1. Introduction
Dupuytren's disease is a pathological change in the connective tissue of the hand that occurs more frequently from the age of 50. This leads to an increased formation of nodular and cord-like connective tissue in the palm of the hand and on fingers. These nodules and cords can be felt under the skin and can continue to thicken and contract. This causes the affected fingers to bend towards the palm of your hand and can then no longer move without restriction.
The exact cause of Dupuytren's disease has not yet been clarified. In addition to hereditary predisposition, external factors such as an injury are being discussed as triggers. The influence of growth hormones is also assumed. The disease appears to occur more frequently in people who have diabetes, smoke or consume excessive amounts of alcohol.
Dupuytren's disease occurs most frequently on the little finger and ring finger, less frequently on the other fingers. In 70 to 80% of cases, both hands are affected.
In the layer between the skin and flexor tendons, nodular and cord-like indurations can be felt at the beginning. As a rule, there is no pain. As the disease progresses, these growths spread further, resulting in crooked fingers that can no longer be extended. The tissue proliferation can also affect nerves and blood vessels, leading to sensory or circulatory problems. The main problem, however, is the limited ability to stretch your hand. Dupuytren's disease can progress over several months and years, so that even simple activities can cause problems over time.
Some conservative measures such as ultrasound treatment, glucocorticoid injections or vitamin E have not yet shown any clear success. Radiotherapy can slow down or halt the progression of the disease in the early stages.
From stage 2 and in the case of functional deficits, surgical therapy can be considered. Complications such as iatrogenic injuries to nerves and vessels, wound edge necrosis, sympathetic reflex dystrophies and the generally high risk of recurrence (up to 40 %) must be taken into account when determining the indication. Conversely, hesitant treatment can lead to complete collapse of the fingers with reduced supply. Postoperative hand therapy (occupational therapy, physiotherapy) must be carried out immediately.
Minimally invasive needle fasciotomy, partial fasciectomy and resection of the palmar aponeurosis and dermofasciectomy with full-thickness skin grafting can also be considered. One disadvantage of open surgery is the long wound healing time and the risk of infection and recurrent contractures due to scarring.
Furthermore, an infiltration of collagenase from Clostridium histolyticum can be performed. In addition, various other treatment options are currently being researched. One example is the intralesional injection of TNF blockers.
Percutaneous needle fasciotomy of Dupuytren's disease is used to structurally weaken the palmar fibrosis in contractures of the long fingers under local anesthesia using a commercially available injection needle and then extended manually by stretching the finger. The procedure can be performed on an outpatient basis. This is followed by a stringent post-treatment regimen with continuous stretching; in severe cases, a plaster splint can be applied temporarily.
The contracture is classified according to
Tubiana, Michon and Thomine, 1968:
- Stage 0: no nodules, no cords, no extensor deficit
- Stage N: nodule formation in the palm without extensor deficit
- Stage 1: extensor deficit up to 45°
- Stage 2: extensor deficit 46 to 90°
- Stage 3: extensor deficit < 91 to 135°
- Stage 4: extensor deficit > 135°
This study analyzed 1146 patient cases with 1803 treated finger rays from 18 years of treatment at one center for this treatment.
2. Materials and Methods
A retrospective analysis of the treatment records of a center for needle fasciotomy in Germany was carried out.
All patients who were treated with a needle fasciotomy were recorded by means of a systematic evaluation of the patient file and, as a first step, the center's internal documentation was evaluated. This was followed by a written survey of all patients using a structured questionnaire about late complications, recurrences, improvement in usability, recommendation and satisfaction. The statistical analysis was carried out using SPSS software.
3. Results
Between 1994 and 2012, 1146 patients (83% m, 14%w average age 52.6 years (19-76y)) with 1803 finger rays were treated, the data of which were analyzed according to the records, 50% right, 45% left, 5% unknown.
44% of the cases affected the little finger, 40% the ring finger, 12% the middle finger, 2% each the index finger and thumb.
The distribution of stages according to Tubiana et al was:
Stage N: 66 cases
Stage 0: 2 cases
Stage 1: 594 cases
Stage 2: 570 cases
Stage 3: 416 cases
Stage 4: 155 cases
The average duration of surgery was 26.9 min (12 - 39), the average duration of pain was 2.6 days (0-12) post-op.
Improvements were achieved depending on the stage:
Table 1.
Improvement post OP.
Table 1.
Improvement post OP.
