1. Introduction
The endoscopic endonasal transsphenoidal surgery is nowadays the standard technique used to approach sellar and parasellar tumors, providing better visualization and improved extent of tumor resection [
1,
2,
3,
4]. The two nostrils/four hands technique was introduced to improve the maneuverability of surgical instruments and to increase the accessibility of the anterior skull base, especially in cases of expanded endoscopic endonasal approaches; at this proposal, the nasoseptal flap concept was developed in order to reduce the risk of cerebrospinal fluid (CSF) leakage [
5,
6]. Since endoscopic endonasal approach (EEA) is a well-established technique with a low rate of complications, the focus has recently shifted to nasal function preservation; nevertheless, EEA inevitably damages the nasal cavities with possible complications such as hyposmia or synechiae, which are often associated with discomfort and reduced quality of life [
7]. To improve sinonasal morbidity, the endoscopic transsphenoidal approach keeps evolving by borrowing the advantages of other and older surgical approaches, such as the microscopic transseptal surgery, which reaches the sellar area through the mono-nostril submucosal transseptal corridor [
8]. Inspired by this approach, which was once the “gold standard”, several modified endoscopic transseptal or mononostril endoscopic endonasal approaches have been described, and many groups have reported promising functional results. However, these modified techniques, although less traumatic than the classic EEA, still require partial o total bilateral submucoperichondrial and sub-mucoperiosteal dissection or violation of a single nostril via the endoscopic endonasal route. Furthermore, it was questioned if the benefit of endoscopic endonasal transseptal approaches in preserving nasal mucosa or mononostril endoscopic endonasal technique could be at the sacrifice of neurosurgical outcomes for their limited surgical exposure and maneuverability [9−15]. Therefore, taking inspiration from the various surgical techniques proposed in the literature, the aim of this study is to describe our experience regarding a single nostril transseptal endoscopic approach, performed in selected cases of pituitary macroadenoma, with complete preservation of the nasal mucosa and turbinates. This study presents the results of this technique applied on a cohort of selected patients with an analysis of the safety and the effectiveness on the quality of resection, considering also the sinonasal morbidity.
2. Materials and Methods
A total of 40 patients, with a midline prevalent pituitary tumor, who underwent EONOTTA from January 2022 to June 2023 were retrospectively reviewed for the evaluation of safety and efficacy of this technique: both secreting and non-secreting pituitary macroadenomas were included. Neuroimaging inclusion criteria, assessed with MRI-pituitary protocol and CT scan, were midline seated lesions, minimal cavernous sinus invasion (Knosp grade 1–2) or absence of kissing carotids and exclusion criteria were recurring adenomas previously operated, any kind of previous sinonasal surgery, massive, cavernous sinus invasion (Knosp grade 3–4) or the need of expanded endoscopic approaches. Clinical data such as age, sex, smoking habits or possible cocaine abuse, dimension of tumor, any abnormalities in hormonal tests, degree of tumor removal, postoperative complications and quality of life including sinonasal morbidity were collected. Surgical technical details were analyzed including type of surgical intervention, duration of surgery, intraoperative complications, intraoperative hematic losses, intraoperative and postoperative cerebrospinal fluid leak rate, and surgical material used for the reconstruction; the overall presence of post-operative endocrinological complication (e.g., diabetes insipidus) was followed. Head CT scan was also always performed on Day 1 to detect any intracranial bleeding or pneumencephalus together with an MRI study before discharge to verify the degree of tumor removal; an endoscopic check-up and endocrinological consultation were performed as well. All patients underwent a follow-up at 1, 3, 6 and 12 months, also evaluating the quality of life in relation to any sino-nasal disorders. Subsequently, a comparison was carried out with a previously studied series (similar in terms of sample size and clinical-radiological characteristics) treated with a classic EEA technique.
3. Results
A total of 40 patients, with a midline prevalent sellar tumor, who underwent endoscopic trans-septal trans-sphenoidal pituitary surgery from January 2022 to June 2023 were reviewed for evaluation of the safety and efficacy of this approach. The surgical corridor was along the entire length of the nasal septum and a zero-degree endoscope was used since the initial phases of the procedure.
At follow-up, after 1 year no recurrences, no CSF leaks and no nasal mucosa scarring related to the approach were registered. The degree of tumor resection was comparable to the control group undergoing the traditional endoscopic endonasal approach and a low rate of nasal complications occured: 1 septal perforation and 1 mucosal dehiscence.
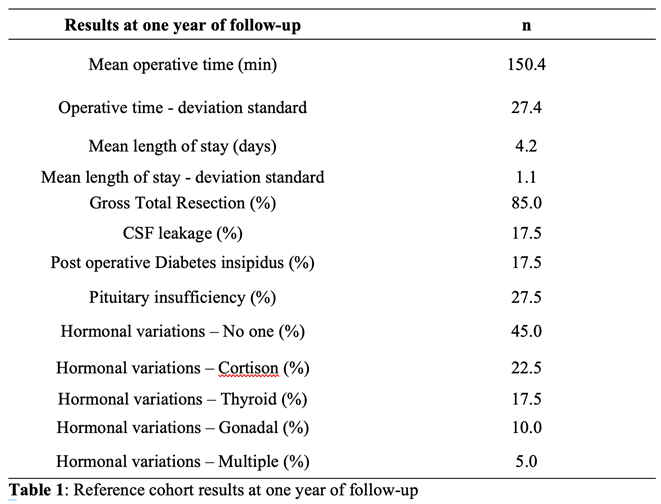
The low rate of postoperative nasal morbidity was also confirmed by the single case of post-procedural synechia; although the occurrence of a longer operating time in the first cases, globally the EONOTTA transeptal approach did not result in a time-consuming technique and a better cosmetic result was noticed at follow-up. Results are summarized in Table 1.
