Submitted:
11 June 2024
Posted:
12 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Obesity and Difficult Airway
3. Obesity and Laryngoscopy
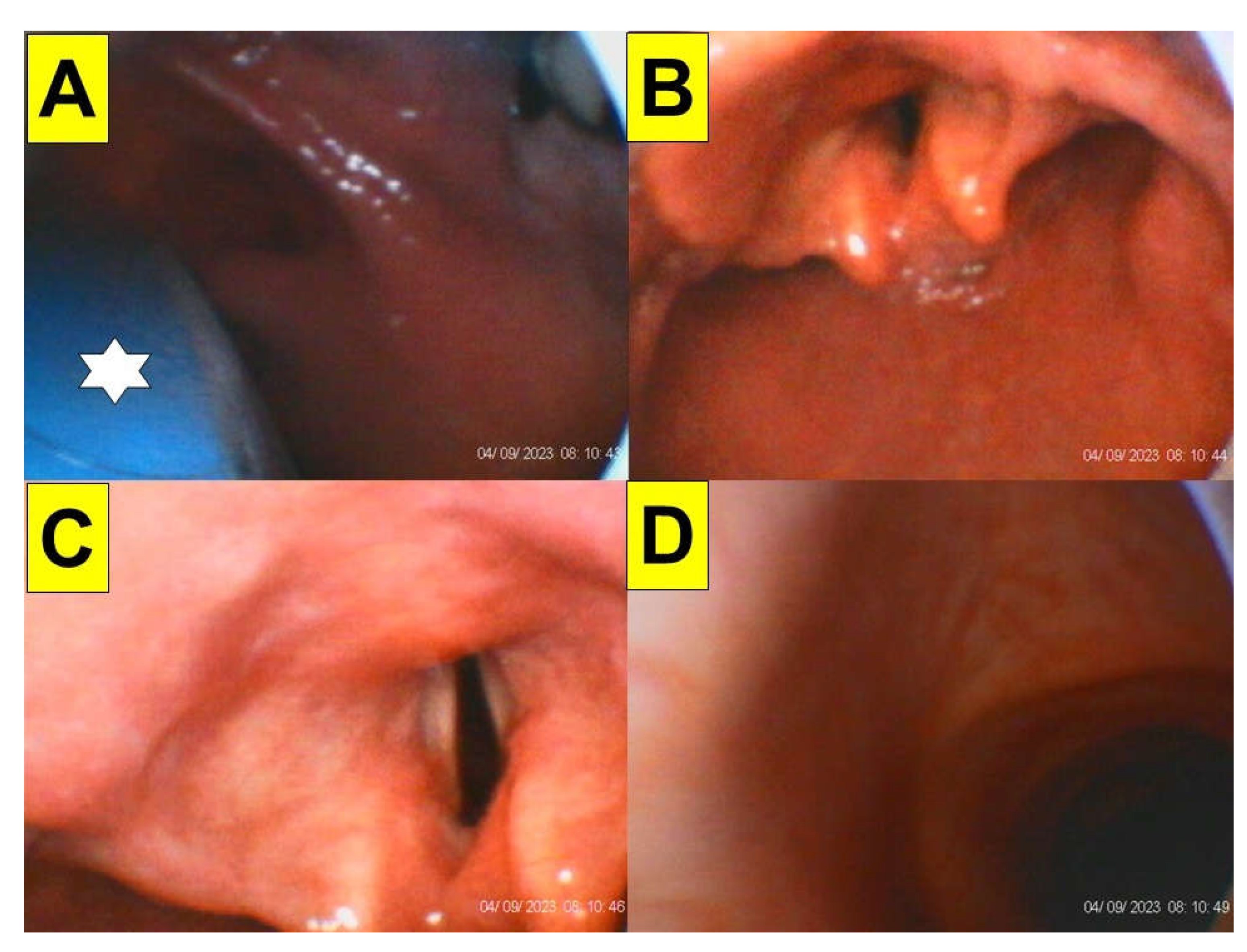
4. Obesity and Styletubation
5. Technical Pitfalls and Pearls
Limitations
6. Conclusion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arterburn, D.E.; Telem, D.A.; Kushner, R.F.; Courcoulas, A.P. Benefits and risks of bariatric surgery in adults: A review. JAMA. 2020, 324, 879–887. [Google Scholar] [CrossRef] [PubMed]
- Ogunnaike, B.O.; Jones, S.B.; Jones, D.B.; Provost, D.; Whitten, C.W. Anesthetic considerations for bariatric surgery. Anesth Analg. 2002, 95, 1793–1805. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, K.H.; Helm, M.; Lak, K.; Higgins, R.M.; Gould, J.C.; Kindel, T.L. The risk of post-operative complications in super-super obesity compared to super obesity in accredited bariatric surgery centers. Obes. Surg. 2019, 29, 2964–2971. [Google Scholar] [CrossRef]
- Mulier, J.P.; Dillemans, B. Anaesthetic factors affecting outcome after bariatric surgery, a retrospective levelled regression analysis. Obes Surg. 2019, 29, 1841–1850. [Google Scholar] [CrossRef] [PubMed]
- Marinari, G.; Foletto, M.; Nagliati, C.; Navarra, G.; Borrelli, V.; Bruni, V.; Fantola, G.; Moroni, R.; Tritapepe, L.; Monzani, R.; Sanna, D.; Carron, M.; Cataldo, R. Enhanced recovery after bariatric surgery: an Italian consensus statement. Surg Endosc. 2022, 36, 7171–7186. [Google Scholar] [CrossRef] [PubMed]
- Seyni-Boureima, R.; Zhang, Z.; Antoine, M.M.L.K.; Antoine-Frank, C.D. A review on the anesthetic management of obese patients undergoing surgery. BMC Anesthesiol. 2022, Apr 5;22(1):98. [CrossRef]
- Kaye, A.D.; Lingle, B.D.; Brothers, J.C.; Rodriguez, J.R.; Morris, A.G.; Greeson, E.M.; Cornett, E.M. The patient with obesity and super-super obesity: Perioperative anesthetic considerations. Saudi J Anaesth. 2022, 16, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Murphy, C.; Wong, D.T. Airway management and oxygenation in obese patients. Can J Anaesth. 2013, 60, 929–945. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, E. Airway management of the morbidly obese patient. J Perioperative Practice. 2016, 26, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Collins, J.S.; Lemmens, H.J.; Brodsky, J.B.; Brock-Utne, J.G.; Levitan, R.M. Laryngoscopy and morbid obesity: a comparison of the "sniff" and "ramped" positions. Obes Surg. 2004, 14, 1171–1175. [Google Scholar] [CrossRef]
- Rao, S.L.; Kunselman, A.R.; Schuler, H.G.; DesHarnais, S. Laryngoscopy and tracheal intubation in the head-elevated position in obese patients: a randomized, controlled, equivalence trial. Anesth Analg. 2008, 107, 1912–1918. [Google Scholar] [CrossRef]
- Lee, S.; Jang, E.A.; Hong, M.; Bae, H.B.; Kim, J. Ramped versus sniffing position in the videolaryngoscopy-guided tracheal intubation of morbidly obese patients: a prospective randomized study. Korean J Anesthesiol. 2023, 76, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.S. Airway management and morbid obesity. Eur J Anaesthesiol. 2010, 27, 923–927. [Google Scholar] [CrossRef] [PubMed]
- Aceto, P.; Perilli, V.; Modesti, C.; Ciocchetti, P.; Vitale, F.; Sollazzi, L. Airway management in obese patients. Surg Obes Relat Dis. 2013, 9, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Langeron, O.; Birenbaum, A.; Le Saché, F.; Raux, M. Airway management in obese patient. Minerva Anestesiol. 2014, 80, 382–392. [Google Scholar] [PubMed]
- Liew, W.J.; Negar, A.; Singh, P.A. Airway management in patients suffering from morbid obesity. Saudi J Anaesth. 2022, 16, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Thota, B.; Jan, K.M.; Oh, M.W.; Moon, T.S. Airway management in patients with obesity. Saudi J Anaesth. 2022, 16, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Waheed, Z.; Amatul-Hadi, F.; Kooner, A.; Afzal, M.; Ahmed, R.; Pande, H.; Alfaro, M.; Lee, A.; Bhatti, J. General anesthetic care of obese patients undergoing surgery: A review of current anesthetic considerations and recent advances. Cureus. 2023, Jul 8;15(7):e41565. [CrossRef]
- Neligan, P.J.; Porter, S.; Max, B.; Malhotra, G.; Greenblatt, E.P.; Ochroch, E.A. Obstructive sleep apnea is not a risk factor for difficult intubation in morbidly obese patients. Anesth Analg. 2009, 109, 1182–1186. [Google Scholar] [CrossRef] [PubMed]
