Submitted:
27 December 2024
Posted:
27 December 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methodology
- (i)
- Clinical or Symptom Characterization (“Symptom Characterization”): Research that primarily aims to identify, list, or quantify the variety of Long COVID symptoms, usually from social media data. The studies may include statistical analysis but do not necessarily perform extensive sentiment or topic modeling. Their main motivation is to gather clinical or epidemiological insights from user posts.
- (ii)
- Advanced NLP or Computational Methods (“NLP and Modeling”): Studies that specifically emphasize methods like deep transformer networks, topic modeling, sentiment analysis, and other elaborate computational approaches. This goes beyond a simple symptom count; it highlights a methods-heavy lens on analyzing data.
- (iii)
- Policy, Advocacy, or Public Health Communication (“Policy and Advocacy”): Papers exploring how organizations, governments, or communities develop health communications, handle policy issues, and communicate guidelines.
- (iv)
- Online Communities & Social Support (“Community and Support”): Studies focusing on how individuals find emotional or experiential support on social media, the way they exchange personal stories, or how group dynamics form around shared experiences. The main emphasis is on the psychosocial aspect, and the support social media platforms provide.


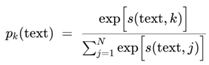
3. Results of Zero-Shot Classification
4. Review of Papers
4.1. NLP and Modeling
4.2. Policy and Advocacy
4.3. Community and Support
4.4. Symptom Characterization
5. Research Gaps and Future Directions
6. Conclusion
Author Contributions
Funding
Institutional Review Board Statement’
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ciotti, M., Ciccozzi, M., Terrinoni, A., Jiang, W.-C., Wang, C.-B., Bernardini, S.: The COVID-19 pandemic. Crit. Rev. Clin. Lab. Sci. 57, 365–388 (2020). [CrossRef]
- Velavan, T.P., Meyer, C.G.: The COVID-19 epidemic. Trop. Med. Int. Health. 25, 278–280 (2020). [CrossRef]
- Yesudhas, D., Srivastava, A., Gromiha, M.M.: COVID-19 outbreak: history, mechanism, transmission, structural studies and therapeutics. Infection. 49, 199–213 (2021). [CrossRef]
- Allen, D.W.: Covid-19 lockdown cost/benefits: A critical assessment of the literature. Int. J. Econ. Bus. 29, 1–32 (2022). [CrossRef]
- Cucinotta, D., Vanelli, M.: WHO Declares COVID-19 a Pandemic. Acta Biomed. Ateneo Parmense. 91, 157–160 (2020). [CrossRef]
- COVID-19 cases. https://covid19.who.int/, last accessed 2024/12/23.
- Raveendran, A.V., Jayadevan, R., Sashidharan, S.: Long COVID: An overview. Diabetes Metab. Syndr. 15, 869–875 (2021). [CrossRef]
- Altmann, D.M., Whettlock, E.M., Liu, S., Arachchillage, D.J., Boyton, R.J.: The immunology of long COVID. Nat. Rev. Immunol. 23, 618–634 (2023). [CrossRef]
- Fernández-de-las-Peñas, C.: Long COVID: current definition. Infection. 50, 285–286 (2022). [CrossRef]
- CDC: Long COVID basics. https://www.cdc.gov/covid/long-term-effects/index.html, last accessed 2024/12/23.
- Committee on Examining the Working Definition for Long COVID, Board on Health Sciences Policy, Board on Global Health, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine: A long COVID definition: A chronic, systemic disease state with profound consequences, (2024). [CrossRef]
- Aiyegbusi, O.L., Hughes, S.E., Turner, G., Rivera, S.C., McMullan, C., Chandan, J.S., Haroon, S., Price, G., Davies, E.H., Nirantharakumar, K., Sapey, E., Calvert, M.J., on behalf of the TLC Study Group: Symptoms, complications and management of long COVID: a review. J. R. Soc. Med. 114, 428–442 (2021). [CrossRef]
- Subramanian, A., Nirantharakumar, K., Hughes, S., Myles, P., Williams, T., Gokhale, K.M., Taverner, T., Chandan, J.S., Brown, K., Simms-Williams, N., Shah, A.D., Singh, M., Kidy, F., Okoth, K., Hotham, R., Bashir, N., Cockburn, N., Lee, S.I., Turner, G.M., Gkoutos, G.V., Aiyegbusi, O.L., McMullan, C., Denniston, A.K., Sapey, E., Lord, J.M., Wraith, D.C., Leggett, E., Iles, C., Marshall, T., Price, M.J., Marwaha, S., Davies, E.H., Jackson, L.J., Matthews, K.L., Camaradou, J., Calvert, M., Haroon, S.: Symptoms and risk factors for long COVID in non-hospitalized adults. Nat. Med. 28, 1706–1714 (2022). [CrossRef]
- Sudre, C.H., Murray, B., Varsavsky, T., Graham, M.S., Penfold, R.S., Bowyer, R.C., Pujol, J.C., Klaser, K., Antonelli, M., Canas, L.S., Molteni, E., Modat, M., Jorge Cardoso, M., May, A., Ganesh, S., Davies, R., Nguyen, L.H., Drew, D.A., Astley, C.M., Joshi, A.D., Merino, J., Tsereteli, N., Fall, T., Gomez, M.F., Duncan, E.L., Menni, C., Williams, F.M.K., Franks, P.W., Chan, A.T., Wolf, J., Ourselin, S., Spector, T., Steves, C.J.: Attributes and predictors of long COVID. Nat. Med. 27, 626–631 (2021). [CrossRef]
- Notarte, K.I., Catahay, J.A., Velasco, J.V., Pastrana, A., Ver, A.T., Pangilinan, F.C., Peligro, P.J., Casimiro, M., Guerrero, J.J., Gellaco, M.M.L., Lippi, G., Henry, B.M., Fernández-de-las-Peñas, C.: Impact of COVID-19 vaccination on the risk of developing long-COVID and on existing long-COVID symptoms: A systematic review. EClinicalMedicine. 53, 101624 (2022). [CrossRef]
- Cabrera Martimbianco, A.L., Pacheco, R.L., Bagattini, Â.M., Riera, R.: Frequency, signs and symptoms, and criteria adopted for long COVID-19: A systematic review. Int. J. Clin. Pract. 75, (2021). [CrossRef]
