Submitted:
10 October 2025
Posted:
11 October 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
1.1. Background on Breast Cancer Screening
1.2. Emergence of Social Media and Digital Platforms in Health Communication
1.3. Rationale and Objectives
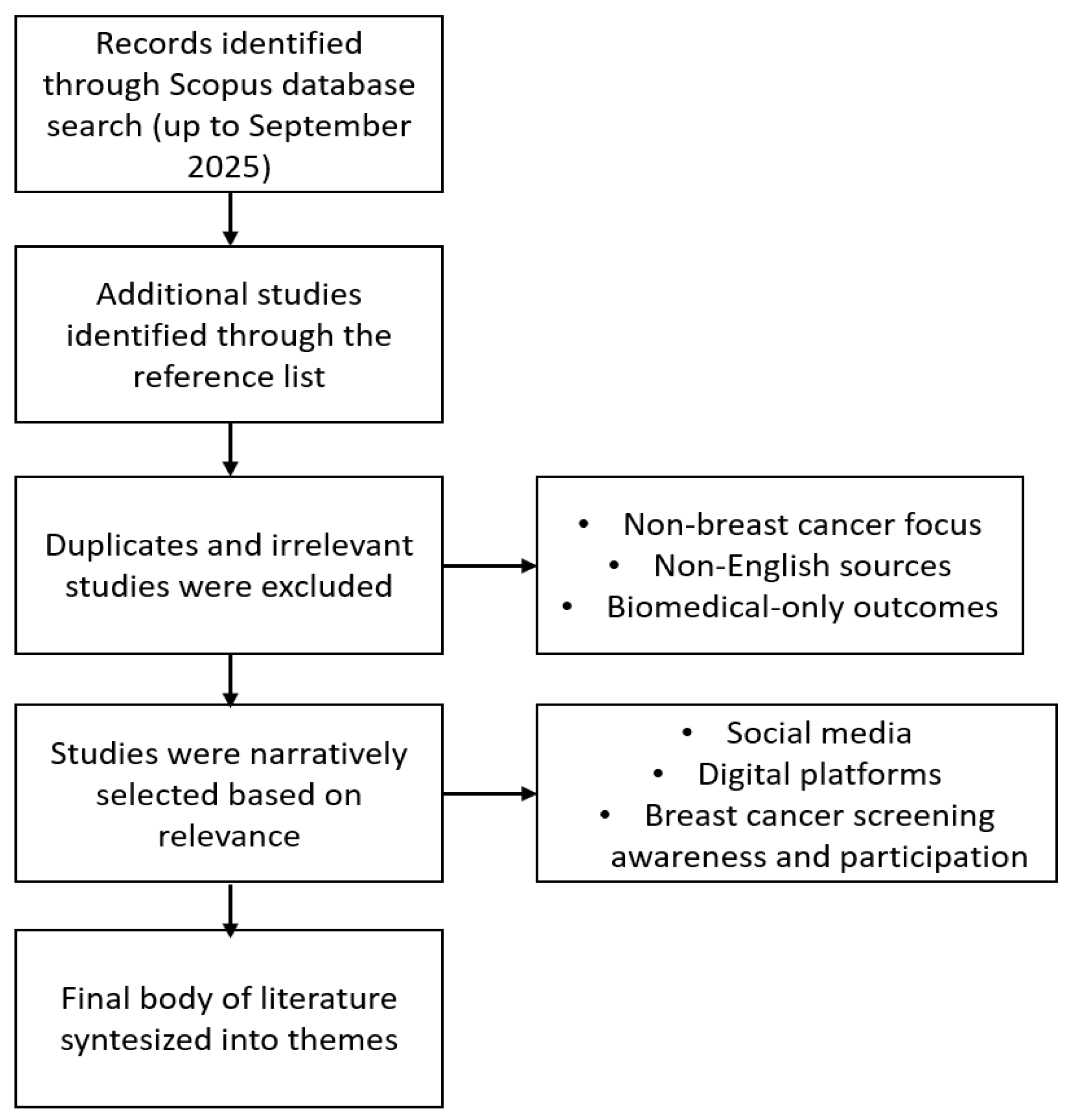
2. Methodology
2.1. Literature Search Strategy
2.2. Assessment of Intervention and Study Designs
2.3. Data Synthesis Approach
2.4. Impact of Social Media and Digital Interventions on Breast Cancer Screening Awareness and Participation
2.5. Barriers to Breast Cancer Screening and Role of Digital Tools in Mitigation
2.6. Quality and Reliability of Online Breast Cancer Screening Information
2.7. The Role of Peer Support, Community Engagement, and Advocacy in Screening Promotion
2.8. Future Directions and Innovations in Personalized Digital Breast Cancer Screening
3. Conclusion
Author Contributions
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sun, M., Reiter, E., Duncan, L. F., & Adam, R. (2025). The role of natural language processing in improving cancer care: A scoping review with narrative synthesis. Artificial Intelligence in Medicine, 168. [CrossRef]
- Alduraidi, H., Tarazi, A., Theeb, L. S., & AlKasaji, M. (2025). Knowledge, Attitudes, and Practices Toward Breast Cancer and Breast Cancer Screening Among Arab Females in the Middle East: A Literature Review. Public Health Nursing, 42(1), 579–588. [CrossRef]
- Padamsee, T. J., Stover, D. G., Tarver, W. L., Washington, C. M., Baltic, R. D., DeGraffinreid, C. R., ... & Nolan, T. S. (2023). Turning the Page on Breast Cancer in Ohio: Lessons learned from implementing a multilevel intervention to reduce breast cancer mortality among Black women. Cancer, 129, 3114–3127. [CrossRef]
- Abuhay, H. W., Alemu, G. G., Aweke, M. N., Fenta, E. T., Mengistu, B., & Mesfin, A. (2025). Clinical breast cancer screening uptake and associated factors among reproductive-age women in Kenya: further analysis of the Kenyan Demographic and Health Survey 2022. PLOS ONE, 20 (4 April). [CrossRef]
- Richardson-Parry, A., Baas, C., Donde, S. S., Ferraiolo, B., Karmo, M., Maravic, Z., ... & Tinianov, S. L. (2023). Interventions to reduce cancer screening inequities: the perspective and role of patients, advocacy groups, and empowerment organizations. International Journal for Equity in Health, 22(1). [CrossRef]
- Jamal, J., MacMillan, F., & McBride, K. (2021). Barriers and facilitators of breast cancer screening amongst culturally and linguistically diverse women in southwestern Sydney: A qualitative explorative study. International Journal of Environmental Research and Public Health, 18(17). [CrossRef]
- Griffiths, M., Scragg, B., Stein-Hodgins, J. R., & Ure, C. (2023). Digital health technologies. In Digital Health (pp. 165–175). [CrossRef]
- Tso, H. H., & Parikh, J. R. (2020). Using Facebook Live to Advocate Breast Cancer Screening. Journal of Digital Imaging, 33(4), 1047–1052. [CrossRef]
