Introduction
Decreased birth rates have been reported in the Czech Republic and many other countries following the COVID-19 pandemic.1-3 Although studies have indicated that COVID-19 vaccination has no appreciable effect on human fertility and that COVID-19 vaccines are safe during pregnancy,4,5 adverse effects of COVID-19 vaccines on menstrual characteristics are well-documented, suggesting that COVID-19 vaccination may influence fecundability, i.e., the probability of achieving successful conception (SC) within a single menstrual cycle.6,7 Unfortunately, the potential influence on reproductive health was not assessed in randomized preauthorization trials of COVID-19 vaccines and investigations aimed at the influence of individual COVID-19 vaccines on human fecundability are encumbered by methodological challenges including, for example, temporal variation in vaccine-related factors (vaccine characteristics, accessibility, eligibility, hesitancy, policies etc.), healthy vaccine and selection bias of available preconception cohorts (pregnancy planners, women undergoing invitro fertilization etc.), and inherent limitations of electronic health care data that are not designed to measure SCs (left-truncation bias, inability to capture early pregnancy loss without registered medical contact etc.).8 However, data that may add to evidence on the potential influence of COVID-19 vaccination on human fecundability are obviously of great importance to public health. The Czech Republic is one of the few countries where nationwide birth data are available for women who were vaccinated or unvaccinated for COVID-19, and we therefore used these data to compare rates of SCs resulting in live births for these two groups.
Material and Methods
Data for the number of live births by women in the Czech Republic aged 18-39 years (hereafter referred to as ‘women’) were retrieved from the Institute of Health Information and Statistics of the Czech Republic (IHIS). The data contained the number of births per month between January 2021 and December 2023 by women who were vaccinated, i.e., had received at least one COVID-19 vaccine dose by the date of delivery, and by women who were unvaccinated, respectively. Furthermore, the number of births per months by women vaccinated during pregnancy was provided. A SC was defined as one that resulted in a live birth 9 months later. Accordingly, the obtained data enabled us to calculate the number of births per month by women who were vaccinated prior to SC, i.e., the number of women vaccinated by the date of delivery 9 months later, minus the number of women who were vaccinated during pregnancy, as well as the number of women who were unvaccinated before SC, respectively. The total number of women vaccinated against COVID-19 per month was also obtained from IHIS, and the total number of women in the population was obtained from the public database of the Czech Bureau of Statistics. Consequently, the numbers of SCs per month per 1,000 women were calculated for women that were pre-SC-vaccinated and pre-SC-unvaccinated, respectively, as well as the number of SCs per month per 1,000 women for all women aged 18-39 years in the Czech Republic. The study relied solely on secondary anonymized data and was, therefore, exempt from research ethics board review.