| Stage prä OP |
n |
Improvement stage |
| N |
66 |
- 0,88 |
| 0 |
2 |
0,00 |
| 1 |
594 |
-0,97 |
| 2 |
570 |
-1,86 |
| 3 |
416 |
-2,55 |
| 4 |
155 |
-3,02 |
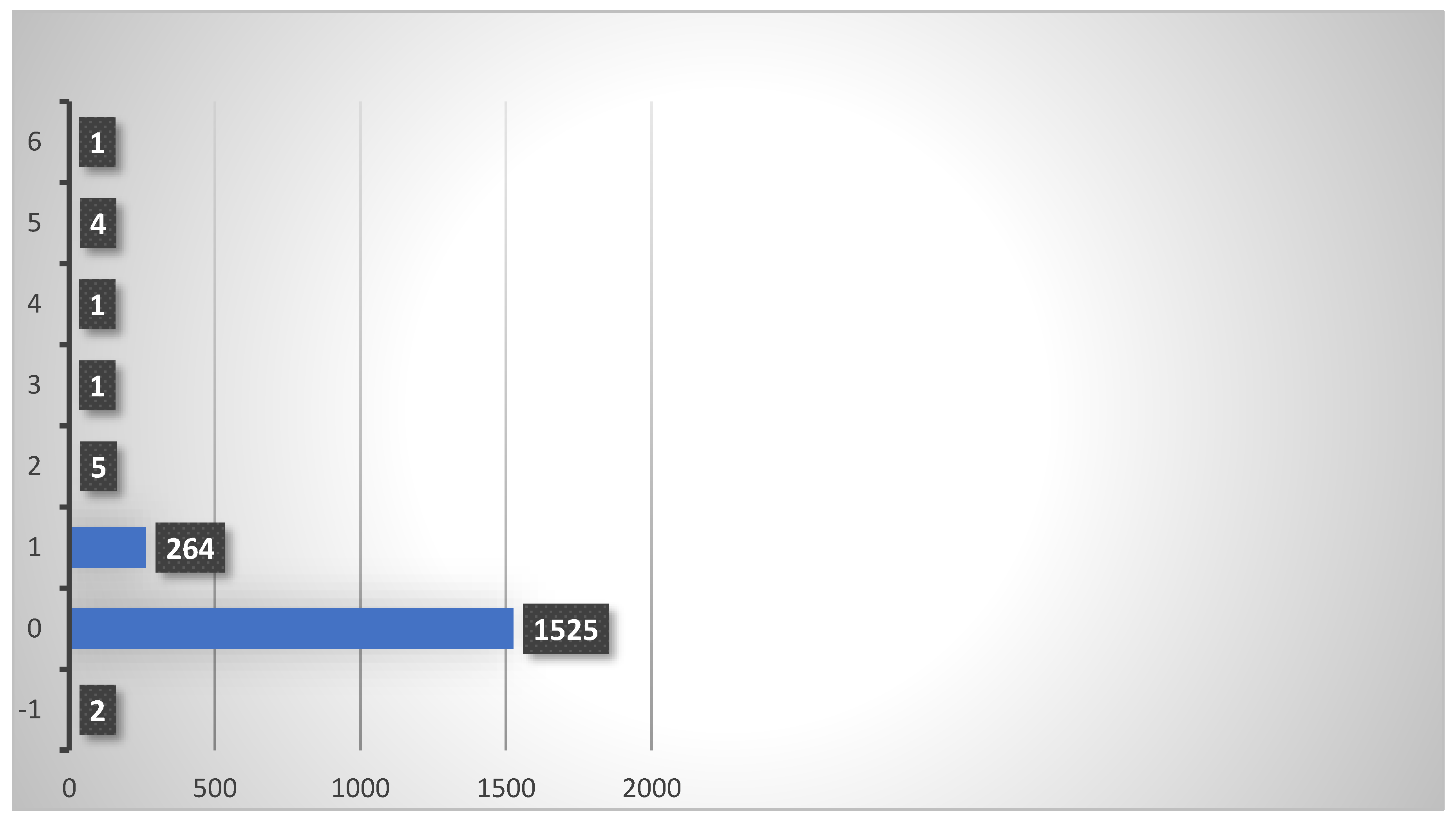
The figures show that in the later stages of the disease, full extension of the finger is often no longer achieved, whereas in stages 1 and 2, full compensation of the contracture is usually achieved. The perioperative complications are shown in
Figure 1:
The main and most frequent complication here was skin lesions, which occurred in 15.8% of cases. These were superficial epidermal tears, all of which healed conservatively and without sutures. Deep lesions with interruption of the continuity of the dermis and the need for surgical treatment such as suturing or stapling did not occur.
The second most common complication was transient swelling (0.2% of cases). All swellings were completely resolved after conservative treatment with elevation, cooling and elastic wrapping. The exact cause could not be further evaluated here, but hematomas and edema are possible causes.
The third most common complication was flexor tendon rupture (0.2% of cases). This is a relevant complication that requires surgical tendon suturing. The complication can occur in particular if a vertical stitch direction is chosen for the fasciotomy and if there are other pre-existing conditions, especially chronic soft tissue damage (e.g. rheumatoid arthritis, scleroderma), which make the tendon more susceptible to rupture. In particular, this complication is rare, but should be mentioned as part of the clarification.
Bone fracture (middle phalanx), hypesthesia and complete treatment failure without improvement of the extension occur in fourth place, but these are exceptional cases with a rate of 0.06% in this study.
Table 2.
Percentage distribution of complications in relation to stage; -1 = not recorded, 0= none, 1 = skin tear, 3= swelling, 4= hypoesthesia, 5= treatment failed/no effect, 6= flexor tendon rupture, 8= fracture (here based on middle phalanx).
Table 2.