The mean operative time in these series was 150,4 min and the mean length of stay in the hospital was 4,2 days. The gross total resection (GTR) was achieved in 85% patients. Hormonal remission, determined by repeated post-operative serum hormone detection, was achieved in 75% at the last follow-up. In regard to the surgical complications, the intraoperative CSF leakage was encountered in 17,5% patients. Other postoperative complications included diabetes insipidus in 17,5% cases and anterior pituitary insufficiency (taking hormone replacement therapy) in 27,5% cases. No ICA Injury or death happened in this series. More than half of the patients (52.3%, 67/128) suffered from decreased visual acuity and visual field defects before surgery. Most of the patients (82.1%, 55/67) improved visual status and no patient presented a worsened visual status.
The main sinonasal complaints at 2 weeks after surgery were: headache (15.6%), nasal discharge (11.7%), trouble breathing (10.2%), hyposmia (7.8%), nasal synechia (2.3%) and epistaxis (0.8%). One month after surgery, most symptoms disappeared and were relieved with 4.7% of patients complaining about nasal discharge, followed by hyposmia (3.9%), trouble breathing (3.1%), and headache (2.3%). At 3 months of follow-up, nearly all these nasal symptoms disappeared. (Table 3) As for the sinonasal quality of life assessed by the ASK nasal- 12, the scores increased two weeks after surgery and significantly decreased 1 month after surgery. Three