- Juvin, P.; Lavaut, E.; Dupont, H.; Lefevre, P.; Demetriou, M.; Dumoulin, J.L.; Desmonts, J.M. Difficult tracheal intubation is more common in obese than in lean patients. Anesth Analg. 2003, 97, 595–600. [Google Scholar] [CrossRef]
- Kim, W.H.; Ahn, H.J.; Lee, C.J.; Shin, B.S.; Ko, J.S.; Choi, S.J.; Ryu, S.A. Neck circumference to thyromental distance ratio: a new predictor of difficult intubation in obese patients. Br J Anaesth. 2011, 106, 743–748. [Google Scholar] [CrossRef]
- De Jong, A.; Molinari, N.; Pouzeratte, Y.; Verzilli, D.; Chanques, G.; Jung, B.; Futier, E.; Perrigault, P.F.; Colson, P.; Capdevila, X.; Jaber, S. Difficult intubation in obese patients: incidence, risk factors, and complications in the operating theatre and in intensive care units. Br J Anaesth. 2015, 114, 297–306. [Google Scholar] [CrossRef]
- Wang, T.; Sun, S.; Huang, S. The association of body mass index with difficult tracheal intubation management by direct laryngoscopy: a meta-analysis. BMC Anesthesiol. 2018, Jun 30;18(1):79. [CrossRef]
- Holmberg, T.J.; Bowman, S.M.; Warner, K.J.; Vavilala, M.S.; Bulger, E.M.; Copass, M.K.; Sharar, S.R. The association between obesity and difficult prehospital tracheal intubation. Anesth Analg. 2011, 112, 1132–1138. [Google Scholar] [CrossRef] [PubMed]
- Yakushiji, H.; Goto, T.; Shirasaka, W.; Hagiwara, Y.; Watase, H.; Okamoto, H.; Hasegawa, K.; Japanese Emergency Medicine Network investigators. Associations of obesity with tracheal intubation success on first attempt and adverse events in the emergency department: An analysis of the multicenter prospective observational study in Japan. PLoS One. 2018, Apr 19;13(4):e0195938. [CrossRef]
- Saasouh, W.; Laffey, K.; Turan, A.; Avitsian, R.; Zura, A.; You, J.; Zimmerman, N.M.; Szarpak, L.; Sessler, D.I.; Ruetzler, K. Degree of obesity is not associated with more than one intubation attempt: a large centre experience. Br J Anaesth. 2018, 120, 1110–1116. [Google Scholar] [CrossRef] [PubMed]
- Moon, T.S.; Fox, P.E.; Somasundaram, A.; Minhajuddin, A.; Gonzales, M.X.; Pak, T.J.; Ogunnaike, B. The influence of morbid obesity on difficult intubation and difficult mask ventilation. J Anesth. 2019, 33, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Brodsky, J.B.; Lemmens, H.J.; Brock-Utne, J.G.; Vierra, M.; Saidman, L.J. Morbid obesity and tracheal intubation. Anesth Analg. 2002, 94, 732–736. [Google Scholar] [CrossRef] [PubMed]
- Riad, W.; Vaez, M.N.; Raveendran, R.; Tam, A.D.; Quereshy, F.A.; Chung, F.; Wong, D.T. Neck circumference as a predictor of difficult intubation and difficult mask ventilation in morbidly obese patients: A prospective observational study. Eur J Anaesthesiol. 2016, 33, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Ezri, T.; Gewürtz, G.; Sessler, D.I.; Medalion, B.; Szmuk, P.; Hagberg, C.; Susmallian, S. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia. 2003, 58, 1111–1114. [Google Scholar] [CrossRef] [PubMed]
- Prathep, S.; Jitpakdee, W.; Woraathasin, W.; Oofuvong, M. Predicting difficult laryngoscopy in morbidly obese Thai patients by ultrasound measurement of distance from skin to epiglottis: a prospective observational study. BMC Anesthesiol. 2022, May 14;22(1):145. [CrossRef]
- Marrel, J.; Blanc, C.; Frascarolo, P.; Magnusson, L. Videolaryngoscopy improves intubation condition in morbidly obese patients. Eur J Anaesthesiol. 2007, 24, 1045–1049. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, R.; Galway, U.; You, J.; Kurz, A.; Sessler, D.I.; Doyle, D.J. A randomized comparison between the Pentax AWS video laryngoscope and the Macintosh laryngoscope in morbidly obese patients. Anesth Analg. 2011, 113, 1082–1087. [Google Scholar] [CrossRef]
- Ranieri, D. Jr.; Filho, S.M.; Batista, S.; do Nascimento, P. Jr. Comparison of Macintosh and Airtraq™ laryngoscopes in obese patients placed in the ramped position. Anaesthesia. 2012, 67, 980–985. [Google Scholar] [CrossRef]
- El Sharkawy, O.; Ibrahim, S. A comparative study on tracheal intubation using Airtraq laryngoscope versus Macintosh laryngoscope in morbidly obese patients. Menoufia Med. J. 2014, 27, 169–173. [Google Scholar] [CrossRef]
