Submitted:
22 June 2025
Posted:
24 June 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Pathophysiological Background
3. Components of the EASE Score
- -
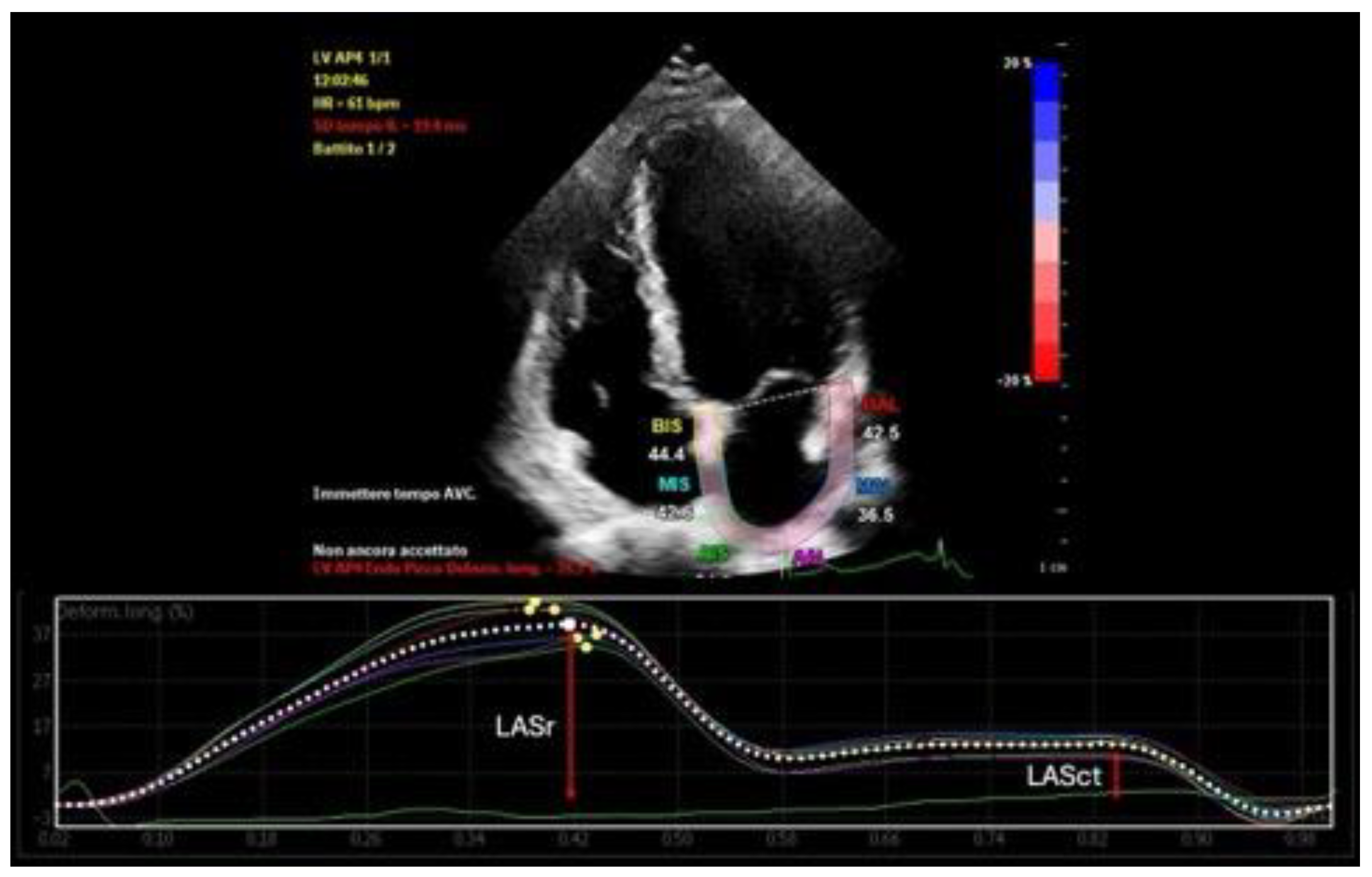
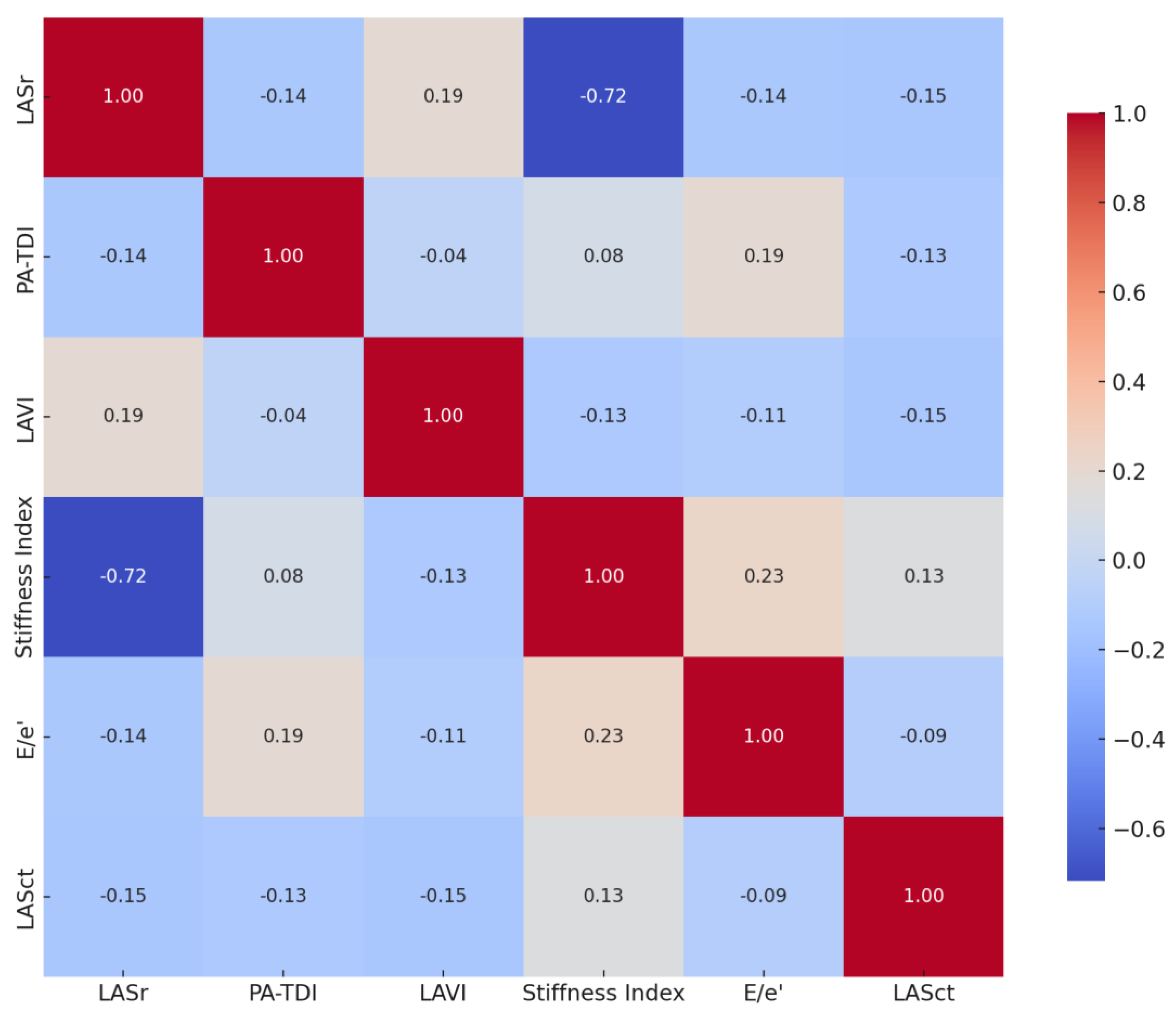
- Left Atrial Reservoir Strain (LASr): LASr is a measure of atrial deformation during ventricular systole, reflecting the reservoir function of the left atrium [19]. It is assessed using 2D speckle-tracking echocardiography and reported as a percentage (Figure 1). A normal LASr value is typically greater than 23%, indicating good atrial compliance and minimal fibrosis. Values between 15% and 23% are considered borderline, while values below 15% suggest advanced atrial remodeling [20]. Reduced LASr has been associated with atrial fibrosis, decreased left atrial compliance, and a higher risk of recurrence after catheter ablation [21].
- -
- Atrial Conduction Time (PA-TDI): PA-TDI is calculated as the time interval from the onset of the P wave on a surface ECG to the onset of the A’ wave measured by tissue Doppler imaging at the lateral mitral annulus [22] (Figure 2). This parameter reflects atrial electromechanical delay and serves as an indicator of electrical remodeling. Normal values are usually below 120 milliseconds, while intervals above 150 milliseconds suggest significant conduction slowing, often due to fibrotic tissue or dilated atrial architecture [23]. Prolonged PA-TDI is independently associated with arrhythmia persistence and ablation failure [24].