months after surgery, the scores returned to the baseline. The Lund-Kennedy score showed that after one month, the nasal cavity of patients who underwent EOTA had recovered to the baseline. The odor identification test also showed that the patients had the same olfactory performance as the baseline one month after surgery.
The study showed that, compared to the control group, where the surgical approach was traditional endoscopic endonasal, the operating times were progressively reduced with the surgeon's increasing experience in performing the EONOTTA approach, reaching a comparable gross total resection value, with less destruction of the nasal mucosa and a lower incidence of complications such as cerebrospinal fluid fistula and anatomical-functional nasal-sinus preservation, as evidenced by endoscopic and follow-up checks.
Clinical Case
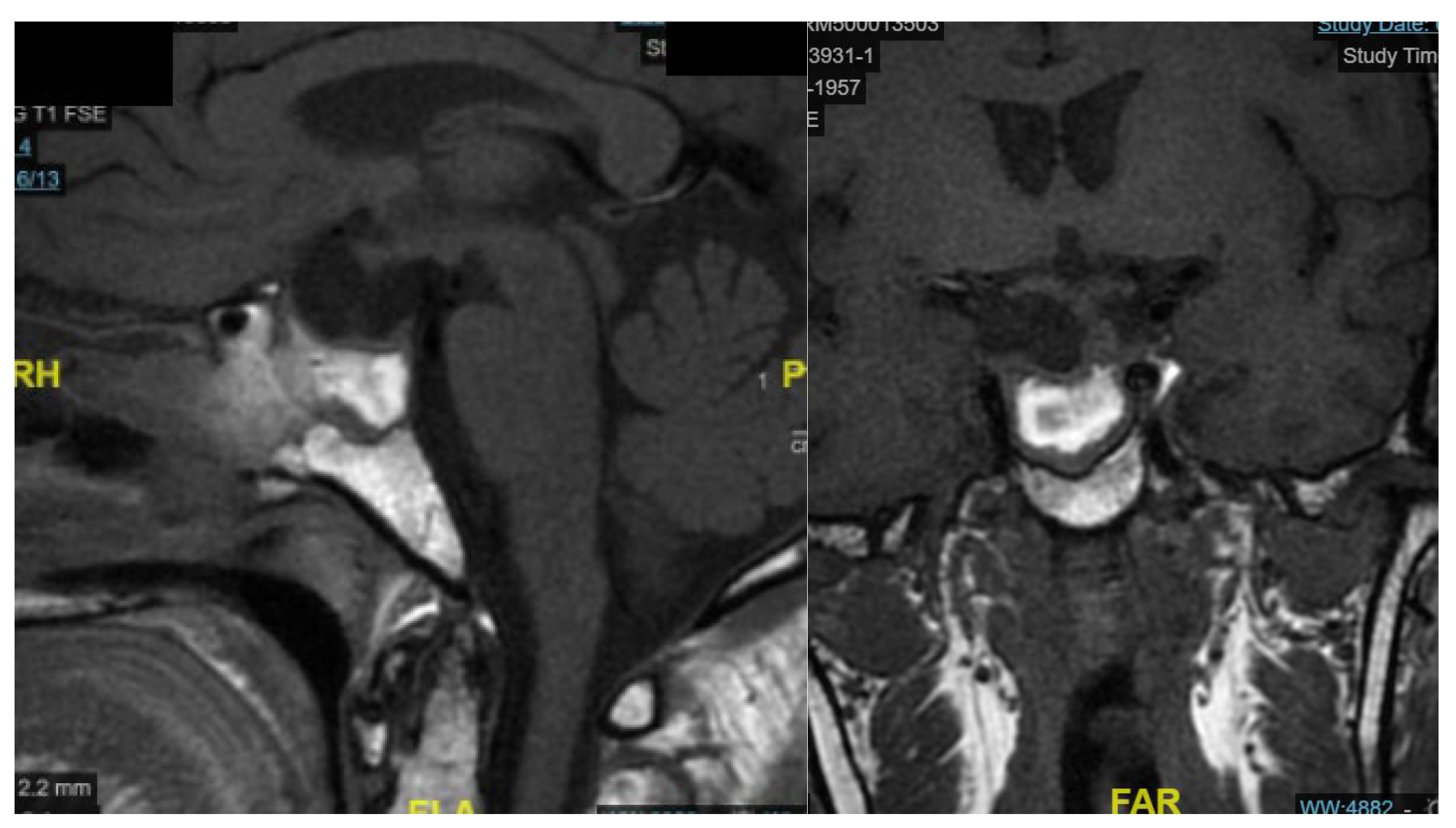
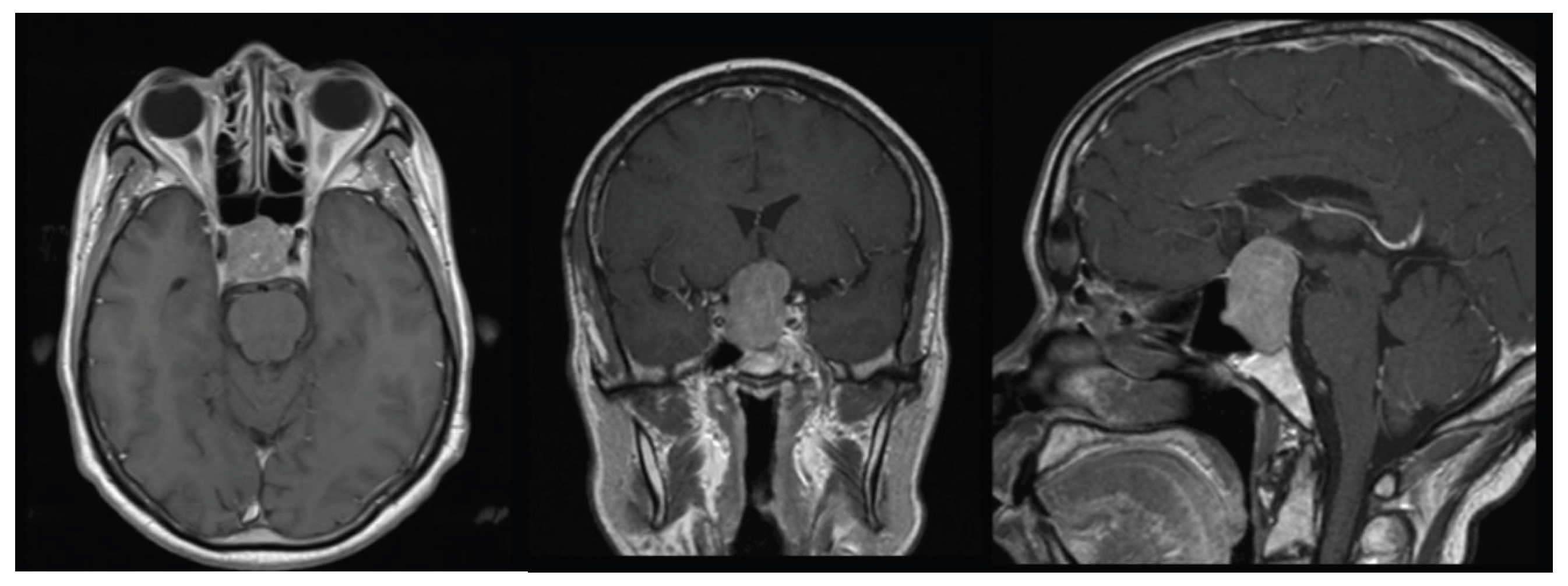
A 58-year-old woman presented with severe hyponatremia, headache, and bitemporal hemianopsia. As shown in
Figure 1, preoperative MRI revealed midline pituitary macroadenoma extending suprasellarly, compressing the optic chiasm and not invading cavernous sinuous.
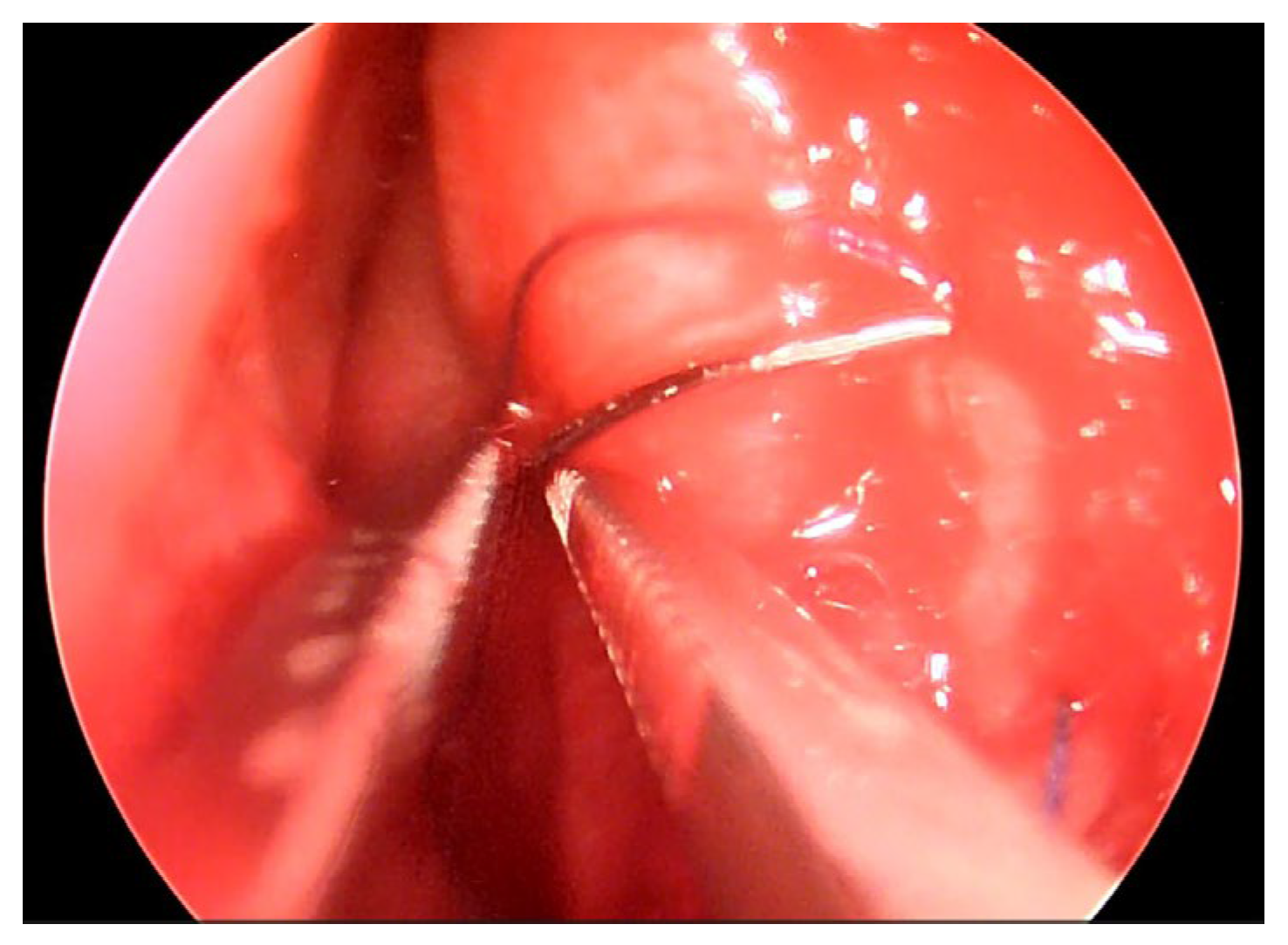
The patient underwent an Endoscopic One Nostril Transseptal Transsphenoidal Approach (EONOTTA) for tumor removal. In
Figure 2 is shown the right mono-nostril approach and the septal mucosal incision with the initial submucosal dissection along the septum.