- Yumul, R.; Elvir-Lazo, O.L.; White, P.F.; Sloninsky, A.; Kaplan, M.; Kariger, R.; Naruse, R.; Parker, N.; Pham, C.; Zhang, X.; Wender, R.H. Comparison of three video laryngoscopy devices to direct laryngoscopy for intubating obese patients: a randomized controlled trial. J Clin Anesth. 2016, 31, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Ander, F.; Magnuson, A.; Berggren, L.; Ahlstrand, R.; de Leon, A. Time-to-intubation in obese patients. A randomized study comparing direct laryngoscopy and videolaryngoscopy in experienced anesthetists. Minerva Anestesiol. 2017, 83, 906–913. [Google Scholar] [CrossRef] [PubMed]
- Castillo-Monzón, C.G.; Marroquín-Valz, H.A.; Fernández-Villacañas-Marín, M.; Moreno-Cascales, M.; García-Rojo, B.; Candia-Arana, C.A. Comparison of the macintosh and airtraq laryngoscopes in morbidly obese patients: a randomized and prospective study. J Clin Anesth. 2017, 36, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Nandakumar, K.P.; Bhalla, A.P.; Pandey, R.K.; Baidya, D.K.; Subramaniam, R.; Kashyap, L. Comparison of Macintosh, McCoy, and Glidescope video laryngoscope for intubation in morbidly obese patients: Randomized controlled trial. Saudi J Anaesth. 2018, 12, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Ruetzler, K.; Rivas, E.; Cohen, B.; Mosteller, L.; Martin, A.; Keebler, A.; Maheshwari, K.; Steckner, K.; Wang, M.; Praveen, C.; Khanna, S.; Makarova, N.; Sessler, D.I.; Turan, A. McGrath video laryngoscope versus Macintosh direct laryngoscopy for intubation of morbidly obese patients: A randomized trial. Anesth Analg. 2020, 131, 586–593. [Google Scholar] [CrossRef] [PubMed]
- Çakir, M.; Özyurt, E. Comparison of direct laryngoscope and McGrath videolaryngoscope in terms of glottic view and hemodynamics in bariatric surgery. Turk J Med Sci. 2020, 50, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, H.; Minville, V.; Delanoue, K.; Mazerolles, M.; Concina, D.; Fourcade, O. The importance of increased neck circumference to intubation difficulties in obese patients. Anesth Analg. 2008, 106, 1132–1136. [Google Scholar] [CrossRef] [PubMed]
- Uribe, A.A.; Zvara, D.A.; Puente, E.G.; Otey, A.J.; Zhang, J.; Bergese, S.D. BMI as a predictor for potential difficult tracheal intubation in males. Front Med (Lausanne). 2015, Jun 4;2:38. [CrossRef]
- Özdilek, A.; Beyoglu, C.A.; Erbabacan, Ş.E.; Ekici, B.; Altındaş, F.; Vehid, S.; Köksal, G.M. Correlation of neck circumference with difficult mask ventilation and difficult laryngoscopy in morbidly obese patients: an observational study. Obes Surg. 2018, 28, 2860–2867. [Google Scholar] [CrossRef] [PubMed]
- Yadav, N.K.; Rudingwa, P.; Mishra, S.K.; Pannerselvam, S. Ultrasound measurement of anterior neck soft tissue and tongue thickness to predict difficult laryngoscopy - An observational analytical study. Indian J Anaesth. 2019, 63, 629–634. [Google Scholar] [CrossRef]
- Andersen, L.H.; Rovsing, L.; Olsen, K.S. GlideScope videolaryngoscope vs. Macintosh direct laryngoscope for intubation of morbidly obese patients: a randomized trial. Acta Anaesthesiol Scand. 2011, 55, 1090–1097. [Google Scholar] [CrossRef]
- Hoshijima, H.; Denawa, Y.; Tominaga, A.; Nakamura, C.; Shiga, T.; Nagasaka, H. Videolaryngoscope versus Macintosh laryngoscope for tracheal intubation in adults with obesity: A systematic review and meta-analysis. J Clin Anesth. 2018, 44, 69–75. [Google Scholar] [CrossRef]
- Evrin, T.; Szarpak, L.; Katipoglu, B.; Mishyna, N.; Kockan, B.S.; Ruetzler, K.; Schläpfer, M. Video-assisted versus macintosh direct laryngoscopy for intubation of obese patients: a meta-analysis of randomized controlled trials. Disaster Emerg Med J. 2022, 7, 30–40. [Google Scholar] [CrossRef]
- Maassen, R.; Lee, R.; Hermans, B.; Marcus, M.; van Zundert, A. A comparison of three videolaryngoscopes: the Macintosh laryngoscope blade reduces, but does not replace, routine stylet use for intubation in morbidly obese patients. Anesth Analg. 2009, 109, 1560–1565. [Google Scholar] [CrossRef] [PubMed]
- Zoremba, M.; Aust, H.; Eberhart, L.; Braunecker, S.; Wulf, H. Comparison between intubation and the laryngeal mask airway in moderately obese adults. Acta Anaesthesiol Scand. 2009, 53, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Dhonneur, G.; Ndoko, S.K.; Yavchitz, A.; Foucrier, A.; Fessenmeyer, C.; Pollian, C.; Combes, X.; Tual, L. Tracheal intubation of morbidly obese patients: LMA CTrachTMvs direct laryngoscopy. Br J Anaesth. 2006, 97, 742–745. [Google Scholar] [CrossRef] [PubMed]