- -
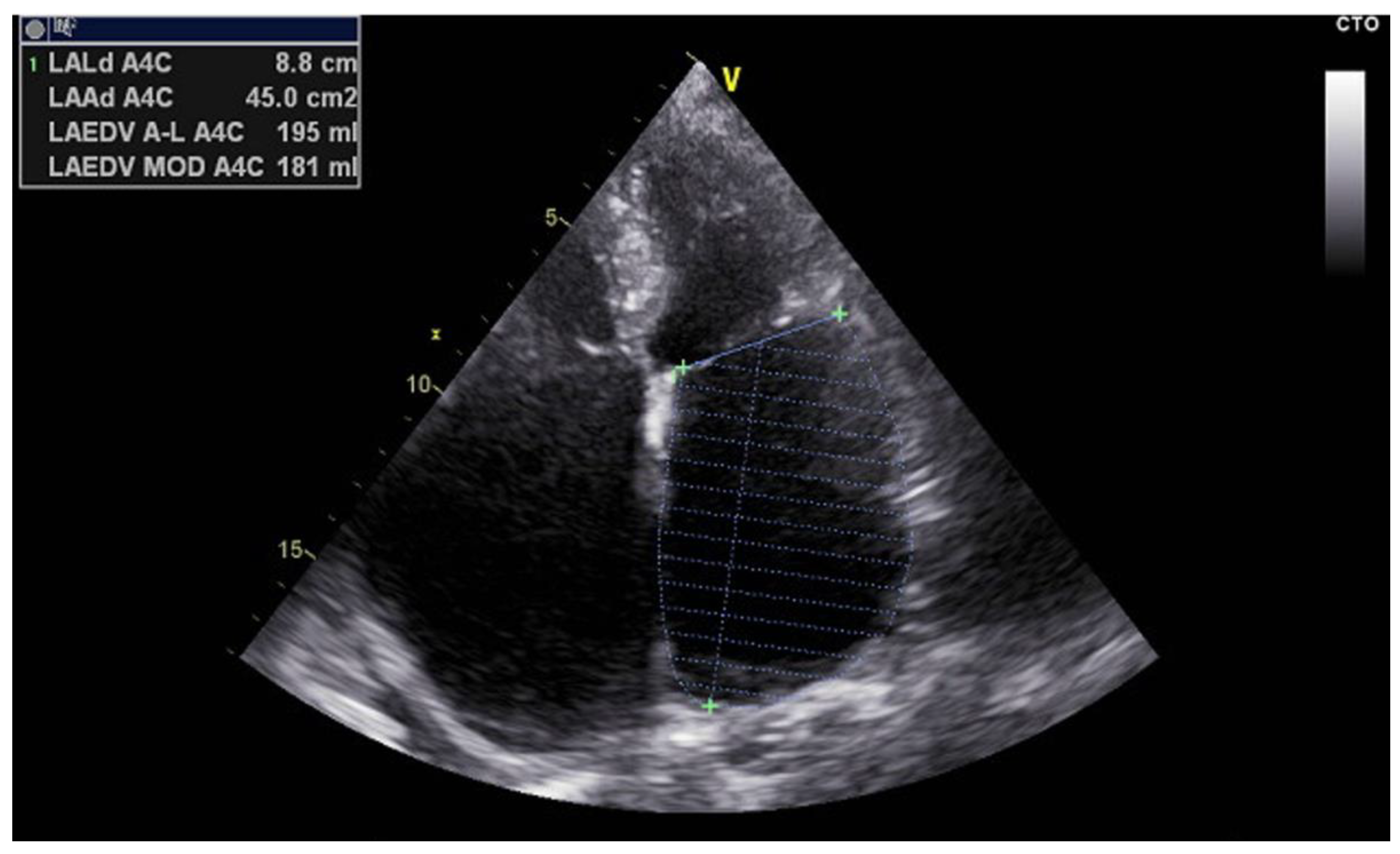
- Left Atrial Volume Index (LAVI): LAVI quantifies the size of the left atrium indexed to body surface area and is measured using the biplane method of disks (modified Simpson’s rule) from apical four- and two-chamber views [25] (Figure 3). Normal LAVI is below 34 mL/m², with values between 34 and 48 mL/m² representing mild to moderate enlargement, and values above 48 mL/m² indicating severe dilation. Increased LAVI reflects chronic pressure or volume overload, often linked to diastolic dysfunction or longstanding atrial fibrillation [26]. It is a robust predictor of adverse cardiovascular events and procedural failure in AF ablation.
- -
- Left Atrial Stiffness Index (E/e’/LASr): This index combines two critical metrics: E/e’, which reflects left ventricular filling pressure, and LASr, which reflects atrial compliance [27]. The stiffness index is calculated by dividing E/e’ by LASr. A value below or equal to 0.5 indicates normal stiffness, whereas a value above 0.5 denotes increased left atrial stiffness. Elevated stiffness is indicative of impaired reservoir function and advanced remodeling, and has been shown to correlate with post-ablation recurrence [28].
- -
- E/e’ Ratio: The E/e’ ratio is a widely used echocardiographic parameter for estimating left ventricular diastolic pressures [29]. It is derived from early mitral inflow velocity (E wave) and early diastolic mitral annular velocity (e’) obtained via pulsed-wave and tissue Doppler imaging, respectively. A ratio above 14 suggests elevated left atrial pressure and diastolic dysfunction [30]. These changes contribute to left atrial strain and enlargement, providing an arrhythmogenic substrate for AF maintenance [31].
- -
- Left Atrial Contractile Strain (LASct): LASct represents the active contraction function of the left atrium and is evaluated using speckle-tracking echocardiography during the late diastolic phase [32] (Figure 1). It is measurable only in patients who are in sinus rhythm at the time of examination. Normal values are typically above 6%, whereas values below this threshold suggest poor contractile function and advanced atrial disease [33]. Impaired LASct has been linked to a greater likelihood of arrhythmia recurrence and reflects the diminished booster pump contribution of the atrium to left ventricular filling [34].