- Ayoubkhani, D., Bermingham, C., Pouwels, K.B., Glickman, M., Nafilyan, V., Zaccardi, F., Khunti, K., Alwan, N.A., Walker, A.S.: Trajectory of long covid symptoms after covid-19 vaccination: community based cohort study. BMJ. 377, e069676 (2022). [CrossRef]
- Davis, H.E., Assaf, G.S., McCorkell, L., Wei, H., Low, R.J., Re’em, Y., Redfield, S., Austin, J.P., Akrami, A.: Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 38, 101019 (2021). [CrossRef]
- Yong, S.J.: Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect. Dis. (Lond.). 53, 737–754 (2021). [CrossRef]
- Koc, H.C., Xiao, J., Liu, W., Li, Y., Chen, G.: Long COVID and its management. Int. J. Biol. Sci. 18, 4768–4780 (2022). [CrossRef]
- Al-Aly, Z., Davis, H., McCorkell, L., Soares, L., Wulf-Hanson, S., Iwasaki, A., Topol, E.J.: Long COVID science, research and policy. Nat. Med. 30, 2148–2164 (2024). [CrossRef]
- Tana, C., Bentivegna, E., Cho, S.-J., Harriott, A.M., García-Azorín, D., Labastida-Ramirez, A., Ornello, R., Raffaelli, B., Beltrán, E.R., Ruscheweyh, R., Martelletti, P.: Long COVID headache. J. Headache Pain. 23, (2022). [CrossRef]
- Peluso, M.J., Deeks, S.G.: Mechanisms of long COVID and the path toward therapeutics. Cell. 187, 5500–5529 (2024). [CrossRef]
- Greenhalgh, T., Sivan, M., Perlowski, A., Nikolich, J.Ž.: Long COVID: a clinical update. Lancet. 404, 707–724 (2024). [CrossRef]
- Sykes, D.L., Holdsworth, L., Jawad, N., Gunasekera, P., Morice, A.H., Crooks, M.G.: Post-COVID-19 symptom burden: What is long-COVID and how should we manage it? Lung. 199, 113–119 (2021). [CrossRef]
- Tsao, S.-F., Chen, H., Tisseverasinghe, T., Yang, Y., Li, L., Butt, Z.A.: What social media told us in the time of COVID-19: a scoping review. Lancet Digit. Health. 3, e175–e194 (2021). [CrossRef]
- Thakur, N.: Social media mining and analysis: A brief review of recent challenges. Information (Basel). 14, 484 (2023). [CrossRef]
- Gottlieb, M., Dyer, S.: Information and disinformation: Social media in the COVID-19 crisis. Acad. Emerg. Med. 27, 640–641 (2020). [CrossRef]
- Thakur, N., Han, C.: An exploratory study of tweets about the SARS-CoV-2 Omicron variant: Insights from sentiment analysis, language interpretation, source tracking, type classification, and embedded URL detection. COVID. 2, 1026–1049 (2022). [CrossRef]
- Hussain, W.: Role of social media in COVID-19 pandemic. Int J Front Sci. 4, (2024). [CrossRef]
- Thakur, N.: Sentiment analysis and text analysis of the public discourse on Twitter about COVID-19 and MPox. Big Data Cogn. Comput. 7, 116 (2023). [CrossRef]
- Shoaei, M.D., Dastani, M.: The role of Twitter during the COVID-19 crisis: A systematic literature review. Acta Inform. Pragensia. 9, 154–169 (2020). [CrossRef]
- Thakur, N., Cui, S., Khanna, K., Knieling, V., Duggal, Y.N., Shao, M.: Investigation of the gender-specific discourse about online learning during COVID-19 on Twitter using sentiment analysis, subjectivity analysis, and toxicity analysis. Computers. 12, 221 (2023). [CrossRef]
- Southwick, L., Guntuku, S.C., Klinger, E.V., Seltzer, E., McCalpin, H.J., Merchant, R.M.: Characterizing COVID-19 content posted to TikTok: Public sentiment and response during the first phase of the COVID-19 pandemic. J. Adolesc. Health. 69, 234–241 (2021). [CrossRef]
- Patel, K.A., Thakur, N.: Dissemination of misinformation about COVID-19 on TikTok: A multimodal analysis. In: Communications in Computer and Information Science. pp. 109–120. Springer Nature Switzerland, Cham (2024).
- Rovetta, A., Bhagavathula, A.S.: Global infodemiology of COVID-19: Analysis of Google web searches and Instagram hashtags. J. Med. Internet Res. 22, e20673 (2020). [CrossRef]
- Thakur, N.: Five years of COVID-19 discourse on Instagram: A labeled Instagram dataset of over half a million posts for multilingual sentiment analysis. In: 2024 7th International Conference on Machine Learning and Natural Language Processing (MLNLP). pp. 1–10. IEEE (2024).
- Mejova, Y., Kalimeri, K.: COVID-19 on Facebook ads: Competing agendas around a public health crisis. In: Proceedings of the 3rd ACM SIGCAS Conference on Computing and Sustainable Societies. pp. 22–31. ACM, New York, NY, USA (2020).
- Perrotta, D., Grow, A., Rampazzo, F., Cimentada, J., Del Fava, E., Gil-Clavel, S., Zagheni, E.: Behaviours and attitudes in response to the COVID-19 pandemic: insights from a cross-national Facebook survey. EPJ Data Sci. 10, 17 (2021). [CrossRef]
- Li, H.O.-Y., Bailey, A., Huynh, D., Chan, J.: YouTube as a source of information on COVID-19: a pandemic of misinformation? BMJ Glob. Health. 5, e002604 (2020). [CrossRef]
- Thakur, N., Cui, S., Knieling, V., Khanna, K., Shao, M.: Investigation of the misinformation about COVID-19 on YouTube using topic modeling, sentiment analysis, and language analysis. Computation (Basel). 12, 28 (2024). [CrossRef]
- Veselovsky, V., Anderson, A.: Reddit in the time of COVID. Proceedings of the International AAAI Conference on Web and Social Media. 17, 878–889 (2023). [CrossRef]
- Nirmalya, T., Kesha, A.P., Audrey, P., Shuqi, C., Nazif, A., Rishika, S., Riyan, S.: Quantifying public response to COVID-19 events: Introducing the Community Sentiment and Engagement Index. https://arxiv.org/abs/2412.16925, (2024).