- Basch, C. H., & MacLean, S. A. (2019). Breast cancer on Instagram: A descriptive study. International Journal of Preventive Medicine, 10(1). [CrossRef]
- Plackett, R., Kaushal, A., Kassianos, A. P., Cross, A., Lewins, D., Sheringham, J. R., ... & von Wagner, C. (2020). Use of Social Media to Promote Cancer Screening and Early Diagnosis: Scoping Review. Journal of Medical Internet Research, 22(11). [CrossRef]
- Sinha, N., & Sharma, A. (2024). Digital media intervention for breast cancer awareness among rural women: A quasi-experimental study from Bihar, India. Clinical Epidemiology and Global Health, 28. [CrossRef]
- Liow, J. J. K., Lim, Z., Sim, T. M. Y., Ho, P. J., Goh, S. A., Choy, S. D., ... & Hartman, M. B. A. (2022). “It Will Lead You to Make Better Decisions about Your Health”—A Focus Group and Survey Study on Women’s Attitudes towards Risk-Based Breast Cancer Screening and Personalized Risk Assessments. Current Oncology, 29(12), 9181–9198. [CrossRef]
- Yang, H., Zhu, C., Zhou, C., Huang, R., Huang, L., Chen, P., ... & Zhu, C. (2025). Evaluation of Douyin Short Videos on Mammography in China: Quality and Reliability Analysis. JMIR Cancer, 11. [CrossRef]
- Rajabi, R., Abedi, P., Araban, M., & Maraghi, E. (2021). Effects of Education via WhatsApp vs. Compact Disk on Health Literacy and Behavior of Middle-Aged Women about Screening Methods for Breast Cancer. Iranian Journal of Breast Diseases, 14(3), 12–22. [CrossRef]
- Scragg, B., Shaikh, S., Shires, G., Stein-Hodgins, J., Mercer, C. E., Robinson, L., & Wray, J. (2017). An exploration of mammographers’ attitudes towards the use of social media for providing breast screening information to clients. Radiography, 23(3), 249–255. [CrossRef]
- Nguyen, T. T., Le, G. M., Nguyen, T., Le, K., Lai, K., Gildengorin, G. L., ... & McPhee, S. J. (2009). Breast Cancer Screening Among Vietnamese Americans. A Randomized Controlled Trial of Lay Health Worker Outreach. American Journal of Preventive Medicine, 37(4), 306–313. [CrossRef]
- Southwell, B. G., Slater, J. S., Rothman, A. J., Friedenberg, L. M., Allison, T. R., & Nelson, C. L. (2010). The availability of community ties predicts the likelihood of peer referral for mammography: Geographic constraints on viral marketing. Social Science and Medicine, 71(9), 1627–1635. [CrossRef]
- Qin, L., Zhang, X., Wu, A., Miser, J. S., Liu, Y., Hsu, J. C. H. S., et al. (2021). Association between social media use and cancer screening awareness and behavior for people without a cancer diagnosis: Matched cohort study. Journal of Medical Internet Research, 23(8). [CrossRef]
- Bancroft, E. K., Saya, S., Brown, E., Thomas, S. R., Taylor, N., Rothwell, J., & Pope, J. (2022). Examining Associations between Source of Cancer Information and Mammography Behavior among Black Church-Going Women. International Journal of Environmental Research and Public Health, 19(20). [CrossRef]