4. Echocardiographic–Electrophysiological Correlation
5. Discussion
6. Preliminary Data and Validation Outlook
7. Limitations and Future Directions
8. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PAF | Paroxysmal Atrial Fibrillation |
| PVI | Pulmonary Vein Isolation |
| EASE | Echocardiographic Atrial Strain and conduction Evaluation (Score) |
| LAVI | Left Atrial Volume Index |
| LASr | Left Atrial Reservoir Strain |
| LASct | Left Atrial Contractile Strain |
| PA-TDI | Atrial Conduction Time Measured by Tissue Doppler Imaging |
| E/e’ | Ratio of early mitral inflow to early diastolic mitral annular velocity |
| E/e’/LASr | Stiffness Index (a derived parameter combining diastolic function and strain) |
| EAT | Epicardial Adipose Tissue |
References
- Van Gelder IC, Rienstra M, Bunting KV, et al. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2024;45(36):3314-3414. [CrossRef]
- Camm AJ, Naccarelli GV, Mittal S, et al. The Increasing Role of Rhythm Control in Patients With Atrial Fibrillation: JACC State-of-the-Art Review. J Am Coll Cardiol. 2022;79(19):1932-1948. [CrossRef]
- Ghannam M, Chugh A. Pulmonary Vein Isolation for Paroxysmal Atrial Fibrillation: When Can We Have It All?. JACC Clin Electrophysiol. 2021;7(3):364-366. [CrossRef]
- Cluckey A, Perino AC, Yunus FN, et al. Efficacy of Ablation Lesion Sets in Addition to Pulmonary Vein Isolation for Paroxysmal Atrial Fibrillation: Findings From the SMASH - AF Meta-Analysis Study Cohort. J Am Heart Assoc. 2019;8(1):e009976. [CrossRef]
- Kueffer T, Bordignon S, Neven K, et al. Durability of Pulmonary Vein Isolation Using Pulsed-Field Ablation: Results From the Multicenter EU-PORIA Registry. JACC Clin Electrophysiol. 2024;10(4):698-708. [CrossRef]
- Kogawa R, Okumura Y, Watanabe I, et al. Left atrial remodeling: Regional differences between paroxysmal and persistent atrial fibrillation. J Arrhythm. 2017;33(5):483-487. [CrossRef]
- Ji M, He L, Gao L, Lin Y, Xie M, Li Y. Assessment of Left Atrial Structure and Function by Echocardiography in Atrial Fibrillation. Diagnostics (Basel). 2022;12(8):1898. Published 2022 Aug 5. [CrossRef]
- Olsen FJ, Darkner S, Chen X, et al. Left atrial structure and function among different subtypes of atrial fibrillation: an echocardiographic substudy of the AMIO-CAT trial. Eur Heart J Cardiovasc Imaging. 2020;21(12):1386-1394. [CrossRef]
- Sim I, Bishop M, O’Neill M, Williams SE. Left atrial voltage mapping: defining and targeting the atrial fibrillation substrate. J Interv Card Electrophysiol. 2019;56(3):213-227. [CrossRef]
- Huang BH, Wu MH, Tsao HM, et al. Morphology of the thoracic veins and left atrium in paroxysmal atrial fibrillation initiated by superior caval vein ectopy. J Cardiovasc Electrophysiol. 2005;16(4):411-417. [CrossRef]
- Zeljkovic I, Knecht S, Spies F, et al. Paroxysmal atrial fibrillation recurrence after redo procedure-ablation modality impact. J Interv Card Electrophysiol. 2020;57(1):77-85. [CrossRef]
- Kong Q, Shi L, Yu R, et al. Biatrial enlargement as a predictor for reablation of atrial fibrillation. Int J Med Sci. 2020;17(18):3031-3038. Published 2020 Oct 18. [CrossRef]
- Pirruccello JP, Di Achille P, Choi SH, et al. Deep learning of left atrial structure and function provides link to atrial fibrillation risk. Nat Commun. 2024;15(1):4304. Published 2024 May 21. [CrossRef]
- Zhao Y, Wang Y, Hu C, et al. Left atrial strain superior to structural remodeling in identifying occult atrial fibrillation. J Clin Ultrasound. 2023;51(8):1301-1307. [CrossRef]
- Karam BS, Chavez-Moreno A, Koh W, Akar JG, Akar FG. Oxidative stress and inflammation as central mediators of atrial fibrillation in obesity and diabetes. Cardiovasc Diabetol. 2017;16(1):120. Published 2017 Sep 29. [CrossRef]
- Bizhanov KA, Аbzaliyev KB, Baimbetov AK, Sarsenbayeva AB, Lyan E. Atrial fibrillation: Epidemiology, pathophysiology, and clinical complications (literature review). J Cardiovasc Electrophysiol. 2023;34(1):153-165. [CrossRef]
