Submitted:
11 July 2025
Posted:
15 July 2025
You are already at the latest version
Abstract
Keywords:
Introduction
Methodology
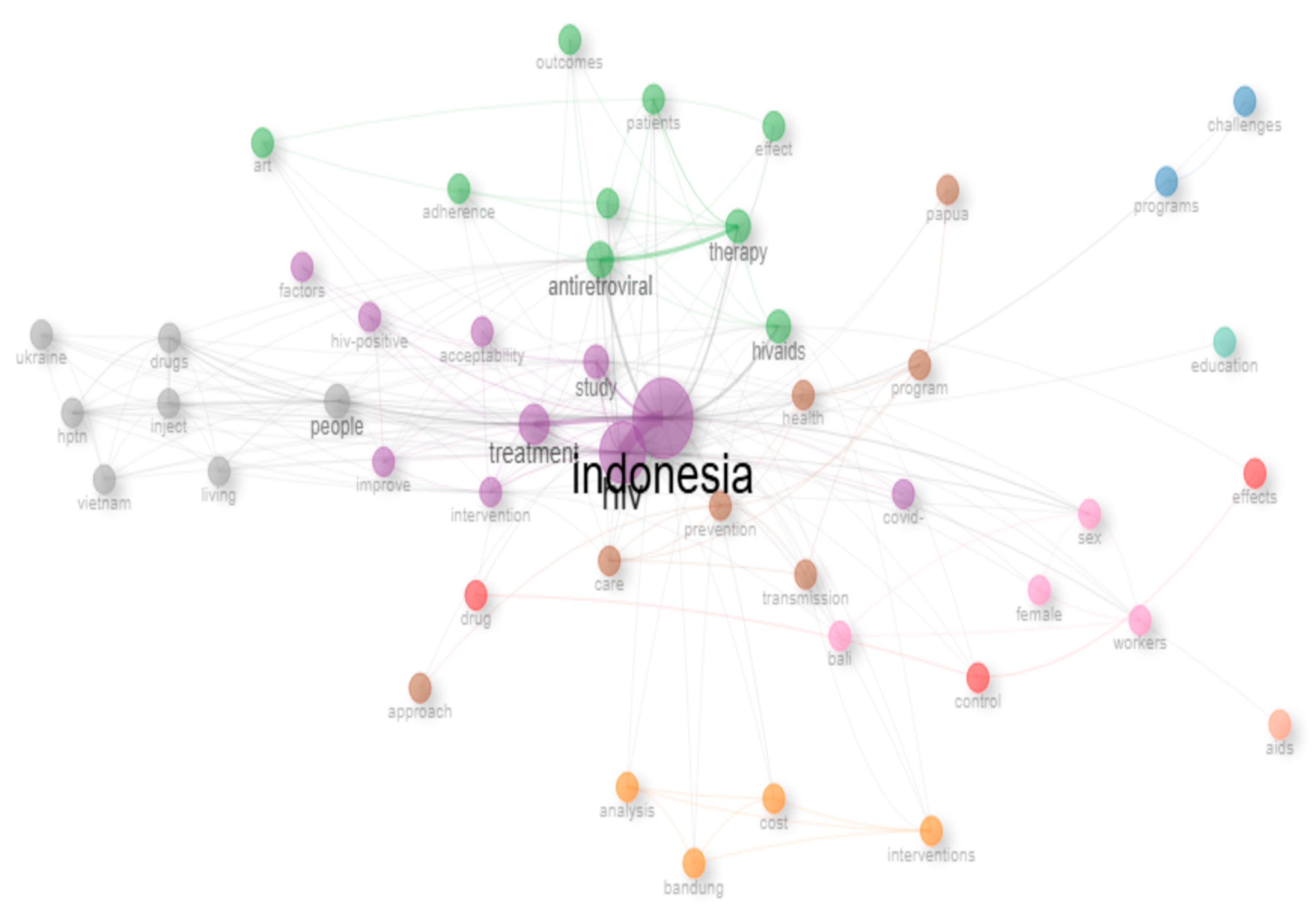
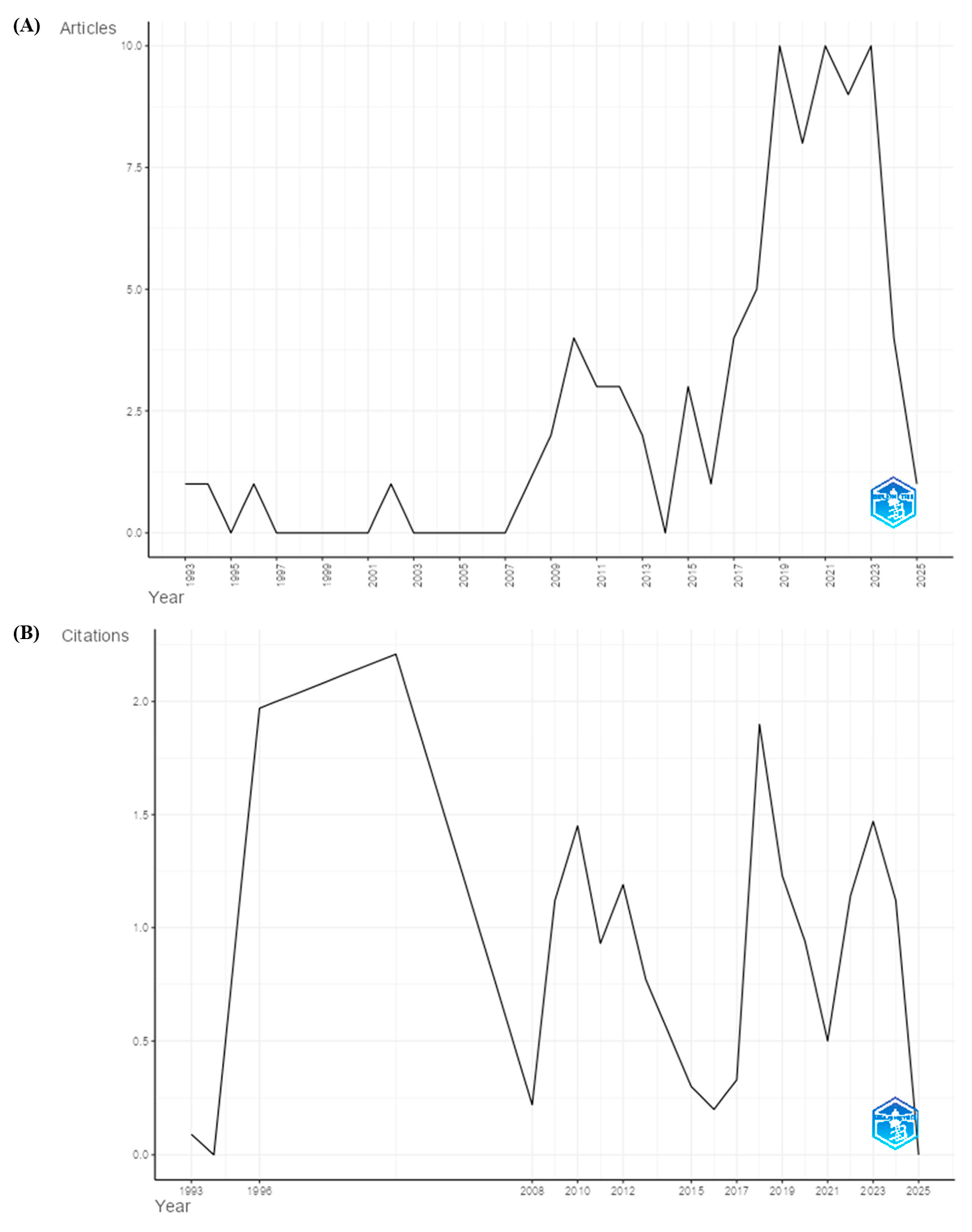
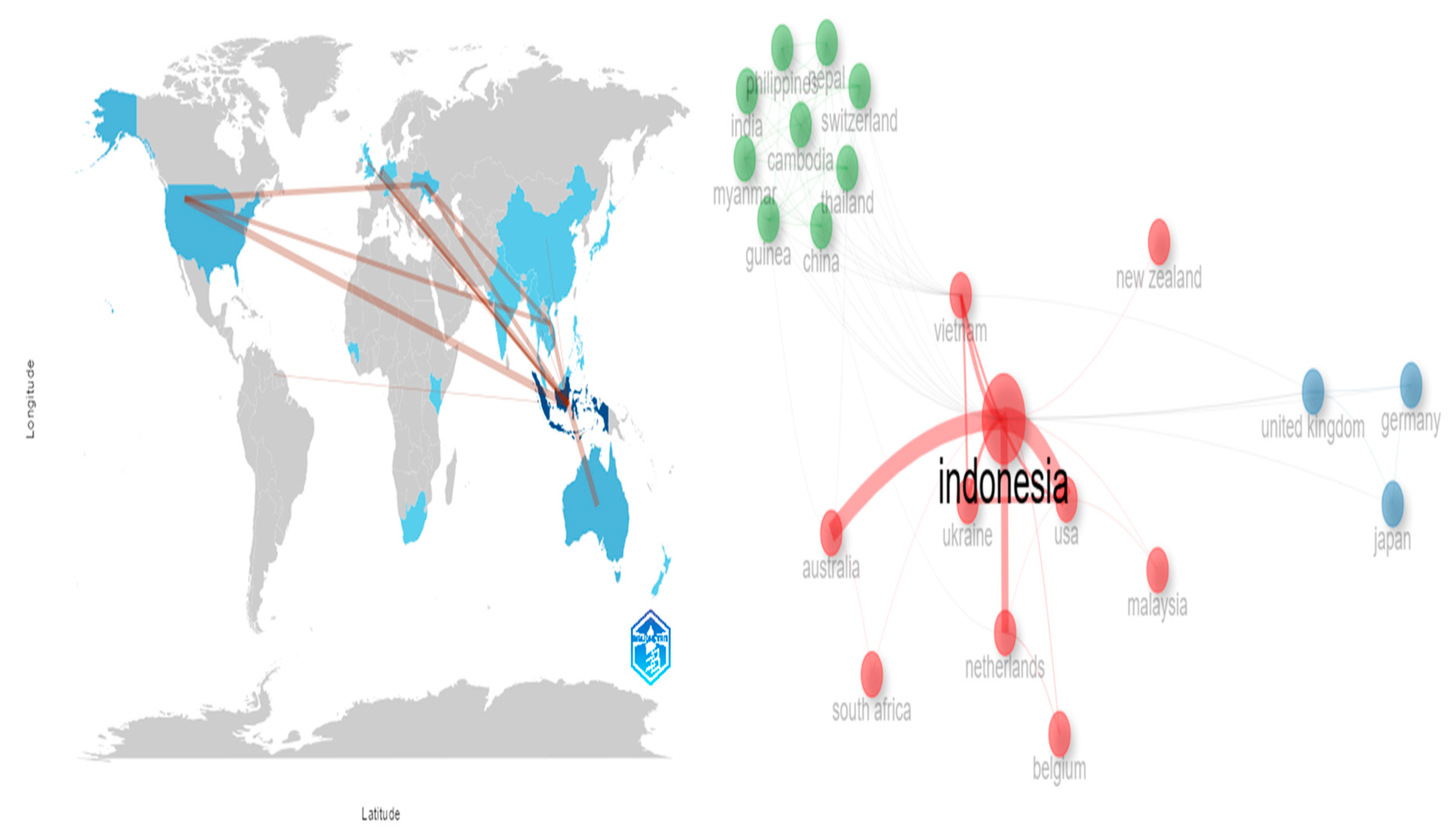
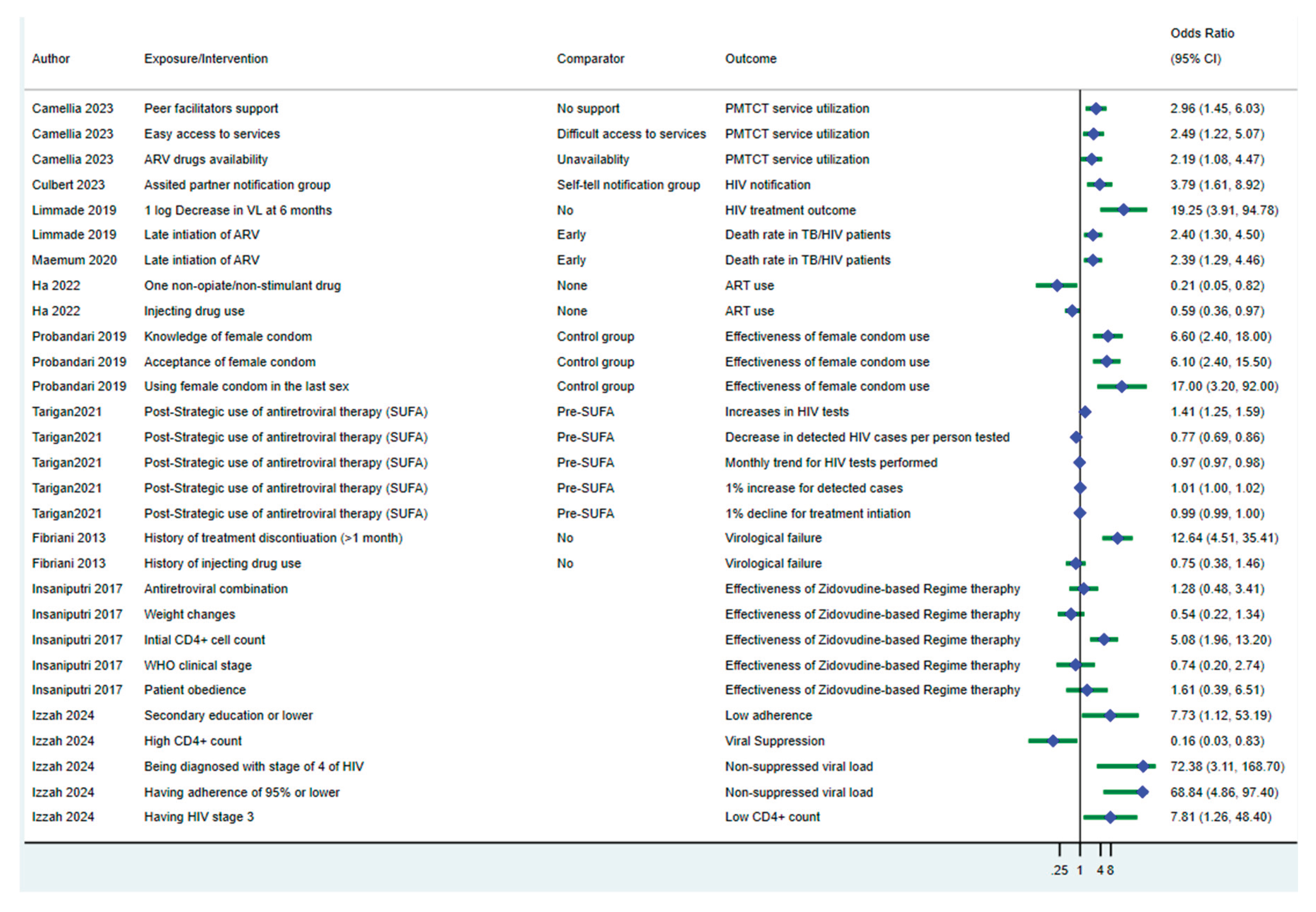
Results
Discussion
Conclusion
Acknowledgments
Funding Statement
Ethical Approval Statement
Patient Consent for Publication Statement
Conflicts of Interest Statement
Data Availability
Supplementary Information
References
- UNAIDS. Fact Sheet 2024: Global HIV Statitics. Switzerland: Joint United Nations Programme on HIV/AIDS. Available at: https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf; 2024.