- Walker, M. J., Blackmore, K. M., Chang, A., Lambert-Côté, L., Turgeon, A., Antoniou, A. C., Bell, K. A., Broeders, M. J. M., Brooks, J. D., & Carver, T. (2024). Implementing Multifactorial Risk Assessment with Polygenic Risk Scores for Personalized Breast Cancer Screening in the Population Setting: Challenges and Opportunities. Cancers, 16(11). [CrossRef]
- Yi, J. C., Ballard, S. A., Walsh, C. A., Friedman, D. N., Ganz, P. A., Jacobs, L. A., Partridge, A. H., Mitchell, S. A., Leisenring, W. M., & Syrjala, K. L. (2025). INteractive survivorship program to improve health care REsources [INSPIRE]: A study protocol testing a digital intervention with stepped care telehealth to improve outcomes for adolescent and young adult survivors. Contemporary Clinical Trials, 148. [CrossRef]
- Dick, K., Humber, J., Ducharme, R., Dingwall-Harvey, A. L. J., Armour, C. M., Hawken, S. J., & Walker, M. C. (2024). The Transformative Potential of AI in Obstetrics and Gynecology. Journal of Obstetrics and Gynaecology Canada, 46(3). [CrossRef]
- Kratzke, C., Garzon, L. S., Lombard, J. R., & Karlowicz, K. A. (2010). Training community health workers: Factors that influence mammography use. Journal of Community Health, 35(6), 683–688. [CrossRef]
| Author(s), Year | Study Design | Intervention Type | Population | Outcomes Measured |
| Sinha & Sharma (2024) | Quasi-experimental | Video-based intervention (educational videos) | Rural women | Knowledge improvement, screening practices |
| Liow et al. (2022) | Mixed-methods (FGDs + surveys) | Risk-based screening discussions (digital + group) | Risk-assessment cohort, diverse women | Attitudes toward screening, willingness to participate |
| Yang et al. (2025) | Cross-sectional content evaluation | YouTube mammography videos | Publicly available videos (online users) | Reliability (DISCERN, GQS), content quality |
| Qin et al. (2021) | Observational (with regression & propensity matching) | Social media exposure (screening awareness campaigns) | Women across sociodemographic strata | Awareness, intention to screen, screening behavior |
| Bancroft et al. (2022) | Experimental & behavioral analysis | Social media campaign + behavior change techniques | Community-based populations | Screening uptake, behavior change mechanisms |
| Plackett et al. (2020) | Scoping review / mixed approaches | Social media interventions (Twitter, Facebook, YouTube) | General women, health-seeking populations | Knowledge dissemination, awareness, screening participation |
| Griffiths et al. (2023) | Observational | Instagram and Twitter engagement analysis | General female users, online communities | User engagement, awareness trends |
| Southwell et al. (2010) | Qualitative & survey-based | Online community & peer support forums | Women engaged in online health communities | Social support, community engagement for screening |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