- Matsunaga-Lee Y, Inoue K, Tanaka N, et al. Duration of atrial fibrillation persistence: Implications for recurrence risk after catheter ablation and efficacy of additional substrate ablation. Heart Rhythm. 2024;21(6):733-740. [CrossRef]
- Cacciapuoti F, Caso I, Crispo S, et al. Linking Epicardial Adipose Tissue to Atrial Remodeling: Clinical Implications of Strain Imaging. Hearts 2025, 6, 3. [CrossRef]
- Hoit BD. Left Atrial Reservoir Strain: Its Time Has Come. JACC Cardiovasc Imaging. 2022;15(3):392-394. [CrossRef]
- Pathan F, D’Elia N, Nolan MT, Marwick TH, Negishi K. Normal Ranges of Left Atrial Strain by Speckle-Tracking Echocardiography: A Systematic Review and Meta-Analysis. J Am Soc Echocardiogr. 2017;30(1):59-70.e8. [CrossRef]
- Mirza M, Caracciolo G, Khan U, et al. Left atrial reservoir function predicts atrial fibrillation recurrence after catheter ablation: a two-dimensional speckle strain study. J Interv Card Electrophysiol. 2011;31(3):197-206. [CrossRef]
- Müller P, Weijs B, Bemelmans NMAA, et al. Echocardiography-derived total atrial conduction time (PA-TDI duration): risk stratification and guidance in atrial fibrillation management. Clin Res Cardiol. 2021;110(11):1734-1742. [CrossRef]
- Karantoumanis I, Doundoulakis I, Zafeiropoulos S, et al. Atrial conduction time associated predictors of recurrent atrial fibrillation. Int J Cardiovasc Imaging. 2021;37(4):1267-1277. [CrossRef]
- Weijs B, de Vos CB, Tieleman RG, et al. Clinical and echocardiographic correlates of intra-atrial conduction delay. Europace. 2011;13(12):1681-1687. [CrossRef]
- Thadani SR, Shaw RE, Fang Q, Whooley MA, Schiller NB. Left Atrial End-Diastolic Volume Index as a Predictor of Cardiovascular Outcomes: The Heart and Soul Study. Circ Cardiovasc Imaging. 2020;13(4):e009746. [CrossRef]
- Chollet L, Iqbal SUR, Wittmer S, et al. Impact of atrial fibrillation phenotype and left atrial volume on outcome after pulmonary vein isolation. Europace. 2024;26(4):euae071. [CrossRef]
- Lage JGB, Bortolotto AL, Scanavacca MI, Bortolotto LA, Darrieux FCDC. Arterial stiffness and atrial fibrillation: A review. Clinics (Sao Paulo). 2022;77:100014. Published 2022 Mar 3. [CrossRef]
- Khurram IM, Maqbool F, Berger RD, et al. Association Between Left Atrial Stiffness Index and Atrial Fibrillation Recurrence in Patients Undergoing Left Atrial Ablation. Circ Arrhythm Electrophysiol. 2016;9(3):e003163. [CrossRef]
- Arques S, Roux E, Luccioni R. Current clinical applications of spectral tissue Doppler echocardiography (E/E’ ratio) as a noninvasive surrogate for left ventricular diastolic pressures in the diagnosis of heart failure with preserved left ventricular systolic function. Cardiovasc Ultrasound. 2007;5:16. Published 2007 Mar 26. [CrossRef]
- Obokata M, Reddy YNV, Borlaug BA. Diastolic Dysfunction and Heart Failure With Preserved Ejection Fraction: Understanding Mechanisms by Using Noninvasive Methods. JACC Cardiovasc Imaging. 2020;13(1 Pt 2):245-257. [CrossRef]
- Arques S. Clinical Relevance of the Spectral Tissue Doppler E/e’ Ratio in the Management of Patients with Atrial Fibrillation: a Comprehensive Review of the Literature. J Atr Fibrillation. 2018;11(2):2038. Published 2018 Aug 31. [CrossRef]
- Gold AK, Kiefer JJ, Feinman JW, Augoustides JG. Left Atrial Strain-A Valuable Window on Left Ventricular Diastolic Function. J Cardiothorac Vasc Anesth. 2021;35(6):1626-1627. [CrossRef]
- Morris DA, Takeuchi M, Krisper M, et al. Normal values and clinical relevance of left atrial myocardial function analysed by speckle-tracking echocardiography: multicentre study. Eur Heart J Cardiovasc Imaging. 2015;16(4):364-372. [CrossRef]
- Hopman LHGA, Bhagirath P, Mulder MJ, et al. Left atrial sphericity in relation to atrial strain and strain rate in atrial fibrillation patients. Int J Cardiovasc Imaging. 2023;39(9):1753-1763. [CrossRef]
- Lisi M, Mandoli GE, Cameli M, et al. Left atrial strain by speckle tracking predicts atrial fibrosis in patients undergoing heart transplantation. Eur Heart J Cardiovasc Imaging. 2022;23(6):829-835. [CrossRef]