- Daglis, T., Tsagarakis, K.P.: A LinkedIn-based analysis of the U.S. dynamic adaptations in healthcare during the COVID-19 pandemic. Healthcare Analytics. 5, 100291 (2024). [CrossRef]
- Pardim, V.I., Pinochet, L.H.C., Souza, C.A., Viana, A.B.N.: The behavior of young people at the beginning of their career through LinkedIn. RAM Rev. Adm. Mackenzie. 23, eRAMG220064 (2022). [CrossRef]
- Hinchey, L., Michon, A., Drews, J., Price, M., Christian, J., Pernice, F., Aquila, R.: Clubhouses as essential communities during the COVID-19 pandemic. J. Psychosoc. Rehabil. Ment. Health. 9, 149–157 (2022). [CrossRef]
- Junaid, S., Mutschler, C., McShane, K., The Canadian Clubhouse Research Group: The impact of COVID-19 on clubhouse employment programs. Community Ment. Health J. 59, 523–530 (2023). [CrossRef]
- Ayob, M.A., Hadi, N.A., Ezad, M., Pahroraji, H.M., Ismail, B., Saaid, M.N.F.: Promoting ‘Discord’ as a platform for learning engagement during Covid-19 pandemic. Asian J. Univ. Educ. 18, 663–673 (2022). [CrossRef]
- Ardiyansah, T.Y., Batubara, R.W., Auliya, P.K.: Using discord to facilitate students in teaching learning process during COVID-19 outbreak. Journal of English Teaching, Literature, and Applied Linguistics. 5, 76 (2021). [CrossRef]
- Yang, Q., Wang, W., Pierce, L., Vaish, R., Shi, X., Shah, N.: Online communication shifts in the midst of the Covid-19 pandemic: A case study on Snapchat. Proceedings of the International AAAI Conference on Web and Social Media. 15, 830–840 (2021). [CrossRef]
- Spieler, B., Batte, C., Mackey, D., Henry, C., Danrad, R., Sabottke, C., Pirtle, C., Mussell, J., Wallace, E.: Diagnosis in a snap: a pilot study using Snapchat in radiologic didactics. Emerg. Radiol. 28, 93–102 (2021). [CrossRef]
- Yue, Z., Zhang, R., Xiao, J.: Social media use, perceived social support, and well-being: Evidence from two waves of surveys peri- and post-COVID-19 lockdown. J. Soc. Pers. Relat. 41, 1279–1297 (2024). [CrossRef]
- Thakur, N., Duggal, Y.N., Liu, Z.: Analyzing public reactions, perceptions, and attitudes during the MPox outbreak: Findings from Topic Modeling of Tweets. Computers. 12, 191 (2023). [CrossRef]
- Thakur, N.: MonkeyPox2022Tweets: A large-scale Twitter dataset on the 2022 Monkeypox outbreak, findings from analysis of Tweets, and open research questions. Infect. Dis. Rep. 14, 855–883 (2022). [CrossRef]
- Perego, E.: #LongCovid. https://twitter.com/elisaperego78/status/1263172084055838721?s=20, last accessed 2024/12/23.
- Thakur, N., Cho, H., Cheng, H., Lee, H.: Analysis of user diversity-based patterns of public discourse on twitter about mental health in the context of online learning during COVID-19. In: Lecture Notes in Computer Science. pp. 367–389. Springer Nature Switzerland, Cham (2023).
- Schillinger, D., Chittamuru, D., Ramírez, A.S.: From “infodemics” to health promotion: A novel framework for the role of social media in public health. Am. J. Public Health. 110, 1393–1396 (2020). [CrossRef]
- Thakur, N., Patel, K.A., Poon, A., Shah, R., Azizi, N., Han, C.: A comprehensive analysis and investigation of the public discourse on twitter about exoskeletons from 2017 to 2023. Future Internet. 15, 346 (2023). [CrossRef]
- Pourpanah, F., Abdar, M., Luo, Y., Zhou, X., Wang, R., Lim, C.P., Wang, X.-Z., Wu, Q.M.J.: A review of generalized zero-shot learning methods. IEEE Trans. Pattern Anal. Mach. Intell. 45, 1–20 (2022). [CrossRef]
- Romera-Paredes, B., Torr, P.H.S.: An embarrassingly simple approach to zero-shot learning. ICML. 37, 2152–2161 (07--09 Jul 2015). [CrossRef]
- Wang, W., Zheng, V.W., Yu, H., Miao, C.: A survey of zero-shot learning: Settings, methods, and applications. ACM Trans. Intell. Syst. Technol. 10, 1–37 (2019). [CrossRef]
- Fu, Y.: Investigating public perceptions regarding the Long COVID on Twitter using sentiment analysis and topic modeling. Med. Data Min. (2022). [CrossRef]
- Rushforth, A., Ladds, E., Wieringa, S., Taylor, S., Husain, L., Greenhalgh, T.: Long Covid – The illness narratives. Soc. Sci. Med. 286, 114326 (2021). [CrossRef]
- Russell, D., Spence, N.J., Chase, J.-A.D., Schwartz, T., Tumminello, C.M., Bouldin, E.: Support amid uncertainty: Long COVID illness experiences and the role of online communities. SSM Qual. Res. Health. 2, 100177 (2022). [CrossRef]
- Meledandri, F.: The impact of polarised social media networking communications in the #longcovid debate between ideologies and scientific facts, (2024). [CrossRef]
- Singh, S.M., Reddy, C.: An analysis of self-reported longcovid symptoms on twitter, (2020). [CrossRef]
- Ziauddeen, N., Gurdasani, D., O’Hara, M.E., Hastie, C., Roderick, P., Yao, G., Alwan, N.A.: Characteristics of Long Covid: findings from a social media survey, (2021). [CrossRef]
- Sarker, A., Ge, Y.: Long COVID symptoms from Reddit: Characterizing post-COVID syndrome from patient reports, (2021). [CrossRef]
- Banda, J.M., Adderley, N., Ahmed, W.-U.-R., AlGhoul, H., Alser, O., Alser, M., Areia, C., Cogenur, M., Fišter, K., Gombar, S., Huser, V., Jonnagaddala, J., Lai, L.Y.H., Leis, A., Mateu, L., Mayer, M.A., Minty, E., Morales, D., Natarajan, K., Paredes, R., Periyakoil, V.S., Prats-Uribe, A., Ross, E.G., Singh, G., Subbian, V., Vivekanantham, A., Prieto-Alhambra, D.: Characterization of long-term patient-reported symptoms of COVID-19: an analysis of social media data, (2021). [CrossRef]
- Massey, D., Berrent, D., Krumholz, H.: Breakthrough symptomatic COVID-19 infections leading to Long Covid: Report from Long Covid Facebook group poll, (2021). [CrossRef]
- Martin, S., Chepo, M., Déom, N., Khalid, A.F., Vindrola-Padros, C.: “#LongCOVID affects children too”: A Twitter analysis of healthcare workers’ sentiment and discourse about Long COVID in children and young people in the UK, (2022). [CrossRef]
- Dolatabadi, E., Moyano, D., Bales, M., Spasojevic, S., Bhambhoria, R., Bhatti, J., Debnath, S., Hoell, N., Li, X., Leng, C., Nanda, S., Saab, J., Sahak, E., Sie, F., Uppal, S., Vadlamudi, N.K., Vladimirova, A., Yakimovich, A., Yang, X., Kocak, S.A., Cheung, A.M.: Using social media to help understand long COVID patient reported health outcomes: A natural language processing approach, (2022). [CrossRef]
- Miao, L., Last, M., Litvak, M.: An interactive analysis of user-reported long COVID symptoms using twitter data. In: Hruschka, E., Mitchell, T., Mladenic, D., Grobelnik, M., and Bhutani, N. (eds.) Proceedings of the 2nd Workshop on Deriving Insights from User-Generated Text. pp. 10–19. Association for Computational Linguistics, Stroudsburg, PA, USA (2022).