Percentage distribution of complications in relation to stage; -1 = not recorded, 0= none, 1 = skin tear, 3= swelling, 4= hypoesthesia, 5= treatment failed/no effect, 6= flexor tendon rupture, 8= fracture (here based on middle phalanx).
| Stage |
|
Complications |
Σ |
| |
-1 |
0 |
1 |
3 |
4 |
5 |
6 |
8 |
all |
compl |
| -1 |
1,5% |
90,9% |
7,6% |
0,0% |
0,0% |
0,0% |
0,0% |
0,0% |
100% |
7,58% |
| 0 |
0,0% |
100,0% |
0,0% |
0,0% |
0,0% |
0,0% |
0,0% |
0,0% |
100% |
0,00% |
| 1 |
0,2% |
91,8% |
7,9% |
0,2% |
0,0% |
0,0% |
0,0% |
0,0% |
100% |
8,08% |
| 2 |
0,0% |
87,5% |
11,9% |
0,4% |
0,0% |
0,0% |
0,2% |
0,0% |
100% |
12,46% |
| 3 |
0,0% |
79,6% |
19,0% |
0,0% |
0,2% |
0,2% |
0,7% |
0,2% |
100% |
20,43% |
| 4 |
0,0% |
56,8% |
41,9% |
1,3% |
0,0% |
0,0% |
0,0% |
0,0% |
100% |
43,23% |
Unsurprisingly, the complication rate was higher in cases with a higher stage of disease. This effect tends to be evident for all complications.
173 questionnaires were analyzed. In 77% of the patients, a recurrence or a noticeable deterioration occurred during the course, of which 35% required treatment.
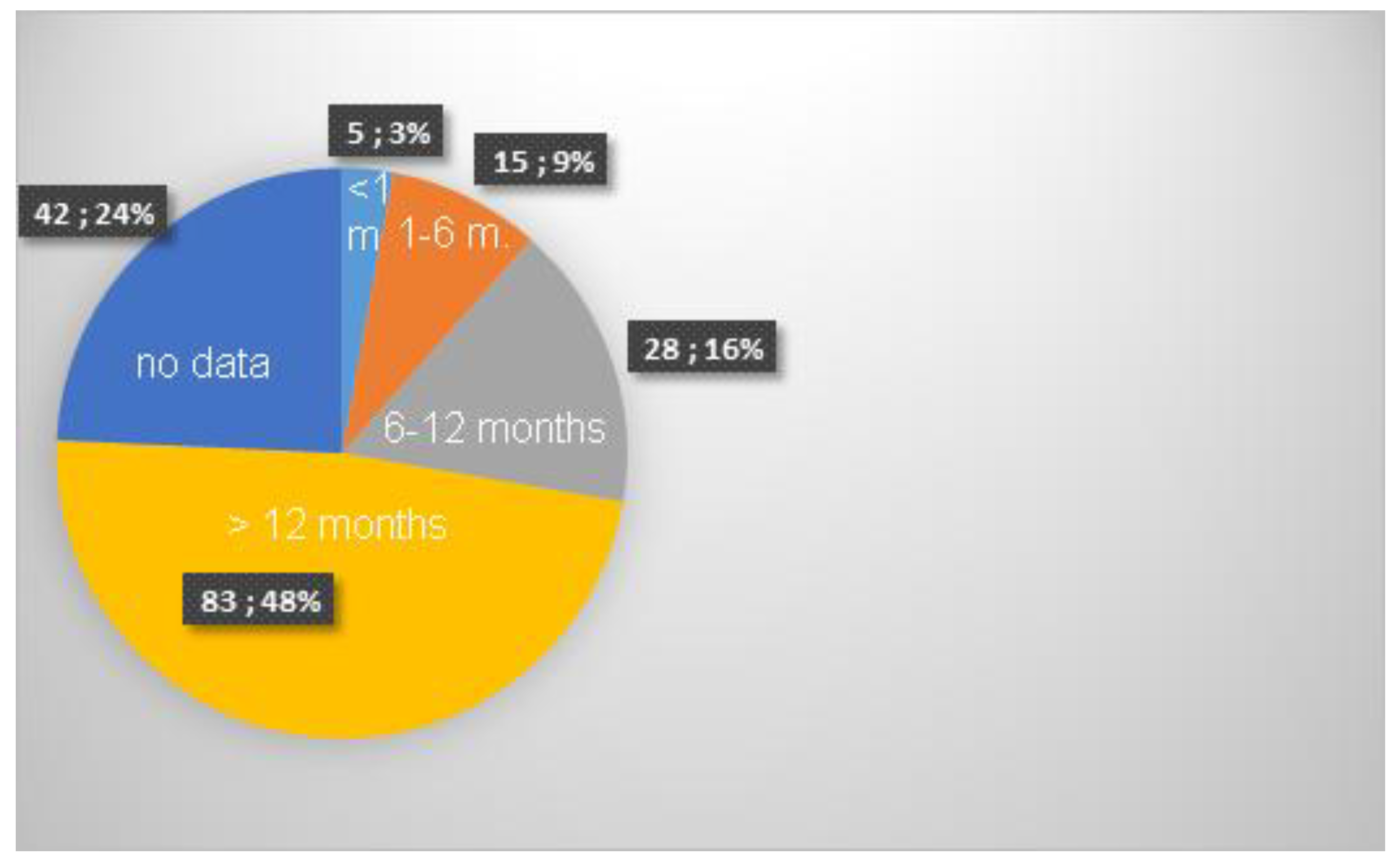
Figure 2.
Time until the occurrence of a recurrence.
Figure 2.
Time until the occurrence of a recurrence.