Results
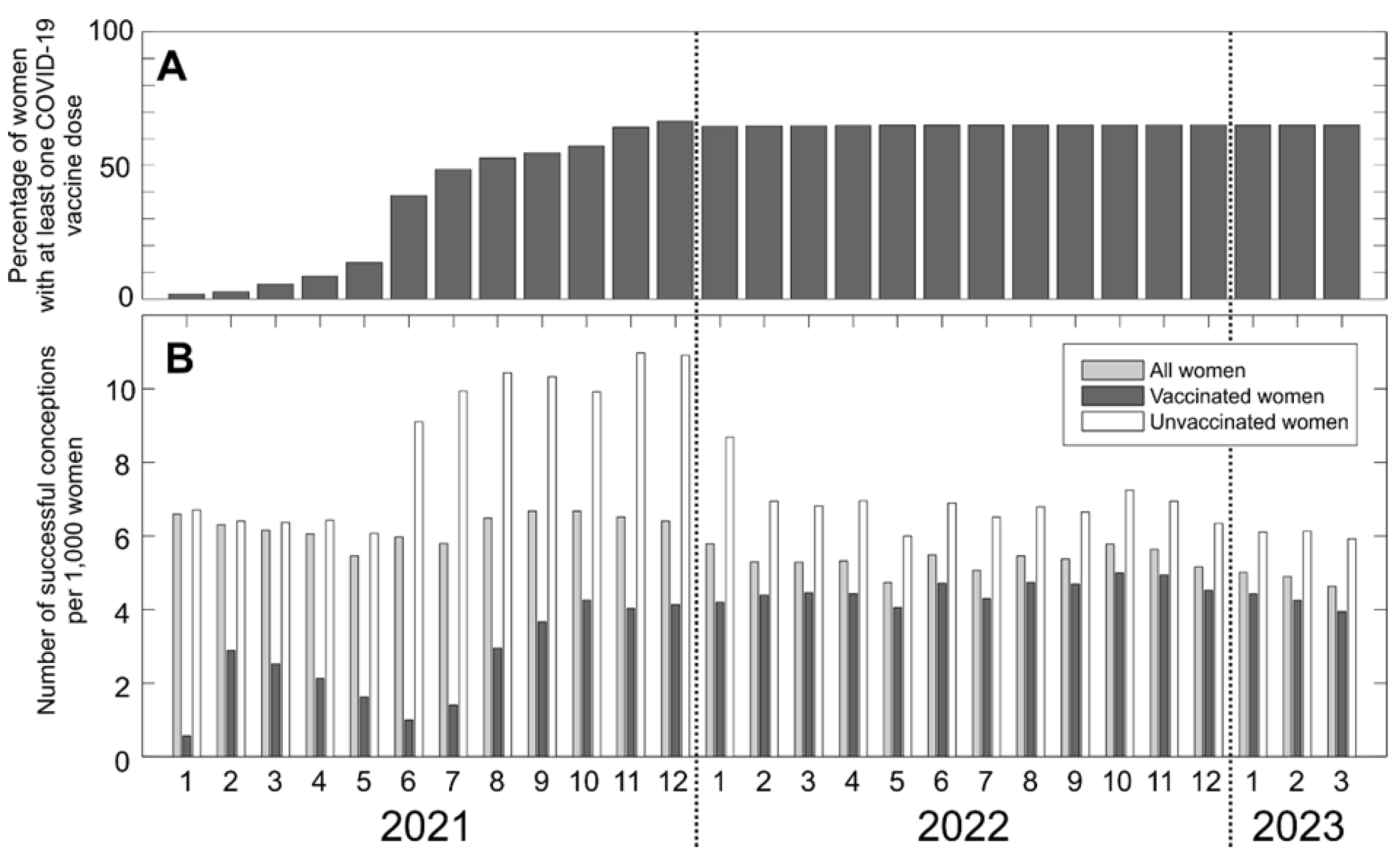
The data for vaccinated and unvaccinated women are shown in Figure During the study period (January 2021–March 2023), there were approximately 1,300,000 women aged 18-39 years in the Czech Republic, and the proportion of vaccinated women increased until reaching a steady state of around 70% of all women by the end of 2021 (
Figure 1A). The Comirnaty (Pfizer-BioNTech) and Spikevax (Moderna) mRNA vaccines comprised 96% of all administered COVID-19 vaccine doses, with a 11:1 ratio in the use of these two vaccines. Notably, during the entire study period, monthly numbers of SCs per 1,000 women were considerably lower for women that were vaccinated before SC, compared to those that were not. SC rates for women vaccinated before SC were generally much lower than expected based on their share of the total population of women (
Figure 1A and B). For example, at the end of June 2021, where 39% of all women had been vaccinated, those vaccinated before SC contributed only 7% of all SCs. In June 2021, a sharp increase in the rate of SC was observed for women unvaccinated before SC, and this higher rate was maintained over the succeeding 6-month period. During 2022, rates of SCs stabilized in both women that were vaccinated and unvaccinated before SC. However, throughout 2022, SC rates remained about 1.5 times higher for women that were unvaccinated before SC compared with those that were vaccinated before SC (
Figure 1B).
Discussion
In this study, we used simple descriptive statistics and data visualization to analyze summary COVID-19 vaccination and birth data for all women aged 18-39 years in the Czech Republic and found that from January 2021 to December 2022, monthly numbers of SCs per 1,000 women were markedly lower for women vaccinated before SC compared to those that were unvaccinated before SC. Furthermore, the contribution of women vaccinated before SC to the total monthly rate of SCs was substantially lower than to be expected according to the proportion of vaccinated women in the total population of women.
Declining birth rates have been reported in many countries following the COVID-19 pandemic and have been linked with economic instability, social inequality, and the stringency of pandemic-related social restrictions.1-3 An association between declining birth rates and onset of COVID-19 vaccinations has also been suggested and thought to indicate that women postponed conception until after vaccination.2,3 Indeed, concern about COVID-19 vaccine safety has been a major reported reason for remaining unvaccinated, and reproductive adults appear particularly anxious about potential adverse effects of COVID-19 vaccination on fertility.9-10 In this regard, although the overall safety of COVID-19 vaccination during pregnancy has been well documented, vaccination may be associated with menstrual pain and changes in menstrual flow and cycle length, and direct effects of the Comirnaty vaccine (Pfizer-BioNTech) on the ovarian follicle were reported recently.5-7 However, to date very little data on birth rate linked to COVID-19 vaccination status have been reported.
