Introduction
Oligozoospermia refers to semen with a low sperm count. WHO reassessed sperm criteria and established a lower reference point, less than 15 million sperm/ml. Oligospermia has many diverse causes, as many different medical conditions can diminish sperm concentration. Out of several causes of male infertility, in clinical practice Oligospermia is considered one of the most prevalent causes [
1,
2,
3,
4,
5].
Infertility and problems of impaired fecundity have been a concern through ages and is also a significant clinical problem today, which affects 8–12% of couples worldwide. Of all infertility cases, approximately 40–50% is due to “male factor” infertility and as many as 2% of all men exhibit suboptimal sperm parameters. As per the WHO, the overall prevalence of primary infertility ranges between 3.9% and 16.8% in India [
6,
7]. Analysis was of retrospective data indicates that sperm counts may have declined in some parts of the world, but there seems to be geographical variations in the semen quality. The reason for geographic variations in semen characteristics is not clear, but it may be due to environmental, nutritional, socioeconomic, or other unknown causes. The decline in the semen quality coincides with an increasing incidence of abnormalities of the male genital tract.
The investigation was designed as nonrandomized open label single arm interventional study assessing the effect of constitutional homoeopathic medicine on low sperm count. Several homoeopathic medicines such as X-ray, sabalserrulata, sulphur, sulfanilamide are indicated for low sperm count according to homeopathic materiamedica [
8,
9,
10]. But the etiology behind oligozoospermia is consequential to psychological, economic, medical implications. Therefore the constitutional approach was most valid in the management of overall male infertility. This study had assessed the improvement in sperm count from baseline to 3 months. Homeopathy treats infertility not as a disease, but as an imbalance to be corrected. It can reverse infertility with constitutional homoeopathic treatment as it goes to the core basis of infertility and arouse the body capability to restore to health itself. Homeopathy treatment for infertility is stimulating and supporting a normal conception gradually.
Objectives
Primary Objective
To investigate the effect of constitutional homoeopathic medicine on oligozoospermia from baseline to 3 months
Secondary Objective
To discuss the application and success rates of homeopathic versus modern treatment for the oligozoospermic patient
Methods
Study Design
Study type: Interventional
Actual Enrolment achieved: 10 patients
Allocation: Non-randomized
Intervention model: Single arm
Masking: Open label
Study duration: November 2018 to March 2019
Screening: 1month (November 2018)
Treatment period: December 2018 to Feb 2019
Data Analysis: March 2019
College and Hospital, Pune, Maharashtra, India
Arms and Intervention
The study was single armed hence only experimental arm was applicable.
Homoeopathic preparation of constitutional medicine was administered in suitable potencies as a single dose. Constitutional medicine was administered over powder form by oral route.
Selection of Patients
Patients were enrolled after satisfying all the inclusion criteria and no exclusion criteria.
Inclusion Criteria
1. 25 Years to 50 Years (Adult) male
2. Oligospermia (< 10 million per mil-litter)
3. Marriage history for >1 year
4. Willing to give specimen of semen before & at the end of the study
5. Informed patients giving written consent
Exclusion Criteria
1. Abnormal karyotype
2. Obstructive azoospermia
3. Azoospermia
4. Aspermia
5. Necrospermia
6. Clinical diagnosis of varicocele& hydrocele
7. History of undescended testis
8. Inguinal hernia on physical examination
9. Male accessory gland infection
10. History of DM, Hypertension and Cardiac disease
11. Any recent medical or surgical illness
12. Underwent treatment for promoting spermatogenic fertility in last 3 months
13. Other Systemic disease requiring specific therapies
14. Known Thyroid disease
15. Past history of Renal, Hepatic or any other chronic illness in the Patient
Outcome Measures
Changes in the total number of sperm cells per milliliter of seminal fluid from baseline to three months
2. Changes in the percentage of total and progressive motility of sperm from baseline to three months
3. Proportion of Sperm morphology
Ethics
This study was conducted as per the guidelines of GCP accepted by Ayush adapted from the ICH. ICH-GCP guidelines as per Declaration of Helsinki 1964 and ICMR code was followed while conducting the study. The primary purpose of this study was ‘treatment’ and intention-to-treat principle was followed throughout the study. The study was commenced only after approval from ethics committee and the consent form was also being translated to the vernacular language.
Data Collection
Data related to semen analysis was and sperm count was collected at baseline and after three months. A computerized data entry was made with respect to patient’s baseline and demographic characteristics. Monthly special telephonic follow-up was arranged as per the requirement. Detailed past history, concomitant medications as well as adverse events (related/unrelated) were recorded accurately. Source data such as case papers, medical records, diagnostic test documents, consent form, referral information was collected and recorded. Batch number of the medicines was recorded and separate treatment accountability log was maintained. All the efforts were being taken to protect the confidentiality of data and records of study participants. All the standard laboratory normal reference ranges for sperm count was be recorded and compared.
Data Analyses
As this was a pilot study no formal calculation of sample size was required. Data was being summarized in the form of tables, and figures. Baseline descriptive data were expressed as Mean±SD. No formal sample size estimation was performed before starting the study. The P value less than 0.05 was considered as significant for the one tailed hypothesis. The data was be analyzed with the help of Microsoft excel and Graph Pad Prism Version 7.0 (academic). Missing data was be imputed from appropriate statistical techniques such as BOCF. Appropriate test of significance for instance parametric students paired‘t’ test was used. Where possible the data for homoeopathic remedies was presented as n (%).