The data show that the vast majority of recurrences only occurred after more than 12 months. While in the immediate post-operative phase up to 3 months post-op only 3% of patients complained of a renewed deterioration, this figure was 12% cumulatively up to the 6th month and 28% up to and including the 12th month. Data on the duration and consequences of independent follow-up treatment, in particular stretching exercises, which should be performed daily for at least 1 year after the operation, could not be collected. The overall recurrence rate was thus 76%, whereby even slight new restrictions of movement that did not significantly restrict clinical function were considered a recurrence.
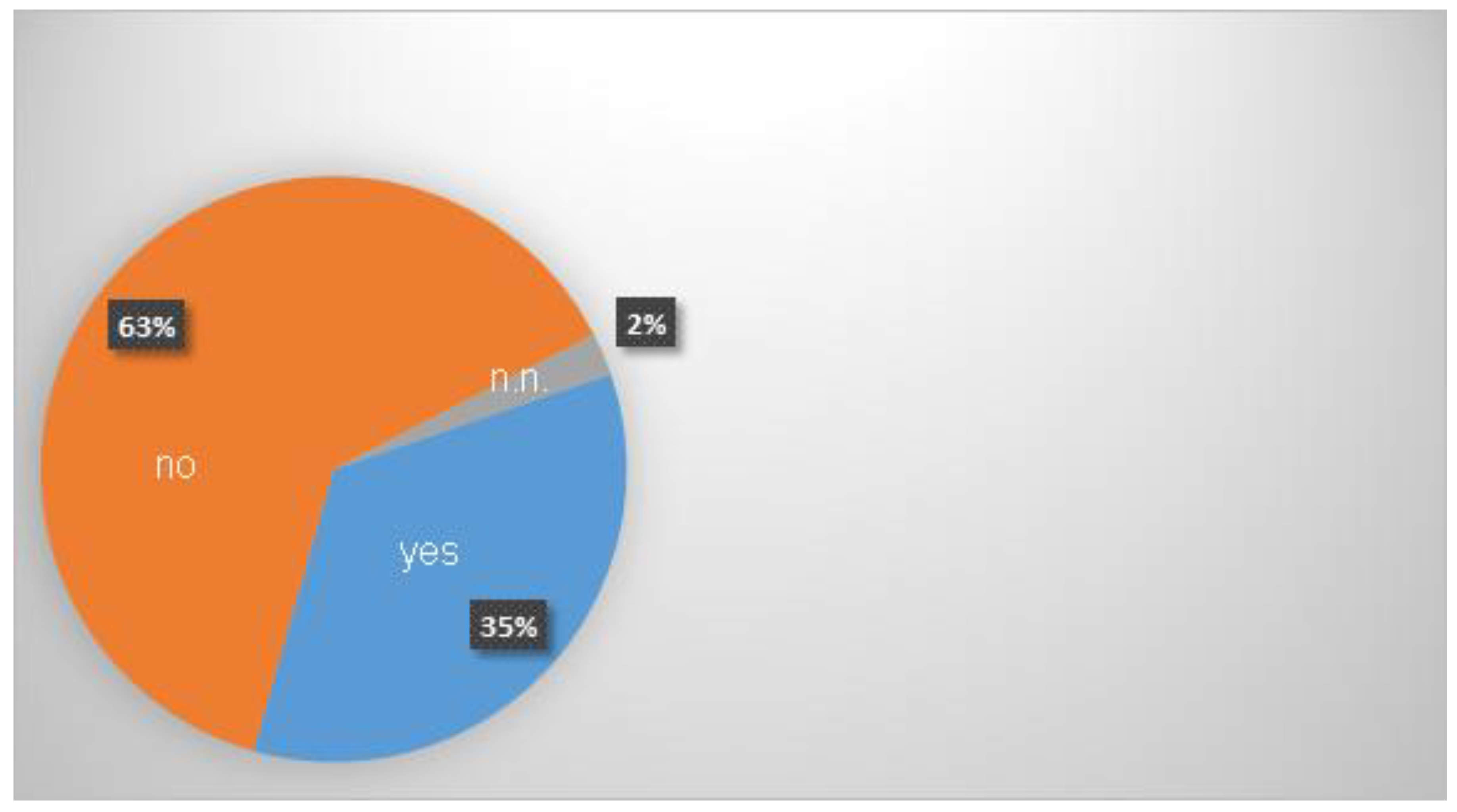
Figure 3.
Re-treatment in the course.
Figure 3.
Re-treatment in the course.
Closely related to the recurrence rate was the question of whether the treated fingers had been treated again.
Here, patients were generally asked about renewed therapy, irrespective of whether a needle fasciotomy, injection therapy or open fasciotomy was performed again.
It is striking that although a total of 76% of patients reported a recurrence, only 35%, i.e. less than half (46%) of patients with a recurrence, underwent further treatment.