- Yousef, G.T.; Abdalgalil, D.A.; Ibrahim, T.H. Orotracheal intubation of morbidly obese patients, comparison of GlideScope® video laryngoscope and the LMA CTrach™ with direct laryngoscopy. Anesth Essays Res. 2012, 6, 174–179. [Google Scholar] [CrossRef]
- Gaszynski, T. TotalTrack video intubating laryngeal mask in super-obese patients - series of cases. Ther Clin Risk Manag. 2016, 12, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Frappier, J.; Guenoun, T.; Journois, D.; Philippe, H.; Aka, E.; Cadi, P.; Silleran-Chassany, J.; Safran, D. Airway management using the intubating laryngeal mask airway for the morbidly obese patient. Anesth Analg. 2003, 96, 1510–1515. [Google Scholar] [CrossRef] [PubMed]
- Combes, X.; Sauvat, S.; Leroux, B.; Dumerat, M.; Sherrer, E.; Motamed, C.; Brain, A.; D'Honneur, G. Intubating laryngeal mask airway in morbidly obese and lean patients: a comparative study. Anesthesiology. 2005, 102, 1106–1109. [Google Scholar] [CrossRef]
- Herman, A.G.; Mahla, M.E. Awake intubating laryngeal mask airway placement in a morbidly obese patient with ankylosing spondylitis and unstable thoracic spine. J Clin Anesth. 2016, 32, 62–64. [Google Scholar] [CrossRef]
- Gaszyński, T. The visualization of glottis during intubation's efforts in super obese patients: a comparison of total track video intubating laryngeal mask and McGrath MAC videolaryngoscope. J Clin Monit Comput. 2017, 31, 1329–1332. [Google Scholar] [CrossRef] [PubMed]
- Turna, C.K.; Arslan, Z.I.; Alparslan, V.; Okyay, K.; Solak, M. Comparison of channelled videolaryngoscope and intubating laryngeal mask airway for tracheal intubation in obese patients: a randomised clinical trial. Braz J Anesthesiol. 2020, 70, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.M. Difficult airway in an obese patient managed with the ProSeal laryngeal mask airway. Eur J Anaesthesiol. 2005, 22, 241–243. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhang, Y.; Hu, T.; Li, X.; Fu, Q. Anesthesia management of morbid obesity and ankylosing spondylitis with a difficult airway: a case report. Am J Transl Res. 2022, 14, 4860–4863. [Google Scholar] [PubMed]
- Uakritdathikarn, T.; Asampinawat, T.; Wanasuwannakul, T.; Yoosamran, B. Awake intubation with Airtraq laryngoscope in a morbidly obese patient. J Med Assoc Thai. 2008, 91, 564–567. [Google Scholar] [PubMed]
- Moore, A.R.; Schricker, T.; Court, O. Awake videolaryngoscopy-assisted tracheal intubation of the morbidly obese. Anaesthesia. 2012, 67, 232–235. [Google Scholar] [CrossRef] [PubMed]
- Ndoko, S.K.; Amathieu, R.; Tual, L.; Polliand, C.; Kamoun, W.; El Housseini, L.; Champault, G.; Dhonneur, G. Tracheal intubation of morbidly obese patients: a randomized trial comparing performance of Macintosh and Airtraq laryngoscopes. Br J Anaesth. 2008, 100, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Dhonneur, G.; Abdi, W.; Ndoko, S.K.; Amathieu, R.; Risk, N.; El Housseini, L.; Polliand, C.; Champault, G.; Combes, X.; Tual, L. Video-assisted versus conventional tracheal intubation in morbidly obese patients. Obes Surg. 2009, 19, 1096–1101. [Google Scholar] [CrossRef] [PubMed]
- Carron, M.; Ieppariello, G.; Linassi, F. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in obese adults: A meta-analysis. J Clin Anesth. 2021, 71, 110216. [Google Scholar] [CrossRef]
- King, M.R.; Jagannathan, N. Should videolaryngoscopy be the standard of care for routine tracheal intubation in obese adults? J Clin Anesth. 2018, 45, 33–34. [Google Scholar] [CrossRef]
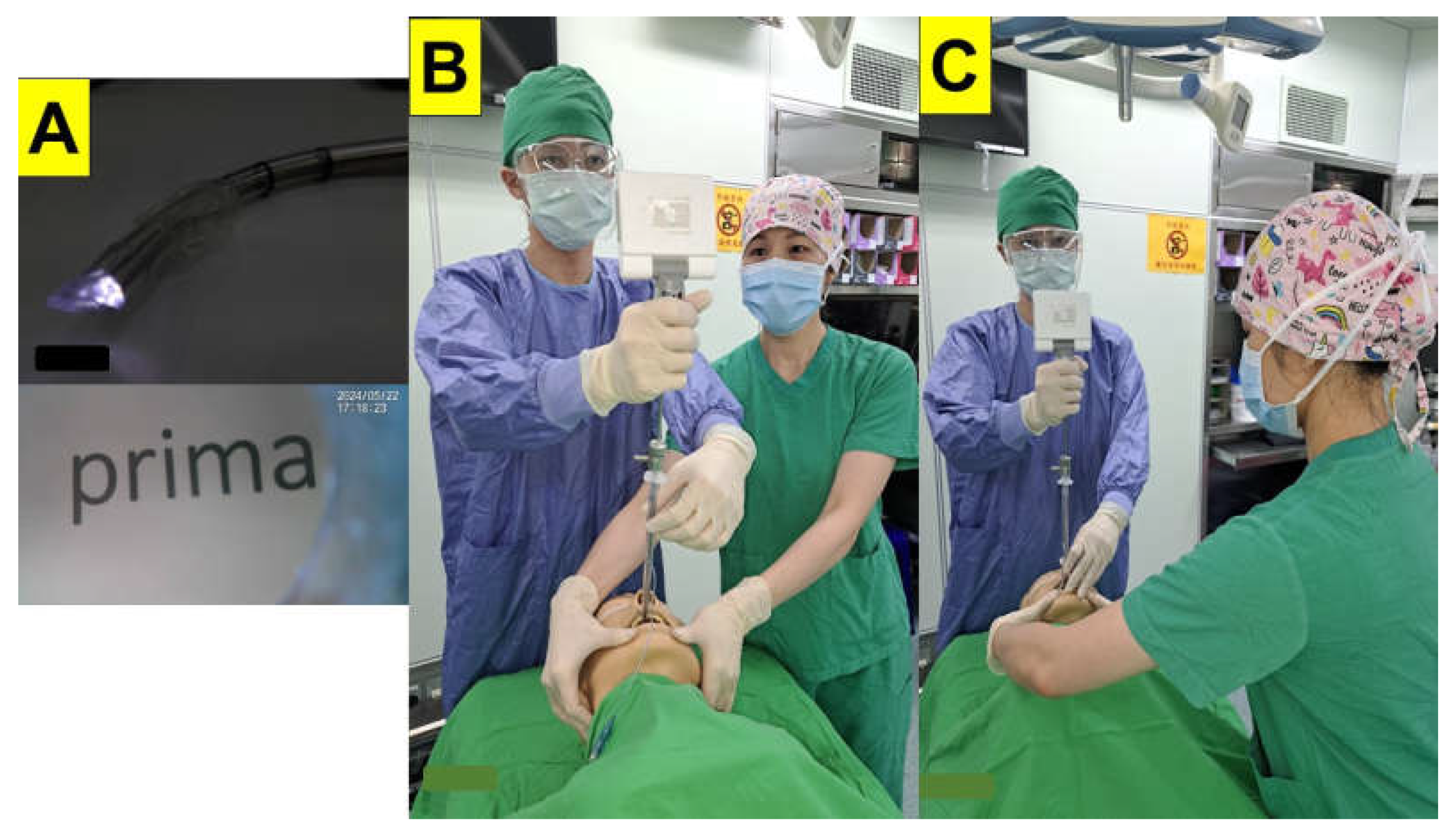
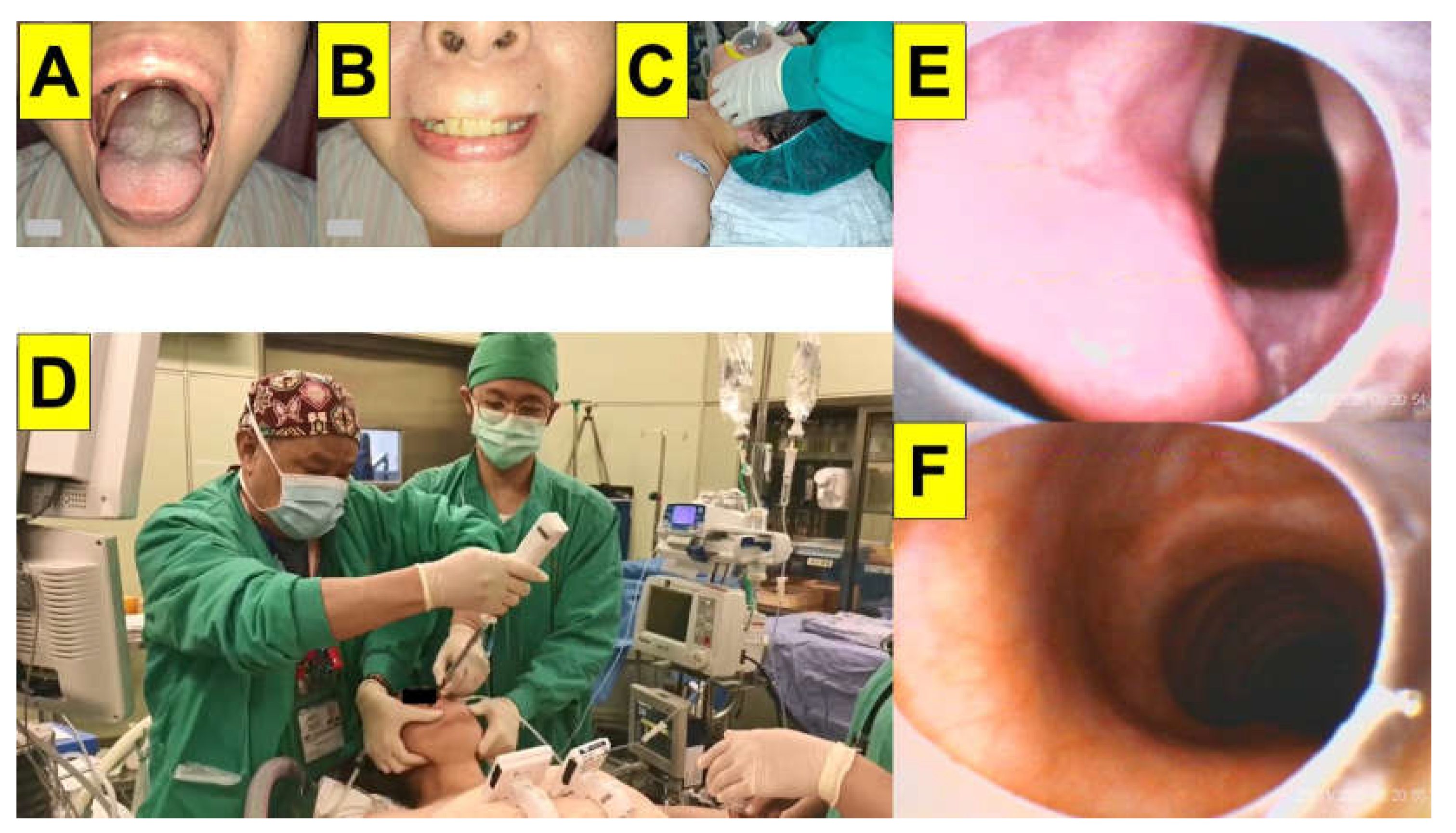
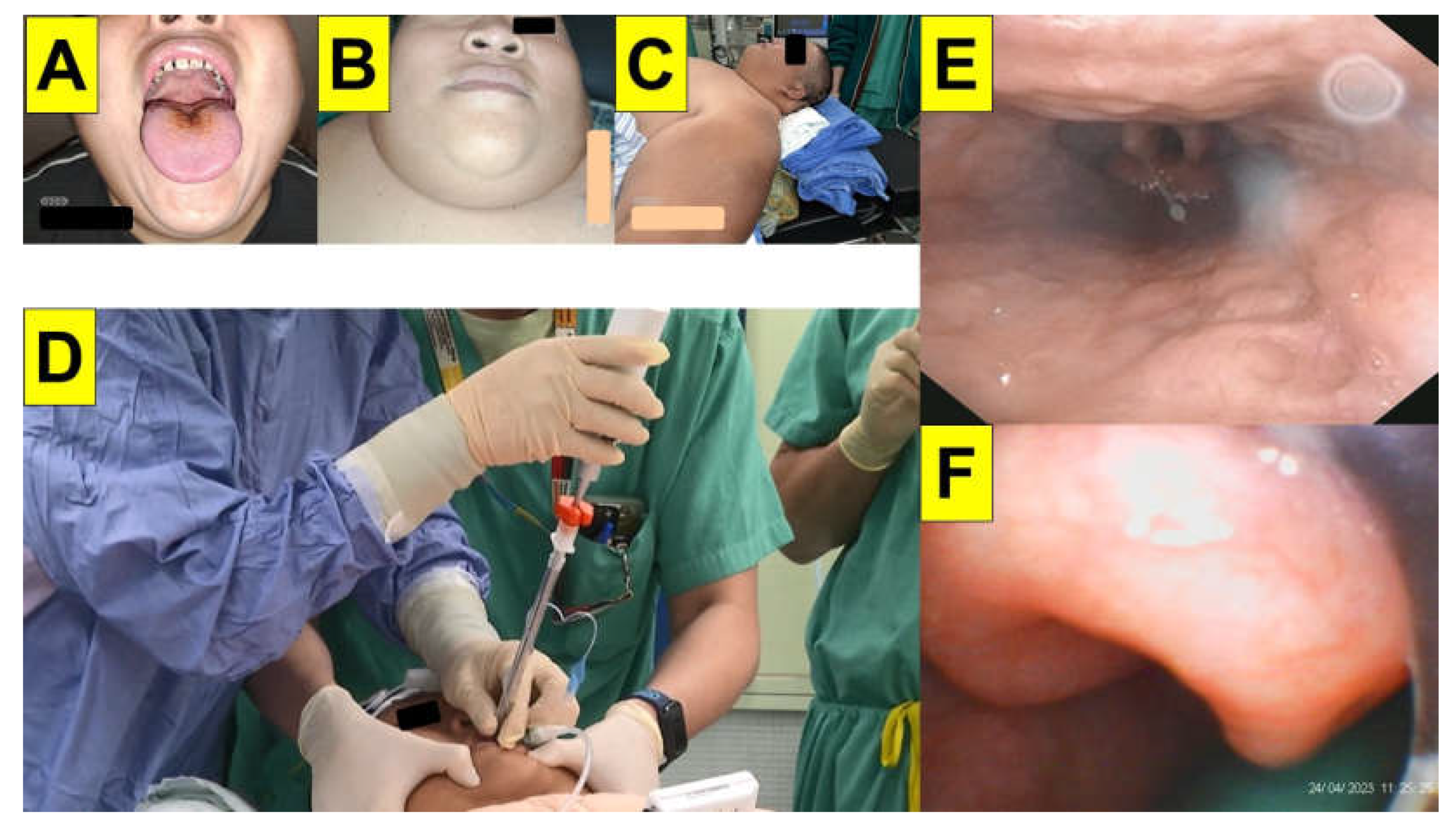
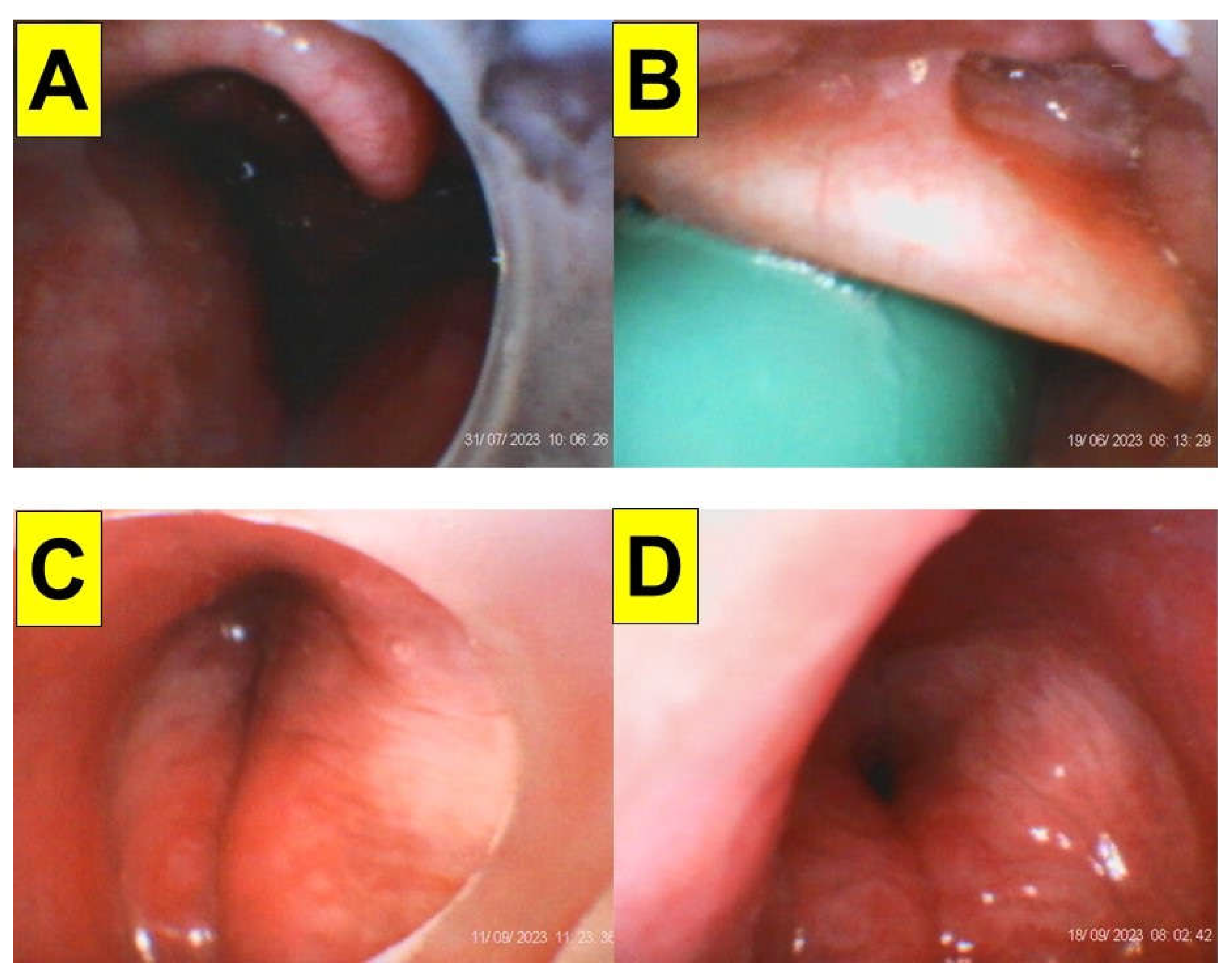
- Luk, H.N.; Qu, J.Z. Styletubation versus laryngoscopy: A new paradigm for routine tracheal intubation. Surgeries. 2024, 5, 135–161. [Google Scholar] [CrossRef]
- Tsay, P.J.; Yang, C.P.; Luk, H.N.; Qu, J.Z.; Shikani, A. Video-assisted intubating stylet technique for difficult intubation: A case series report. Healthcare (Basel). 2022, Apr 15;10(4):741. [CrossRef]
- Shih, T.L.; Koay, K.P.; Hu, C.Y.; Luk, H.N.; Qu, J.Z.; Shikani, A. The use of the Shikani video-assisted intubating stylet technique in patients with restricted neck mobility. Healthcare (Basel). 2022, Sep 4;10(9):1688. [CrossRef]