Appropriateness of Measurements
Semen Analysis
Semen analysis is the most fundamental part of the assessment of male factor infertility. After 2–5 days of abstinence, a semen sample can be collected usually by masturbation into a special container or by intercourse into a special condom. The semen sample needs to be examined in the laboratory within an hour of collection. The finding of an abnormal semen analysis result should be followed up by another semen analysis, ideally 3 months later to allow sufficient time for new sperm to be formed. Complete semen analysis includes ejaculate volume, sperm count, concentration, motility, and morphology. Basic semen analysis measures the number of spermatozoa (per unit volume and per ejaculate), motility and morphology. The semen analysis, in the present study was performed according to the guidelines established by the World Health Organization (WHO) by a certified andrology laboratory [
11].
Results
Baseline and Demographic Characteristics of Respondents
Baseline and demographic characteristics of respondents are explained in
Table 1. Out of 23 initially screened participants, only 10 (43.47%) participants were enrolled and followed up in the study. Majority of the male individuals participated in this study were Hindu. Large numbers of patients were belonged to middle to low income group and found working as daily wages workers. The average sperm count at baseline was < 10 million per mil-litter, thus satisfying the main inclusion criteria [
2].
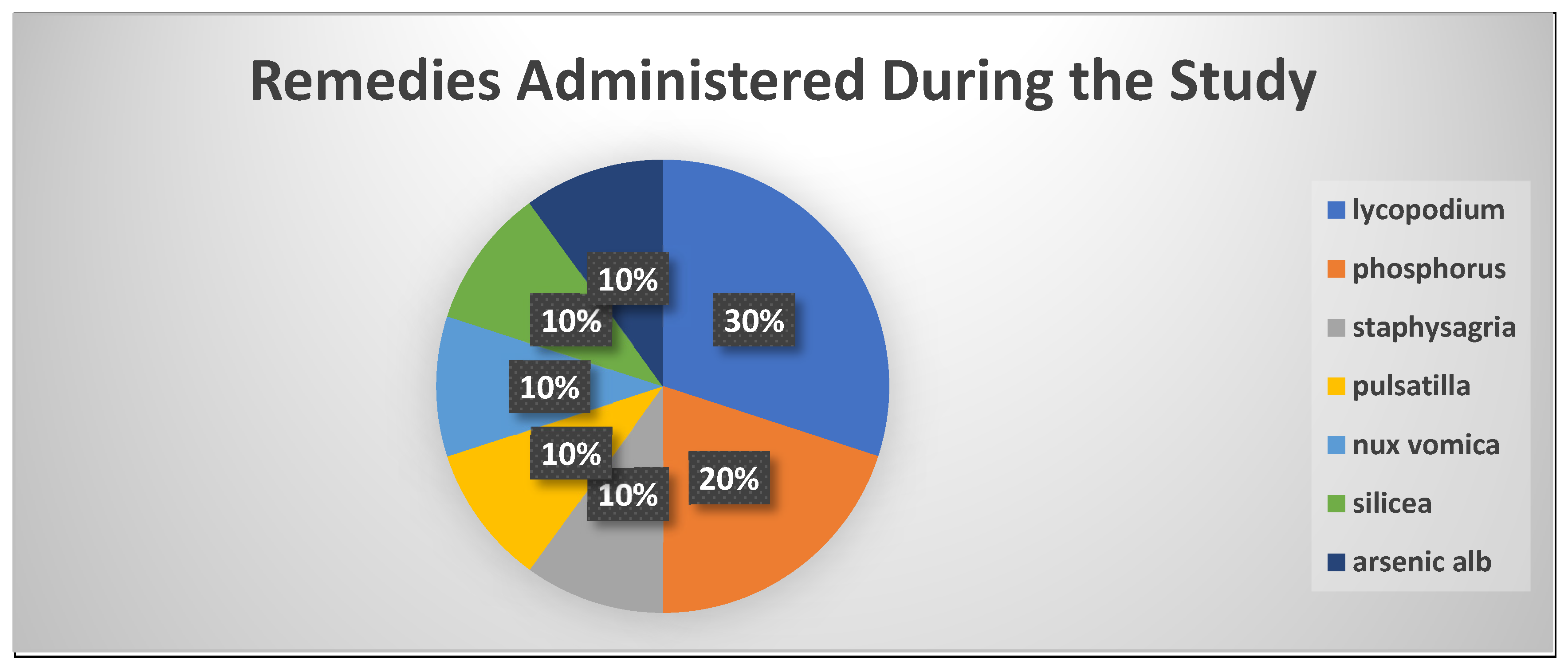
Homoeopathic Medicines Administered During the Treatment Period
Total of 7 constitutional medicines were prescribed for total of 10 male individuals. Out of 10 individuals lycopodium was prescribed to more number of patients 3(30%) followed by phosphorus 2(20%). The detailed analysis of percentage distribution of homoeopathic constitutional medicines is given in a
Figure 1. Nux vomica 1(10%) and lycopodium 1(10%) were prescribed in 200CH potency while remaining all medicines were prescribed in 30CH potency as a single powdered dose.