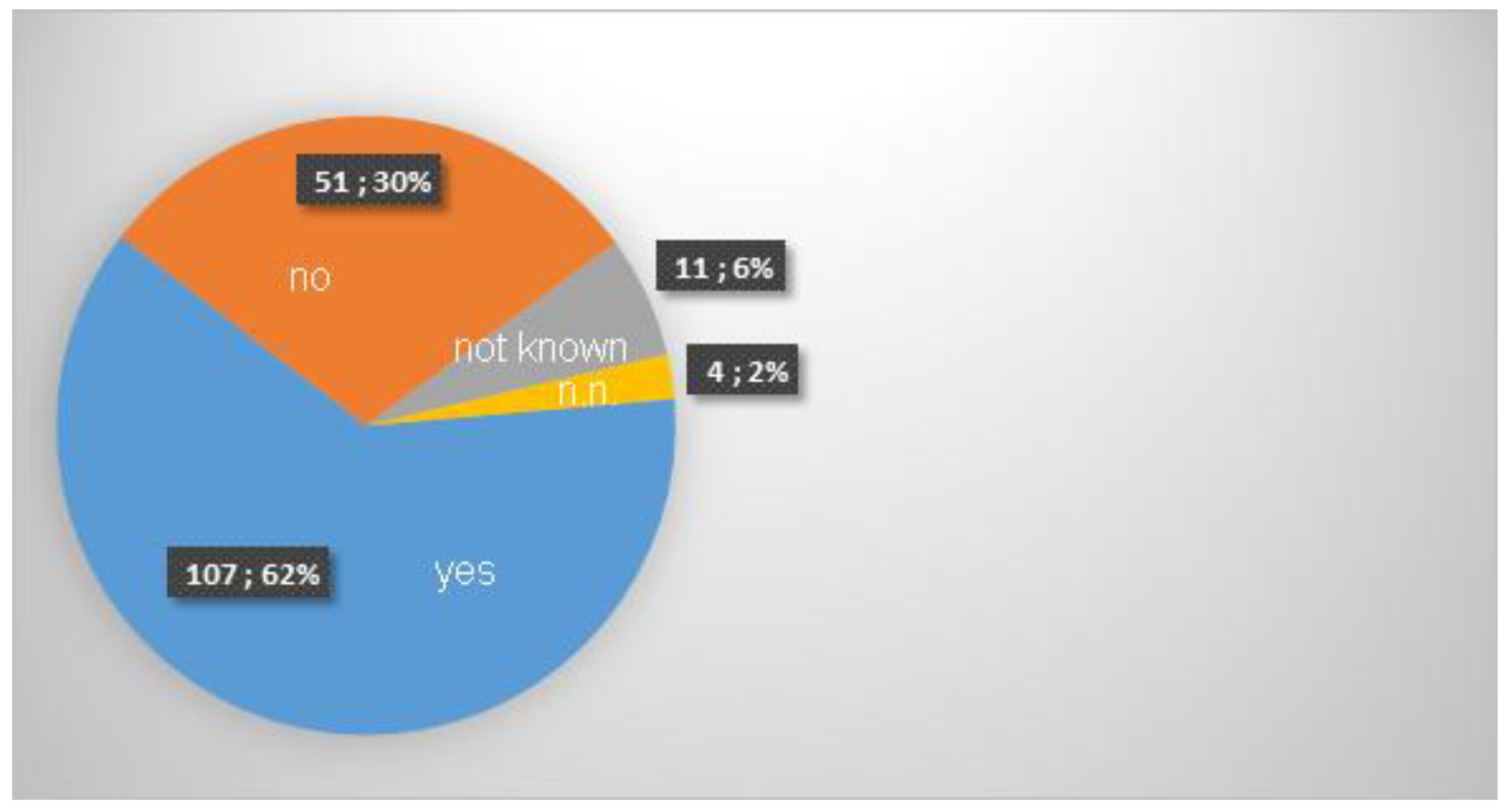
In 62% of cases, there was an improvement in the ability to use the treated hand in everyday life.
Figure 4.
Improvement of usability.
Figure 4.
Improvement of usability.
The majority of patients reported an improvement in everyday function after the operation. It should be noted that although the success rate of the operation (with an improvement in extension) was 99.9% (1802 of 1803 cases), only 30% of respondents reported no improvement in everyday function. It should be noted that everyday function was surveyed at the time of the interview, i.e. a maximum of 18 years after the procedure. This figure should therefore be viewed in conjunction with the recurrence rate.