- Guocheng, F., Huaiyu, C., Wei, Q.: Exploring the emotional and mental well-being of individuals with Long COVID through twitter analysis. https://arxiv.org/abs/2307.07558, (2023).
- Jordan, A., Park, A.: Understanding the long haulers of COVID-19: Mixed methods analysis of YouTube content. JMIR AI. 3, e54501 (2024). [CrossRef]
- Kusuma, I.Y., Suherman, S.: The pulse of long COVID on Twitter: A social network analysis. Arch. Iran. Med. 27, 36–43 (2024). [CrossRef]
- Thakur, N.: Investigating and analyzing self-reporting of Long COVID on Twitter: Findings from sentiment analysis. Appl. Syst. Innov. 6, 92 (2023). [CrossRef]
- Awoyemi, T., Ebili, U., Olusanya, A., Ogunniyi, K.E., Adejumo, A.V.: Twitter sentiment analysis of long COVID syndrome. Cureus. 14, e25901 (2022). [CrossRef]
- DIGITAL LONG-HAULER LIFELINES: UNDERSTANDING HOW PEOPLE WITH LONG COVID BUILD COMMUNITY ON REDDIT. https://www.researchgate.net/publication/385720439_Digital_Long-Hauler_Lifelines_Understanding_How_People_with_Long_Covid_Build_Community_on_Reddit, last accessed 2024/12/24.
- Bhattacharyya, A., Seth, A., Rai, S.: The effects of long COVID-19, its severity, and the need for immediate attention: Analysis of clinical trials and Twitter data. Front. Big Data. 5, (2022). [CrossRef]
- Matharaarachchi, S., Domaratzki, M., Katz, A., Muthukumarana, S.: Discovering long COVID symptom patterns: Association rule mining and sentiment analysis in social media tweets. JMIR Form. Res. 6, e37984 (2022). [CrossRef]
- Koss, J., Bohnet-Joschko, S.: Social media mining of long-COVID self-medication reported by Reddit users: Feasibility study to support drug repurposing. JMIR Form. Res. 6, e39582 (2022). [CrossRef]
- Ayadi, H., Bour, C., Fischer, A., Ghoniem, M., Fagherazzi, G.: The Long COVID experience from a patient’s perspective: a clustering analysis of 27,216 Reddit posts. Front. Public Health. 11, (2023). [CrossRef]
- Garrett, C., Aghaei, A., Aggarwal, A., Qiao, S.: The role of social media in the experiences of COVID-19 among long-hauler women: Qualitative study. JMIR Hum. Factors. 11, e50443 (2024). [CrossRef]
- Laestadius, L.I., Guidry, J.P.D., Bishop, A., Campos-Castillo, C.: State health department communication about long COVID in the United States on Facebook: Risks, prevention, and support. Int. J. Environ. Res. Public Health. 19, 5973 (2022). [CrossRef]
- Izquierdo-Condoy, J.S., Fernandez-Naranjo, R., Vasconez-González, E., Cordovez, S., Tello-De-la-Torre, A., Paz, C., Delgado-Moreira, K., Carrington, S., Viscor, G., Ortiz-Prado, E.: Long COVID at different altitudes: A countrywide epidemiological analysis. Int. J. Environ. Res. Public Health. 19, 14673 (2022). [CrossRef]
- Santarossa, S., Rapp, A., Sardinas, S., Hussein, J., Ramirez, A., Cassidy-Bushrow, A.E., Cheng, P., Yu, E.: Understanding the #longCOVID and #longhaulers conversation on Twitter: Multimethod study. JMIR Infodemiology. 2, e31259 (2022). [CrossRef]
- Déguilhem, A., Malaab, J., Talmatkadi, M., Renner, S., Foulquié, P., Fagherazzi, G., Loussikian, P., Marty, T., Mebarki, A., Texier, N., Schuck, S.: Identifying profiles and symptoms of patients with long COVID in France: Data mining infodemiology study based on social media. JMIR Infodemiology. 2, e39849 (2022). [CrossRef]
- Dolatabadi, E., Moyano, D., Bales, M., Spasojevic, S., Bhambhoria, R., Bhatti, J., Debnath, S., Hoell, N., Li, X., Leng, C., Nanda, S., Saab, J., Sahak, E., Sie, F., Uppal, S., Vadlamudi, N.K., Vladimirova, A., Yakimovich, A., Yang, X., Kocak, S.A., Cheung, A.M.: Using social media to help understand patient-reported health outcomes of post–COVID-19 condition: Natural language processing approach. J. Med. Internet Res. 25, e45767 (2023). [CrossRef]
- Ziauddeen, N., Gurdasani, D., O’Hara, M.E., Hastie, C., Roderick, P., Yao, G., Alwan, N.A.: Characteristics and impact of Long Covid: Findings from an online survey. PLoS One. 17, e0264331 (2022). [CrossRef]
- Segneri, L., Babina, N., Hammerschmidt, T., Fronzetti Colladon, A., Gloor, P.A.: Too much focus on your health might be bad for your health: Reddit user’s communication style predicts their Long COVID likelihood. PLoS One. 19, e0308340 (2024). [CrossRef]
- Singh, S.M., Reddy, S.C., Kathiravan, S.: An analysis of self-reported long COVID-19 symptoms on twitter. J. Postgrad. Med. Educ. Res. 57, 79–81 (2023). [CrossRef]
- Mining Long-COVID symptoms from Reddit: what we know so far. https://www.researchgate.net/profile/Abeed-Sarker/publication/352208391_Mining_Long-COVID_symptoms_from_Reddit_what_we_know_so_far/links/60bedc6ca6fdcc22eae8b87a/Mining-Long-COVID-symptoms-from-Reddit-what-we-know-so-far.pdf, last accessed 2024/12/24.