- Yang, C.P.; Luk, H.N.; Qu, J.Z.; Shikani, A. The use of a video-assisted intubating stylet technique in a critically ill and contagious COVID-19 patient. Healthcare (Basel). 2022, Feb 18;10(2):388. [CrossRef]
- Huang, C.H.; Su, I.M.; Jhuang, B.J.; Luk, H.N.; Qu, J.Z.; Shikani, A. Video-assisted stylet intubation with a plastic sheet barrier, a safe and simple technique for tracheal intubation of COVID-19 patients. Healthcare (Basel). 2022, Jun 14;10(6):1105. [CrossRef]
- Wu, B.G.; Luk, H.N.; Qu, J.Z.; Shikani, A. Styletubation in bariatric surgery: A case report. Healthcare (Basel). 2023, Aug 10;11(16):2256. [CrossRef]
- Foulds, L.T.; McGuire, B.E.; Shippey, B.J. A randomised cross-over trial comparing the McGrath(®) Series 5 videolaryngoscope with the Macintosh laryngoscope in patients with cervical spine immobilisation. Anaesthesia. 2016, 71, 437–442. [Google Scholar] [CrossRef] [PubMed]
- Suppan, L.; Tramèr, M.R.; Niquille, M.; Grosgurin, O.; Marti, C. Alternative intubation techniques vs Macintosh laryngoscopy in patients with cervical spine immobilization: systematic review and meta-analysis of randomized controlled trials. Br J Anaesth. 2016, 116, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Singleton, B.N.; Morris, F.K.; Yet, B.; Buggy, D.J.; Perkins, Z.B. Effectiveness of intubation devices in patients with cervical spine immobilisation: a systematic review and network meta-analysis. Br J Anaesth. 2021, 126, 1055–1066. [Google Scholar] [CrossRef] [PubMed]
- Paik, H.; Park, H.P. Randomized crossover trial comparing cervical spine motion during tracheal intubation with a Macintosh laryngoscope versus a C-MAC D-blade videolaryngoscope in a simulated immobilized cervical spine. BMC Anesthesiol. 2020, Aug 15;20(1):201. [CrossRef]
- Maharaj, C.H.; Costello, J.F.; Higgins, B.D.; Harte, B.H.; Laffey, J.G. Learning and performance of tracheal intubation by novice personnel: a comparison of the Airtraq and Macintosh laryngoscope. Anaesthesia. 2006, 61, 671–677. [Google Scholar] [CrossRef] [PubMed]
- Ray, D.C.; Billington, C.; Kearns, P.K.; Kirkbride, R.; Mackintosh, K.; Reeve, C.S.; Robinson, N.; Stewart, C.J.; Trudeau, T. A comparison of McGrath and Macintosh laryngoscopes in novice users: a manikin study. Anaesthesia. 2009, 64, 1207–1210. [Google Scholar] [CrossRef] [PubMed]
- Ambrosio, A.; Pfannenstiel, T.; Bach, K.; Cornelissen, C.; Gaconnet, C.; Brigger, M.T. Difficult airway management for novice physicians: a randomized trial comparing direct and video-assisted laryngoscopy. Otolaryngol Head Neck Surg. 2014, 150, 775–778. [Google Scholar] [CrossRef]
- Choi, J.W.; Kim, J.A.; Jung, H.J.; Kim, W.H. Tracheal Intubation with a McGrath® Series 5 Video Laryngoscope by Novice Personnel in a Cervical-immobilized Manikin. J Emerg Med. 2016, 50, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Eismann, H.; Sieg, L.; Etti, N.; Friedrich, L.; Schröter, C.; Mommsen, P.; Krettek, C.; Zeckey, C. Improved success rates using videolaryngoscopy in unexperienced users: a randomized crossover study in airway manikins. Eur J Med Res. 2017, Aug 10;22(1):27. [CrossRef]
- Yong, S.A.; Chaou, C.H.; Yu, S.R.; Kuan, J.T.; Lin, C.C.; Liu, H.P.; Chiu, T.F. Video assisted laryngoscope facilitates intubation skill learning in the emergency department. J Acute Med. 2020, 10, 60–69. [Google Scholar] [CrossRef]
- Nalubola, S.; Jin, E.; Drugge, E.D.; Weber, G.; Abramowicz, A.E. Video versus direct laryngoscopy in novice intubators: A systematic review and meta-analysis. Cureus. 2022, Sep 25;14(9):e29578. [CrossRef]
- Webb, A.; Kolawole, H.; Leong, S.; Loughnan, T.E.; Crofts, T.; Bowden, C. Comparison of the Bonfils and Levitan optical stylets for tracheal intubation: a clinical study. Anaesth Intensive Care. 2011, 39, 1093–1097. [Google Scholar] [CrossRef]
- Kleine-Brueggeney, M.; Greif, R.; Urwyler, N.; Wirthmüller, B.; Theiler, L. The performance of rigid scopes for tracheal intubation: a randomised, controlled trial in patients with a simulated difficult airway. Anaesthesia. 2016, 71, 1456–1463. [Google Scholar] [CrossRef]
- Theiler, L.; Greif, R.; Bütikofer, L.; Arheart, K.; Kleine-Brueggeney, M. The skill of tracheal intubation with rigid scopes-a randomised controlled trial comparing learning curves in 740 intubations. BMC Anesthesiol. 2020, Oct 16;20(1):263. [CrossRef]