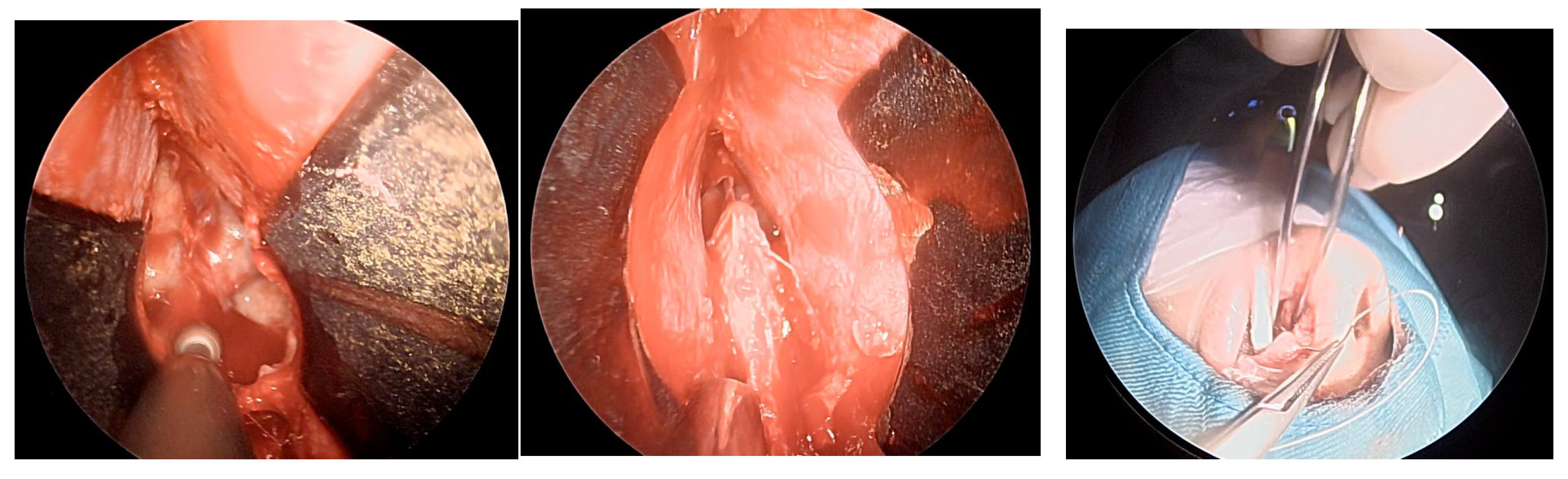
Once the mucosal dissection is completed, self-retaining nasal speculum is placed between the mucosal flap and the cartilaginous nasal septum obtaining sphenoidal exposure (
Figure 3).
After removal of the adenoma and placement of autologous adipose tissue, as shown in