- Miyake, E., Martin, S.: Long Covid: Online patient narratives, public health communication and vaccine hesitancy. Digit. Health. 7, (2021). [CrossRef]
- Sarker, A., Ge, Y.: Mining long-COVID symptoms from Reddit: characterizing post-COVID syndrome from patient reports. JAMIA Open. 4, (2021). [CrossRef]
- Jordan, A.A.D.: Understanding the plight of covid-19 long haulers through computational analysis of YouTube content, (2022).
- Minel, B.J.A.: Using topic modeling and NLP tools for analyzing long Covid coverage by French press and Twitter. In: Nagar et al, A. (ed.) Intelligent Sustainable Systems, Lecture Notes in Networks and Systems 817. Springer Nature Singapore, Singapore (2024). [CrossRef]
- Ozduran, E., Büyükçoban, S.: A content analysis of the reliability and quality of Youtube videos as a source of information on health-related post-COVID pain. PeerJ. 10, e14089 (2022). [CrossRef]
- Déom, N., Khalid, A.F., Martin, S., Chepo, M., Vindrola-Padros, C.: Unlocking the mysteries of long COVID in children and young people: Insights from a policy review and social media analysis in the UK. https://osf.io/preprints/f48yg/, (2023). [CrossRef]
- Jacques, E.T., Basch, C.H., Park, E., Kollia, B., Barry, E.: Long haul COVID-19 videos on YouTube: Implications for health communication. J. Community Health. 47, 610–615 (2022). [CrossRef]
- Strain, W.D., Sherwood, O., Banerjee, A., Van der Togt, V., Hishmeh, L., Rossman, J.: The impact of COVID vaccination on symptoms of long COVID: An international survey of people with lived experience of long COVID. Vaccines (Basel). 10, 652 (2022). [CrossRef]
- Wongtavavimarn, K.: Social support and narrative sensemaking online: A content analysis of Facebook posts by COVID-19 long haulers. https://uh-ir.tdl.org/bitstream/handle/10657/10745/WONGTAVAVIMARN-THESIS-2022.pdf?sequence=1, last accessed 2024/12/24.
- Helmy, Y.A., Fawzy, M., Elaswad, A., Sobieh, A., Kenney, S.P., Shehata, A.A.: The COVID-19 pandemic: A comprehensive review of taxonomy, genetics, epidemiology, diagnosis, treatment, and control. J. Clin. Med. 9, 1225 (2020). [CrossRef]
- Gasser, U., Ienca, M., Scheibner, J., Sleigh, J., Vayena, E.: Digital tools against COVID-19: taxonomy, ethical challenges, and navigation aid. Lancet Digit. Health. 2, e425–e434 (2020). [CrossRef]
- Albahri, O.S., Zaidan, A.A., Albahri, A.S., Zaidan, B.B., Abdulkareem, K.H., Al-qaysi, Z.T., Alamoodi, A.H., Aleesa, A.M., Chyad, M.A., Alesa, R.M., Lim, C.K., Lakulu, M.M., Ibrahim, A.B., Rashid, N.A.: Systematic review of artificial intelligence techniques in the detection and classification of COVID-19 medical images in terms of evaluation and benchmarking: Taxonomy analysis, challenges, future solutions and methodological aspects. J. Infect. Public Health. 13, 1381–1396 (2020). [CrossRef]
- Awassa, L., Jdey, I., Dhahri, H., Hcini, G., Mahmood, A., Othman, E., Haneef, M.: Study of different deep learning methods for Coronavirus (COVID-19) pandemic: Taxonomy, survey and insights. Sensors (Basel). 22, 1890 (2022). [CrossRef]
- Shahid, Z., Kalayanamitra, R., McClafferty, B., Kepko, D., Ramgobin, D., Patel, R., Aggarwal, C.S., Vunnam, R., Sahu, N., Bhatt, D., Jones, K., Golamari, R., Jain, R.: COVID-19 and older adults: What we know. J. Am. Geriatr. Soc. 68, 926–929 (2020). [CrossRef]
- Thakur, N., Han, C.Y.: A study of fall detection in assisted living: Identifying and improving the optimal machine learning method. J. Sens. Actuator Netw. 10, 39 (2021). [CrossRef]
- Lebrasseur, A., Fortin-Bédard, N., Lettre, J., Raymond, E., Bussières, E.-L., Lapierre, N., Faieta, J., Vincent, C., Duchesne, L., Ouellet, M.-C., Gagnon, E., Tourigny, A., Lamontagne, M.-È., Routhier, F.: Impact of the COVID-19 pandemic on older adults: Rapid review. JMIR Aging. 4, e26474 (2021). [CrossRef]
- Thakur, N., Han, C.Y.: Multimodal approaches for Indoor Localization for Ambient Assisted Living in Smart Homes. Information (Basel). 12, 114 (2021). [CrossRef]
- Nanda, A., Vura, N.V.R.K., Gravenstein, S.: COVID-19 in older adults. Aging Clin. Exp. Res. 32, 1199–1202 (2020). [CrossRef]
- Miller, E.A.: Protecting and improving the lives of older adults in the COVID-19 era. J. Aging Soc. Policy. 32, 297–309 (2020). [CrossRef]
- Thakur, N., Han, C.Y.: Indoor localization for personalized ambient assisted living of multiple users in multi-floor smart environments. Big Data Cogn. Comput. 5, 42 (2021). [CrossRef]
- Saxon, S.V., Mary Jean Etten, EdD, GNP, CMP, FT, Elizabeth A. Perkins, PhD, RNLD, FAAIDD, FGSA: Physical Change and aging, Seventh Edition: A guide for Helping Professions. Springer Publishing Company (2021).
- Engelman, M., Jackson, H.: Gradual change, homeostasis, and punctuated equilibrium: Reconsidering patterns of health in later life. Demography. 56, 2323–2347 (2019). [CrossRef]
- Thakur, N., Han, C.Y.: An intelligent ubiquitous activity aware framework for smart home. In: Advances in Intelligent Systems and Computing. pp. 296–302. Springer International Publishing, Cham (2021).
