, recent studies [11, 21] have reported no significant difference in the forces and torques of aligners stored in distilled water versus those stored in artificial saliva.
Not only the aligners exert forces on the teeth, but also the teeth deliver forces to the aligners resulting in mechanical loading and deformation of the aligner. Clinically, the forces acting on the aligner from teeth decrease over time due to the periodontal remodeling processes. However, in vitro the PDL is absent, thus the mechanical load caused by the resin model remains constant during testing. The results in the current experiment provide an indication that the mechanical loading of aligners has a greater influence on their mechanical properties, however pure thermal loading has no significant effect. Furthermore, the greatest force decay already occurred within the first two days and thus the results of all further aging days no longer differ significantly from each other, in agreement with previous studies [11, 21].
The reasons could be that TPU has viscoelastic property and its glass transition temperature (Tg) was reported in the range of 80 °C [
13], well above the oral temperature and the used thermocycling temperature range. These kind of materials have intermediate properties between viscous and elastic materials. Their mechanical performance begin to decay due to creep and stress relaxation. Creep means that when the aligner splint is mechanically loaded repeatedly below the yield point, it is permanently deformed over time. Stress relaxation is the gradual reduction of force exerted by a material in response to a constant deflection [15, 19]. Too, repeated mechanical loading of materials leads to material fatigue and the formation of micro-cracks, which facilitate water leakage into the polymer structure and weakens material strength. On the contrary, mechanical properties are unlikely to change during pure thermocycling under the Tg temperature [
13].
Optimal orthodontic strength varies individually and per tooth, but it should provide maximum movement with the least possible biological damage and the greatest patient comfort [
38]. However, it was reported [
39] that the magnitude of the orthodontic force stays less important as long as the tooth deflection distance is less than or equal to the width of the periodontal ligament (PDL) gap (0.1 - 0.3 mm), since this would not stop capillary blood flow. In addition, the tooth moves away over time in response to the forces applied to it by the aligner, together with the periodontal remodeling processes, which reduce the initial force applied to the tooth accordingly, even if the deflection distance is high.
Proffit [
40] gave approximate recommendations with force specifications for various tooth movements. His recommendations of 0.1 - 0.2 N for intrusion and 0.7 - 1.2 N for translation is for at least four to eight hours constant force per day [
40]. The literature does not offer any clear guidelines with regard to the torque, but one could set the values mentioned in relation to the root surface in order to get an indication of the appropriate torque for the maxillary second premolar. Torque of 30 Nmm [
41] referred to a molar with an average root surface of about 430 mm
2 [
42]. Tooth 25 has a root surface of 220 mm
2 [
42], thus the appropriate torque is 10.5 - 15.8 Nmm, as reported by Sander et al. [
43].
In the current study, mean force values are up to 3.0 N and mean torque values are up to 40.0 Nmm, well above the values reported in the literature. That could be referred to the rigidity of the used mechanical testing system (OMSS) and the absence of the PDL. Besides, OMSS is based on the assumption of a linear relationship between the speed of tooth movement and the amount of applied force, which does not truly simulate the biomechanical behavior of the PDL. Furthermore, a virtual ideal center of resistance was set for the measured tooth [
16].
Nevertheless, Hahn et al. [9, 10] reported,
in vitro using similar 3D force-torque sensor, the oro-vestibular forces at a 0.15 mm deflection of a maxillary central incisor. The horizontal forces were in the range of 2.7 N (oral) – 3.1 N (vestibular). With respect to the type of tooth measured and the magnitude of the deflection, the force measurements in the present study can be considered similar in magnitude. Likewise, Elkholy et al. found that 0.5 mm thick aligners exerted a torque of 73.6 Nmm during a 10° mesial rotation of a maxillary central incisor [
44]. While, the average torque for 0.75 mm thick aligners during a 15° distal rotation of a mandibular canine was 42.5 Nmm [
45]. In the current study, torque values without aging ranged from 13.6 Nmm (mesial rotation) to 40.0 Nmm (distal rotation) for an upper second premolar rotation of only 2°.