Clinical Endpoints
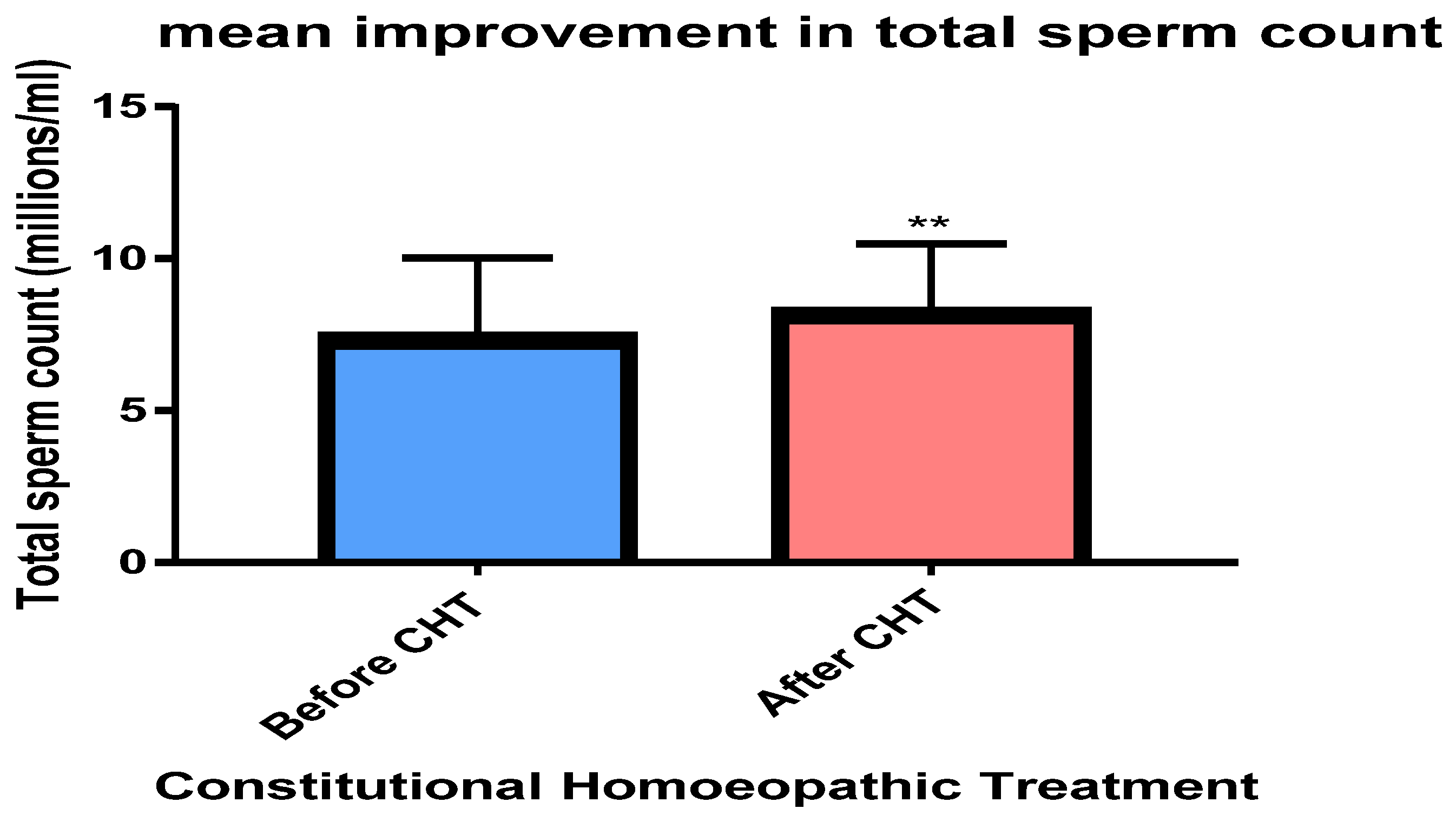
Total Sperm Count
There was statistically significant (
p=0.0013) improvement observed in total sperm count after the treatment with homoeopathic constitutional medicines. The detail of mean increase in total sperm count from baseline to 3 months is shown in
Figure 2.