- UNAIDS. UNAIDS DATA 2023. Switzerland: Joint United Nations Programme on HIV/AIDS. Available at: https://www.unaids.org/sites/default/files/media_asset/data-book-2023_en.pdf; 2024.
- Kementerian Kesehatan, R.I. Laporan Situasi Perkembangan HIV/AIDS dan PIMS Triwulan IV Tahun 2022. Indonesia: Kementerian Kesehatan Republik Indonesia; 2023.
- Kementerian Kesehatan, R.I. Laporan Perkembangan HIV/AIDS dan Penyakit Menular Seksual Tahun 2023. Indonesia:: Kementerian Kesehatan Republik Indonesia. Available at: file:///C:/Users/manek/Downloads/Rev_Laporan_Tahunan_dan_Triwulan_HIVPIMS_2023%20(3).pdf; 2024.
- Frescura, L.; Godfrey-Faussett, P.; Feizzadeh, A.A.; El-Sadr, W.; Syarif, O.; Ghys, P.D.; et al. Achieving the 95 95 95 targets for all: A pathway to ending AIDS. PLoS ONE 2022, 17, e0272405. [Google Scholar] [CrossRef] [PubMed]
- BPS. Jumlah Penduduk menurut Kelompok Umur dan Jenis Kelamin, Indonesia, 2022. Indonesia: Badan Pusat Statistik. Available at: https://sensus.bps.go.id/topik/tabular/sp2022/188/1/0; 2023.
- Wringe, A.; Renju, J.; Seeley, J.; Moshabela, M.; Skovdal, M. Bottlenecks to HIV care and treatment in sub-Saharan Africa: A multi-country qualitative study. Sexually Transmitted Infections 2017, 93, e053172. [Google Scholar] [CrossRef] [PubMed]
- Threats, M.; Brawner, B.M.; Montgomery, T.M.; Abrams, J.; Jemmott, L.S.; Crouch, P.C.; Freeborn, K.; Kamitani, E.; Enah, C. A Review of Recent HIV Prevention Interventions and Future Considerations for Nursing Science. The Journal of the Association of Nurses in AIDS Care JANAC 2021, 32, 373–391. [Google Scholar] [CrossRef] [PubMed]
- Mbuagbaw, L.; Hajizadeh, A.; Wang, A.; Mertz, D.; Lawson, D.O.; Smieja, M.; Benoit, A.C.; Alvarez, E.; Puchalski Ritchie, L.; Rachlis, B.; et al. Overview of systematic reviews on strategies to improve treatment initiation, adherence to antiretroviral therapy and retention in care for people living with HIV: Part 1. BMJ Open 2020, 10, e034793. [Google Scholar] [CrossRef] [PubMed]
- Deuba, K.; Sapkota, D.; Shrestha, U.; Shrestha, R.; Rawal, B.B.; Badal, K.; Baird, K.; Ekström, A.M. Effectiveness of interventions for changing HIV related risk behaviours among key populations in low-income setting: A Meta-Analysis, 2001–2016. Scientific Reports 2020, 10, 2197. [Google Scholar] [CrossRef] [PubMed]
- Manby, L.; Aicken, C.; Delgrange, M.; Bailey, J.V. Effectiveness of eHealth Interventions for HIV Prevention and Management in Sub-Saharan Africa: Systematic Review and Meta-analyses. AIDS and behavior 2022, 26, 457–469. [Google Scholar] [CrossRef] [PubMed]
- Moreno, R.; Nababan, H.Y.; Ota, E.; Wariki, W.M.V.; Ezoe, S.; Gilmour, S.; Shibuya, K. Structural and community-level interventions for increasing condom use to prevent the transmission of HIV and other sexually transmitted infections. Cochrane Database of Systematic Reviews 2014. [Google Scholar] [CrossRef] [PubMed]
- Culbert, G.J.; Williams, A.B. Cultural adaptation of a medication adherence intervention with prisoners living with HIV in Indonesia: A pragmatic approach to intervention development. Journal of the Association of Nurses in AIDS Care 2018, 29, 454–465. [Google Scholar] [CrossRef] [PubMed]
- Maemun, S.; Mariana, N.; Rusli, A.; Mahkota, R.; Bayu Purnama, T. Early Initiation of ARV Therapy Among TB–HIV Patients in Indonesia Prolongs Survival Rates! Journal of Epidemiology and Global Health 2020, 10, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Catrianiningsih, D.; Sanjaya, G.Y.; Chan, G.; Nababan, B.W.Y.; Triasih, R.; Intani, D.D.; Rahayu, E.S. Innovations in TB Screening and Preventive Therapy Services for PLHIV in Yogyakarta City, Indonesia. Tropical Medicine and Infectious Disease 2025, 10, 28. [Google Scholar] [CrossRef] [PubMed]
- Suryana, K.; Suharsono, H.; Sindhughosa, D. Co-trimoxazole preventive therapy reduces active pulmonary tuberculosis risk in people living with HIV/AIDS on antiretroviral at Wangaya hospital in Denpasar, Bali, Indonesia: A prospective cohort study. Asian Journal of Pharmaceutical and Clinical Research 2020. [Google Scholar] [CrossRef]
- Probandari, A.; Setyani, R.A.; Pamungkasari, E.P.; Widyaningsih, V.; Demartoto, A. Improving knowledge, acceptance, and utilization of female condoms among sex workers through a peer education: A mixed methods study in Surakarta Municipality, Central Java Province, Indonesia. Health Care for Women International 2020, 41, 600–618. [Google Scholar] [CrossRef] [PubMed]
- Camellia, A.; Swandari, P.; Irwanto, I.; Rahma, G.; Merati, T.P. Peer facilitators’s role to support pregnant women in utilizing HIV services during the COVID-19 pandemic. International Journal of Public Health Science 2023, 12, 377–384. [Google Scholar] [CrossRef]
- Herdiman; Lindayani, L. The effectiveness of motivational interviewing on HIV awareness and prevention behavior among adolescents in Bandung City, Indonesia: A randomized controlled trial. Malays. J. Med. Health Sci 2022, 18, 262–269. [Google Scholar]
- Ford, K.; Wirawan, D.N.; Fajans, P.; Meliawan, P.; MacDonald, K.; Thorpe, L. Behavioral interventions for reduction of sexually transmitted disease/HIV transmission among female commercial sex workers and clients in Bali, Indonesia. Aids 1996, 10, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Culbert, G.J.; Levy, J.A.; Steffen, A.D.; Waluyo, A.; Earnshaw, V.A.; Rahadi, A. Findings from a prison-based model of HIV assisted partner notification in Indonesia. 2023.
- Garg, P.R.; Uppal, L.; Mehra, S.; Mehra, D. Mobile health app for self-learning on HIV prevention knowledge and services among a young Indonesian key population: Cohort study. JMIR mHealth and uHealth 2020, 8, e17646. [Google Scholar] [CrossRef] [PubMed]
- Idrus, L.R.; Fitria, N.; Hasan, N.; Saidi, K.; Postma, M.; Alffenaar, J.-W.C. Usability Testing of IeHS (Integrated E-Healthcare Services) Web-Based Application in the Therapy Management of HIV and Tuberculosis in Indonesia: A Concurrent Nested Study Design. Available at SSRN 4488946. 2023.