- Laish-Farkash A, Perelshtein Brezinov O, Valdman A, et al. Evaluation of left atrial remodeling by 2D-speckle-tracking echocardiography versus by high-density voltage mapping in patients with atrial fibrillation. J Cardiovasc Electrophysiol. 2021;32(2):305-315. [CrossRef]
- Kanda T, Masuda M, Asai M, et al. Extensive Left Atrial Low-Voltage Area During Initial Ablation is Associated with A Poor Clinical Outcome Even Following Multiple Procedures. J Atr Fibrillation. 2021;14(2):20200491. Published 2021 Aug 31. [CrossRef]
- Müller P, Schiedat F, Bialek A, et al. Total atrial conduction time assessed by tissue doppler imaging (PA-TDI Interval) to predict early recurrence of persistent atrial fibrillation after successful electrical cardioversion. J Cardiovasc Electrophysiol. 2014;25(2):161-167. [CrossRef]
- Miragoli M, Glukhov AV. Atrial Fibrillation and Fibrosis: Beyond the Cardiomyocyte Centric View. Biomed Res Int. 2015;2015:798768. [CrossRef]
- Beyer C, Tokarska L, Stühlinger M, et al. Structural Cardiac Remodeling in Atrial Fibrillation. JACC Cardiovasc Imaging. 2021;14(11):2199-2208. [CrossRef]
- Yoon YE, Kim HJ, Kim SA, et al. Left atrial mechanical function and stiffness in patients with paroxysmal atrial fibrillation. J Cardiovasc Ultrasound. 2012;20(3):140-145. [CrossRef]
- Masuda M, Fujita M, Iida O, et al. An E/e’ ratio on echocardiography predicts the existence of left atrial low-voltage areas and poor outcomes after catheter ablation for atrial fibrillation. Europace. 2018;20(5):e60-e68. [CrossRef]
- Nielsen AB, Skaarup KG, Djernæs K, et al. Left atrial contractile strain predicts recurrence of atrial tachyarrhythmia after catheter ablation. Int J Cardiol. 2022;358:51-57. [CrossRef]
- Strisciuglio T, El Haddad M, Debonnaire P, et al. Paroxysmal atrial fibrillation with high vs. low arrhythmia burden: atrial remodelling and ablation outcome. Europace. 2020;22(8):1189-1196. [CrossRef]
- Barletta V, Canu AM, Parollo M, et al. A Long Atrial Electromechanical Interval is Associated with Arrhythmic Recurrence after Catheter Ablation: How to Find What Has Been Lost. J Cardiovasc Echogr. 2024;34(3):125-131. [CrossRef]
- Bajraktari G, Bytyçi I, Henein MY. Left atrial structure and function predictors of recurrent fibrillation after catheter ablation: a systematic review and meta-analysis. Clin Physiol Funct Imaging. 2020;40(1):1-13. [CrossRef]
- Correia ETO, Barbetta LMDS, Silva OMPD, Mesquita ET. Left Atrial Stiffness: A Predictor of Atrial Fibrillation Recurrence after Radiofrequency Catheter Ablation - A Systematic Review and Meta-Analysis. Arq Bras Cardiol. 2019;112(5):501-508. [CrossRef]
- Lin J, Ma H, Gao L, et al. Left atrial reservoir strain combined with E/E’ as a better single measure to predict elevated LV filling pressures in patients with coronary artery disease. Cardiovasc Ultrasound. 2020;18(1):11. Published 2020 Apr 25. [CrossRef]
- Chahine Y, Chamoun N, Kassar A, Bockus L, Macheret F, Akoum N. Atrial fibrillation substrate and impaired left atrial function: a cardiac MRI study. Europace. 2024;26(11):euae258. [CrossRef]
- Samaras A, Doundoulakis I, Antza C, Zafeiropoulos S, Farmakis I, Tzikas A. Comparative Analysis of Risk Stratification Scores in Atrial Fibrillation. Curr Pharm Des. 2021;27(10):1298-1310. [CrossRef]
- Wijesurendra RS, Casadei B. Mechanisms of atrial fibrillation. Heart. 2019;105(24):1860-1867. [CrossRef]
- Stefani LD, Trivedi SJ, Ferkh A, Altman M, Thomas L. Changes in left atrial phasic strain and mechanical dispersion: Effects of age and gender. Echocardiography. 2021;38(3):417-426. [CrossRef]
- Chiotis S, Doundoulakis I, Pagkalidou E, et al. Total Atrial Conduction Time as a Predictor of Atrial Fibrillation Recurrence: A Systematic Review and Meta-Analysis. Cardiol Rev. 2025;33(1):70-76. [CrossRef]
- Parajuli P, Alahmadi MH, Ahmed AA. Left Atrial Enlargement. In: StatPearls. Treasure Island (FL): StatPearls Publishing; January 22, 2025.