Figure 4 unilateral mucosal reconstruction is performed by placing a simple interrupted suture thought mucosal flap and cartilaginous septum.
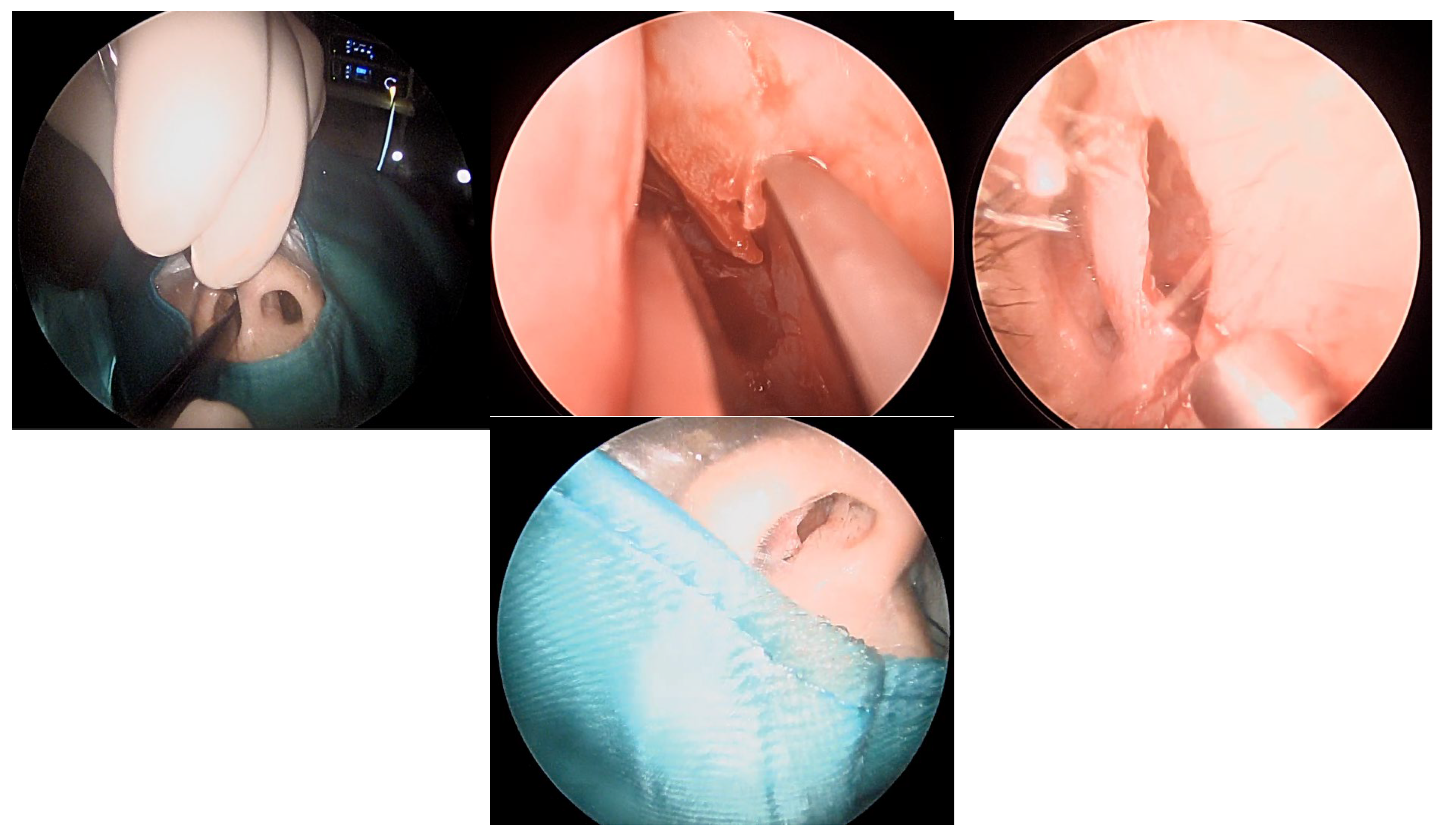
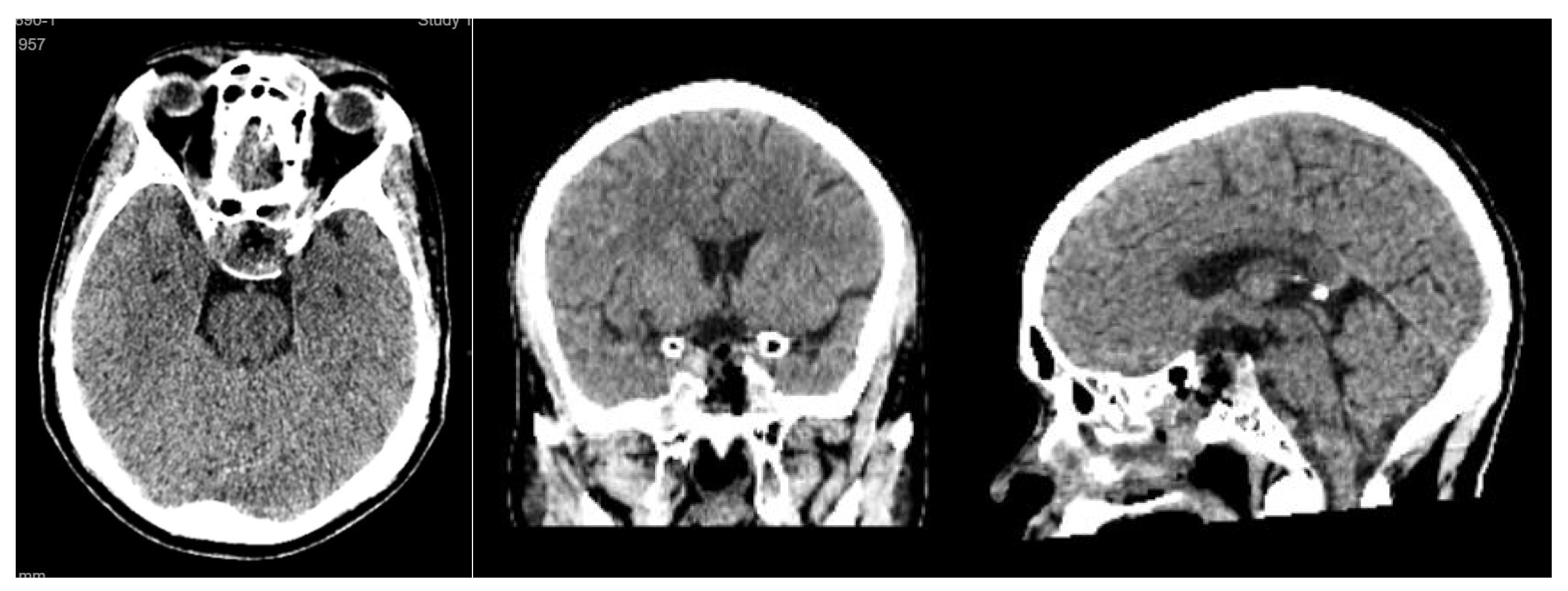
Postoperative imaging demonstrated near-total resection of the lesion with decompression of the optic apparatus and restoration of normal sellar anatomy (
Figure 5).