- Mejia, C.; Wu, M.; Zhang, Y.; Kajikawa, Y. Exploring Topics in Bibliometric Research Through Citation Networks and Semantic Analysis. Frontiers in Research Metrics and Analytics 2021, 6. [Google Scholar] [CrossRef] [PubMed]
- Altarturi, H.H.M.; Saadoon, M.; Anuar, N.B. Cyber parental control: A bibliometric study. Children and Youth Services Review 2020, 116, 105134. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Montazeri, A.; Mohammadi, S.; Hesari, P.M.; Ghaemi, M.; Riazi, H.; Sheikhi-Mobarakeh, Z. Preliminary guideline for reporting bibliometric reviews of the biomedical literature (BIBLIO): A minimum requirements. Syst Rev 2023, 12, 239. [Google Scholar] [CrossRef] [PubMed]
- Koukopoulos, A.; Neimeyer, R.A. Prolonged grief disorder: A bibliometric analysis. Death studies 2024, 48, 150–163. [Google Scholar] [CrossRef] [PubMed]
- Aria, M.; Cuccurullo, C. bibliometrix: An R-tool for comprehensive science mapping analysis. Journal of Informetrics 2017, 11, 959–975. [Google Scholar] [CrossRef]
- Altarturi, H.H.M.; Nor, A.R.M.; Jaafar, N.I.; Anuar, N.B. A bibliometric and content analysis of technological advancement applications in agricultural e-commerce. Electronic Commerce Research 2023. [Google Scholar] [CrossRef]
- Thomas, J.; Harden, A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology 2008, 8, 45. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.C.; Hoffman, I.F.; Hanscom, B.S.; Ha, T.V.; Dumchev, K.; Djoerban, Z.; Rose, S.M.; Latkin, C.A.; Metzger, D.S.; Lancaster, K.E.; et al. A scalable, integrated intervention to engage people who inject drugs in HIV care and medication-assisted treatment (HPTN 074): A randomised, controlled phase 3 feasibility and efficacy study. Lancet 2018, 392, 747–759. [Google Scholar] [CrossRef] [PubMed]
- Ford, K.; Wirawan, D.N.; Reed, B.D.; Muliawan, P.; Wolfe, R. The Bali STD/AIDS Study: Evaluation of an intervention for sex workers. Sex Transm Dis 2002, 29, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Ali, R.; Chiamwongpae, S.; Isfandari, S.; Jirammakoon, S.; Mardiati, R.; Murauskiene, L.; Newcombe, D.; Subata, E.; Poznyak, V.; Uchtenhagen, A. the WHO collaborative study on substitution therapy of Opioid Dependence and HIV/AIDS. World Health Organization 2005.
- Hardiawan, D.; Juwita, M.N.; Vadra, J.; Prawiranegara, R.; Mambea, I.Y.; Wisaksana, R.; Handayani, M.; Subronto, Y.W.; Kusmayanti, N.A.; Januraga, P. Cost of improved test and treat strategies in Indonesia. AIDS 2023, 37, 1189–1201. [Google Scholar] [CrossRef] [PubMed]
- Nugroho, A.; Erasmus, V.; Krier, S.E.; Reviagana, K.P.; Laksmono, P.A.; Widihastuti, A.; Richardus, J.H. Client perspectives on an outreach approach for HIV prevention targeting Indonesian MSM and transwomen. Health Promotion International 2020, 35, 916–924. [Google Scholar] [CrossRef] [PubMed]
- Putri, W.; Ulandari, L.P.S.; Valerie, I.C.; Prabowo, B.R.; Hardiawan, D.; Sihaloho, E.D.; Relaksana, R.; Wardhani, B.D.K.; Harjana, N.P.A.; Nugrahani, N.W.; et al. Costs and scale-up costs of community-based Oral HIV Self-Testing for female sex workers and men who have sex with men in Jakarta and Bali, Indonesia. BMC Health Serv Res 2024, 24, 114. [Google Scholar] [CrossRef] [PubMed]
- Siregar, A.Y.M.; Juwita, M.N.; Hardiawan, D.; Akbar, A.; Rachman, Z.H.; Haekal, M.D.F.; Marwah, Y.S.; Putri, T.A.; Rakhmat, F.F.; Pohan, M.N.; et al. Cost of implementing HIV pre-exposure prophylaxis at community-based clinics in Indonesia. Trop Med Int Health 2024, 29, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Subronto, Y.W.; Kusmayanti, N.A.; Januraga, P.P.; Dewa Wirawan, L.N.; Wisaksana, R.; Sukmaningrum, E.; Kawi, N.H.; Iskandar, S.; Mulyani, T.; Sulaiman, N.; et al. Simplified clinical algorithm for immediate antiretroviral therapy initiation: The HATI [HIV awal (early) Test & Treat in Indonesia] implementation research in Indonesia. Indian J Med Res 2022, 156, 729–741. [Google Scholar] [CrossRef] [PubMed]
- Sukmaningrum, E.; Ayu, A.P.; Wongso, L.V.; Handayani, M.; Hendrianti, S.; Kawi, N.H.; Kusmayanti, N.A.; Sulaiman, N.; Irwanto, I.; Law, M.; et al. Motivational Interviewing as an Intervention to Improve Antiretroviral Treatment Initiation Among People who Inject Drugs (PWID): A Pilot Study in Jakarta and Bandung, Indonesia. Current Drug Research Reviews 2024, 16, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Tarigan, Y.N.; Woodman, R.J.; Miller, E.R.; Wisaksana, R.; Ward, P.R. Impact of strategic use of antiretroviral therapy intervention to the HIV continuum of care in 13 cities in Indonesia: An interrupted time series analysis. AIDS Res Ther 2021, 18, 22. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.C.; Praptoraharjo, I.; Muryani, N.; Soeselo, D.A.; Ghosh, S.; Levy, J.A. Introduction of Voluntary Medical Male Circumcision for HIV Prevention in Tanah Papua, Indonesia. AIDS and Behavior 2025. [Google Scholar] [CrossRef] [PubMed]
- Diarsvitri, W.; Utomo, I. The importance of reproductive health and HIV/AIDS education program for young people in Papua and West Papua Provinces, Indonesia 2011.