To our knowledge, the relationship between COVID-19 vaccination status and rates of SCs has not been examined previously on a population level. However, a prospective cohort study of pregnancy planners (n=2,126 women) in the US and Canada indicated that preconception COVID-19 vaccination did not influence the probability of SC, albeit that study only included women who were trying to conceive and was also limited by use of self-reported vaccination status.11 Contrary to these findings, our current real-world population data from the Czech Republic indicated that COVID-19 vaccination was linked with substantial decreases in SC rates compared to non-vaccinated women.
While the strength of our study is its nationwide unselected sample of fertile women, the observed association between decreased SC rates and COVID-19 vaccination is, of course, not proof of a causal relationship between vaccination and fecundability. For example, it is possible that more women who wished to become pregnant, i.e., achieve SC, chose not to be vaccinated, and/or that more women who did not plan to become pregnant opted for vaccination. Indeed, such self-selection bias is compatible with the decrease in SC observed amongst women vaccinated before SC in the first months of the vaccination campaign as well as the sudden increase in SCs of the women unvaccinated before SC in June 2021 (
Figure 1B). However, to defer vaccination was against sanctioned national public recommendations in the Czech Republic at the time, and if this type of self-selection bias had been the predominant underlying factor for the observed reduction in SC rates in vaccinated women, the total fertility rate would have remained relatively constant throughout the study period. However, the total fertility rate in the Czech Republic decreased from 1.83 births per 1000 women in 2021, to 1.62 in 2022, and 1.45 in 2023,
12 and self-selection bias, therefore, does not seem to fully explain the observed link between vaccination status and SC rates. Notably, we and others have previously found a batch-dependent safety signal for the Comirnaty vaccine (Pfizer-BioNTech) in the Czech Republic, Denmark, Sweden, and the US, and the possibility of a disproportionate influence of early batches of this vaccine on SC rates remains to be investigated.
13-16
The current study should be interpreted in view of other limitations that include, for example, unmeasured confounders such as socioeconomic factors, comorbidities, effects of individual COVID-19 vaccination boosters, concurrent COVID-19 infection specifics, preconception fertility, contraception use, pregnancy loss, stillbirths, and paternal vaccination status. In addition, the Czech Republic population is almost exclusively Caucasian, and results may not apply to other ethnicities.
Conclusions
We conclude that during the study period, SC rates in the Czech Republic for all women vaccinated against COVID-19 before SC were substantially lower than for those who were unvaccinated before SC. These hypothesis-generating and preliminary results call for further studies of the influence of COVID-19 vaccination on human fecundability and fertility.
Author Contributions
Conceptualization: TF, VM; Methodology: TF, VM; Investigation: TF, VM, PRH; Data curation: TF, MS; Formal analysis: TF, VM, MS, JDG, PRH; Writing-Original draft: VM, TF, JDG, PRH; Writing-Review and editing; VM, TF, MS, JDG, PRH; Project administration: VM; Funding acquisition: VM.
Funding
This study was supported by donation-based crowdfunding (Danish Ministry of Justice, Department of Civil Affairs, journal number 23-700-06725). The funding source did not have any role in the writing of the manuscript or the decision to submit it for publication.
Data Availability Statement
Conflicts of interest
None.