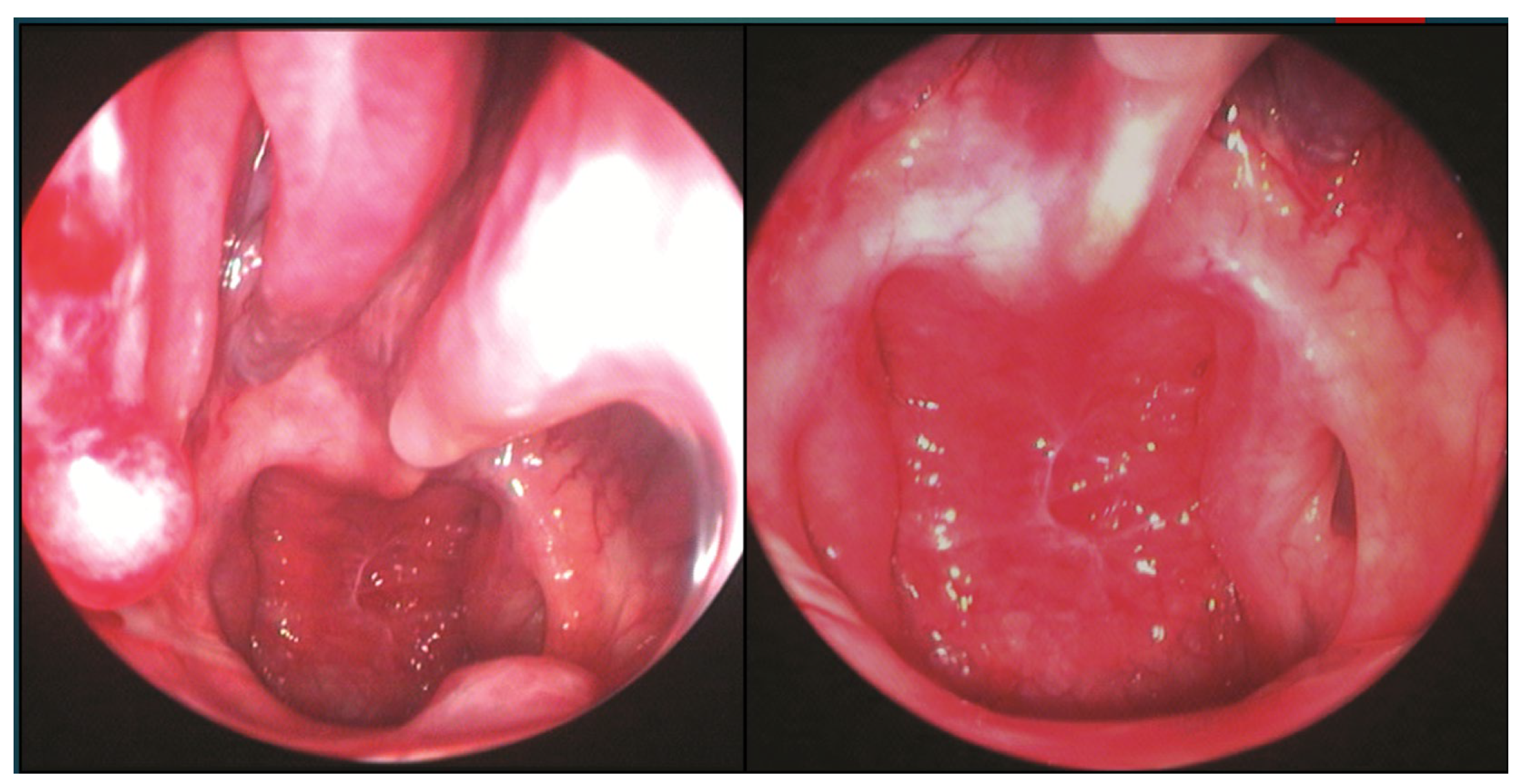
The patient underwent endoscopic ENT follow-up 4 days after the operation and 30 days later (
Figure 6).
The patient showed significant clinical improvement, with resolution of visual symptoms and normalization of serum sodium levels. No postoperative cerebrospinal fluid leakage, nasal crusting, or olfactory dysfunction was observed. The MRI examination performed one month later shows packing material with no radiological evidence of residual lesion.
Figure 7.
sagittal and coronal MRI one month after surgery.
Figure 7.
sagittal and coronal MRI one month after surgery.
The EONOTTA approach proved effective in achieving optimal tumor control and functional recovery while minimizing sinonasal morbidity. This case highlights the value of the transseptal endoscopic technique in selected pituitary macroadenomas without major lateral extension, ensuring both surgical efficacy and improved postoperative quality of life.
4. Discussion
Pituitary adenomas are benign clonal neuroendocrine tumors deriving from adenohypophysial cells, which are nowadays referred to as pituitary neuroendocrine tumor (Pit-NET) [
16]. Halstead, in 1910 followed by Harvey Cushing were the first to describe pituitary surgery via a sublabial transseptal approach. In 1961, Gérard Guiot after performing resection with an operating microscope, was the first to introduce the endoscope to control tumor resection, limited by the optical quality of the endoscopes available at the time. Roger Jankowski in 1992, performed the first entirely endoscopic endonasal procedure and today most endoscopic surgical procedures are now performed according to this technique [
17]. In literature, many endoscopic techniques to approach sellar lesions are reported, but they can be overall summarized in two categories; the classic EEA performed in both or single nostrils or transseptal techniques that involve both sides of the septal mucosa. Therefore, either the nasal cavity is violated mono or bilaterally or the septal mucosa is violated bilaterally. In this article, we would like to propose the endoscopic one nostril transseptal transphenoidal approach, that we have applied in selected cases of pituitary macroadenoma and have observed to be effective in controlling the disease with minimally invasiveness for the sinonasal structures. The introduction of this technique into our clinical practice, which is nothing more than a revisitation of the old microscopic transseptal approach, arises from the idea that, in selected mid-line cases, when there is no need to perform an extended endoscopic approach, a unilateral transseptal surgical corridor is sufficient to gain a good exposure of the disease and a comfortable working angle. This allowed two surgeons always working together at the same time, thus addressing the removal of the tumor as in the classic EEA, with less morbidity affecting the nasal structures and often without the need for pedunculated flaps, as repositioning the vascularized mucosa of the septum unilaterally acts as a flap itself [19−20]. In some cases of large CSF fistulas, the classic pedunculated nasoseptal flap may still be necessary for skull base reconstruction but harvesting of this vascularized flap involves cutting the mucosa and is associated with an increased risk of postoperative nasal crusting, raising concern about worsening postoperative sinonasal quality of life. The EONOTTA presents numerous advantages regarding sinonasal anatomy, as it is a strictly midline approach avoiding the constraints related to possible turbinate hypertrophy or a deviated septum. The dissection in the avascular subperichondrial/subperiosteal plane is generally associated with minimal bleeding, decreases the risk of the posterior nasal artery injury and preserving of the middle and superior turbinates also theoretically decreases the risk of post-operative epistaxis and anosmia. It also allows the use of the nasoseptal flaps which can be used in the same procedure, or later if a revision surgery is needed