- Hidayat, R.; Marguari, D.; Hairunisa, N.; Suparno, H.; Magnani, R. Community HIV Screening Among MSM in Three Indonesian Cities. Curr HIV Res 2019, 17, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Amanah, A.; Komala, I.; Kurniasari, M.D.; Dharmana, E.; Gasem, M.H. Effect of Mangosteen (Garcinia mangostana) PEEL Extract towards CD4+, CD8+ T LYMPHOCYTES, CD38 Expression, NK Cells, IL-2 and IFNγ in Hiv Patients with Antiretroviral Therapy. Hiroshima Journal of Medical Sciences 2018, 67, 56–62. [Google Scholar]
- Middlestadt, S.E. Encouraging discussion with partners and building negotiation skills: HIV prevention strategies for women in relationships in Brazil, Tanzania and Indonesia. Advances in consumer research. Association for Consumer Research (U.S.) 1993, 20, 297–301. [Google Scholar] [PubMed]
- Merati, T.P. Condom distribution in Bali: Assuring supply meets demand. AIDSlink Eastern Central Southern Africa 1994, 7. [Google Scholar]
- Gani, R.A.; Yunihastuti, E.; Krisnuhoni, E.; Saraswati, H.; Djauzi, S.; Lesmana, L.A.; Lee, S.; Price, P. Periportal CD4+ Cell Infiltration Increases in HIV/Hepatitis C Virus-Coinfected Patients Commencing ART, Whereas CD8+ Cells Clear From the Liver. Journal of Infectious Diseases 2014, 210, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Asturiningtyas, I.P.; Subronto, Y.W.; Kusmayanti, N.A. Nutritional status and other predictors of immune response recovery among HIV-AIDS patients receiving antiretroviral therapy in Dr. Sardjito Hospital, Yogyakarta, Indonesia: A retrospective cohort study. Malaysian Journal of Nutrition 2020, 26, 441–452. [Google Scholar] [CrossRef]
- Damayanti, N. Analysis of First-Line Antiretroviral Therapy toward Patients with HIV/AIDS in Indonesia. Journal of Pharmaceutical Sciences and Research 2020, 12, 730–733. [Google Scholar]
- Limmade, Y.; Fransisca, L.; Rodriguez-Fernandez, R.; Bangs, M.J.; Rothe, C. HIV treatment outcomes following antiretroviral therapy initiation and monitoring: A workplace program in Papua, Indonesia. PLoS ONE 2019, 14, e0212432. [Google Scholar] [CrossRef] [PubMed]
- Pangarungan, M.; Arguni, E. Immunological outcomes after six months with first line antiretroviral therapy: A lesson from Yogyakarta, Indonesia. The Journal of Infection in Developing Countries 2018, 12, 385–389. [Google Scholar] [CrossRef] [PubMed]
- Zeziulin, O.; Mollan, K.R.; Shook-Sa, B.E.; Hanscom, B.; Lancaster, K.E.; Dumchev, K.; Go, V.F.; Chu, V.A.; Kiriazova, T.; Syarif, Z.; et al. Depressive symptoms and use of HIV care and medication-assisted treatment among people with HIV who inject drugs. Aids 2021, 35, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Fibriani, A.; Wisaksana, R.; Indrati, A.; Hartantri, Y.; van de Vijver, D.; Schutten, M.; Alisjahbana, B.; Sudjana, P.; Boucher, C.A.; van Crevel, R.; et al. Virological failure and drug resistance during first line anti-retroviral treatment in Indonesia. J Med Virol 2013, 85, 1394–1401. [Google Scholar] [CrossRef] [PubMed]
- Insaniputri, P.; Supardi, S.; Andrajati, R. Comparison of zidovudine combination and tenofovir combination on the effectiveness of therapy and side effects in HIV/AIDS patients in rsal mintohardjo. Asian Journal of Pharmaceutical and Clinical Research 2017, 10, 93. [Google Scholar] [CrossRef]
- Izzah, Z.; Suprapti, B.; Asmarawati, T.P.; Åberg, C.; Touw, D.J. Antiretroviral adherence and treatment outcomes among patients living with HIV at an Indonesian HIV clinic: A cross-sectional study. Pharmacy Practice 2024, 22, 2898. [Google Scholar]
- Lancaster, K.E.; Mollan, K.R.; Hanscom, B.S.; Shook-Sa, B.E.; Ha, T.V.; Dumchev, K.; Djoerban, Z.; Rose, S.M.; Latkin, C.A.; Metzger, D.S.; et al. Engaging People Who Inject Drugs Living With HIV in Antiretroviral Treatment and Medication for Opioid Use Disorder: Extended Follow-up of HIV Prevention Trials Network (HPTN) 074. Open Forum Infectious Diseases 2021, 8, ofab281. [Google Scholar] [CrossRef] [PubMed]
- Tanaskovic, S.; Fernandez, S.; Saraswati, H.; Yunihastuti, E.; Gani, R.A.; Djauzi, S.; Price, P. Naive and Memory CD4⁺ T Cells Are Differentially Affected in Indonesian HIV Patients Responding to ART. Viral immunology 2016, 29, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Yuneti, O.N.; Sawitri, A.A.S.; Wulandari, L.P.L.; Muliawan, P.; Widyanthini, D.N.; Kathy, P.K.; Amin, J.; Mathers, B.; Kaldor, J.; Merati, T.; et al. P16.18 Influence of baseline characteristics on the increase cd4 >350 cells/mm3 among HIV/AIDS patients receiving antiretroviral therapy in indonesia. Sexually Transmitted Infections 2015, 91, A218. [Google Scholar] [CrossRef]
- Palumbo, P.J.; Zhang, Y.; Fogel, J.M.; Guo, X.; Clarke, W.; Breaud, A.; Richardson, P.; Piwowar-Manning, E.; Hart, S.; Hamilton, E.L. HIV drug resistance in persons who inject drugs enrolled in an HIV prevention trial in Indonesia, Ukraine, and Vietnam: HPTN 074. PLoS ONE 2019, 14, e0223829. [Google Scholar] [CrossRef] [PubMed]
- Suryana, K. The Impact of Universal Test and Treat Program on Highly Active Anti Retroviral Therapy Outcomes (Coverage, Adherence and Lost to Follow Up) at Wangaya Hospital in Denpasar, Bali-Indonesia: A Retrospective Cohort Study. The Open AIDS Journal 2021, 15, 28–34. [Google Scholar] [CrossRef]
- Ramdan, R.; Winata, B. The effect of a modified alarm medicine box in HIV patients undergoing antiretroviral therapy. HIV & AIDS Review 2018, 17. [Google Scholar] [CrossRef]
- Gedela, K.; Rajus, N.; Luis, H.; Fridayantara, W.D.; Irwanto, I.; Sukmaningrum, E.; Wignall, F.S. Antiretroviral drug switches to zidovudine-based regimens and loss to follow-up during the first COVID-19 lockdown in Bali, Indonesia. HIV Medicine 2022, 23, 1025–1030. [Google Scholar] [CrossRef] [PubMed]
- Hoke, T.; Bateganya, M.; Toyo, O.; Francis, C.; Shrestha, B.; Philakone, P.; Pandey, S.R.; Persaud, N.; Cassell, M.M.; Wilcher, R. How home delivery of antiretroviral drugs ensured uninterrupted HIV treatment during COVID-19: Experiences from Indonesia, Laos, Nepal, and Nigeria. Global Health Science and Practice 2021, 9, 978–989. [Google Scholar] [CrossRef] [PubMed]
- Ariyanto, I.A.; Estiasari, R.; Karim, B.; Wijaya, I.P.; Bela, B.; Soebandrio, A.; Price, P.; Lee, S. Which NK cell populations mark the high burden of CMV present in all HIV patients beginning ART in Indonesia? AIDS Research & Therapy 2022, 19, 1–10. [Google Scholar] [CrossRef]
- Wijaya, I.P.; Karim, B.; Azizi, M.S.; Ariyanto, I.; Mansjoer, A.; Yunihastuti, E.; Harimurti, K.; Alwi, I.; Lee, S.; Price, P. Cytomegalovirus may influence vascular endothelial health in Indonesian HIV-infected patients after 5 years on ART. AIDS Research & Therapy 2021, 18, 1–7. [Google Scholar] [CrossRef]