- Busse, P.J., Mathur, S.K.: Age-related changes in immune function: Effect on airway inflammation. J. Allergy Clin. Immunol. 126, 690–699 (2010). [CrossRef]
- Howcroft, T.K., Campisi, J., Louis, G.B., Smith, M.T., Wise, B., Wyss-Coray, T., Augustine, A.D., McElhaney, J.E., Kohanski, R., Sierra, F.: The role of inflammation in age-related disease. Aging (Albany NY). 5, 84–93 (2013). [CrossRef]
- Pawelec, G., Goldeck, D., Derhovanessian, E.: Inflammation, ageing and chronic disease. Curr. Opin. Immunol. 29, 23–28 (2014). [CrossRef]
- Thakur, N., Han, C.Y.: A framework for facilitating human-human interactions to mitigate loneliness in elderly. In: Advances in Intelligent Systems and Computing. pp. 322–327. Springer International Publishing, Cham (2021).
- Novak, M.: Issues in aging. Routledge, Fourth edition. | New York, NY : Routledge, 2018. (2018).
- Silverstein, M.: Meeting the challenges of an aging workforce. Am. J. Ind. Med. 51, 269–280 (2008). [CrossRef]
- Thakur, N., Y. Han, C.: Pervasive activity logging for indoor localization in smart homes. In: 2021 4th International Conference on Data Science and Information Technology. pp. 246–255. ACM, New York, NY, USA (2021).
- Thakur, N., Han, C.Y.: An improved approach for complex activity recognition in smart homes. In: Lecture Notes in Computer Science. pp. 220–231. Springer International Publishing, Cham (2019).
- Thakur, N., Han, C.Y.: An activity analysis model for enhancing user experiences in affect aware systems. In: 2018 IEEE 5G World Forum (5GWF). pp. 516–519. IEEE (2018).
- Thakur, N., Han, C.Y.: A context-driven complex activity framework for smart home. In: 2018 IEEE 9th Annual Information Technology, Electronics and Mobile Communication Conference (IEMCON). pp. 801–806. IEEE (2018).
- Kogan, A.C., Wilber, K., Mosqueda, L.: Person-centered care for older adults with chronic conditions and functional impairment: A systematic literature review. J. Am. Geriatr. Soc. 64, (2016). [CrossRef]
- Matthew-Maich, N., Harris, L., Ploeg, J., Markle-Reid, M., Valaitis, R., Ibrahim, S., Gafni, A., Isaacs, S.: Designing, implementing, and evaluating mobile health technologies for managing chronic conditions in older adults: A scoping review. JMIR MHealth UHealth. 4, e29 (2016). [CrossRef]
- PACC Research Group, Anaby, D., Miller, W.C., Eng, J.J., Jarus, T., Noreau, L.: Participation and well-being among older adults living with chronic conditions. Soc. Indic. Res. 100, 171–183 (2011). [CrossRef]
- Ferrari, M., Harrison, B., Rawashdeh, O., Hammond, R., Avery, Y., Rawashdeh, M., Sa’deh, W., Maddens, M.: Clinical feasibility trial of a motion detection system for fall prevention in hospitalized older adult patients. Geriatr. Nurs. 33, 177–183 (2012). [CrossRef]
- Thakur, N., Han, C.Y.: A simplistic and cost-effective design for real-world development of an ambient assisted living system for fall detection and indoor localization: Proof-of-concept. Information (Basel). 13, 363 (2022). [CrossRef]
- Townsley, C.A., Chan, K.K., Pond, G.R., Marquez, C., Siu, L.L., Straus, S.E.: Understanding the attitudes of the elderly towards enrolment into cancer clinical trials. BMC Cancer. 6, (2006). [CrossRef]
- Thakur, N., Han, C.Y.: A framework for prediction of cramps during activities of daily living in elderly. In: 2020 International Conference on Big Data, Artificial Intelligence and Internet of Things Engineering (ICBAIE). pp. 284–287. IEEE (2020).
- Fontes, A.P., Neri, A.L.: Resilience in aging: literature review. Cien. Saude Colet. 20, 1475–1495 (2015). [CrossRef]
- Thakur, N., Han, C.Y.: A multimodal approach for early detection of cognitive impairment from tweets. In: Lecture Notes in Networks and Systems. pp. 11–19. Springer International Publishing, Cham (2022).
- Stern, Y., Albert, M., Barnes, C.A., Cabeza, R., Pascual-Leone, A., Rapp, P.R.: A framework for concepts of reserve and resilience in aging. Neurobiol. Aging. 124, 100–103 (2023). [CrossRef]
- Chen, Z., Yu, J., Song, Y., Chui, D.: Aging Beijing: Challenges and strategies of health care for the elderly. Ageing Res. Rev. 9, S2–S5 (2010). [CrossRef]
- Thakur, N., Han, C.Y.: Towards a knowledge base for activity recognition of diverse users. In: Advances in Intelligent Systems and Computing. pp. 303–308. Springer International Publishing, Cham (2021).
- Dunér, A., Nordström, M.: Intentions and strategies among elderly people: Coping in everyday life. J. Aging Stud. 19, 437–451 (2005). [CrossRef]
- Spoorenberg, S.L.W., Uittenbroek, R.J., Middel, B., Kremer, B.P.H., Reijneveld, S.A., Wynia, K.: Embrace, a model for integrated elderly care: study protocol of a randomized controlled trial on the effectiveness regarding patient outcomes, service use, costs, and quality of care. BMC Geriatr. 13, (2013). [CrossRef]
- Thakur, N.: A large-scale dataset of Twitter chatter about online learning during the current COVID-19 Omicron wave. Data (Basel). 7, 109 (2022). [CrossRef]
- Storey, V.C., O’Leary, D.E.: Text analysis of evolving emotions and sentiments in COVID-19 twitter communication. Cognit. Comput. 16, 1834–1857 (2024). [CrossRef]
- Bainotti, L., Caliandro, A., Gandini, A.: From archive cultures to ephemeral content, and back: Studying Instagram Stories with digital methods. New Media Soc. 23, 3656–3676 (2021). [CrossRef]
- Cardell, K., Douglas, K., Maguire, E.: ‘stories.’ In: Mediating Memory. pp. 157–172. Routledge (2017).