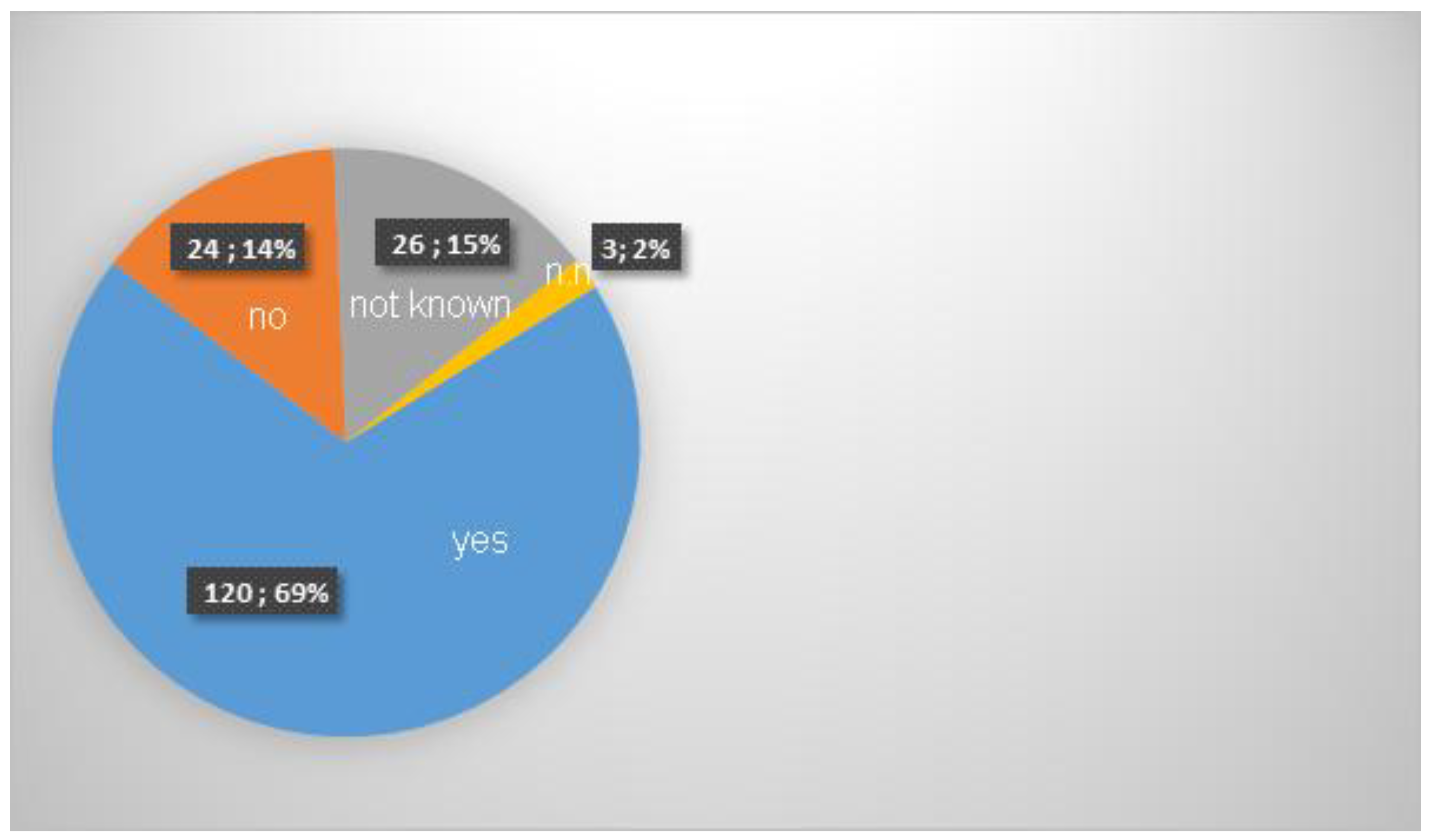
69% of patients would recommend the operation to others.
Figure 5.
recommendation.
Figure 5.
recommendation.
Overall satisfaction had a value of 7.2 on a scale of 1 - 10.
4. Discussion
Dupuytren's disease is a disease of the palmar aponeurosis of the hand that is characterized in the early stages by thickening and hardening, and in the advanced stages by a flexion contracture/extension deficit of the long fingers. Males between the ages of 40 and 50 are most frequently affected; the cause is unclear. For existing contractures, minimally invasive needle fasciotomy is used in addition to collagen injection and open fasciotomy. The advantages of needle fasciotomy compared to open resection are that it is less invasive, faster wound healing and technically easier to perform, while the disadvantage is the higher recurrence rate.
Needle fasciotomy was first introduced in 1993 by the French surgeon Badois [
1] was published. At that time, skin lesions were reported in 16%, sensory disturbances in 2% and infection in 2% of cases. Bleton et al [
2] reported skin lesions in 4%, sensory disturbances in 2% and an infection rate of 1% in a prospective study. A number of other authors have also published case series [
4,
5,
6,
7,
8,
9,
10,
11,
12,
13,
14], Here the recurrence rates were between 12% [
6] and 73% [
4] but with a maximum follow-up period of 7 years.
In the present study, a very long follow-up period of 20 years was realized for the first time with a relevant number of cases. The results and in particular the recurrence rate correspond to the above-mentioned values in the literature, which suggests that no further recurrences are to be expected after 5-7 years postoperatively.
Improvement in the ability to use the joint in everyday life was 62% in our study, van Rijssen [
15] reports an improvement in 77% of cases.
By far the most common complication of the procedure is a skin lesion. This is due to several circumstances. Firstly, the skin is perforated during the needle fasciotomy, and secondly, the condition usually affects patients over the age of 50, meaning that the skin is tendentially more vulnerable than in younger patients. Injuries can therefore occur due to the sometimes high force required for stretching. The data also show that skin lesions increase significantly in the later stages of the disease, from 19% in stage 3 to 41% in stage 4. This can easily be explained by the fact that patients in later stages tend to have a significantly longer duration of disease and thus also a shortening of the soft tissue, so that lesions are more likely to occur during forced stretching. However, all skin lesions were only superficial and the continuity of the dermis was not impaired in any case. All skin lesions healed completely under conservative treatment with wound dressings and no suturing was necessary in any case. This complication is therefore not considered serious. One disadvantage, however, is that a skin injury makes the necessary follow-up treatment more difficult. Aftercare involves patients consistently stretching the treated finger completely several times a day, for example by placing the palm of the hand on a table top. This follow-up treatment is necessary because the scar tissue causing the contracture is not removed as in open surgery, but only perforated. The tissue itself is therefore still present and can lead to further contractures as the perforation heals. This must be counteracted consistently and permanently. Simple physiotherapy is not sufficient here, as it cannot be carried out several times a day on a permanent basis. Instructing patients on the simple stretching exercise mentioned above and consistent implementation are therefore essential for successful treatment. Due to skin lesions, this exercise can be more painful for a few days after the procedure, but this did not result in a deterioration in the outcome.
