Submitted:
18 March 2025
Posted:
21 March 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
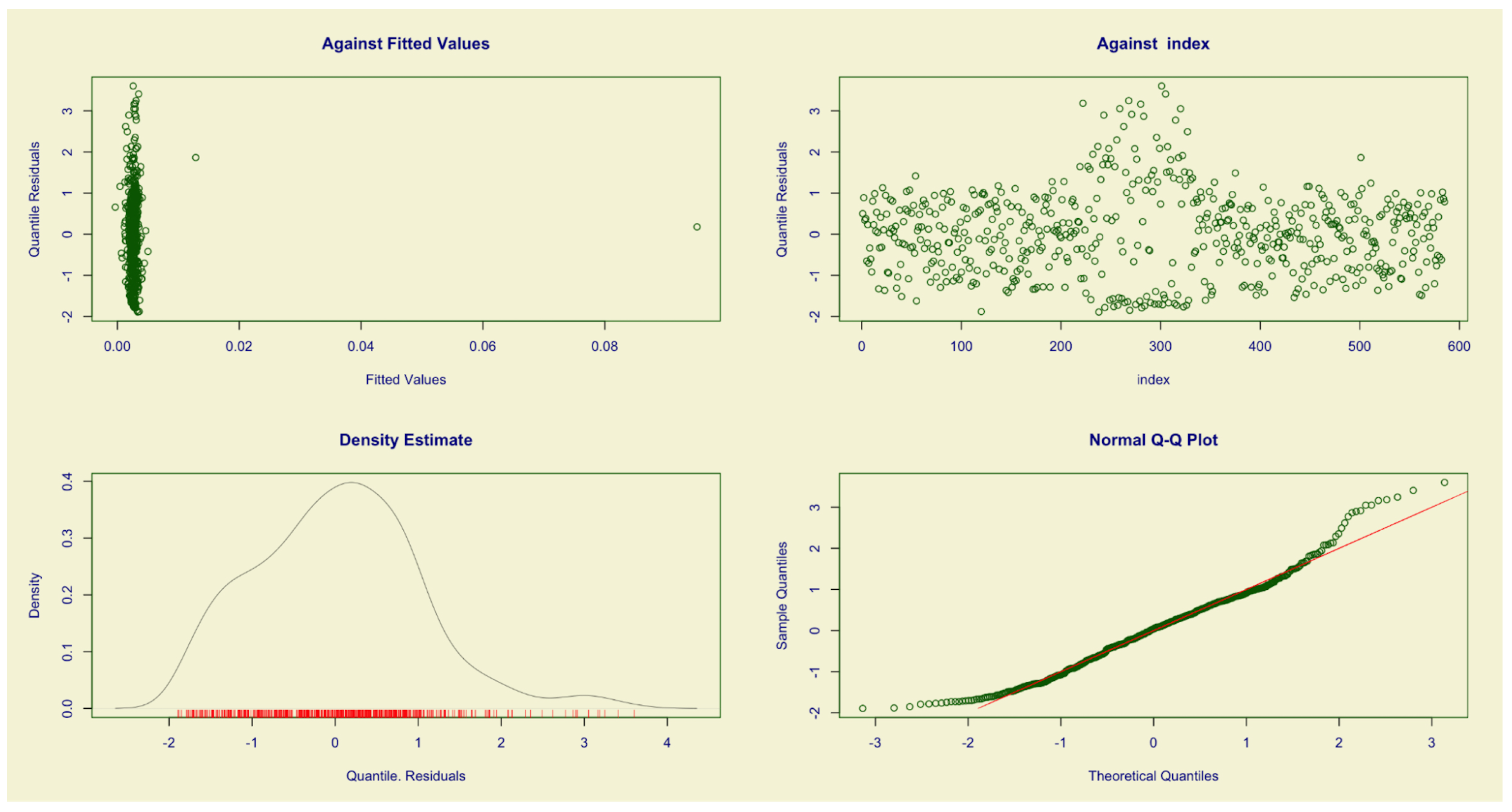
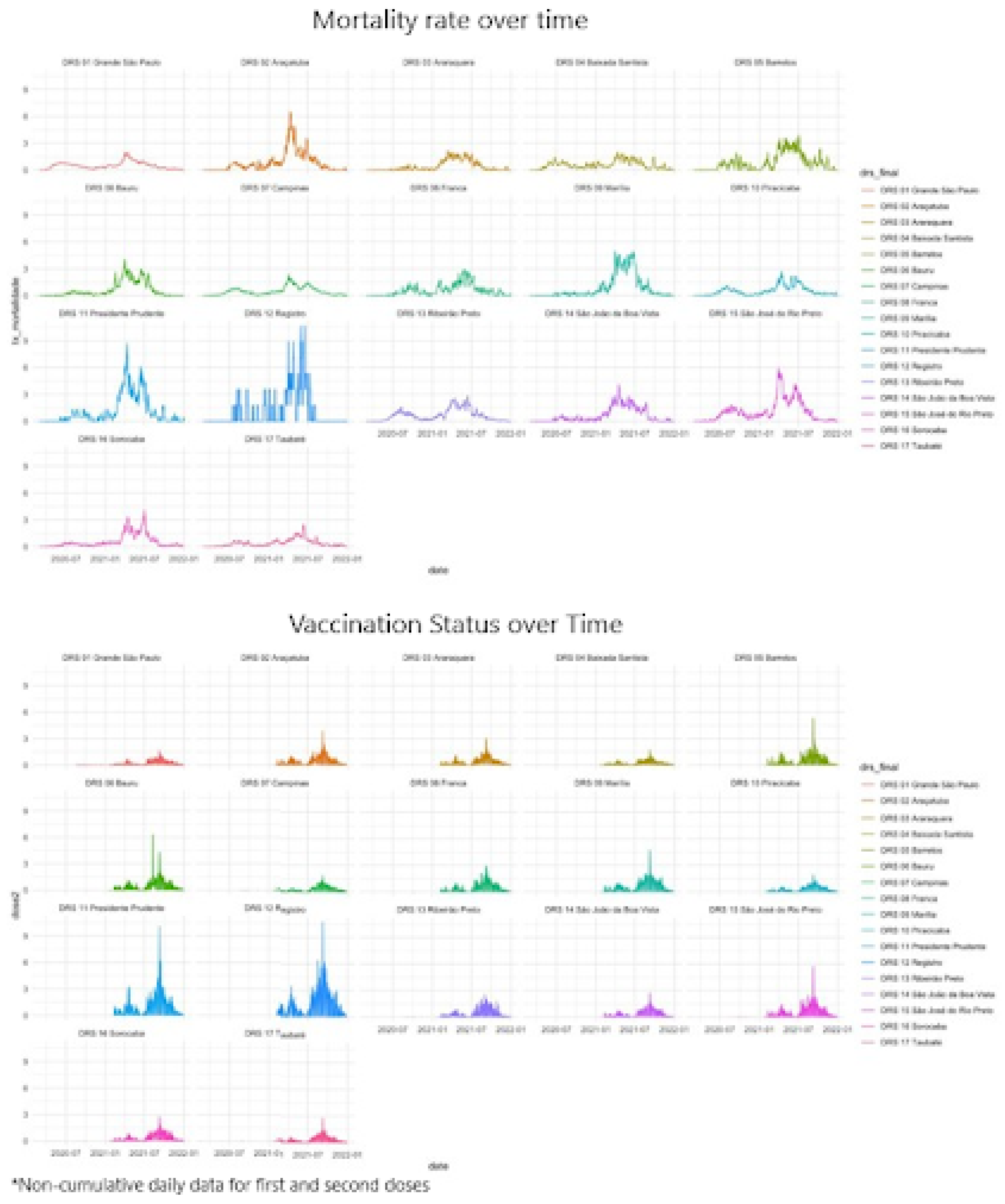
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Barbosa, T. P., Costa, F. B., Ramos, A. C. V., Berra, T. Z., Arroyo, L. H., Alves, Y. M., Santos, F. L., & Arcêncio, R. A. (2022). Morbimortalidade por COVID-19 associada a condições crônicas, serviços de saúde e iniquidades: evidências de sindemia. Revista Panamericana de Salud Pública, 46(1), 1. Available from. [CrossRef]
- Arcêncio, R. (2021). Reiterando o sentido da epidemiologia social na compreensão das desigualdades e avanço da equidade em tempos da COVID-19. ihmt. Available from: https://anaisihmt.com/index.php/ihmt/article/view/375.