As well, Barbagallo et al. [
46] reported, using pressure-sensitive polyester films
in vivo, mean force of 5.1 N on upper first premolar by 0.8 mm thick aligners. Their values clearly exceed Proffit's recommendations. In the current study, a maximum mean force of 2.0 N (60 % of Barbagallo’s value) was measured for vestibular translation. However, considering that the maximum deflection distance of 0.2 mm used in this work is only 40 % of the deflection distance reported by Barbagallo et al. (0.5 mm), the values of the present work are in line with those of Barbagallo et al.
In line with the current results, Kwon et al. [
25] reported that mechanical loading has a greater influence on the forces generated by aligners than pure thermocycling. At a 3-point deflection distance of 0.2 mm of the unaged aligner sheets, the measured force was 0.5 N. After pure thermocycling, the force was the same, while after mechanical loading, the value was 0.65 N. In the current study, although force values are up to six times higher, the specimen’s shape may be reason behind that. Kwon et al. used a flat, rectangular specimen, while in our work the sheets were deep-drawn over anatomical tooth models with larger curvatures, which may increase the stiffness and thus the force acting on the tooth [10, 11, 13, 45].
According to various studies, the amount of stress relaxation and decay of generated forces in aligner materials differs based on their composition, with values ranging from 15-44 % [
15]. One study [
19] found that 34-58 % of generated forces decayed after 3 hours of testing, while another [
45] reported a loss of 44-76 % of initial forces after 24 hours of testing different standardized stone blocks made from different aligner materials with varying geometries.
Li et al. [
13] used the dynamic mechanical analysis test to quantify stress relaxation of raw materials and thermoformed aligners have different compositions. They reported 51.2 % stress relaxation rate of TPU. However, these study results have limited clinical applicability because they did not assess aligners utilized in actual clinical settings, since the shape and characteristics of teeth can significantly affect the thickness and mechanical properties of the aligner materials, it is critical to measure the stress relaxation of real aligners to determine the remaining force that contributes to tooth movement [
13]. In our study, forces generated by thermoformed aligners were tested in 3D. The force decay rate was the most after the first two days of aging and further aging days no longer differ significantly from each other. The force/torque decay after 14 days reached 76 % with intrusion, 100 % with extrusion, 83 % with oral translation, and 96 % with rotation.
Similar to the current study, Engelke et al. [
22] studied the force and torque output of aligners on upper central incisor after artificial aging including thermocycling and mechanical loading. They reported a statistically significant reduction in intrusive forces and rotational torques after aging. Too, Elshazly and Nang [
11] reported the force/torque generation on tooth 25 by Essix ACE
® thermoplastic aligners after pure aging in deionized water and in artificial saliva over two weeks at 37 °C. Their results showed that pure thermal loading of aligners has no significant effect on force and torque decay, compatible with the current study.
The current experimental mechanical testing has some limitations, on top of them is the absence of the PDL. Furthermore, it reported only on the force system of one thermoplastic polyurethane material (Zendura), hence further investigation of different materials is proposed to be done. Moreover, the mechanical influences from the opposing dentition in the form of mastication, which occurs intraorally [
23], were not considered. Also, the forces generated by swallowing processes [
40] were not simulated. Although previous studies [11, 21] showed no significant effect of using artificial saliva in place of deionized water during experimental testing of aligners, serious changes in polymeric structures and mechanical properties of the aligner may resulted from the change in pH of oral cavity and the interactions with enzymes, ions, bacterial byproducts, as well as ingested components.
6. Conclusion
Studying the forces/torques generated by orthodontic aligners made of polyurethane thermoplastic materials showed a significant decrease after combined artificial aging by thermocycling and mechanical loading at the first 2 days of aging, with no significant decay in the following days, up to 14 days of aging. Moreover, the mechanical loading of aligners has a greater influence on their mechanical properties than pure thermocycling. In addition, force and torque generation is direction dependent, where with the studied tooth (Tooth 25), the intrusion force, vestibular force, and distal torque were higher than extrusion force, oral force, and mesial torque, respectively.
Authors Contributions: Conceptualization: CB, Data curation and Analysis, Investigation, and Methodology: TE, DN, BG, LK, Resources: CB, Software: Supervision, Validation and Visualization: TE, CB, LK, Writing—original draft: TE, DN, Writing—review & editing: TE, DN, HE, CB. All authors have read and agreed to the published version of the manuscript.