- Yunihastuti, E.; Rusdi, L.; Syahrir Azizi, M.; Estiasari, R.; Jasirwan, C.O.M.; Wulandari, E.A.T.; Purnamasari, D.; Shinta Noviar, M.; Aman Nasution, S. Effect of atorvastatin on subclinical atherosclerosis in virally-suppressed HIV-infected patients with CMV seropositivity: A randomized double-blind placebo-controlled trial. F1000Res 2021, 10, 151. [Google Scholar] [CrossRef] [PubMed]
- Go, V.F.; Hershow, R.B.; Kiriazova, T.; Sarasvita, R.; Bui, Q.; Latkin, C.A.; Rose, S.; Hamilton, E.; Lancaster, K.E.; Metzger, D.; et al. Client and Provider Perspectives on Antiretroviral Treatment Uptake and Adherence Among People Who Inject Drugs in Indonesia, Ukraine and Vietnam: HPTN 074. AIDS Behavior 2019, 23, 1084–1093. [Google Scholar] [CrossRef] [PubMed]
- Kiriazova, T.; Go, V.F.; Hershow, R.B.; Hamilton, E.L.; Sarasvita, R.; Bui, Q.; Lancaster, K.E.; Dumchev, K.; Hoffman, I.F.; Miller, W.C.; et al. Perspectives of clients and providers on factors influencing opioid agonist treatment uptake among HIV-positive people who use drugs in Indonesia, Ukraine, and Vietnam: HPTN 074 study. Harm Reduct J 2020, 17, 69. [Google Scholar] [CrossRef] [PubMed]
- Lancaster, K.E.; Miller, W.C.; Kiriazova, T.; Sarasvita, R.; Bui, Q.; Ha, T.V.; Dumchev, K.; Susami, H.; Hamilton, E.L.; Rose, S.; et al. Designing an Individually Tailored Multilevel Intervention to Increase Engagement in HIV and Substance Use Treatment Among People Who Inject Drugs With HIV: HPTN 074. AIDS education and prevention 2019, 31, 95–110. [Google Scholar] [CrossRef] [PubMed]
- Achmad, Y.M.; Istiqomah, A.N.; Iskandar, S.; Wisaksana, R.; van Crevel, R.; Hidayat, T. Integration of methadone maintenance treatment and HIV care for injecting drug users: A cohort study in Bandung, Indonesia. Acta Med Indones 2009, 41, 23–27. [Google Scholar] [PubMed]
- Afriandi, I.; Siregar, A.Y.; Meheus, F.; Hidayat, T.; van der Ven, A.; van Crevel, R.; Baltussen, R. Costs of hospital-based methadone maintenance treatment in HIV/AIDS control among injecting drug users in Indonesia. Health Policy 2010, 95, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Wammes, J.J.; Siregar, A.Y.; Hidayat, T.; Raya, R.P.; van Crevel, R.; van der Ven, A.J.; Baltussen, R. Cost-effectiveness of methadone maintenance therapy as HIV prevention in an Indonesian high-prevalence setting: A mathematical modeling study. Int J Drug Policy 2012, 23, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Ha, T.V.; Hoffman, I.F.; Miller, W.C.; Mollan, K.R.; Lancaster, K.E.; Richardson, P.; Zeziulin, O.; Djoerban, Z.; Sripaipan, T.; Chu, V.A.; et al. Association between drug use and ART use among people living with HIV who inject drugs in Vietnam, Ukraine and Indonesia: Results from HPTN 074. Journal of Substance Use 2022, 27, 648–657. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.C.; Lancaster, K.E.; Metzger, D.S.; Dvoriak, S.; Mollan, K.R.; Reifeis, S.A.; Hudgens, M.G.; Piwowar-Manning, E.M.; Richardson, P.; Eshleman, S.H.; et al. A scalable, integrated intervention to engage people who inject drugs in HIV care and medication-assisted treatment (HPTN 074): A randomised, controlled phase 3 feasibility and efficacy study. Lancet 2018, 392, 747–759. [Google Scholar] [CrossRef] [PubMed]
- Sugarman, J.; Trumble, I.; Hamilton, E.; Sarasvita, R.; Dumchev, K.; Viet, H.; Hoffman, I.; Miller, W.; Hanscom, B. Reported Participation Benefits in International HIV Prevention Research with People Who Inject Drugs. Ethics & human research 2019, 41, 28–34. [Google Scholar] [CrossRef]
- Tingginehe, R.; Makaba, S. Effect of sago caterpillar (Rhyncophorus bilinetaus var papuanus) oil extract against lymphocyte, leukocyte, and cd4 levels of human immunodeficiency virus patients in papua, indonesia. Asian Journal of Pharmaceutical and Clinical Research 2018, 11, 494. [Google Scholar] [CrossRef]
- Siregar, A.Y.; Komarudin, D.; Wisaksana, R.; van Crevel, R.; Baltussen, R. Costs and outcomes of VCT delivery models in the context of scaling up services in Indonesia. Trop Med Int Health 2011, 16, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Wulandari, L.P.L.; Kaldor, J.; Guy, R. Uptake and acceptability of assisted and unassisted HIV self-testing among men who purchase sex in brothels in Indonesia: A pilot intervention study. BMC Public Health 2020, 20, 730. [Google Scholar] [CrossRef] [PubMed]
- Widyanthini, D.N.; Januraga, P.P.; Wisaksana, R.; Subronto, Y.W.; Sukmaningrum, E.; Kusmayanti, N.A.; Dewi, H.; Law, M.; Kaldor, J.M.; Wirawan, D.N. HIV self-testing for men who have sex with men: An implementation trial in Indonesia. AIDS Care 2022, 34, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Sawitri, A.A.S.; Sutarsa, I.N.; Merati, K.T.P.; Bakta, I.M.; Wirawan, D.N. Why Counseling Intervention Fails to Improve Compliance towards Antiretroviral Therapy: Findings from a Mixed-Methods Study among People Living with HIV in Bali Province, Indonesia. Infect Dis Rep 2021, 13, 136–147. [Google Scholar] [CrossRef] [PubMed]
- Nelwan, E.J.; Isa, A.; Alisjahbana, B.; Triani, N.; Djamaris, I.; Djaja, I.; Pohan, H.T.; Zwanikken, P.; Crevel, R.v.; van der Ven, A.; et al. Routine or targeted HIV screening of Indonesian prisoners. International Journal of Prisoner Health 2016, 12, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Wongso, L.V.; Rahadi, A.; Sukmaningrum, E.; Handayani, M.; Wisaksana, R. Acceptability of a pilot motivational interviewing intervention at public health facilities to improve the HIV treatment cascade among people who inject drugs in Indonesia. Harm Reduct J 2024, 21, 73. [Google Scholar] [CrossRef] [PubMed]
- Marhaeni, G.; Surati, I.; Armini, N.W.; Suiraoka, I.P. Youth Resilience Capabilities Avoid Free Sex, HIVAIDS and Drugs based on Sekaa Teruna. Indian Journal of Public Health Research Development 2018, 11, 435–440. [Google Scholar] [CrossRef]
- Surilena; Ismail, R.; Irwanto, I.; Djoerban, Z.; Utomo, B.; Sabarinah, S.; Iwan; Akip, A. The Effect of Rational Emotive Behavior Therapy (REBT) on Antiretroviral Therapeutic Adherence and Mental Health in Women Infected with HIV/AIDS. Acta medica Indonesiana 2014, 46, 283–291. [Google Scholar] [PubMed]
- Fauzi, A.; Anggraini, N.; Fatkhurohman, N. Self-management: A comprehensive approach to improve quality of life among people living with HIV in Indonesia. Belitung Nursing Journal 2021, 7, 395. [Google Scholar] [CrossRef] [PubMed]
- Nurmalia. Efektivitas intervensi media audio visual aku bangga aku tahu dalam pencegahan penularan HIV-AIDS pada remaja. HEALTHY: Jurnal Inovasi Riset Ilmu Kesehatan 2022, 1, 158–165. [Google Scholar] [CrossRef]
- Saputri, T.; Lilia, D. Peningkatan Pengetahuan Tentang Bahaya HIV/AIDS Setelah Intervensi Media Audio Visual. Media Informasi 2024. [Google Scholar] [CrossRef]
- Widyasari, R.; Besral, B.; Widiastuti, S.; Siauta, J.A. PENINGKATAN PENGETAHUAN REMAJA TENTANG BAHAYA HIV/AIDS SETELAH INTERVENSI MEDIA AUDIO VISUAL DI SMPN 21 BANDAR LAMPUNG. NUSANTARA Jurnal Ilmu Pengetahuan Sosial 2021, 8. [Google Scholar] [CrossRef]