- Lima Kubo, H. K., Campiolo, E. L., Ochikubo, G. T., & Batista, G. (2020). Impacto da pandemia do COVID19 no serviço de saúde: uma revisão de literatura. Interamerican Journal of Medicine and Health, 3. Available from. [CrossRef]
- Secretaria de Estado da Saúde de São Paulo. (2020). Plano de Contingência do Estado de São Paulo para a Infecção Humana pelo novo Coronavírus (SARS-CoV-2). Available from: https://www.saude.sp.gov.br/resources/ccd/homepage/covid-19/versao_final_finalplano_de_contigencia_03_04_rev_3.pdf.
- Secretaria de Estado da Saúde de São Paulo. (2012). Estado de São Paulo, segundo Departamentos de Saúde. Available from: https://www.saude.sp.gov.br/ses/institucional/departamentos-regionais-de-saude/regionais-de-saude.
- Secretaria da Saúde. (2023). Departamentos Regionais de Saúde - Secretaria da Saúde - Governo do Estado de São Paulo. Available from: https://saude.sp.gov.br/ses/institucional/departamentos-regionais-de-saude/ [cited 2023 Oct 5].
- IBGE. (2022). São Paulo | Cidades e Estados | IBGE. Available from: https://www.ibge.gov.br/cidades-e-estados/sp.html.
- Butantan. (2022). Vacinação contra COVID-19 no Brasil completa 1 ano com grande impacto da CoronaVac na redução de hospitalizações e mortes. Available from: https://butantan.gov.br/noticias/vacinacao-contra-covid-19-no-brasil-completa-1-ano-com-grande-impacto-da-coronavac-na-reducao-de-hospitalizacoes-e-mortes.
- Brasil. Fundação Sistema Estadual de Análise de Dados (SEADE). (2022). Dados Abertos. Available from: https://github.com/seade-R/dados-covid-sp.
- Brasil. Ministério da Saúde. DATASUS. (2022). COVID-19 - Vacinação. Available from: https://opendatasus.saude.gov.br/dataset/covid-19-vacinacao/.
- Cleveland, W. S., & Grosse, E. (1991). Computational methods for local regression. Statistics and Computing, 1(1), 47–62. Available from. [CrossRef]
- Box, G. E., & Cox, D. R. (1964). An analysis of transformations. Journal of the Royal Statistical Society: Series B (Methodological), 26(2), 211–243. Available from. [CrossRef]
- Heller, G. Z., Stasinopoulos, M. D., Rigby, R. A., & Bastiani, F. D. (2019). Distributions for Modeling Location, Scale, and Shape: Using GAMLSS in R. Taylor & Francis Group.
- Akaike, H. (1974). A new look at statistical model identification. IEEE Transactions on Automatic Control, 19(6), 716–723. Available from. [CrossRef]
- Azzalini, A., & Capitanio, A. (2003). Distributions generated by perturbation of symmetry with emphasis on a multivariate skew t-distribution. Journal of the Royal Statistical Society: Series B (Statistical Methodology), 65(2), 367–389. Available from. [CrossRef]
- World Health Organization (WHO). (2020). Coronavirus Disease (COVID-19) Situation Reports. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- Barbosa, I. R., Galvão, M. H. R., Souza, T. A. de, Gomes, S. M., Medeiros, A. de A., & Lima, K. C. de. (2020). Incidence of and mortality from COVID-19 in the older Brazilian population and its relationship with contextual indicators: an ecological study. Revista Brasileira de Geriatria e Gerontologia, 23(1). Available from: https://www.scielo.br/pdf/rbgg/v23n1/pt_1809-9823-rbgg-23-01-e200171.pdf.