- Tseng, K.Y.; Chau, S.W.; Su, M.P.; Shih, C.K.; Lu, I.C.; Cheng, K.I. A comparison of Trachway intubating stylet and Airway Scope for tracheal intubation by novice operators: a manikin study. Kaohsiung J Med Sci. 2012, 28, 448–451. [Google Scholar] [CrossRef]
- Hung, K.C.; Tan, P.H.; Lin, V.C.; Wang, H.K.; Chen, H.S. A comparison of the Trachway intubating stylet and the Macintosh laryngoscope in tracheal intubation: a manikin study. J Anesth. 2013, 27, 205–210. [Google Scholar] [CrossRef]
- Ong, J.; Lee, C.L.; Huang, S.J.; Shyr, M.H. Comparison between the Trachway video intubating stylet and Macintosh laryngoscope in four simulated difficult tracheal intubations: A manikin study. Ci Ji Yi Xue Za Zhi. 2016, 28, 109–112. [Google Scholar] [CrossRef]
- Park, J.W.; An, S.; Park, S.; Nahm, F.S.; Han, S.H.; Kim, J.H. Comparison of a new video intubation stylet and McGrath® MAC video laryngoscope for intubation in an airway manikin with normal airway and cervical spine immobilization scenarios by novice personnel: A randomized crossover study. Biomed Res Int. 2021, Nov 10;2021:4288367. [CrossRef]
- Chen, Y.Y.; Lin, J.C.; Tsai, M.J.; Cheng, K.Y. Retromolar intubation with video intubating stylet in difficult airway: A randomized crossover manikin study. Am J Emerg Med. 2022, 54, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Kelly, F.E.; Cook, T.M. Seeing is believing: getting the best out of videolaryngoscopy. Br J Anaesth. 2016, 117, Suppl 1:i9–i13. [Google Scholar] [CrossRef]
- Bathory, I.; Granges, J.C.; Frascarolo, P.; Magnusson, L. Evaluation of the Video Intubation Unit in morbid obese patients. Acta Anaesthesiol Scand. 2010, 54, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Prekker, M.E.; Driver, B.E.; Trent, S.A.; Resnick-Ault, D.; Seitz, K.P.; Russell, D.W.; Gaillard, J.P.; Latimer, A.J.; Ghamande, S.A.; Gibbs, K.W.; Vonderhaar, D.J.; Whitson, M.R.; Barnes, C.R.; Walco, J.P.; Douglas, I.S.; Krishnamoorthy, V.; Dagan, A.; Bastman, J.J.; Lloyd, B.D.; Gandotra, S.; Goranson, J.K.; Mitchell, S.H.; White, H.D.; Palakshappa, J.A.; Espinera, A.; Page, D.B.; Joffe, A.; Hansen, S.J.; Hughes, C.G.; George, T.; Herbert, J.T.; Shapiro, N.I.; Schauer, S.G.; Long, B.J.; Imhoff, B.; Wang, L.; Rhoads, J.P.; Womack, K.N.; Janz, D.R.; Self, W.H.; Rice, T.W.; Ginde, A.A.; Casey, J.D.; Semler, M.W. DEVICE investigators and the pragmatic critical care research group. Video versus direct laryngoscopy for tracheal intubation of critically ill adults. N Engl J Med. 2023, 389, 418–429. [Google Scholar] [CrossRef]
- Maassen, R.; Lee, R.; van Zundert, A.; Cooper, R. The videolaryngoscope is less traumatic than the classic laryngoscope for a difficult airway in an obese patient. J Anesth. 2009, 23, 445–448. [Google Scholar] [CrossRef]
- Luk, H.N.; Qu, J.Z.; Shikani, A. Styletubation: The paradigmatic role of video-assisted intubating stylet technique for routine tracheal intubation. Asian J Anesthesiol. 2023, 61, 102–106. [Google Scholar] [CrossRef]
- Treki, A.A.; Straker, T. Limitations of the videolaryngoscope: An anesthetic management reality. Int Anesthesiol Clin. 2017, 55, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Thong, S.Y.; Wong, T.G. Clinical uses of the Bonfils retromolar intubation fiberscope: a review. Anesth Analg. 2012, 115, 855–866. [Google Scholar] [CrossRef] [PubMed]
- Lan, C.H.; Luk, H.N.; Qu, J.Z.; Shikani, A. An approach to improve the effectiveness of the video-assisted intubating stylet technique for tracheal intubation: A case series report. Healthcare (Basel). 2023, Mar 20;11(6):891. [CrossRef]
- Wilson, S.L.; Mantena, N.R.; Halverson, J.D. Effects of atropine, glycopyrrolate, and cimetidine on gastric secretions in morbidly obese patients. Anesth Analg. 1981, 60, 37–40. [Google Scholar] [CrossRef] [PubMed]
- Halliday, T.A.; Sundqvist, J.; Hultin, M.; Walldén, J. Post-operative nausea and vomiting in bariatric surgery patients: an observational study. Acta Anaesthesiol Scand. 2017, 61, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Van Zundert, A.A.; Pieters, B.M. Combined technique using videolaryngoscopy and Bonfils for a difficult airway intubation. Br J Anaesth. 2012, 108, 327–328. [Google Scholar] [CrossRef] [PubMed]