These data are consistent with the results of van Rijssen [
15], who reported no major complication and non-irritant healing skin lesions in 30 cases, Nydick [
16], who reported no major complication in 29 cases, and the meta-study by Beaudreuil [
17], who found skin lesions in 8% of cases, transient dysesthesia in 3%, localized infection in 0.7% and flexor tendon lesions in 0.2%.
Strömberg [
18] found no difference in outcome after 2 years between needle fasciotomy and collagenase injection. It should be noted that needle fasciotomy is considerably less expensive.
Despite the comparatively high recurrence rate compared to open fasciotomy, we achieved a high patient satisfaction and recommendation rate.
An improvement in everyday function and the recommendation rate of patients were of the same order of magnitude (62% / 69%). It is striking that the improvement in everyday function does not correlate well with the initially very high improvement in contracture. It can be assumed that this is partly due to the fact that a relevant rate of recurrences was reported, but also to the fact that patients do not perceive the limitations caused by the Duputryen's contracture in everyday life as pronounced. 32% of the patients came for treatment in stage 3 or 4, when there were already significant contractures with severe loss of movement. As these mainly affect fingers IV and V, the impairments in the patients' everyday lives do not appear to be pronounced. This fact is also supported by the fact that although 77% of patients experienced a recurrence or worsening of function during the course of treatment, less than half (35%) underwent further treatment (regardless of the treatment method used for the new treatment).
The very low rates of other complications should be emphasized. With a “blind” technique, in which tissue is cut with a sharp blade, significantly higher rates of vascular injuries (which did not occur at all), nerve transections (N=1), failure of therapy without improvement intraoperatively (N=1) and flexor tendon ruptures (N=4) would be expected.
In order to achieve these low complication rates, some technical details need to be considered. Firstly, it seems sensible to use sufficient local anesthesia. The needle must be able to move freely in the tissue during the procedure without causing significant pain in order to achieve the necessary large-area splitting of the thickened fascia. With transverse fasciotomy, the needle tip can often be recognized under the opposite skin without perforating the cutis of the opposite side. This ensures that the full width of the fascia has been severed and that no fibers that are remote from the cutaneous insertion site have been missed.
It is also advisable to keep the finger extended during the fasciotomy, thereby tensing the fascia. This gives a good feel for the fasciotomy as the needle cuts through the coarse tissue. The surgeon has good haptic feedback from the needle; there is a coarse resistance in the tissue and a real feeling of cutting through coarse fascial tissue. This differs significantly from the haptic feedback when, for example, the flexor tendon is hit. This is significantly softer and offers much less resistance to the needle.
The permanent stretching of the affected finger also provides a good indication of when a fasciotomy has been performed and the tissue is giving way. This can be determined by a typical loss of resistance, together with a typical crepitatio that can be felt and heard in the surgical area. Ideally, the finger can then be fully extended immediately. In some cases, the extension can then be completed with slightly higher force. However, caution is advised in cases of known osteoporosis to avoid provoking a fracture. However, in view of the above figures (1 fracture in 1803 fingers treated), this risk should also be regarded as low.
This study does not differentiate between patients with or without concomitant rheumatoid arthritis. However, given the known risk of joint instability and - in the case of long-term cortisone therapy - osteoporosis, caution is advised in these patients. In these cases, it is advisable to make the fasciotomy somewhat more extensive so that less force is required to stretch the fingers.
It is striking that only 46% of patients with a recurrence underwent further treatment. This is particularly due to the fact that needle fasciotomy, as a minimally invasive and less traumatizing procedure, leaves all treatment options open for recurrence treatment. After a needle fasciotomy, a new needle fasciotomy, an injection treatment or an open fasciotomy can be performed; in particular, minimally invasive treatment options are still available.
Although there are no structured studies comparing the various treatment options for recurrences, the authors do not consider it expedient to use needle fasciotomy for recurrences following open fasciotomy. On the one hand, the tissue is much more contacted due to the scarring of the open operation and it is technically much more difficult to loosen the adhesion, and on the other hand, the risk of vascular, nerve or tendon injury in the case of altered anatomy does not seem sufficiently calculable to us. However, further examinations should be carried out on patients with recurrences.
The fact that the majority of patients with a recurrence did not undergo further treatment suggests that they did not complain of any significant restrictions in their everyday function, i.e. that the recurrence did not impair their function. Although the exact degree of recurrence was not queried because the data did not appear to be sufficiently usable for medical laypersons, it can be assumed on the basis of the low re-therapy rates that predominantly mild recurrences occurred. However, this is a conclusion that cannot be drawn directly from the data collected.
One of the key findings of the study is the improvement in everyday functioning. Here, 30% of the patients surveyed reported no improvement in everyday function. It should be noted here that the questionnaire asked about the improvement in everyday function at the time of the survey, i.e. the recurrences, which occurred in 76% of cases, were already taken into account. As the survey was conducted up to 18 years after the operation, it can be assumed that the primary rate of improvement in everyday function postoperatively is significantly higher. At this point, it should again be pointed out that consistent follow-up treatment with independent stretching exercises by the patients is essential. In the early days of needle fasciotomy, this necessity was not emphasized with great urgency, so that deficits can certainly be expected here.