- Lorenz, C., Ferreira, P. M., Masuda, E. T., Lucas, P. C., Palasio, R. G., Nielsen, L., ... & Carvalhanas, T. R. (2021). COVID-19 no estado de São Paulo: a evolução de uma pandemia. Revista Brasileira de Epidemiologia, 24. Available from. [CrossRef]
- Gold, M. S., Sehayek, D., Gabrielli, S., Zhang, X., McCusker, C., & Ben-Shoshan, M. (2020). COVID-19 and comorbidities: a systematic review and meta-analysis. Postgraduate Medicine, 132(8), 749–755. Available from. [CrossRef]
- Wang, Z., Deng, H., Ou, C., Liang, J., Wang, Y., Jiang, M., & Li, S. (2020). Clinical symptoms, comorbidities and complications in severe and non-severe patients with COVID-19. Medicine, 99(48), e23327. Available from. [CrossRef]
- Jain, V., & Yuan, J. M. (2020). Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis. International Journal of Public Health, 65(5), 533–546. Available from. [CrossRef]
- Kumar, A., Arora, A., Sharma, P., Anikhindi, S. A., Bansal, N., Singla, V., ... & Srivastava, A. (2020). Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(4), 535–545. Available from. [CrossRef]
- Sentongo, P., Ssentongo, A. E., Heilbrunn, E. S., Ba, D. M., & Chinchilli, V. M. (2020). Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis. PLOS ONE, 15(8), e0238215. Available from. [CrossRef]
- The Lancet. (2020). COVID-19: a new lens for non-communicable diseases. The Lancet, 396(10252), 649. Available from. [CrossRef]
- Clark, A., Jit, M., Warren-Gash, C., Guthrie, B., Wang, H. H., Mercer, S. W., ... & et al. (2020). Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. The Lancet Global Health, 8(8), e1003–e1017. Available from. [CrossRef]
- Azarpazhooh, M. R., Morovatdar, N., Avan, A., Phan, T. G., Divani, A. A., Yassi, N., ... & Di Napoli, M. (2020). COVID-19 pandemic and burden of non-communicable diseases: An ecological study on data of 185 countries. Journal of Stroke and Cerebrovascular Diseases, 29(9), 105089. Available from. [CrossRef]
- Kluge, H. H., Wickramasinghe, K., Rippin, H. L., Mendes, R., Peters, D. H., Kontsevaya, A., & Breda, J. (2020). Prevention and control of non-communicable diseases in the COVID-19 response. The Lancet, 395(10238), 1678–1680. Available from. [CrossRef]
- Richardson, S., Hirsch, J. S., Narasimhan, M., Crawford, J. M., McGinn, T., Davidson, K. W., ... & et al. (2020). Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA, 323(20), 2052. Available from. [CrossRef]