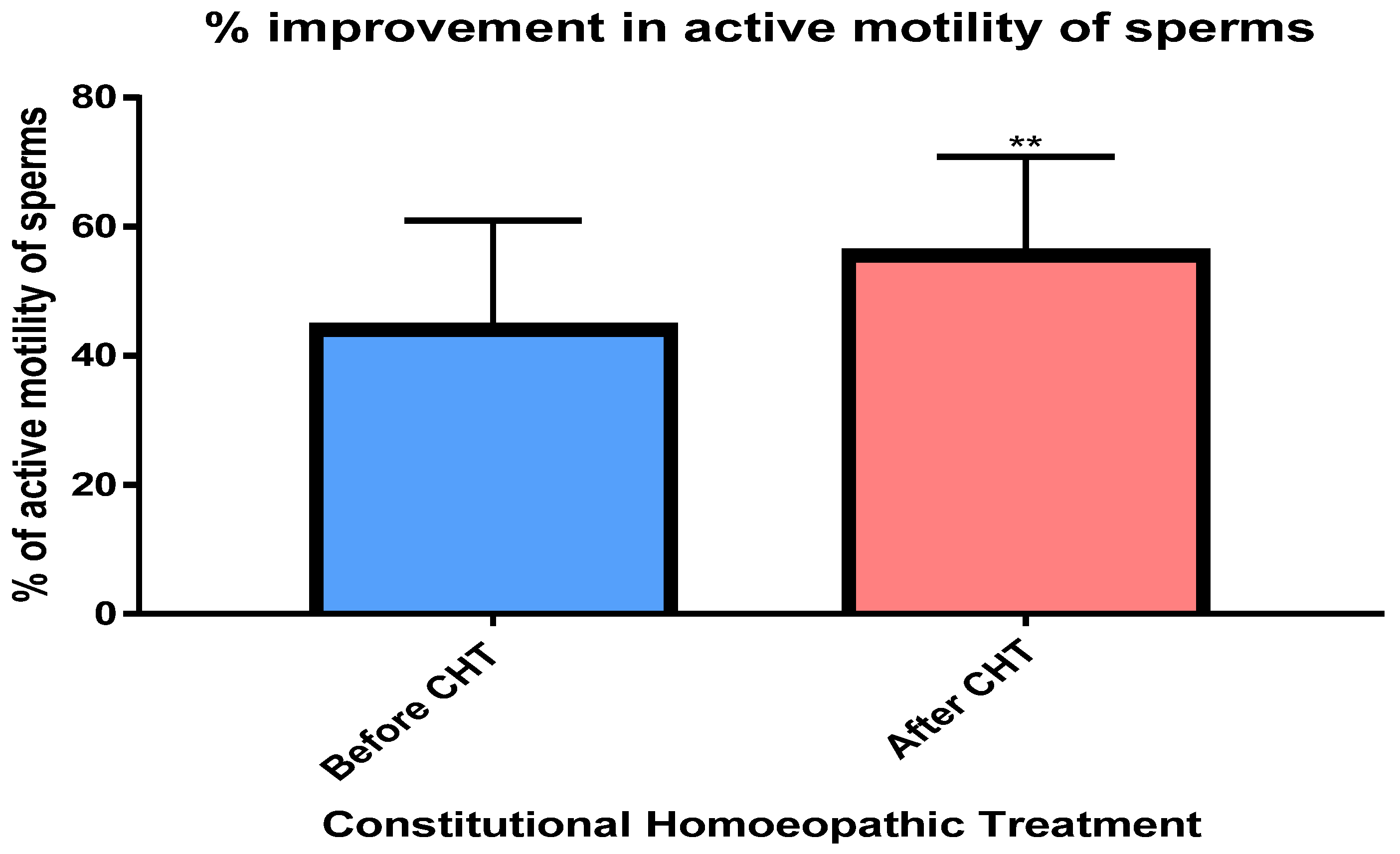
Active Motility
There was statistically significant improvement (
p= 0.0027) observed in active sperm motility after the treatment with homoeopathic constitutional medicines. The detail of % increase in total active sperm motility from baseline to 3 months is shown in
Figure 3.
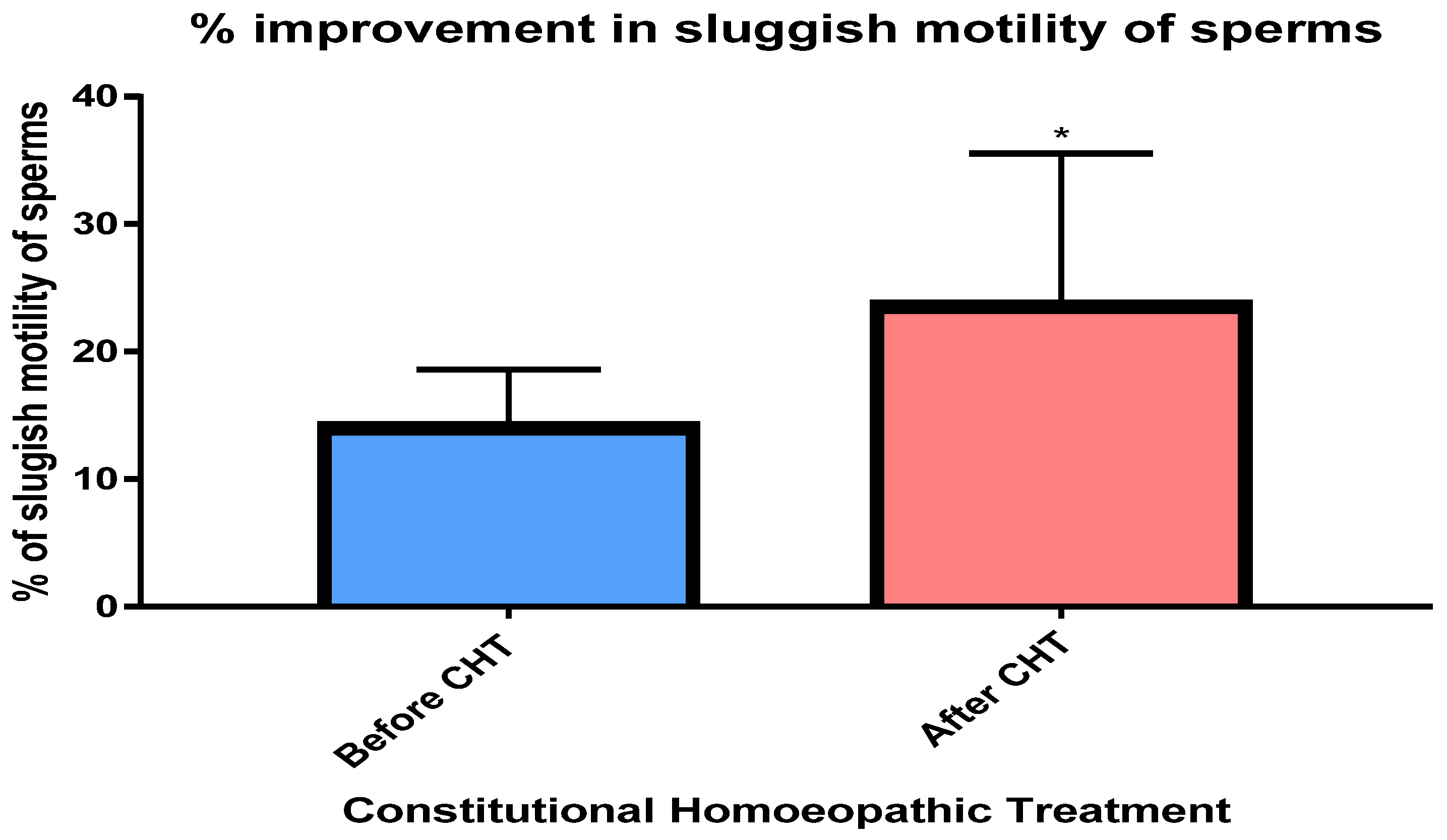
Sluggish Motility
There was statistically significant (