21. Functional complications related to the transseptal approach are rare and endonasal anatomy is globally preserved in most cases. Although initially more time-consuming than classic EEA, the transseptal approach is nevertheless familiar for ENT surgeons due to the similarities with conventional septoplasty techniques. Endoscopic trasnseptal technique was introduced therefore with the aim of reducing sinonasal morbidity and improving sinonasal quality of life, but the speculum restricts the bimanual handling of instruments, and therefore it would be suboptimal in cases of tumors with significant lateral extension and in all those patients who require an extended endoscopic approach [22−24]. Our study revealed that the patients who underwent EONOTTA had less postoperative pain, better nasal outcomes with intact olfactory function than the standard endoscopic transnasal approaches and a degree of disease control comparable to the latter surgical technique. Therefore, in our preliminary experience, EONOTTA can be deemed a favorable technique that combines, in selected cases, the advantages of both approaches: comparable neurosurgical outcomes from the endoscopic transnasal approach and minimal nasal morbidities from the microscopic transseptal approach. Even though this transseptal approach seems attractive, we should still remember that every procedure has its limits: dissection of the septal mucosal flap could be difficult in patients with previous nasal surgery, including septoplasty/rhinoplasty, and tumors with more lateral extension may not be removed thoroughly. Furthermore, it is very difficult in our experience to try to define and quantify the relative contribution of postoperative nasal symptoms to overall quality life. Obviously, the perception of nasal disturbance is difficult to ascertain because it impacts the quality of life differently, also depending on the expectations and what the patient deals within his working life. This transseptal surgical technique clearly benefits from a multidisciplinary team composed of neurosurgeon and ENT surgeon; the latter is essential to perform the rhinologic phases, avoiding mucosal lesion or septal perforation during the first stages of the approach, and to prevent time consumption.
Several limitations in this work have been encountered: firstly, the study was retrospective in nature and included a small-size sample; results still require validation with randomized-controlled studies. Histologically, only pituitary adenoma were treated with the transeptal technique and whether the conclusions can be generalized to other sellar pathologies remains unexplored. Finally, we only analyzed data until 1 year after surgery. Long-term complications, especially septal complications, require a longer follow-up.
The EONOTTA is, in our opinion, a safe and minimally invasive approach to address pituitary macroadenomas without major lateral extension, that enables a nice exposure of the intrasphenoidal anatomical landmarks with maximal preservation of the nasal mucosa and better nasal recovery than classic endoscopic endonasal approaches. This approach enables intrasellar working without major drawbacks with a two-hand to three-hand technique. It might be considered as an alternative surgical technique for pituitary adenoma under selected circumstances. The results of this study confirm the safety and the efficiency of this approach for non-extended pituitary surgery.
5. Conclusions
According to our experience, this study confirms the excellent risk-benefit ratio supporting the use of trans-sphenoidal endoscopic transseptal approach in selected cases: this working corridor for pituitary surgery was found to be easy for an experienced multidisciplinary team providing good maneuverability and an effective approach with a minimal rate of post-operative complications.
References
- Li, A.; Liu, W.; Cao, P.; Zheng, Y.; Bu, Z.; Zhou, T. Endoscopic Versus Microscopic Transsphenoidal Surgery in the Treatment of Pituitary Adenoma: A Systematic Review and Meta-Analysis. World Neurosurg. 2017, 101, 236–246. [Google Scholar] [CrossRef]
- Roethlisberger, M.; Jayapalan, R.R.; Hostettler, I.C.; Kadir, K.A.B.A.; Mun, K.S.; Brand, Y.; Mariani, L.; Prepageran, N.; Waran, V. Evolving Strategies for Resection of Sellar/Parasellar Synchronous Tumors via Endoscopic Endonasal Approach: A Technical Case Report and Systematic Review of the Literature. World Neurosurg. 2020, 133, 381–391.e2. [Google Scholar] [CrossRef]
- Schwartz, T.H.; Morgenstern, P.F.; Anand, V.K. Lessons learned in the evolution of endoscopic skull base surgery. J. Neurosurg. 2019, 130, 337–346. [Google Scholar] [CrossRef]
- Hughes, M.A.; Culpin, E.; Darley, R.; McKinlay, J.; Nix, P.; Smedley, A.; Tyagi, A.; Sheikh, A.; Phillips, N. Enhanced recovery and accelerated discharge after endoscopic transsphenoidal pituitary surgery: safety, patient feedback, and cost implications. Acta Neurochir. 2020, 162, 1281–1286. [Google Scholar] [CrossRef]
- Almutairi, R.D.; Muskens, I.S.; Cote, D.J.; Dijkman, M.D.; Kavouridis, V.K.; Crocker, E.; Ghazawi, K.; Broekman, M.L.D.; Smith, T.R.; Mekary, R.A.; et al. Gross total resection of pituitary adenomas after endoscopic vs. microscopic transsphenoidal surgery: a meta-analysis. Acta Neurochir. 2018, 160, 1005–1021. [Google Scholar] [CrossRef]
- Kelly, D.; Lobo, B.; Heng, A.; Barkhoudarian, G.; Griffiths, C. The expanding role of the endonasal endoscopic approach in pituitary and skull base surgery: A 2014 perspective. Surg. Neurol. Int. 2015, 6, 82. [Google Scholar] [CrossRef]