- Asrina, A.; Ikhtiar, M.; Idris, F.P. Intervensi Media Promosi Kesehatan Terhadap Perubahan Sikap Anggota OSIS mengenai Pencegahan HIV AIDS. Jurnal Keperawatan 2022, 14, 703–708. [Google Scholar]
- Ismail, R.; Yona, S.; Nurachmah, E.; Khariroh, S.; Sujianto, U.; Santoso, W.; Bangun, S.A.; Voss, J.G. Feasibility of Lantern Using WhatsApp to Improve Antiretroviral Therapy Adherence. CIN: Computers, Informatics, Nursing 2023, 41, 915–920. [Google Scholar] [CrossRef] [PubMed]
- Rositasari, D.V.; Wardani, E.M.; Rohmawati, R.; Hidaayah, N. Analysis of the application of «My therapy application» to the compliance of drinking (ARV) in HIV/AIDS people in Kompeda, Surabaya. Journal Infectology 2024, 15, 125–130. [Google Scholar] [CrossRef]
- Suyono, T.A.; Prasetyo, P.; Shafira, E.; Tanjung, F.; Syazwani, F.; Yudiana, W. Apakah intervensi prasangka lewat media bisa mengurangi prasangka implisit terhadap orang dengan HIV/AIDS? Eksperimen menggunakan Implicit Association Test (IAT). Jurnal Psikologi Sosial 2020, 18, 131–144. [Google Scholar] [CrossRef]
- Lindayani, L. The Effectiveness of Skills for Adolescents with Healthy Sexuality (SAHS) Program on Reducing the Risk of HIV Transmission among Adolescents. Indonesian Nursing Journal of Education & Clinic (INJEC) 2018, 3, 1–8. [Google Scholar]
- Nelwan, E.J.; Indrati, A.K.; Isa, A.; Triani, N.; Alam, N.N.; Herlan, M.S.; Husen, W.; Pohan, H.T.; Alisjahbana, B.; Meheus, A. Effect of HIV prevention and treatment program on HIV and HCV transmission and HIV mortality at an Indonesian narcotic prison. Southeast Asian J Trop Med Public Health 2015, 46, 880–891. [Google Scholar] [PubMed]
- Ford, K.; Wirawan, D.N.; Reed, B.D.; Muliawan, P.; Wolfe, R. The Bali STD/AIDS Study: Evaluation of an intervention for sex workers. Sexually transmitted diseases 2002, 29, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Ford, K.; Wirawan, D.N.; Fajans, P. Factors related to condom use among four groups of female sex workers in Bali, Indonesia. AIDS education and prevention: Official publication of the International Society for AIDS Education 1998, 10, 34–45. [Google Scholar] [PubMed]
- Chua, A.C.; Leo, Y.S.; Lee, C.C. Building partnerships to address the HIV epidemic. Singapore Med J 2008, 49, 376–379. [Google Scholar] [PubMed]
- Lancaster, K.E.; Hoffman, I.F.; Hanscom, B.; Ha, T.V.; Dumchev, K.; Susami, H.; Rose, S.; Go, V.F.; Reifeis, S.A.; Mollan, K.R. Regional differences between people who inject drugs in an HIV prevention trial integrating treatment and prevention (HPTN 074): A baseline analysis. Journal of the International AIDS Society 2018, 21, e25195. [Google Scholar] [CrossRef] [PubMed]
- Purnamawati, D.; Djuwita, R.; Siregar, K.; Kamso, S.; Utomo, B.; Pratomo, H.; Muhaimin, T. Improving access to PMTCT services via a novel implementation model: Organizational support, health education, and HIV testing at the community level of West Java, Indonesia. International Journal of Health Promotion & Education 2020, 58, 282–292. [Google Scholar] [CrossRef]
- Badriah, F.; Tahangnacca, M.; Alkaff, R.; Takeru, A.; Hanifah, L. Implementation of Program for the Prevention of Mother-to-Child Transmission of HIV in South Jakarta. Kesmas: National Public Health Journal 2018, 12, 159–164. [Google Scholar] [CrossRef]
- Hardon, A.P.; Oosterhoff, P.; Imelda, J.D.; Anh, N.T.; Hidayana, I. Preventing mother-to-child transmission of HIV in Vietnam and Indonesia: Diverging care dynamics. Social science & medicine (1982) 2009, 69, 838–845. [Google Scholar] [CrossRef]
- Hegarty, B.; Nanwani, S.; Praptoraharjo, I. Understanding the challenges faced in community-based outreach programs aimed at men who have sex with men in urban Indonesia. Sexual Health 2020, 17, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Utami, N.W. Effect of Group Education (Simulation Model) on Information Disclosure and HIV/AIDS Transmission Prevention for HIV/AIDS Risk Groups. Medico-Legal Update 2019, 19, 184–187. [Google Scholar] [CrossRef]
- Darmawansyah; Arifin, M.A.; Abadi, M.Y.; Fajrin, M.A.; Mallongi, A. Decentralization Implementation of HIV/Aids Programs in the Province of South Sulawesi. Medico-Legal Update 2020, 20, 1126–1130. [Google Scholar] [CrossRef]
- Vadra, J.; Komarudin, D.; Prawiranegara, R.; Lestari, M.; Wisaksana, R.; Siregar, A.Y.M. The cost of providing hospital-based (early) antiretroviral treatment in Indonesia: What has changed in almost a decade? AIDS Care 2023, 35, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Verstraaten, E.J.M.; Beeren, F.M.M.; Janssen, J.L.C.; Kemper, S.; Siregar, A.Y.M.; Tromp, N.; Baltussen, R. Comparative Cost Analysis of Four Interventions to Prevent HIV Transmission in Bandung, Indonesia. Acta Med Indones 2017, 49, 236–242. [Google Scholar] [PubMed]
- de Bresser, I.; Remers, T.E.; Wieland, M.W.; Prawiranegara, R.; Siregar, A.Y.; Baltussen, R. Prioritizing HIV/AIDS prevention strategies in Bandung, Indonesia: A cost analysis of three different HIV/AIDS interventions. PLoS ONE 2019, 14, e0221078. [Google Scholar] [CrossRef] [PubMed]
- Tromp, N.; Prawiranegara, R.; Siregar, A.; Wisaksana, R.; Pinxten, L.; Pinxten, J.; Lesmana Putra, A.; Kurnia Sunjaya, D.; Jansen, M.; Hontelez, J.; et al. Translating international HIV treatment guidelines into local priorities in Indonesia. Trop Med Int Health 2018, 23, 279–294. [Google Scholar] [CrossRef] [PubMed]
- Pinxten, W.; Ia, T.; Hospers, H.; Alisjahbana, B.; Meheus, A. IMPACT-Bandung: A learning organization approach to build HIV prevention and care in Indonesia. Procedia-Social and Behavioral Sciences 2011, 15, 623–627. [Google Scholar] [CrossRef]
- Coulthard, P.; Tappuni, A.R.; Ranauta, A. Oral health and HIV: What dental students need to know. Oral Diseases 2020, 26, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Newland, J.; Lestari, D.; Poedjanadi, M.N.; Kelly-Hanku, A. Co-locating art and health: Engaging civil society to create an enabling environment to respond to HIV in Indonesia. Sexual health 2021, 18, 84–94. [Google Scholar] [CrossRef] [PubMed]
- Ford, K.; Wirawan, D.N.; Suastina, S.S.; Reed, B.D.; Muliawan, P. Evaluation of a peer education programme for female sex workers in Bali, Indonesia. Int J STD AIDS 2000, 11, 731–733. [Google Scholar] [CrossRef] [PubMed]
- Alim, A.; Maulana, D.; Adam, A.; Thamrin, M.H. The influence of the HIV/AIDS program on the knowledge and attitudes of the labourer in the building construction project of the Faculty of Engineering, University of Hasanuddin, Indonesia. European Journal of Molecular & Clinical Medicine 2021, 8, 2021. [Google Scholar]
- Fauk, N.K.; Lau, F.; Fernandez, G.M.B.; Tetik, F.S.; Seran, D. HIV/AIDS, PMS dan Masyarakat Kita; Gita Kasih: Kupang, Indonesia, 2014. [Google Scholar]
- Fauk, N.K. Risk factors and the impact of HIV among women living with HIV and their families in Yogyakarta and Belu district, Indonesia. Flinders University, Australia, 2022.