p= 0.0119) increase observed in sluggish sperm motility after the treatment with homoeopathic constitutional medicines. The detail of % increase in total sluggish sperm motility from baseline to 3 months is shown in
Figure 4.
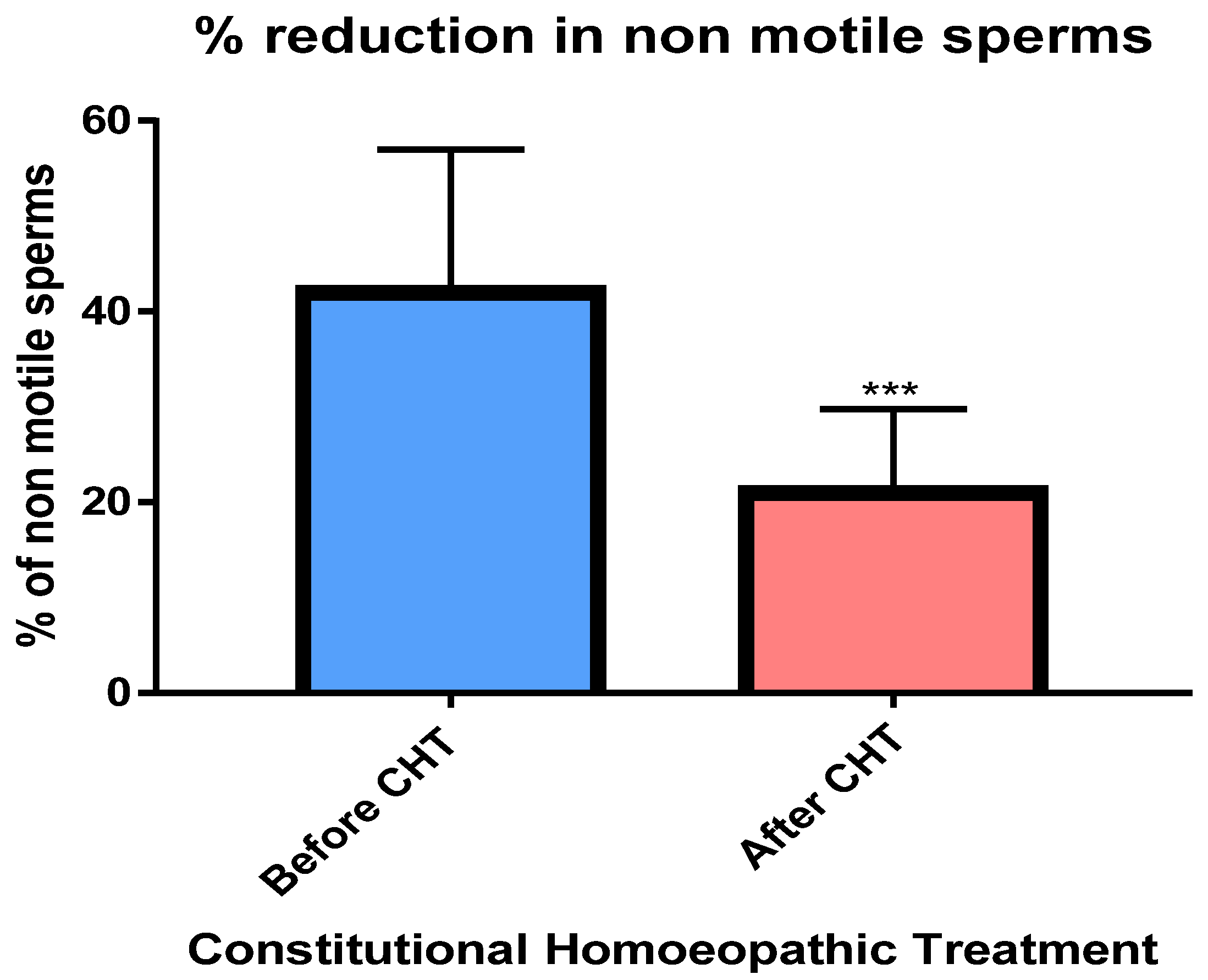
Non-Motile Sperms
There was statistically significant (
p= 0.0006) reduction observed in % of non motile sperms after the treatment with homoeopathic constitutional medicines. The detail of % reduction in non motile sperms from baseline to 3 months is shown in
Figure 5.