At present, it is consistently emphasized in the treatment of the authors that stretching exercises should be performed several times a day for at least 1 year. These are simple and can be performed within a few seconds by placing the hand with the palm flat on the table and pressing the affected finger with the other hand into full contact with the table top, i.e. until it is fully extended. This can be done easily, for example at every meal, and without aids or an assistant. Providing a leaflet and arranging check-ups every 3 months are helpful in maintaining adherence to therapy.
Needle fasciotomy thus appears to be suitable as a minimally invasive first-line therapy for treating patients with Dupuytren's contractures. The rate of serious complications is very low, in line with the literature. In the event of an unsatisfactory result or the occurrence of a recurrence, open fasciectomy and collagenase injection can also be resorted to without any disadvantages or increased risks for the patient.
The limitation of our retrospective study lies in the restriction to one surgeon and the selection of the questionnaire return due to the necessary active cooperation of the patients. Furthermore, the results could not be collected in a blinded manner..
5. Conclusions
Needle fasciotomy is a low-complication and gentle treatment for Duputryen's contracture, but with a relevant recurrence rate. The need for revision is 35% in the long term. This makes needle fasciotomy as a first line therapy a minimally invasive and a gentle treatment method.
Author Contributions
Conceptualization, methodology, OA, PG; investigation, resources, data curation, writing—original draft preparation, PG; Supervision, OA.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to retrospective literature analysis.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Badois FJ, Lermusiaux JL, Massé C, Kuntz D. Traitement non chirurgical de la maladie de Dupuytren par aponevrotomie a l’aiguille. Rev Rhum Ed Fr 1993, 60, 808–813. [Google Scholar]
- Bleton R, Marcireau D, Almot J-Y, Treatment of Dupuytren disease by percutaneous needle fasciotomy. In Saffer P, Amadio PC,Foucher G, eds. Current practice in hand surgery. London: Martin Dunitz, 1997:187–193.
- Lermusiaux JL, Debeyre N. Le traitement medical de la malidie de Dupuytren. Rhumatologique. Expans. Sci. 1979, 338–343. [Google Scholar]
- Jurisic D, Kovic I, Lulic I, Stanec Z, Kapovic M, Uravic M. Dupuytren disease characteristics in Primorsko-goranska County, Croatia. Coll Antropol 2008, 32, 1209–1213. [Google Scholar]
- Tonkin MA, Burke FD, Varian JP. Dupuytren contracture, a comparative study of fasciectomy and dermofasciectomy in one hundred patients. J Hand Surg 1984, 9B, 156–162. [Google Scholar]
- Ullah AS, Dias JJ, Bhowal B. Does a “firebreak” full-thickness Skin graft prevent recurrence after surgery for Dupuytren contracture? A prospective, randomised trial. J Bone Joint Surg 2009, 91B, 374–378. [Google Scholar]
- Gelberman RH, Amiel D, Rudolph RM, Vance RM. Dupuytren contracture. An electron microscopic, biochemical, and clinical correlative study. J Bone Joint Surg 1980, 62A, 425–432. [Google Scholar]
- Dias JJ, Braybrooke J. Dupuytren contracture, an audit of the outcomes of surgery. J Hand Surg 2006, 31B, 514–521. [Google Scholar]
- Citron ND, Nunez V. Recurrence after surgery for Dupuytren disease, a randomized trial of two skin incisions. J Hand Surg 2005, 30B, 563–566. [Google Scholar]
- Hueston, JT. Recurrent Dupuytren contracture. Plast Reconstr Surg 1963, 31, 66–69. [Google Scholar] [CrossRef] [PubMed]
- Cools H, Verstreken J. The open palm technique in the treatment of Dupuytren disease. Acta Orthop Belg 1994, 60, 413–420. [Google Scholar]
- Adam RF, Loynes RD. Prognosis in Dupuytren disease. J Hand Surg 1992, 17A, 312–317. [Google Scholar]
- Foucher G, Cornil C, Lenoble E. Open palm technique for Dupuytren disease. A five-Year Follow-up. Ann Chir Main Memb Super 1992, 11, 362–366. [Google Scholar]
- Nieminen S, Lehto M. Resection of the palmaris longus tendon in surgery for Dupuytren contracture. Ann Chir Gynaecol 1986, 75, 164–167. [Google Scholar]
- van Rijssen AL, Werker PN. Percutaneous needle fasciotomy in Dupuytren disease. J Hand Surg 2006, 31B, 498–501. [Google Scholar]
- Nydick JA, Olliff BW, Garcia MJ, Hess AV, Stone JDA comparison of percutaneous needle fasciotomy and collagenase injection for Dupuytren disease. J. Hand Surg. 2013, 38, 2377–2380. [CrossRef] [PubMed]
- Beaudreuil J, Lellouche H, Orcel P, Bardin T. Needle aponeurotomy in Dupuytren's disease. Jt. Bone Spine 2012, 79, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Strömberg, J. , Sörensen, A. I., & Fridén, J. Percutaneous needle fasciotomy versus collagenase treatment for Dupuytren contracture, a randomized controlled trial with a two-year follow-up. JBJS 2018, 100, 1079–1086. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).