- Baker, R.W. Indonesia In Crisis. Singore: The Institute of Southeast Asian Studies. Available at: https://www.files.ethz.ch/isn/28415/api036.pdf; 1998.
- Tarmidi, L.T. Kiris moneter Indonesia: Sebab, dampak, peran IMF dan saran. Buletin Ekonomi Moneter dan Perbankan 1999, 1, 1–25. [Google Scholar] [CrossRef]
- Hotchkiss, D.R.; Jacobalis, S. Indonesian heath care and the economic crisis: Is managed care the needed reform? Health Policy 1999, 46, 195–216. [Google Scholar] [CrossRef] [PubMed]
- Utomo, B. Health Status in Indonesia During the Economic Crisis. In The Indonesia Crisis: A Human Development Perspective; Ananta, A., Ed.; Institute of Southeast Asian Studies: Singapore, 2003. [Google Scholar]
- Purdey, J. Kekerasan Anti-Tionghoa di Indonesia, 1996–1999; University of Hawaii Press: Honolulu, 2006. [Google Scholar]
- Bain-Brickley, D.; Butler, L.M.; Kennedy, G.E.; Rutherford, G.W. Interventions to improve adherence to antiretroviral therapy in children with HIV infection. Cochrane Database of Systematic Reviews 2011, 1–34. [Google Scholar] [CrossRef] [PubMed]
- Hosek, S.; Pettifor, A. HIV Prevention Interventions for Adolescents. Current HIV/AIDS reports 2019, 16, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Ward, P.R.; Puspitasari, R.; Rose, A.; Gebremariyam, B.S.; Fauk, N.K. Understanding HIV-Related Mental Health Challenges and Contributing Factors Among Indonesian Adolescents Living with HIV. Int J Environ Res Public Health 2025, 22. [Google Scholar] [CrossRef] [PubMed]
- Fauk, N.K.; Hawke, K.; Mwanri, L.; Ward, P.R. Stigma and Discrimination towards People Living with HIV in the Context of Families, Communities, and Healthcare Settings: A Qualitative Study in Indonesia. International Journal of Environmental Research and Public Health 2021, 18, 5424. [Google Scholar] [CrossRef] [PubMed]
- Fauk, N.K.; Ward, P.R.; Hawke, K.; Mwanr, L. HIV Stigma and Discrimination: Perspectives and Personal Experiences of Healthcare Providers in Yogyakarta and Belu, Indonesia. Frontiers in Medicine 2021, 8, 625. [Google Scholar] [CrossRef] [PubMed]
- Mahamboro, D.B.; Fauk, N.K.; Ward, P.R.; Merry, M.S.; Siri, T.A.; Mwanri, L. HIV Stigma and Moral Judgement: Qualitative Exploration of the Experiences of HIV Stigma and Discrimination among Married Men Living with HIV in Yogyakarta. Int J Environ Res Public Health 2020, 17, 636. [Google Scholar] [CrossRef] [PubMed]
- Fauk, N.K.; Ward, P.R.; Hawke, K.; Mwanri, L. Cultural and religious determinants of HIV transmission: A qualitative study with people living with HIV in Belu and Yogyakarta, Indonesia. PLoS ONE 2021, 16, e0257906. [Google Scholar] [CrossRef] [PubMed]
- Fauk, N.K.; Kustanti, C.Y.; Wulandari, R.; Damayani, A.D.; Mwanri, L. Societal determinants of HIV vulnerability among clients of female commercial sex workers in Indonesia. PLoS ONE 2018, 13, e0207647. [Google Scholar] [CrossRef] [PubMed]
- Fauk, N.K.; Merry, M.S.; Putra, S.; Sigilipoe, M.A.; Crutzen, R.; Mwanri, L. Perceptions among transgender women of factors associated with the access to HIV/AIDS-related health services in Yogyakarta, Indonesia. PLoS ONE 2019, 14, e0221013. [Google Scholar]
- Fauk, N.K.; Merry, M.S.; Siri, T.A.; Mwanri, L.; Ward, P.R. Structural, Personal and Socioenvironmental Determinants of HIV Transmission among Transgender Women in Indonesia. International Journal of Environmental Research and Public Health 2021, 18, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Pisani, E.; Girault, P.; Gultom, M.; Sukartini, N.; Kumalawati, J.; Jazan, S.; Donegan, E. HIV, syphilis infection, and sexual practices among transgenders, male sex workers, and other men who have sex with men in Jakarta, Indonesia. Sexually Transmitted Infections 2004, 80, 536–540. [Google Scholar] [CrossRef] [PubMed]
- Kendall, M.; Razali, K. Sex Wotk and HIV, Indonesia. USA: UNAIDS. Available at: https://new.aidsdatahub.org/sites/default/files/resource/sex-work-hiv-indonesia.pdf; 2016.
- Fauk, N.K.; Merry, M.S.; Mwanri, L.; Hawke, K.; Ward, P.R. Mental Health Challenges and the Associated Factors in Women Living with HIV Who Have Children Living with HIV in Indonesia: A Qualitative Study. Int J Environ Res.Public Health 2022, 19, 6879. [Google Scholar] [CrossRef] [PubMed]
- Fauk, N.K.; Mwanri, L.; Hawke, K.; Mohammadi, L.; Ward, P.R. Psychological and Social Impact of HIV on Women Living with HIV and Their Families in Low- and Middle-Income Asian Countries: A Systematic Search and Critical Review. Int J Environ Res Public Health 2022, 19, 6668. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Ma, S.; Dang, B.; Shi, H.; Wei, Y.; Wang, X. Effectiveness of telemedicine for the prevention of mother-to-child transmission of HIV in low-income and middle-income countries: A systematic review and meta-analysis. International journal of infectious diseases 2024, 143, 106981. [Google Scholar] [CrossRef] [PubMed]
- Tudor Car, L.; Van Velthoven, M.H.M.M.T.; Brusamento, S.; Elmoniry, H.; Car, J.; Majeed, A.; Tugwell, P.; Welch, V.; Marusic, A.; Atun, R. Integrating Prevention of Mother-to-Child HIV Transmission Programs to Improve Uptake: A Systematic Review. PLoS ONE 2012, 7, e35268. [Google Scholar] [CrossRef] [PubMed]
- BPS. Jumlah Kabupaten, 2002-2004. Jakarta, Indonesia: Badan Pusat Statistik. Avaiilable at: https://www.bps.go.id/id/statistics-table/2/MTU0IzI=/jumlah-kabupaten.html; 2024.
- Fauk, N.K.; Gesesew, H.A.; Seran, A.L.; Ward, P.R. Barriers to access to antiretroviral therapy by people living with HIV in an indonesian remote district during the COVID-19 pandemic: A qualitative study. BMC Infectious Diseases 2023, 23, 296. [Google Scholar] [CrossRef] [PubMed]
- Hutahaean, B.S.H.; Stutterheim, S.E.; Jonas, K.J. Barriers and Facilitators to HIV Treatment Adherence in Indonesia: Perspectives of People Living with HIV and HIV Service Providers. Trop Med Infect Dis 2023, 8. [Google Scholar] [CrossRef] [PubMed]

| Item | Results |
|---|---|
| Main information | |
| Timespan | 1993-2025 |
| Sources (Journals, Books, etc) (n) | 65 |
| Documents (n) | 84 |
| Document average age (mean) | 7.45 |
| Average citation per document (mean) | 8.48 |
| Authors | |
| Authors | 400 |
| Authors of single-authored docs | 2 |
| International co-authorship (%) | 51.19 |
| Co-author per document | 7.17 |
| Content | |
| Keywords Plus | 549 |
| Author’s Keywords | 220 |
| Document types | |
| Article | 77 |
| Short survey | 1 |
| Review | 3 |
| Others | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