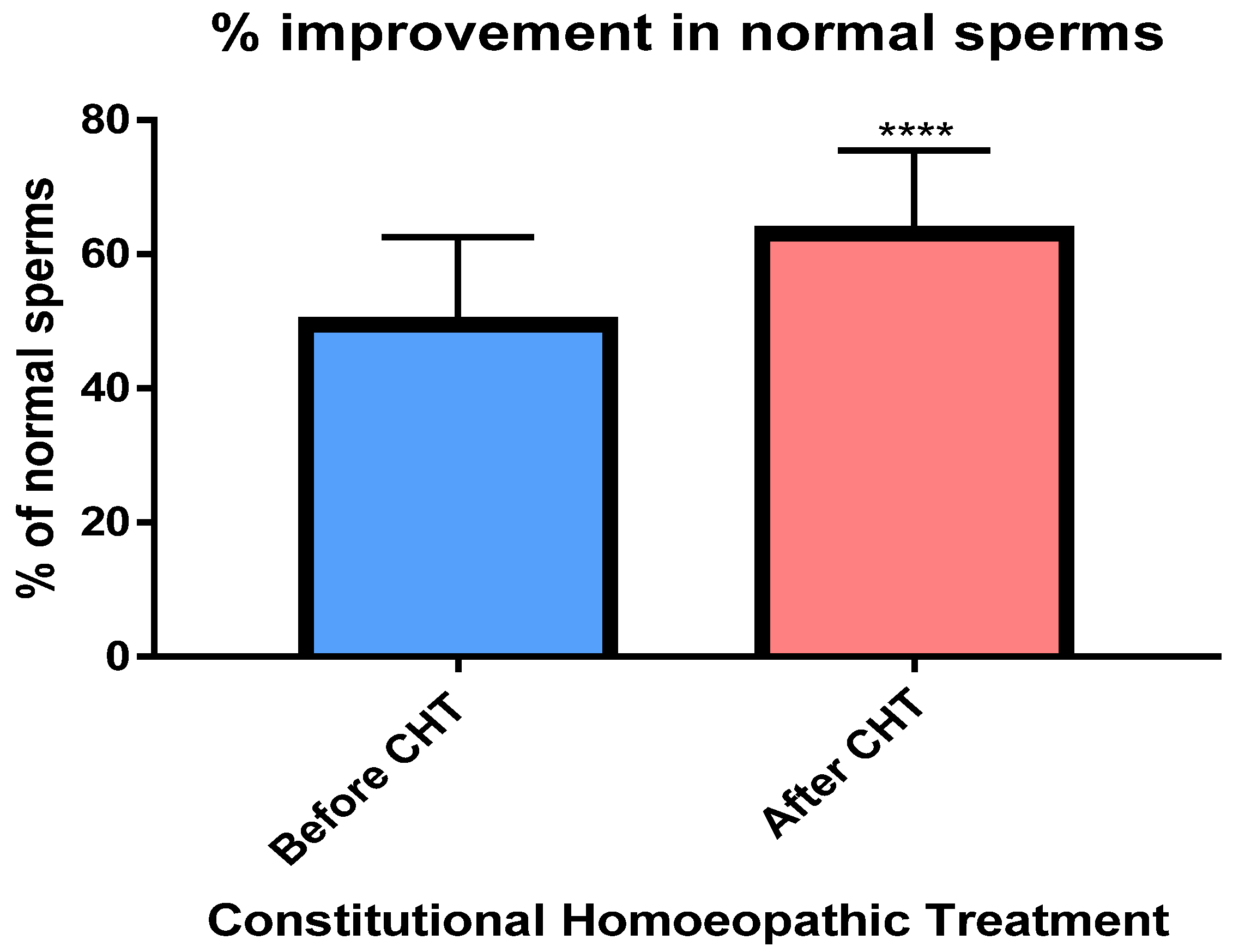
Normal Sperms
There was statistically significant improvement (
p<0.0001) observed in normal sperms after the treatment with homoeopathic constitutional medicines. The detail of % increase in total normal sperms from baseline to 3 months is shown in
Figure 6.
