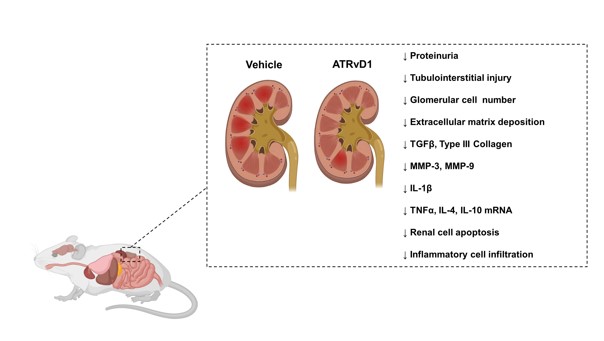
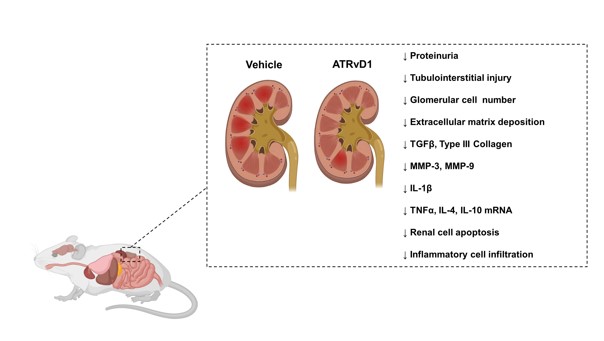
Current interventions are not effectives in preventing sepsis-induced acute kidney injury and its long-term outcomes or even after second renal insult. Therapeutic strategies using lipid mediators, as aspirin-triggered resolvin D1 (ATRvD1), can contribute for resolution of acute and chronic inflammation. In this study, we examined the potential effect of ATRvD1 on long-term kidney dysfunction after severe sepsis. Fifteen days after cecal ligation and puncture (CLP), sepsis-surviving BALB/c mice were subjected to a tubulointerstitial injury through intraperitoneal injections of bovine serum albumin (BSA) for 7 days, called subclinical acute kidney injury (subAKI) animal model. ATRvD1 treatment was performed right before BSA injections. On day 22 after CLP, urinary protein/creatinine ratio (UPC), histologic parameters, fibrosis, cellular infiltration, apoptosis, inflammatory markers levels, and mRNA expression were determined. ATRvD1 treatment mitigated tubulointerstitial injury by reducing the proteinuria excretion, UPC ratio, glomerular cell number and extracellular matrix deposition. Pro-fibrotic markers, as transforming growth factor β (TGFb), type 3 collagen and metalloproteinase (MMP)-3 and -9 were reduced after ATRvD1 administration. Post-septic mice treated with ATRvD1 were protected from renal apoptosis and recruitment of F4/80+ cells. Interleukin-1b (IL-1b) levels were increased in subAKI animal model, being attenuated by ATRvD1. Tumor necrosis factor-a (TNF-a), IL-10 and IL-4 mRNA expression was increased in the kidney of BSA-challenged post-septic mice and it was also reduced after ATRvD1. These results suggest that ATRvD1 protects the kidney against a second insult as BSA-induced tubulointerstitial injury and fibrosis by suppressing inflammatory and pro-fibrotic mediators in renal dysfunction after sepsis.