- Lin, H.: ‘Let’s purchase coloured live chat messages’: the impact of user engagement with Super Chat on YouTube. Inf. Commun. Soc. 1–19 (2024). [CrossRef]
- Sun, H., Chen, J., Fan, M.: Effect of live chat on traffic-to-sales conversion: Evidence from an online marketplace. Prod. Oper. Manag. 30, 1201–1219 (2021). [CrossRef]
- Perez, B., Musolesi, M., Stringhini, G.: You are your metadata: Identification and obfuscation of social media users using metadata information. Proceedings of the International AAAI Conference on Web and Social Media. 12, (2018). [CrossRef]
- Chen, L.-S., Lin, Z.-C., Chang, J.-R.: FIR: An effective scheme for extracting useful metadata from social media. J. Med. Syst. 39, (2015). [CrossRef]
- Gerber, H.R., Lynch, T.L.: Into the meta: Research methods for moving beyond social media surfacing. TechTrends. 61, 263–272 (2017). [CrossRef]
- Jones, S.M., Neblitt-Jones, V., Weigle, M.C., Klein, M., Nelson, M.L.: It’s all about the cards: Sharing on social media encouraged HTML metadata growth. In: 2021 ACM/IEEE Joint Conference on Digital Libraries (JCDL). pp. 110–119. IEEE (2021).
- Rolls, K., Hansen, M., Jackson, D., Elliott, D.: How health care professionals use social media to create virtual communities: An integrative review. J. Med. Internet Res. 18, e166 (2016). [CrossRef]
- Lu, Y., Wu, Y., Liu, J., Li, J., Zhang, P.: Understanding health care social media use from different stakeholder perspectives: A content analysis of an online health community. J. Med. Internet Res. 19, e109 (2017). [CrossRef]
- Sundaram, A., Subramaniam, H., Hamid, S.H.A., Nor, A.M.: A systematic literature review on social media slang analytics in contemporary discourse. IEEE Access. 11, 132457–132471 (2023). [CrossRef]
- Sundaram, A., Subramaniam, H., Ab Hamid, S.H., Nor, A.M.: A three-step procedural paradigm for domain-specific social media slang analytics. In: 2024 International Conference on Trends in Quantum Computing and Emerging Business Technologies. pp. 1–7. IEEE (2024).
- Matsumoto, K., Ren, F., Matsuoka, M., Yoshida, M., Kita, K.: Slang feature extraction by analysing topic change on social media. CAAI Trans. Intell. Technol. 4, 64–71 (2019). [CrossRef]
| Full Author List | Title | Classification Label |
| Yu-Bo Fu [62] | Investigating public perceptions regarding the Long COVID on Twitter using sentiment analysis and topic modeling | NLP and Modeling |
| Alex Rushforth, Emma Ladds, Sietse Wieringa, Sharon Taylor, Laiba Husain and Trisha Greenhalgh [63] | Long Covid – The illness narratives | Policy and Advocacy |
| David Russell, Naomi J. Spence, Jo-Ana D. Chase, Tatum Schwartz, Christa M. Tumminello and Erin Bouldin [64] | Support amid uncertainty: Long COVID illness experiences and the role of online communities | Community and Support |
| Francesco Meledandri [65] | The Impact of Polarised Social Media Networking Communications in the #Longcovid Debate between Ideologies and Scientific Facts | Community and Support |
| Shubh Mohan Singh and Chaitanya Reddy [66] | An Analysis of Self-reported Longcovid Symptoms on Twitter | Symptom Characterization |
| Nida Ziauddeen, Deepti Gurdasani, Margaret E O’Hara, Claire Hastie, Paul Roderick, Guiqing Yao and Nisreen A Alwan [67] | Characteristics of Long Covid: findings from a social media survey | Symptom Characterization |
| Abeed Sarker and Yao Ge [68] | Long COVID symptoms from Reddit: Characterizing post-COVID syndrome from patient reports | Symptom Characterization |
| Juan M. Banda, Nicola Adderley, Waheed-Ul-Rahman Ahmed, Heba AlGhoul, Osaid Alser, Muath Alser, Carlos Areia, Mikail Cogenur, Krisitina Fišter, Saurabh Gombar, Vojtech Huser, Jitendra Jonnagaddala, Lana YH Lai, Angela Leis, Lourdes Mateu, Miguel Angel Mayer, Evan Minty, Daniel Morales, Karthik Natarajan, Roger Paredes, Vyjeyanthi S. Periyakoil, Albert Prats-Uribe, Elsie G. Ross, Gurdas Singh, Vignesh Subbian, Arani Vivekanantham and Daniel Prieto-Alhambra [69] | Characterization of long-term patient-reported symptoms of COVID-19: an analysis of social media data | Symptom Characterization |
| Daisy Massey, Diana Berrent and Harlan Krumholz [70] | Breakthrough Symptomatic COVID-19 Infections Leading to Long Covid: Report from Long Covid Facebook Group Poll | Symptom Characterization |
| Sam Martin, Macarena Chepo, Noémie Déom, Ahmad Firas Khalid and Cecilia Vindrola-Padros [71] | “#LongCOVID affects children too”: A Twitter analysis of healthcare workers’ sentiment and discourse about Long COVID in children and young people in the UK | Symptom Characterization |
| Elham Dolatabadi, Diana Moyano, Michael Bales, Sofija Spasojevic, Rohan Bhambhoria, Junaid Bhatti, Shyamolima Debnath, Nicholas Hoell, Xin Li, Celine Leng, Sasha Nanda, Jad Saab, Esmat Sahak, Fanny Sie, Sara Uppal, Nirma Khatri Vadlamudi, Antoaneta Vladimirova, Artur Yakimovich, Xiaoxue Yang, Sedef Akinli Kocak and Angela M. Cheung [72] | Using Social Media to Help Understand Long COVID Patient Reported Health Outcomes: A Natural Language Processing Approach | Symptom Characterization |
| Lin Miao, Mark Last and Marina Litvak [73] | An Interactive Analysis of User-reported Long COVID Symptoms using Twitter Data | Symptom Characterization |
| Guocheng Feng, Huaiyu Cai and Wei Quan [74] | Exploring the Emotional and Mental Well-Being of Individuals with Long COVID Through Twitter Analysis | Symptom Characterization |
| Alexis Jordan and Albert Park [75] | Understanding the Long Haulers of COVID-19: Mixed Methods Analysis of YouTube Content | NLP and Modeling |
| Ikhwan Yuda Kusuma and Suherman Suherman [76] | The Pulse of Long COVID on Twitter: A Social Network Analysis | NLP and Modeling |