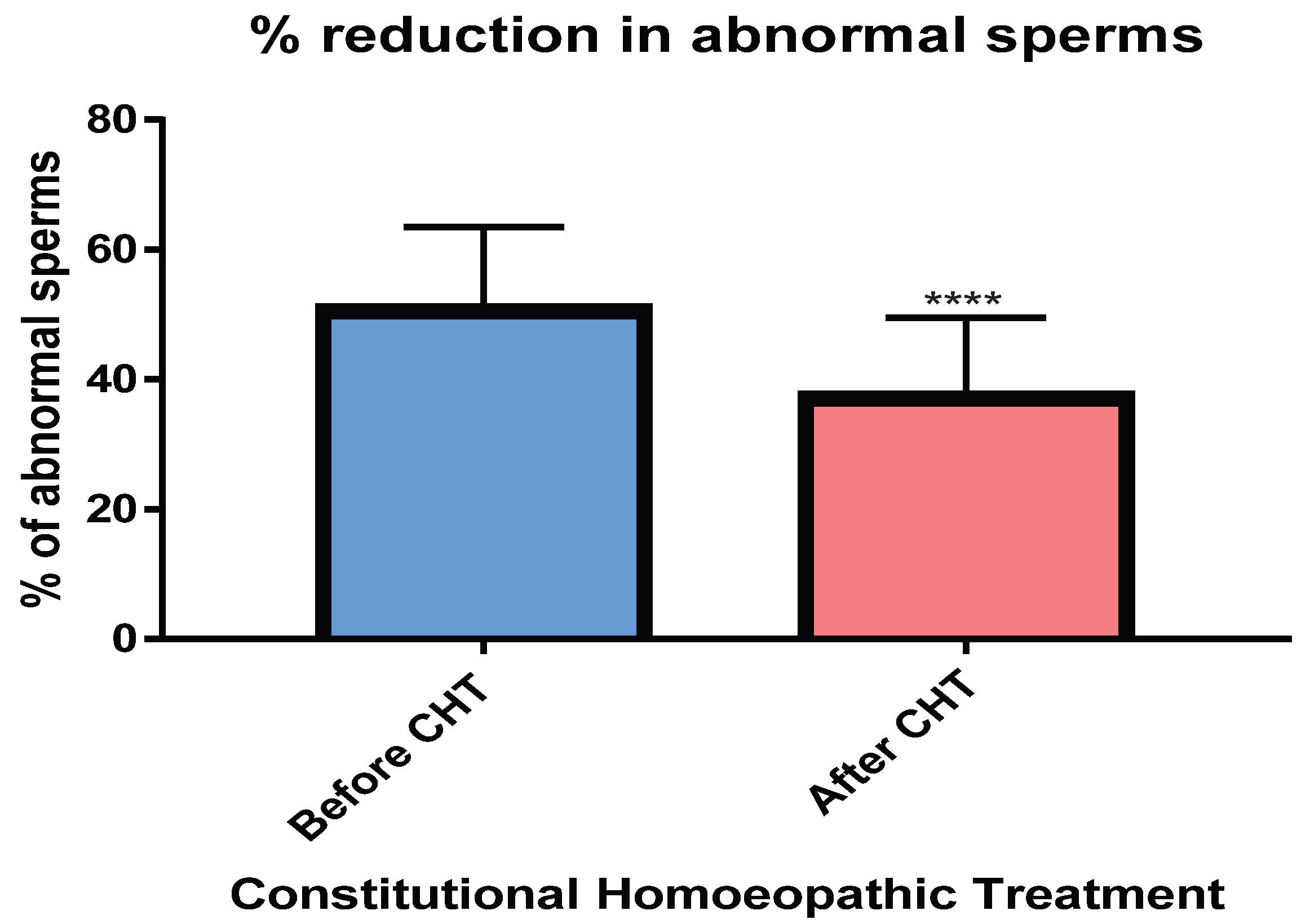
Abnormal Sperms
There was statistically significant (
p<0.0001) reduction observed in % of abnormal sperms after the treatment with homoeopathic constitutional medicines. The detail of % reduction in abnormal sperms from baseline to 3 months is shown in
Figure 7.
Cumulative Rate of Conception
Out of 10 male individuals participated in this study, 2 (20%) female partners were conceived during the study.
Discussion
The present study was conducted between November 2018 and March 2019 at BharatiVidyapeeth (Deemed to be University) Homoeopathic Medical College and Hospital and Post Graduate Research Centre. The study was an interventional, non-randomized, single arm model. It was an open label study. The written and signed ICF by the participants was taken before the study enrolment. Ten participants out of 23 male individuals were enrolled in the study after fulfilling predetermined eligibility criteria. The process of case taking was perfomed in accordance with the 6th edition of Organon of medicine (Ꞩ83-92). The case was analyzed with the help of Radar 10.5 homoeopathic software. The diagnosis was confirmed by the semen analysis with the average abstinence of 4 days. The individualized (constitutional) homoeopathic medicines were administered orally as single dose and the potency was determined by individual’s susceptibility. The primary objective of this study was to investigate the effect of constitutional homoeopathic medicine on oligozoospermia from baseline to 3 months. While secondary objective was to discuss the application and success rates of homeopathic versus modern treatment for the oligozoospermic patients.