- Shahid, Z., Kalayanamitra, R., McClafferty, B., Kepko, D., Ramgobin, D., Patel, R., ... & Jain, R. (2020). COVID-19 and older adults: What we know. Journal of the American Geriatrics Society, 68(5), 926–929. Available from. [CrossRef]
- Barbosa, I. R., Galvão, M. H., Souza, T. A., Gomes, S. M., Medeiros, A. D., & Lima, K. C. (2020). Incidence of and mortality from COVID-19 in the older Brazilian population and its relationship with contextual indicators: an ecological study. Revista Brasileira de Geriatria e Gerontologia, 23(1). Available from. [CrossRef]
- Curtin, S. C., & Heron, M. (2022). COVID-19 death rates in urban and rural areas: United States, 2020. NCHS Data Brief, no 447. Hyattsville, MD: National Center for Health Statistics. Available from: . [CrossRef]
- Mecha López, R. (2021). Review of: Méndez Gutiérrez del Valle, R. (2020). Besieged by the pandemic. From collapse to reconstruction: geographic notes. Espacio Tiempo y Forma. Series VI, Geography, 14, 227–232. Available from. [CrossRef]
- Guimarâes, R. B., Catão, R. D., Martinuci, O. D., Pugliesi, E. A., & Matsumoto, P. S. (2020). O raciocínio geográfico e as chaves de leitura da Covid-19 no território brasileiro. Estudos Avançados, 34(99), 119–140. Available from. [CrossRef]
- De Castro Leiva, G., Dos Reis, D. S., & Filho, R. D. (2020). Estrutura urbana e mobilidade populacional: implicações para o distanciamento social e disseminação da Covid-19. Revista Brasileira de Estudos de População, 37, 1–22. Available from. [CrossRef]
- Velavan, T. P., & Meyer, C. G. (2020). The COVID-19 epidemic. Tropical Medicine & International Health, 25(3), 278–280. Available from. [CrossRef]
- Lau, H., Khosrawipour, V., Kocbach, P., Mikolajczyk, A., Schubert, J., Bania, J., ... & Khosrawipour, T. (2020). The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. Journal of Travel Medicine, 27(3). Available from. [CrossRef]
- Sathler, D., & Leiva, G. (2022). A cidade importa: urbanização, análise regional e segregação urbana em tempos de pandemia de Covid-19. Revista Brasileira de Estudos de População, 39, 1–30. Available from. [CrossRef]