| Nirmalya Thakur [77] | Investigating and Analyzing Self-Reporting of Long COVID on Twitter: Findings from Sentiment Analysis | NLP and Modeling |
| Toluwalase Awoyemi, Ujunwa Ebili, Abiola Olusanya, Kayode E. Ogunniyi and Adedolapo V. Adejumo [78] | Twitter Sentiment Analysis of Long COVID Syndrome | Symptom Characterization |
| Sam Rhodehamel [79] | Digital Long Hauler Lifelines: Understanding How People with Long Covid Build Community on Reddit | Community and Support |
| Arinjita Bhattacharyya, Anand Seth and Shesh Rai [80] | The Effects of Long COVID-19, Its Severity, and the Need for Immediate Attention: Analysis of Clinical Trials and Twitter Data | Policy and Advocacy |
| Surani Matharaarachchi, Mike Domaratzki, Alan Katz and Saman Muthukumarana [81] | Discovering Long COVID Symptom Patterns: Association Rule Mining and Sentiment Analysis in Social Media Tweets | Symptom Characterization |
| Jonathan Koss and Sabine Bohnet-Joschko [82] | Social Media Mining of Long-COVID Self-Medication Reported by Reddit Users: Feasibility Study to Support Drug Repurposing | Symptom Characterization |
| Hanin Ayadi, Charline Bour, Aurélie Fischer, Mohammad Ghoniem and Guy Fagherazzi [83] | The Long COVID Experience from a Patient's Perspective: A Clustering Analysis of 27,216 Reddit Posts | Symptom Characterization |
| Camryn Garrett, Atefeh Aghaei, Abhishek Aggarwal and Shan Qiao [84] | The Role of Social Media in the Experiences of COVID-19 Among Long-Hauler Women: Qualitative Study | Community and Support |
| Linnea I. Laestadius, Jeanine P. D. Guidry, Andrea Bishop and Celeste Campos-Castillo [85] | State Health Department Communication about Long COVID in the United States on Facebook: Risks, Prevention, and Support | Policy and Advocacy |
| Juan S. Izquierdo-Condoy, Raul Fernandez-Naranjo, Eduardo Vasconez-González, Simone Cordovez, Andrea Tello-De-la-Torre, Clara Paz, Karen Delgado-Moreira, Sarah Carrington, Ginés Viscor and Esteban Ortiz-Prado [86] | Long COVID at Different Altitudes: A Countrywide Epidemiological Analysis | Symptom Characterization |
| Sara Santarossa, Ashley Rapp, Saily Sardinas, Janine Hussein, Alex Ramirez, Andrea E Cassidy-Bushrow, Philip Cheng and Eunice Yu [87] | Understanding the #longCOVID and #longhaulers Conversation on Twitter: Multimethod Study | Community and Support |
| Amélia Déguilhem, Joelle Malaab, Manissa Talmatkadi, Simon Renner, Pierre Foulquié, Guy Fagherazzi, Paul Loussikian, Tom Marty, Adel Mebarki, Nathalie Texier and Stephane Schuck [88] | Identifying Profiles and Symptoms of Patients With Long COVID in France: Data Mining Infodemiology Study Based on Social Media | Symptom Characterization |
| Elham Dolatabadi, Diana Moyano, Michael Bales, Sofija Spasojevic, Rohan Bhambhoria, Junaid Bhatti, Shyamolima Debnath, Nicholas Hoell, Xin Li, Celine Leng, Sasha Nanda, Jad Saab, Esmat Sahak, Fanny Sie, Sara Uppal, Nirma Khatri Vadlamudi, Antoaneta Vladimirova, Artur Yakimovich, Xiaoxue Yang, Sedef Akinli Kocak and Angela M. Cheung [89] | Using Social Media to Help Understand Patient-Reported Health Outcomes of Post–COVID-19 Condition: Natural Language Processing Approach | Symptom Characterization |
| Nida Ziauddeen, Deepti Gurdasani, Margaret E. O’Hara, Claire Hastie, Paul Roderick, Guiqing Yao and Nisreen A. Alwan [90] | Characteristics and Impact of Long Covid: Findings from an Online Survey | Symptom Characterization |
| Ludovica Segneri, Nandor Babina, Teresa Hammerschmidt, Andrea Fronzetti Colladon and Peter A. Gloor [91] | Too Much Focus on Your Health Might Be Bad for Your Health: Reddit User’s Communication Style Predicts Their Long COVID Likelihood | Symptom Characterization |
| Sai C. Reddy, Sanjana Kathiravan and Shubh M. Singh [92] | An Analysis of Self-reported Long COVID-19 Symptoms on Twitter | Symptom Characterization |
| Abeed Sarker [93] | Mining Long-COVID Symptoms from Reddit: What We Know So Far | Symptom Characterization |
| Esperanza Miyake and Sam Martin [94] | Long COVID: Online Patient Narratives, Public Health Communication, and Vaccine Hesitancy | Community and Support |
| Abeed Sarker and Yao Ge [95] | Mining Long-COVID Symptoms from Reddit: Characterizing Post-COVID Syndrome from Patient Reports | Symptom Characterization |
| Alexis Jordan and Albert Park [96] | Understanding the Plight of COVID-19 Long Haulers Through Computational Analysis of YouTube Content | NLP and Modeling |
| Brigitte Juanals and Jean-Luc Minel [97] | Using topic modeling and NLP tools for analyzing long Covid coverage by French press and Twitter | Community and Support |
| Erkan Ozduran and Sibel Büyükçoban [98] | A Content Analysis of the Reliability and Quality of YouTube Videos as a Source of Information on Health-Related Post-COVID Pain | Community and Support |
| Noémie Déom, Ahmad Firas Khalid, Sam Martin, Macarena Chepo, and Cecilia Vindrola-Padros [99] | Unlocking the Mysteries of Long COVID in Children and Young People: Insights from a Policy Review and Social Media Analysis in the UK | Policy and Advocacy |
| Erin T. Jacques, Corey H. Basch, Eunsun Park, Betty Kollia and Emma Barry [100] | Long Haul COVID-19 Videos on YouTube: Implications for Health Communication | Symptom Characterization |
| William David Strain, Ondine Sherwood, Amitava Banerjee, Vicky Van der Togt, Lyth Hishmeh and Jeremy Rossman [101] | The Impact of COVID Vaccination on Symptoms of Long COVID: An International Survey of People with Lived Experience of Long COVID | Symptom Characterization |
| Krittiya Wongtavavimarn [102] | Social Support and Narrative Sensemaking Online: A Content Analysis of Facebook Posts by COVID-19 Long Haulers | Community and Support |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