In this study the total sperm count along with the sperm motility and morphology was found to be statistically significantly (
p<0.05) improved after the treatment with homoeopathic constitutional medicines. A similar study conducted with homoeopathic medicines for unexplained infertility demonstrated marginally improved fertility rate and quality of life. The same study was conducted over 27 males and 28 females and the outcomes were conception and pregnancy. The lycopodium was given to 9(16.36%) patients in this study. Similarly in our study lycopdium was the most frequently prescribed medicine given to 3(30%) of the study participants. Current study records the cumulative conception rate as 2(20%) compared to previous study with homoeopathic medicines 03 (0.05%) [
12].
Another prospective observational pilot study investigated the effect of individualized homeopathy on male infertility based on sperm count, hormone values and general health. Forty-five sub fertile men were treated with single homeopathic remedies for an average of 10.3 months. The drugs were prescribed on the basis of the overall symptomatic situation. The variables ‘sperm density’, ‘percentage of sperm with good progressive motility’ and ‘density of sperm with good propulsive motility’ improved significantly, especially in cases of oligoasthenozoospermia [
13].
Other treatment modalities like clomiphene citrate (CC), tamoxifen, recombinant FSH, zinc, selenium, and L-carnitine have been tried with minimal success. Similarly gonadotrophins, letrozole, synthetic testosterone pills, injections, are also used as line of treatment in oligozoospermia
. Many studies confirm CC shows significant improvement in fertility rates and some studies show improvement in semen parameters [
14].
The present investigation though provides a statistically significant results, the external validity of the results is limited because of low sample size. For further investigation it is necessary to adopt randomized, controlled design against the conventional andrological therapy. Subsequently extensive follow up is necessary to obtain normal sperm count and quality alongside baby take home rate for already conceived female partners during this study.
Conclusions
Individualized Homoeopathic Treatment with constitutional medicines significantly (p=0.0013) improves total sperm count, sperm motility, normal sperms. Further study might be explored by increasing the sample sizewith randomized controlled trial design.
Acknowledgments
Authors are thankful to BharatiVidyapeeth (Deemed to be university) Homoeopathic Medical College and research Centre for providing necessary infrastructure and research facilities.Dr. Anjali Gokhale for constant check on the progress of the project, andDr.TejasPrabhakarGosavi for his relentless guidance and for this great opportunity provided by the Short term studentship in Homoeopathy (STSH) ,organised by CCRH, under Ministry of AYUSH , Govt of India. And I would like to Thank specially my parents for their constant support and unconditional love.
Conflict of Interest
There is no conflict of interest.
Source of funding
STSH scheme from CCRH, Ministry of Ayush.
References
- Zegers-Hochschild F, Adamson GD, de Mouzon J, Washihara O, Mansour R, Nygren K, et al. International Committee for Monitoring Asswasted Reproductive Technology (ICMART) and the World Health Organization (WHO) revwased glossary of ART terminology, 2009. FertilSteril. 2009;92:1520–4.
- Practice Committee of the American Society for Reproductive Medicine. Definitions of infertility and recurrent pregnancy loss. FertilSteril. 2008; 90(5 Suppl):S60. [CrossRef]
- Mascarenhas MN, Cheung H, Mathers CD, Stevens GA. Measuring infertility in populations: Constructing a standard definition for use with demographic and reproductive health surveys. Popul Health Metr. 2012; 10:17. [CrossRef]
- Boivin J, Bunting L, Collins JA, Nygren KG. International estimates of infertility prevalence and treatment-seeking: Potential need and demand for infertility medical care. Hum Reprod. 2007; 22:1506–12. [CrossRef]
- Calverton, Maryland, USA: ORC Macro and the World Health Organization; 2004. World Health Organization. Infecundity, Infertility, and Childlessness in Developing Countries. DHS Comparative Reports No 9.
- Sciarra J. Infertility: An international health problem. Int J Gynaecol Obstet. 1994; 46:155–63.
- Population Council. New Delhi: Population Council; 2004. Infertility. Looking Back, Looking Forward: A Profile of Sexual and Reproductive Health in India; pp. 67–72.
- Boericke W. Pocket Manual of Homoeopathic MateriaMedica& Repertory: Comprwasing of the Characterwastic and Guiding Symptoms of All Remedies (clinical and Pahtogenetic [sic]) Including Indian Drugs. B. Jain publwashers; 2002.
- Kent JT. Lectures on Homoeopathic MateriaMedica: Together with Kent’s” New Remedies” Incorporated and Arranged in One Alphabetical Order. B. Jain Publwashers; 1984.
- Murphy R. Homoeopathic Medical Repertory (Iind Ed.). B. Jain Publwashers; 1998.
- Mittal, Suneeta. “Investigating infertility.” (2018): 356-357. [CrossRef]
- Udachankar SM, Daddikar P, Patil AS, Jadhav AB, Gizare DV, Dole SM, Udachankar SM, Daddikar P, Patil AS, Jadhav AB, Gizare DV. Evaluation of role of homoeopathic treatment in unexplained infertility. 2018 Oct; 5 (04):7-17.
- Gerhard I, Wallis E. Individualized homeopathic therapy for male infertility. Homeopathy. 2002 Jul; 91(03):133-44. [CrossRef]
- Wheeler KM, Sharma D, Kavoussi PK, Smith RP, Costabile R. Clomiphene Citrate for the Treatment of Hypogonadism. Sexual medicine reviews. 2018 Dec 3. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).