- Couto, M. T., Barbieri, C. L., & Mattos, C. C. (2021). Considerações sobre o impacto da covid-19 na relação indivíduo-sociedade: da hesitação vacinal ao clamor por uma vacina. Saúde e Sociedade, 30(1). Available from. [CrossRef]
- Orellana, J. D., Cunha, G. M., Marrero, L., Leite, I. D., Domingues, C. M., & Horta, B. L. (2022). Mudanças no padrão de internações e óbitos por COVID-19 após substancial vacinação de idosos em Manaus, Amazonas, Brasil. Cadernos de Saúde Pública, 38(5). Available from. [CrossRef]
- Orellana, J. D., Cunha, G. M., Marrero, L., Horta, B. L., & Leite, I. D. (2020). Explosão da mortalidade no epicentro amazônico da epidemia de COVID-19. Cadernos de Saúde Pública, 36(7). Available from. [CrossRef]

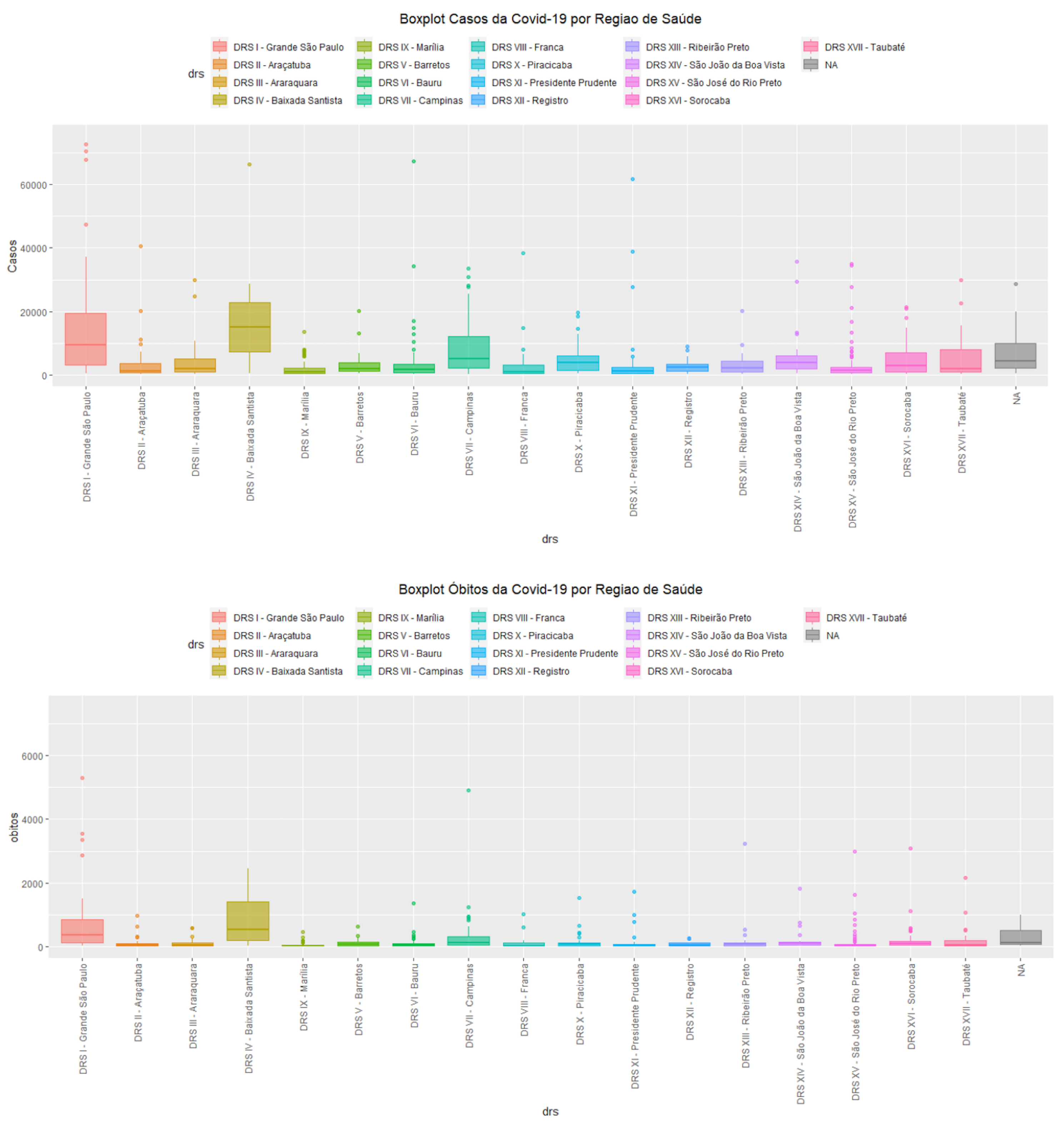
| Dimension | Variables | Data Source |
|---|---|---|
| COVID-19 | COVID-19 mortality rate per 100,000 inhabitants | SEADE |
| Health Indicators | Applied doses (COVID-19 vaccines; 1st and 2nd doses) | DATASUS |
| Deaths from non-communicable chronic diseases | DATASUS | |
| Social Indicators | General population | IBGE |
| Population by age group | SEADE | |
| Urban population | IBGE | |
| Gini index | DATASUS |
| Variable | Min | Median | Average | Max |
|---|---|---|---|---|
| Mortality rate per 100,000 inhabitants | 0 | 0.0032 | 0.0067 | 0.4979 |
| Deaths from chronic non-communicable diseases (% of total population) | 0 | 0.0019 | 0.0197 | 0.8615 |
| Population aged 0-14 years (% of total population) | 7.40 | 21.44 | 21.31 | 30.49 |
| Population aged 15-60 years (% of total population) | 57.09 | 65.38 | 68.91 | 2177.64 |
| Population aged 61+ years (% of total population) | 6.15 | 13.04 | 13.12 | 25.02 |
| Urban population (% of total population) | 24.90 | 88.7 | 84.85 | 100 |
| Gini index (range 0-1) | 0 | 0.4573 | 0.4586 | 0.6858 |
| COVID-19 Vaccination Coverage | 0.10 | 84.36 | 90.76 | 2986.84 |
| Variable | Estimate | Std. Error | t value | P value | Relative Increase (%) |
|---|---|---|---|---|---|
| (Intercept) | -2.28 | 0.671 | -3.391 | 0.000743 *** | - |
| V2 | -1.37 | 0.653 | -2.091 | 0.036939 * | -74.59 |
| V4 | 0.0002 | 0.0008 | 0.246 | 0.805826 | - |
| V5 | 0.0827 | 0.0169 | 4.902 | 1.23e-06 *** | 8.62 |
| V9 | 0.0235 | 0.0036 | 6.572 | 1.11e-10 *** | 2.38 |
| V10 | -0.930 | 0.871 | -1.068 | 0.286068 | - |
| V11 | 0.0268 | 0.0044 | 6.075 | 2.25e-09 *** | 2.72 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