- Gaszynski, T.; Pietrzyk, M.; Szewczyk, T.; Gaszynska, E. A comparison of performance of endotracheal intubation using the Levitan FPS optical stylet or Lary-Flex videolaryngoscope in morbidly obese patients. Scientific World J. 2014, 2014:207591. [CrossRef]
- Chiu, W.C.; Wu, Z.F.; Lai, M.F.; Lai, H.C. Combination use of laryngoscope, jaw thrust, and trachway for improving difficult tracheal intubation in obese. J Med Sci. 2022, 42, 197–198. [Google Scholar] [CrossRef]
- Jhuang, B.J.; Luk, H.N.; Qu, J.Z.; Shikani, A. Video-twin technique for airway management, combining video-intubating stylet with videolaryngoscope: A case series report and review of the literature. Healthcare (Basel). 2022, Oct 30;10(11):2175. [CrossRef]
- Yang, M.; Kim, J.A.; Ahn, H.J.; Choi, J.W.; Kim, D.K.; Cho, E.A. Double-lumen tube tracheal intubation using a rigid Video Stylet: a randomized controlled comparison with the Macintosh laryngoscope. Br J Anaesth. 2013, 111, 990–995. [Google Scholar] [CrossRef]
- Zhang, T.; Zhao, K.Y.; Zhang, P.; Li, R.H. Comparison of video laryngoscope, video stylet, and flexible videoscope for transoral endotracheal intubation in patients with difficult airways: a randomized, parallel-group study. Trials. 2023, Sep 21;24(1):599. [CrossRef] [PubMed] [PubMed Central]
- Gu, Y.; Zhou, Q.; Zhou, H.; Liu, M.; Feng, D.; Wei, J.; Min, K.; Zhu, W.; Chen, Y.; Lv, X. A randomized study of rigid video stylet versus Macintosh laryngoscope for double-lumen endobronchial tube intubation assistance in thoracoscopic pulmonary surgery. J Clin Med. 2023, Jan 9;12(2):540. [CrossRef]
| Predictive Factors | References |
|---|---|
| Gender | [19,27,29,32,33,34,35,36,37,38,39,40,41] |
| Age | [27,32,33,34,35,36,37,38,39,40,41] |
| BMI | [29,31,32,33,34,35,36,37,38,39,40,41,42,43] |
| Mallampati score | [19,21,27,29,32,33,34,35,36,37,38,40,41,42,43,44,45] |
| Mouth opening (inter-incisor distance) | [32,34,35,36,38,40] |
| Poor dentition | [27,36,40] |
| Tongue thickness | [45] |
| Neck circumference | [29,30,32,34,35,36,37,38,40,42,44,45] |
| Thyro-mental distance | [27,31,32,35,36,38,40,42] |
| Sternomental distance | [31,34,40,44] |
| Neck circumference/thyro-mental distance ratio | [21] |
| Range of motion of neck | [40,44] |
| Upper lip bite test | [40,44] |
| Sleep apnea syndrome | [29,32,40] |
| Anterior neck soft tissue thickness (distance from skin to epiglottis) | [30,31,45] |
| Parameters | DL | VL | Styletubation (Table 4, n = 20) |
|---|---|---|---|
| BMI (kg/m2) | 44 [32] 43 [63] 40 [64] 41 [46] 43 [33] 43 [34] 44 [52] 41 [35] 42 [36] 47 [40] 46 [41] 47 [38] 45 [39] |
43 [32] 44 [63] 43 [64] 42 [46] 41 [33] 44 [34] 43 [52] 40 [35] 41 [36] 46 [40] 46 [41] 46 [38] 47 [39] |
38 (mean; 103 ― 34.8); 48 (median) |
| Intubation time | 93 s [32] 56 s [63] 69 s [64] 32 s [46] 26 s [33] 37 s [34] 100 s [52] 18 s [35] 43 s [36] 26 s [37] 27 s [40] 46 s [41] 22 s [38] 32 s [39] |
59 s [32] 24 s [63] 29 s [64] 48 s [46] 38 s [33] 14 s [34] 86 s [52] 12 s [35] 40 s [36] 25 s [37] 28 s [40] 57 s [41] 17 s [38] 54 s [39] |
12 s (mean; 5 s ― 22 s); 11 s (median) |
| First-attempt success rate | 80% [32] 93 [63] 92% [46] 92% [33] 84% [34] 70% [52] 90% [35] 74% [36] 87% [37] 89% [40] 91% [38] |
95% [32] 100% [63] 98% [46] 86% [33] 100% [34] 90% [52] 100% [35] 70% [36] 100% [37] 92% [40] 91% [38] |
100% |
| Failed intubation | 0% [32] 0.9% [64] 4% [46] 0% [33] 1.6% [34] 20% [52] 20% [35] 0% [36] 13% [37] 8% [40] 0% [38] |
0% [32] 0% [64] 0% [46] 10% [33] 0% [34] 0% [52] 5% [35] 0% [36] 0% [37] 3% [40] 0% [38] |
0% |
| Cormack–Lehane grade 3/4 | 15%/0% [32] 19%/2% [63] 15%/0% [64] 20%/8% [46] 22% [33] 6%/5% [34] 20%/3% [52] 40%(3) [35] 16%/19% [36] 10%/6% [40] 58% [41] |
0%/0% [32] 0%/0% [63] 0%/0% [64] 4%/0% [46] 14% [33] 0%/0% [34] 0%/0% [52] 5%(3) [35] 0%/0% [36] 5%/0% [40] 58% [41] |
NA |
| POGO | 75% [64] 57% [36] 29%/35% [POGO75%/100%] [40] |
97% [64] 91% [36] 17%/67% [POGO75%/100%] [40] |
100% |
| Increased lifting force required (%) | 40% [46] 33% [52] |
22% [46] 0% [52] |
NA |
| Subjective difficulty of intubation | More difficult [63] Similar to VL [46] 40 (0-100 scale) [33] 15% [35] 11% [40] 13% [38] 0% [39] |
Easy [63] Similar to DL [46] 52 (0-100 scale) [33] 40% [35] 6% [40] 4% [38] 7% [39] Easier than DL [52] |
Easy |
| 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | |
|---|---|---|---|---|---|---|---|---|