- Pilichowska-Paszkiet E, Baran J, Sygitowicz G, et al. Noninvasive assessment of left atrial fibrosis. Correlation between echocardiography, biomarkers, and electroanatomical mapping. Echocardiography. 2018;35(9):1326-1334. [CrossRef]
- Kiliszek M, Uziębło-Życzkowska B, Krzyżanowski K, et al. Value of Left Atrial Strain in Predicting Recurrence after Atrial Fibrillation Ablation. J Clin Med. 2023;12(12):4034. Published 2023 Jun 13. [CrossRef]
- Chahine Y, Macheret F, Ordovas K, Kim J, Boyle PM, Akoum N. MRI-quantified left atrial epicardial adipose tissue predicts atrial fibrillation recurrence following catheter ablation. Front Cardiovasc Med. 2022;9:1045742. Published 2022 Dec 2. [CrossRef]
- Dell’Aversana F, Tuccillo R, Monfregola A, et al. Epicardial Adipose Tissue Volume Assessment in the General Population and CAD-RADS 2.0 Score Correlation Using Dual Source Cardiac CT. Diagnostics (Basel). 2025;15(6):681. Published 2025 Mar 10. [CrossRef]

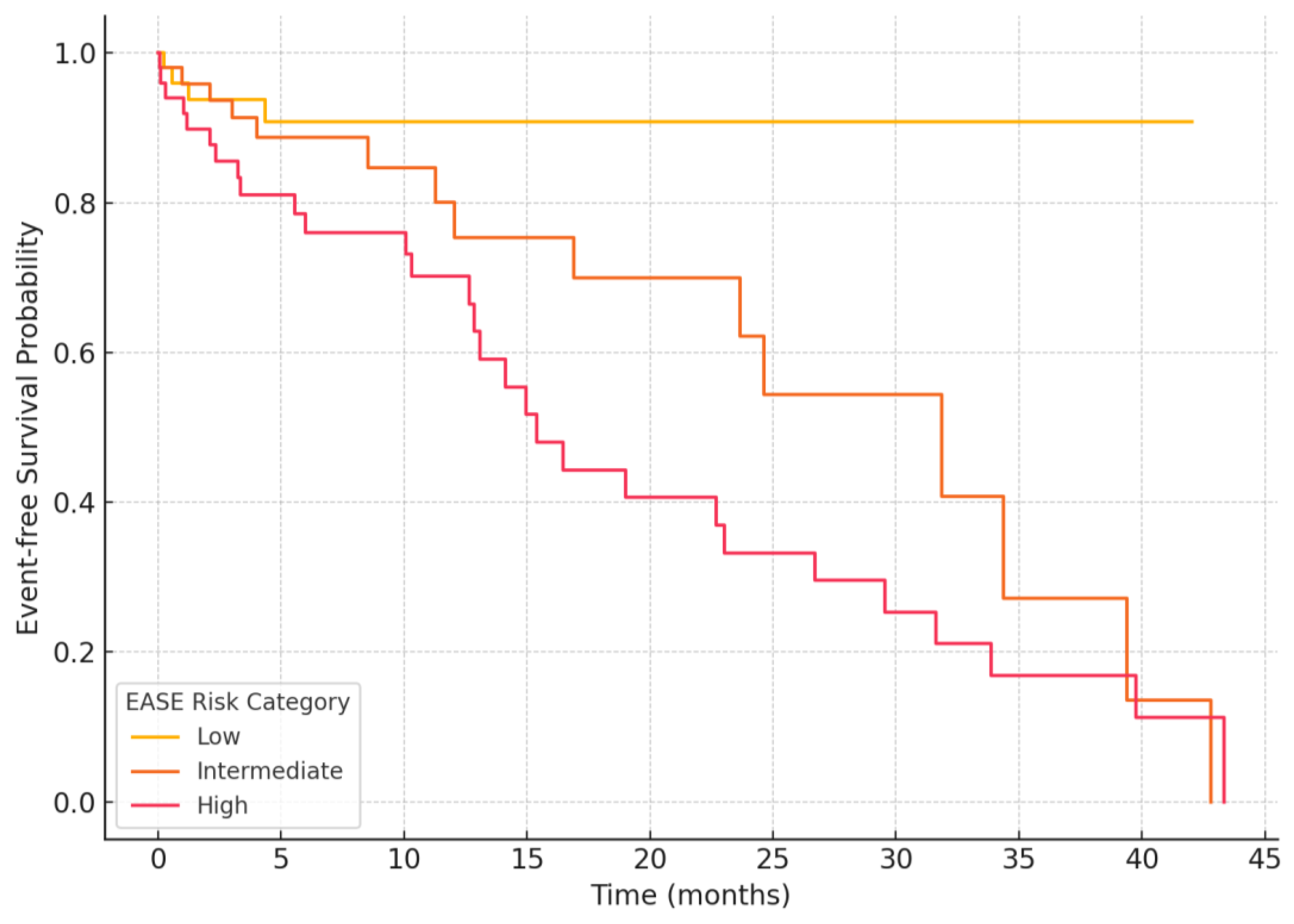
| EASE Score | Risk Category | Interpretation |
|---|---|---|
| 0-3 | Low | Minimal atrial remodeling; high likelihood of ablation success |
| 4-8 | Intermediate | Moderate remodeling; variable outcomes; consider enhanced monitoring |
| 9-12 | High | Extensive remodeling; increased risk of recurrence; consider adjunctive strategies |
| EASE Parameter | Pathophysiological Role | Electrophysiological Correlate |