- Awad, A.J.; Mohyeldin, A.; El-Sayed, I.H.; Aghi, M.K. Sinonasal morbidity following endoscopic endonasal skull base surgery. Clin. Neurol. Neurosurg. 2015, 130, 162–167. [Google Scholar] [CrossRef]
- Hong, S.D.; Nam, D.-H.; Seol, H.J.; Choi, N.Y.; Kim, H.Y.; Chung, S.-K.; Dhong, H.-J. Endoscopic Binostril versus Transnasal Transseptal Microscopic Pituitary Surgery: Sinonasal Quality of Life and Olfactory Function. Am. J. Rhinol. Allergy 2015, 29, 221–225. [Google Scholar] [CrossRef]
- Hong, S.D.; Nam, D.-H.; Kong, D.-S.; Kim, H.Y.; Chung, S.-K.; Dhong, H.-J. Endoscopic Modified Transseptal Transsphenoidal Approach for Maximal Preservation of Sinonasal Quality of Life and Olfaction. World Neurosurg. 2016, 87, 162–169. [Google Scholar] [CrossRef]
- Favier, V.; Boetto, J.; Cartier, C.; Segnarbieux, F.; Crampette, L. Endoscopic transnasal transseptal pituitary surgery. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2019, 136, 131–134. [Google Scholar] [CrossRef]
- Al-Baldawi, I.A. Bi-nostril transseptal endoscopic approach to the sphenoidal gate. A new technique. Acta Neurochir. 2017, 159, 1247–1252. [Google Scholar] [CrossRef]
- Valdes, C.J.; Zeitouni, A.; Sirhan, D.; Maio, S.; Tewfik, M.A. The Endoscopic Hemi-Transseptal Approach to the Sella Turcica: Operative Technique and Case-Control Study. J. Neurol. Surg. Part B: Skull Base 2014, 75, 415–420. [Google Scholar] [CrossRef]
- Wen, G.; Tang, C.; Zhong, C.; Li, J.; Cong, Z.; Zhou, Y.; Liu, K.; Zhang, Y.; Tohti, M.; Ma, C. One-and-a-half nostril endoscopic transsphenoidal approach for pituitary adenomas—a technical report. J. Otolaryngol. - Head Neck Surg. 2016, 45, 1–9. [Google Scholar] [CrossRef]
- Takeda, T.; Omura, K.; Mori, E.; Mori, R.; Ishii, Y.; Otori, N. Endoscopic modified transseptal bi-nostril approach for pituitary tumors. Efficacy of complex preservation of every turbinate and olfaction: A STROBE analysis. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2022, 139, 337–342. [Google Scholar] [CrossRef]
- Bove, I.; Solari, D.; Bruneau, M.; Berhouma, M.; Jouanneau, E.; Cornelius, J.F.; Messerer, M.; Daniel, R.T.; Froelich, S.; Mazzatenta, D.; et al. Endoscopic endonasal pituitary surgery: How we do it. Consensus statement on behalf of the EANS skull base section. Brain Spine 2023, 3, 102687. [Google Scholar] [CrossRef]
- Asa, S.L.; Casar-Borota, O.; Chanson, P.; Delgrange, E.; Earls, P.; Ezzat, S.; Grossman, A.; Ikeda, H.; Inoshita, N.; Karavitaki, N.; et al. From pituitary adenoma to pituitary neuroendocrine tumor (PitNET): an International Pituitary Pathology Club proposal. Endocrine-Related Cancer 2017, 24, C5–C8. [Google Scholar] [CrossRef]
- Wang, A.J.; Zaidi, H.A.; Laws, E.R. History of endonasal skull base surgery. 2016, 60, 441–453. [Google Scholar]
- Conrad, J.; Ayyad, A.; Wüster, C.; Omran, W.; Weber, M.M.; Konerding, M.A.; Müller-Forell, W.; Giese, A.; Oertel, J. Binostril versus mononostril approaches in endoscopic transsphenoidal pituitary surgery: clinical evaluation and cadaver study. J. Neurosurg. 2016, 125, 334–345. [Google Scholar] [CrossRef]
- Cavallo, L.M.; Solari, D.; Somma, T.; Cappabianca, P. The 3F (Fat, Flap, and Flash) Technique For Skull Base Reconstruction After Endoscopic Endonasal Suprasellar Approach. World Neurosurg. 2019, 126, 439–446. [Google Scholar] [CrossRef]
- Hadad, G.; Bassagasteguy, L.; Carrau, R.L.; Mataza, J.C.; Kassam, A.; Snyderman, C.H.; Mintz, A. A Novel Reconstructive Technique After Endoscopic Expanded Endonasal Approaches: Vascular Pedicle Nasoseptal Flap. Laryngoscope 2006, 116, 1882–1886. [Google Scholar] [CrossRef]
- Yang, J.; Wen, G.; Tang, C.; Zhong, C.; Zhu, J.; Cong, Z.; Ma, C. Evaluation of Surgical Freedom for One-and-a-Half Nostril, Mononostril, and Binostril Endoscopic Endonasal Transsphenoidal Approaches. J. Neurol. Surg. Part B: Skull Base 2020, 82, 383–391. [Google Scholar] [CrossRef]
- Oertel, J.; Gaab, M.R.; Tschan, C.A.; Linsler, S. Mononostril endoscopic transsphenoidal approach to sellar and peri-sellar lesions: Personal experience and literature review. Br. J. Neurosurg. 2015, 29, 532–537. [Google Scholar] [CrossRef]
- Mazzatenta, D.; Rustici, A.; Serra, C. Editorial: Advances and controversies in skull base tumors: implication for diagnosis, treatment and management. Front. Oncol. 2024, 14, 1377868. [Google Scholar] [CrossRef]
- Pojskić, M.; Arnautovic, A.; Kovacevic, M.; Beckford, N.S.; Qureshi, M.N.; Linder, J.; Arnautović, K.I. Combined Microsurgical, Endoscopic and Neuronavigation Assisted Transseptal-Transsphenoidal Resection of Pituitary Tumors. Acta Medica Acad. 2021, 49, 14–22. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).