| Total anesthesia number | 16077 | 17831 | 17998 | 19307 | 19721 | 19244 | 19765 | 22438 |
| GA number | 15339 | 16893 | 17497 | 18481 | 19009 | 18574 | 19061 | 22099 |
| LMA-GA number | 5544 | 5134 | 5816 | 5902 | 5863 | 5714 | 4932 | 5763 |
| ET-GA number | 5953 | 6504 | 6920 | 6966 | 7418 | 6982 | 7602 | 8329 |
| VL | 0 | 0 | 20 | 100 | 635 | 336 | 305 | 280 |
| Styletubation | 5953 | 6504 | 6900 | 6866 | 6783 | 6646 | 7297 | 8049 |
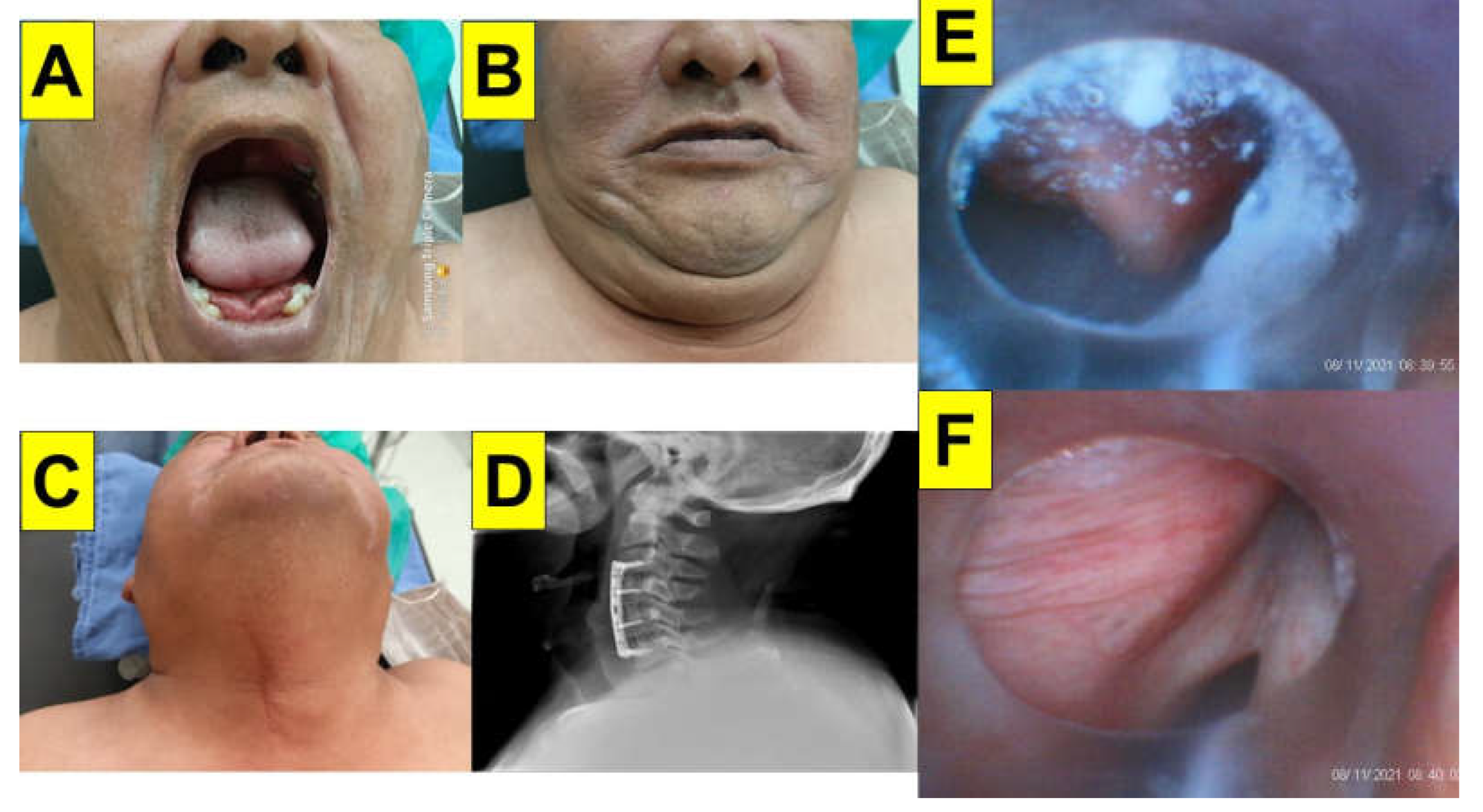
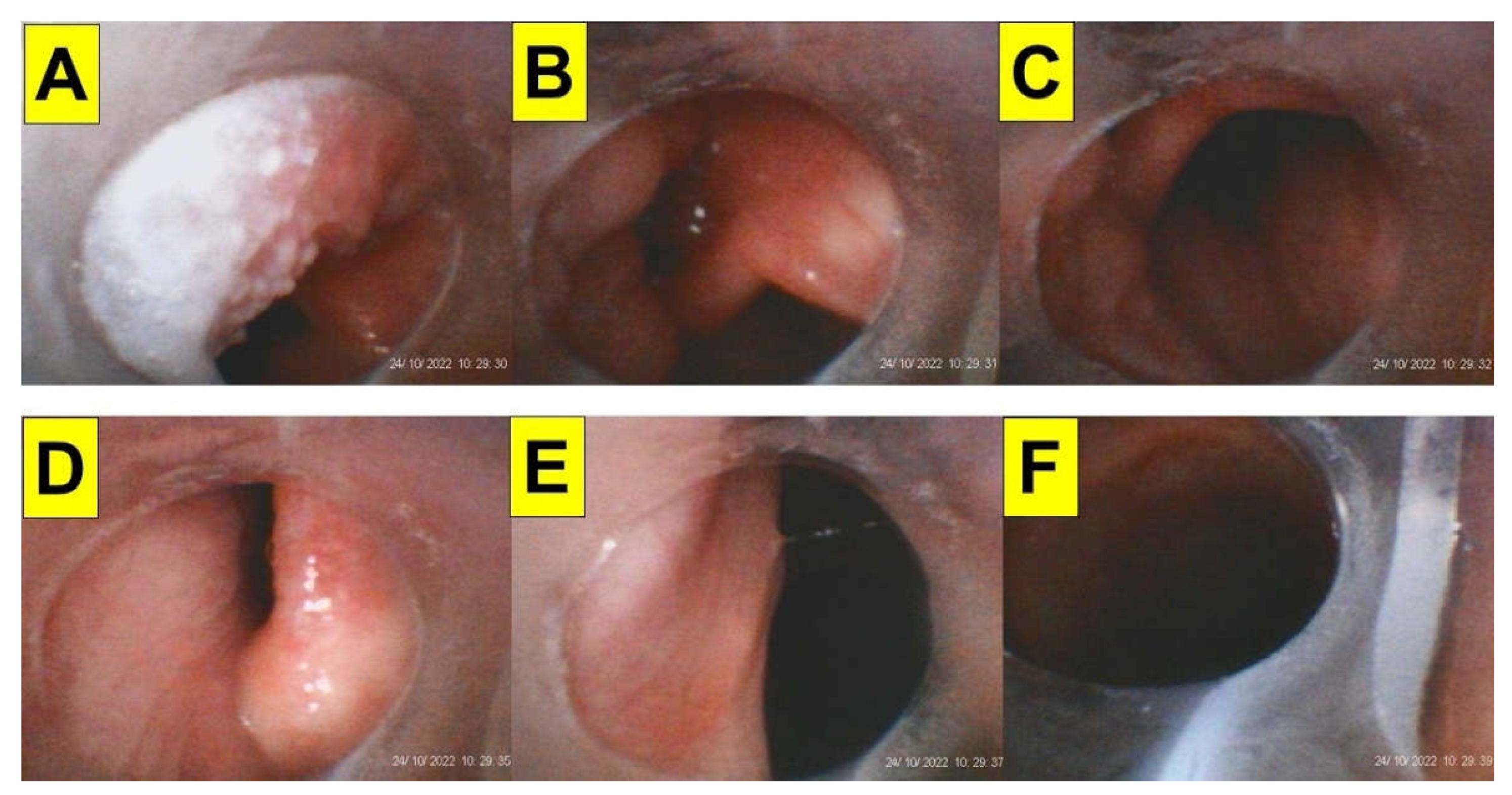
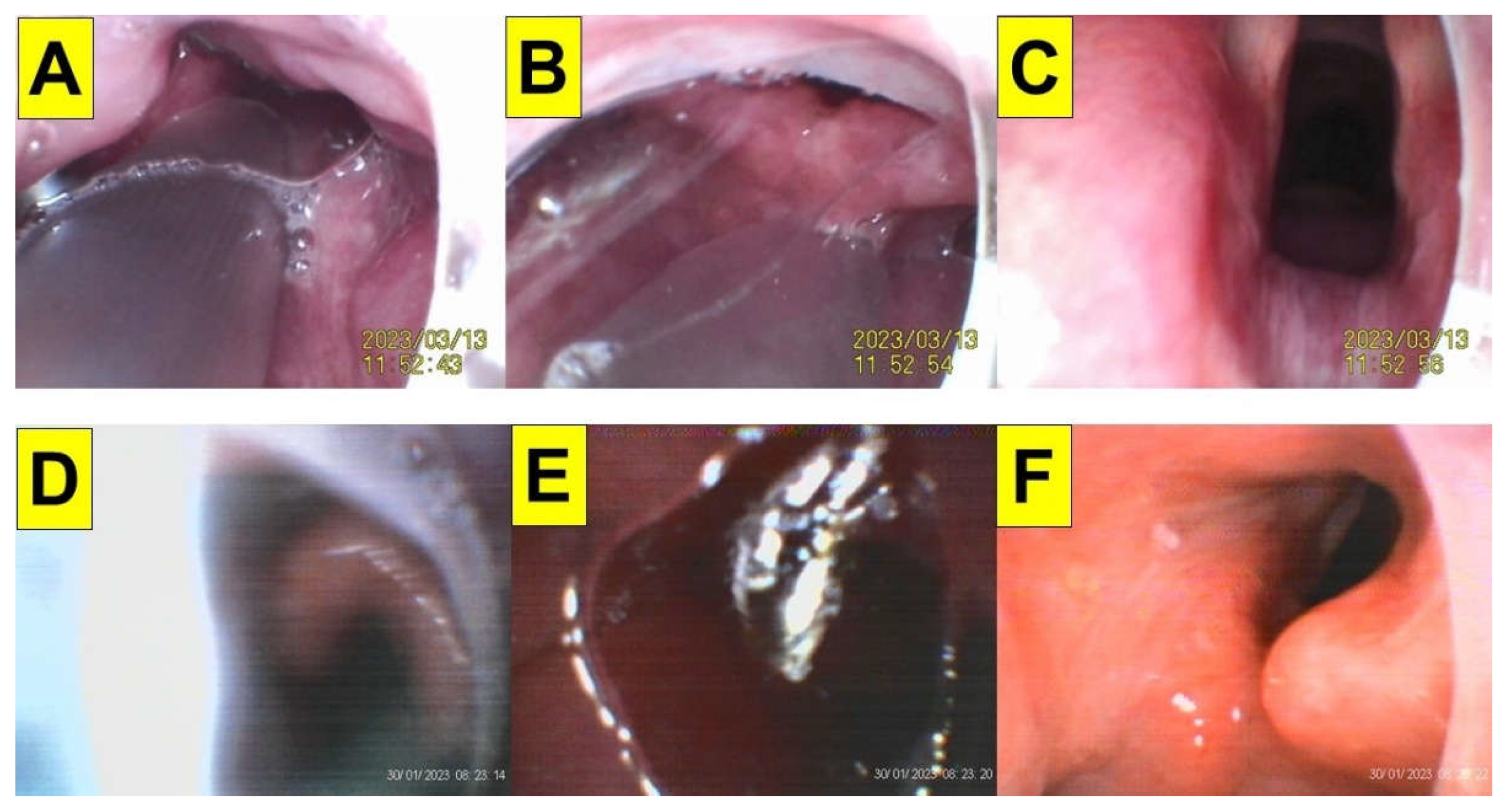
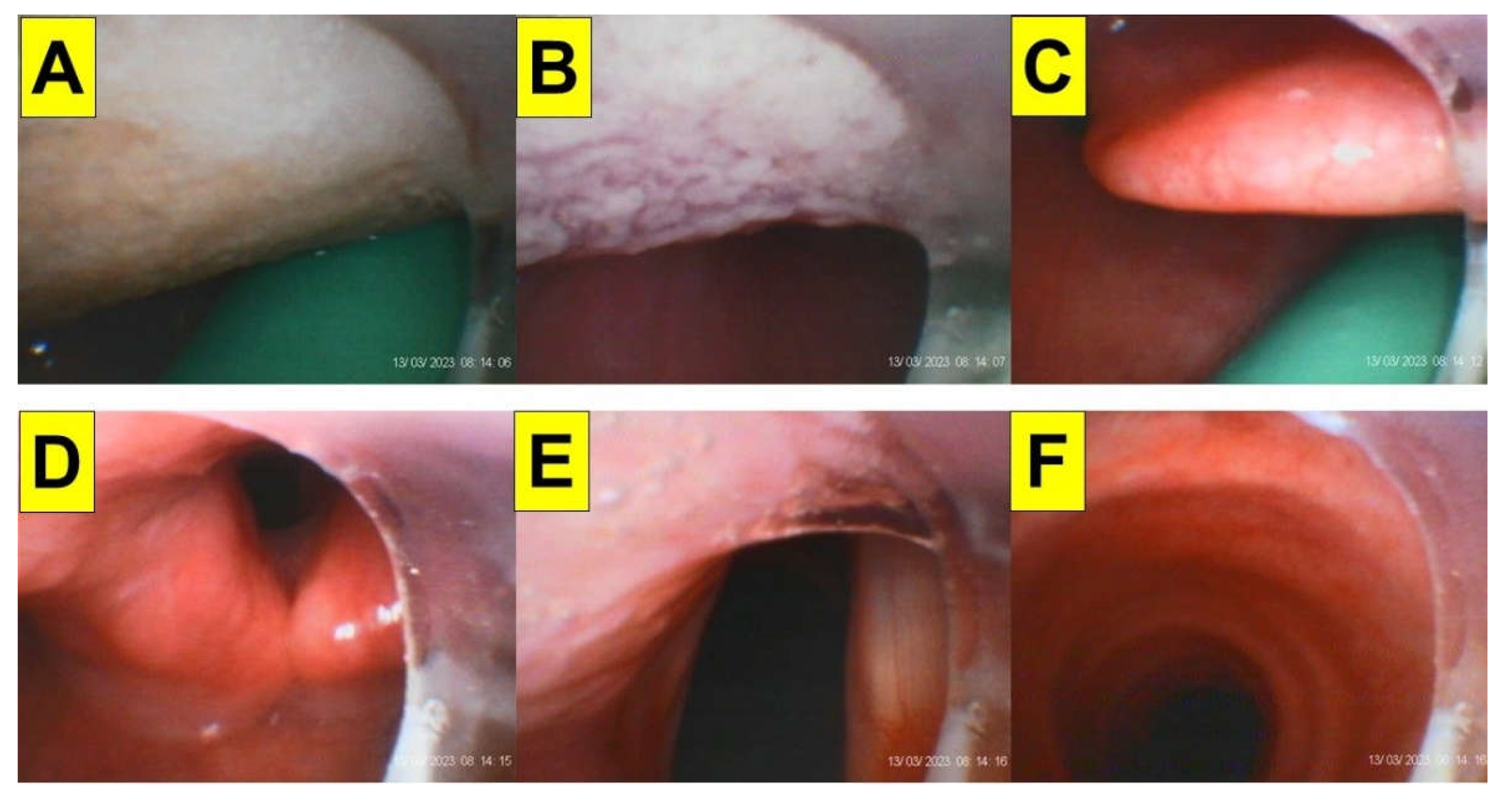
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | Case 10 | Case 11 | Case 12 | Case 13 | Case 14 | Case 15 | Case 16 | Case 17 | Case 18 | Case 19 | Case 20 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age/Gender (years old) | 33/M | 42/M | 42/F | 49/M | 57/F | 51/F | 26/F | 45/M | 32/F | 37/F | 23/M | 56/M | 41/F | 26/M | 48/M | 56/M | 38/M | 42/M | 40/M | 58/F |
| Height (cm) | 158 | 165 | 161 | 180 | 153 | 160 | 160 | 171 | 157 | 162 | 176 | 159 | 158 | 166 | 175 | 170 | 178 | 166 | 174 | 166 |
| Weight (kg) | 258 | 172 | 165 | 175 | 120 | 131 | 130 | 147 | 119 | 126 | 146 | 115 | 111 | 121 | 124 | 112 | 120 | 101 | 109 | 96 |
| BMI (kg/m2) | 103 | 63.1 | 63.6 | 54 | 51.2 | 51.1 | 50.7 | 50.2 | 48.2 | 48 | 47.1 | 45.4 | 44.4 | 43.9 | 40.4 | 38.7 | 37.8 | 36.6 | 36 | 34.8 |
| Surgery | LSG | OAGB | OAGB | LSG | LSG | OAGB | LSG | LSG | OAGB | OAGB | LSG | LSG | LSG | LSG | LSG | OAGB | LSG | LSG | LSG | LSG |
| Comorbidity | HTN/DM/OSAS | HTN/DM/OSAS | HTN/OSAS | HTN/OSAS | HTN/CAD/cirrhosis of liver | HTN/OSAS | Obesity/OSAS | CAD/CVA/OSAS | OSAS | HTN/DM | OSAS | HTN/DM/CVA | DM/asthma | OSAS | OSAS | HTN/DM/CAD | OSAS | OSAS/COPD | HTN/DM/OSAS | HTN/DM |
| ASA class | III | III | II | II | III | II | II | III | II | III | II | III | II | II | II | III | II | II | III | III |
| MMT | 4 | 4 | 3 | 3 | 3 | 3 | 2 | 2 | 2 | 2 | 2 | 3 | 2 | 2 | 2 | 2 | 3 | 3 | ||
| Interincisor distance | 4.5 | 5.5 | 5 | 5.5 | 5 | 4.5 | 6 | 5 | 4 | 4 | 4.5 | 4.5 | 4 | 5 | 5.5 | 4.5 | 5 | 4.5 | 4 | 4.5 |
| ULBT | 2 | 2 | 1 | 2 | 2 | 1 | 1 | 1 | 2 | 1 | 1 | 2 | 1 | 1 | 2 | 1 | 1 | 1 | 2 | 1 |
| Thyromental distance (cm) | 8 | 6 | 7 | 9 | 8 | 7 | 9 | 9 | 9 | 9 | 8 | 6 | 7 | 7 | 9 | 9 | 7 | 7 | 6 | 8 |
| Sternomental distance (cm) | 17 | 15 | 16 | 15 | 14 | 16 | 20 | 18 | 16 | 17 | 16 | 15 | 16 | 18 | 13 | 16 | 17 | 16 | 16 | 18 |
| Neck circumference (cm) | 54 | 54 | 42 | 50 | 37 | 47 | 39 | 48 | 45 | 39 | 50 | 49 | 45 | 47 | 44 | 46 | 44 | 41 | 44 | 38 |
| Neck fat deposition/soft tissue loading on the upper airway | moderate | moderate | mild | moderate | moderate | moderate | Mild | mild | mild | Mild | mild | moderate | mild | mild | mild | mild | mild | mild | mild | mild |
| Waist circumference (cm) | 200 | 166 | 155 | 150 | 142 | 155 | 132 | 143 | 142 | 133 | 143 | 133 | 114 | 124 | 140 | 115 | 124 | 112 | 119 | 110 |
| Hip circumference (cm) | 202 | 154 | 158 | 148 | 144 | 150 | 146 | 126 | 156 | 134 | 148 | 126 | 140 | 128 | 124 | 115 | 118 | 120 | 120 | 126 |
| LQS grading | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 1 |
| POGO (%) | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Time to intubation | 12 s | 14 s | 18 s | 22 s | 6 s | 10 s | 8 s | 11 s | 5 s | 5 s | 11 s | 13 s | 9 s | 6 s | 18 s | 8 s | 12 s | 22s | 20 s | 5 s |
| Expected cause of prolonged time of tracheal intubation | Performed by a third- year resident | Prior cervical spine surgery, copious secretions | For demonstration purpose | For demonstration purpose | ||||||||||||||||
| First-pass success | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes |
| Subjective easiness | easy | easy | easy | easy | easy | easy | easy | easy | easy | easy | easy | easy | easy | easy | easy | easy | easy | easy | easy | easy |
| Airway-related complications | none | none | none | none | none | none | none | none | none | none | none | none | none | none | none | none | none | none | none | none |
| Supplemental video-clips | Video S1 | Video S2 | Video S3 | Video S4 | Video S5 | Video S6 | Video S7 | Video S8 | Video S9 | Video S10 | Video S11 | Video S12 | NA | Video S13 | Video S14 | Video S15 | Video S16 | Video S17 | Video S18 | Video S19 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