|---|---|---|
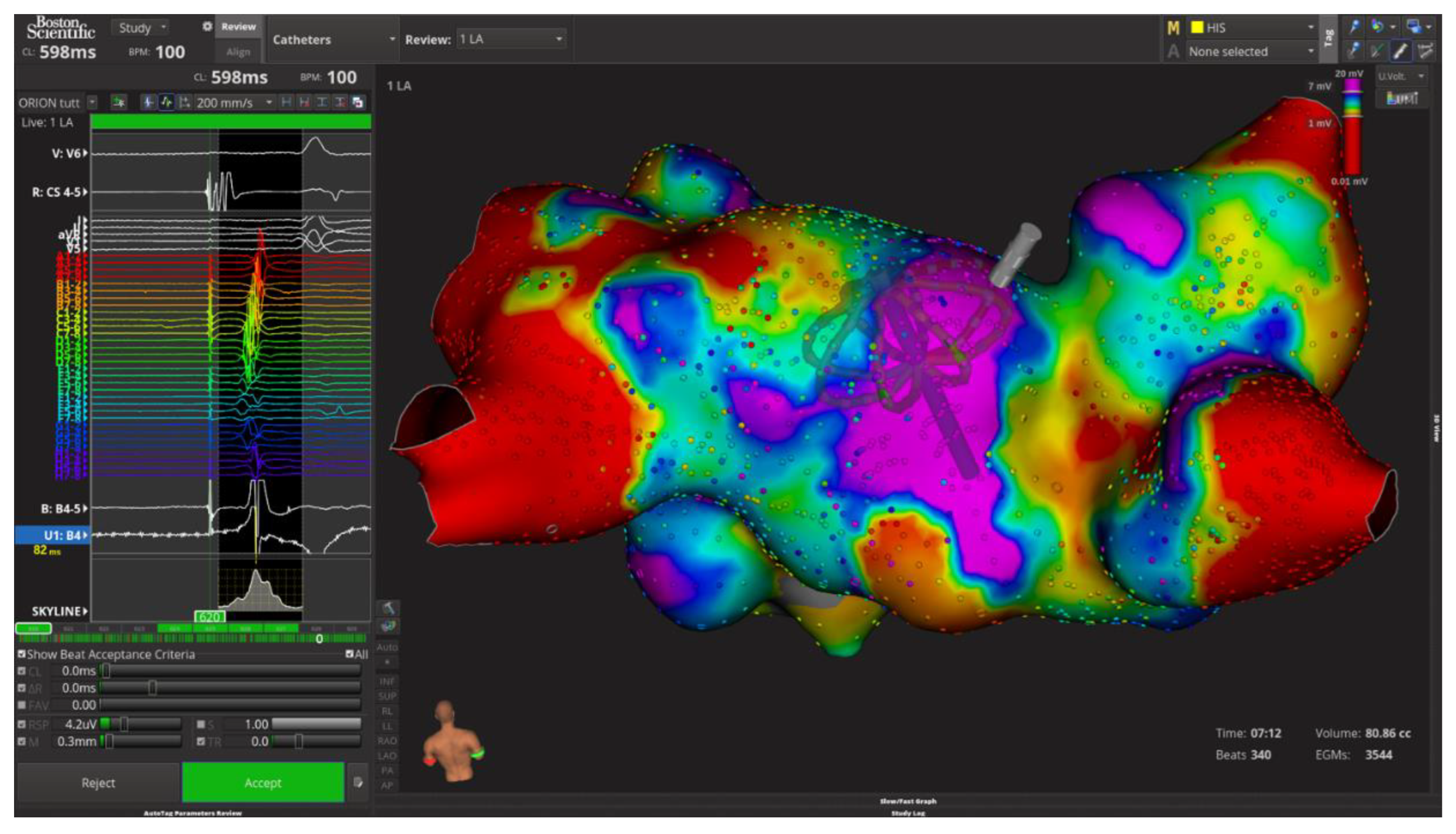
| LASr (Reservoir Strain) | Reflects LA compliance and fibrosis; lower values indicate impaired reservoir function | Corresponds to low-voltage zones (<0.5 mV), reduced CFAE density, and fibrotic substrate |
| PA-TDI (Atrial Conduction Time) | Indicates intra-atrial conduction delay and electromechanical dysfunction | Associated with prolonged activation time, interatrial dyssynchrony, and zig-zag conduction |
| LAVI (Volume Index) | Indicates chronic structural remodeling and LA dilation due to volume/pressure overload | Correlates with widespread CFAEs, multiple breakthrough sites, and complex activation patterns |
| E/e’ (Diastolic Pressure Estimate) | Reflects elevated LV filling pressure and LA pressure overload | Associated with prolonged electrogram duration, low voltage density, and post-ablation recurrence |
| Stiffness Index (E/e’/LASr) | Integrates diastolic burden and atrial compliance; higher values reflect stiffer LA | Overlaps with fragmented potentials, conduction heterogeneity, and low-voltage regions |
| LASct (Contractile Strain) | Reflects active LA contraction; low values indicate poor contractile function | Predictive of atrial standstill, late potentials loss, and reduced sinus rhythm maintenance post-ablation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