References
- Pomar L, Favre G, de Labrusse C, Contier A, Boulvain M, Baud D. Impact of the first wave of the COVID-19 pandemic on birth rates in Europe: a time series analysis in 24 countries. Hum Reprod 2022, 37, 2921–2931. [Google Scholar] [CrossRef] [PubMed]
- Bujard M, Andersson G. Fertility Declines Near the End of the COVID-19 Pandemic: Evidence of the 2022 Birth Declines in Germany and Sweden. Eur J Population 2024, 40, 4. [CrossRef] [PubMed]
- Winkler-Dworak M, Zeman K, Sobotka T. Birth rate decline in the later phase of the COVID-19 pandemic: the role of policy interventions, vaccination programmes, and economic uncertainty. Hum Reprod Open 2024, 2024, hoae052. [Google Scholar] [CrossRef] [PubMed]
- Wang C, Wang M, Li G, Song B, Xing Q, Cao Y. Effects of COVID-19 vaccination on human fertility: a post-pandemic literature review. Ann Med 2023, 55, 2261964. [Google Scholar] [CrossRef] [PubMed]
- Fernández-García S, Del Campo-Albendea L, Sambamoorthi D, Sheikh J, Lau K, Osei-Lah N, Ramkumar A, Naidu H, Stoney N, Sundaram P, Sengupta P, Mehta S, Attarde S, Maddock S, Manning M, Meherally Z, Ansari K, Lawson H, Yap M, Kew T, Punnoose A, Knight C, Sadeqa E, Cherian J, Ravi S, Chen W, Walker K, O'Donoghue K, van Wely M, van Leeuwen E, Kostova E, Kunst H, Khalil A, Brizuela V, Kara E, Kim CR, Thorson A, Oladapo OT, Mofenson L, Gottlieb SL, Bonet M, Moss N, Zamora J, Allotey J, Thangaratinam S; PregCOV-19 Living Systematic Review Consortium. Effectiveness and safety of COVID-19 vaccines on maternal and perinatal outcomes: a systematic review and meta-analysis. BMJ Glob Health 2024, 9, e014247. [Google Scholar] [CrossRef] [PubMed]
- Payne LA, Wise LA, Wesselink AK, Wang S, Missmer SA, Edelman A. Association between COVID-19 vaccination and menstruation: a state of the science review. BMJ Sex Reprod Health 2024, 50, 212–225. [Google Scholar] [CrossRef] [PubMed]
- Bar-Joseph H, Raz Y, Eldar-Boock A, Michaan N, Angel Y, Saiag E, Nemerovsky L, Ben-Ami I, Shalgi R, Grisaru D. The direct effect of SARS-CoV-2 virus vaccination on human ovarian granulosa cells explains menstrual irregularities. NPJ Vaccines 2024, 9, Erratum in: NPJ Vaccines 2024, 9, 172. [Google Scholar]
- Regan AK, Fell DB, Wise LA, Vazquez-Benitez G, Håberg SE, Ogar C, Yland JJ, Wesselink AK, Zerbo O. Challenges & opportunities for the epidemiological evaluation of the effects of COVID-19 vaccination on reproduction and pregnancy. Vaccine 2023, 41, 5931–5935. [Google Scholar]
- SteelFisher GK, Blendon RJ, Caporello H. An Uncertain Public - Encouraging Acceptance of Covid-19 Vaccines. N Engl J Med 2021, 384, 1483–1487. [Google Scholar] [CrossRef] [PubMed]
- Diaz P, Reddy P, Ramasahayam R, Kuchakulla M, Ramasamy R. COVID-19 vaccine hesitancy linked to increased internet search queries for side effects on fertility potential in the initial rollout phase following Emergency Use Authorization. Andrologia 2021, 53, e14156.
- Wesselink AK, Hatch EE, Rothman KJ, Wang TR, Willis MD, Yland J, Crowe HM, Geller RJ, Willis SK, Perkins RB, Regan AK, Levinson J, Mikkelsen EM, Wise LA. A Prospective Cohort Study of COVID-19 Vaccination, SARS-CoV-2 Infection, and Fertility. Am J Epidemiol 2022, 191, 1383–1395. [Google Scholar] [CrossRef]
- Czech Statistical Office. Birth Statics. Available online: https://csu.gov.cz/births (accessed on day month year).
- Schmeling M, Manniche V, Hansen PR. Batch-dependent safety of the BNT162b2 mRNA COVID-19 vaccine. Eur J Clin Invest 2023, 53, e13998. [Google Scholar] [CrossRef] [PubMed]
- Fürst T, Šourek P, Krátká Z, Janošek J. Batch-dependent safety of COVID-19 vaccines in the Czech Republic and comparison with data from Denmark. Eur J Clin Invest 2024, 54, e14271. [Google Scholar] [CrossRef] [PubMed]
- Manniche V, Schmeling M, Gilthorpe JD, Hansen PR. Reports of Batch-Dependent Suspected Adverse Events of the BNT162b2 mRNA COVID-19 Vaccine: Comparison of Results from Denmark and Sweden. Medicina (Kaunas) 2024, 60, 1343. [Google Scholar] [CrossRef] [PubMed]
- Jablonowski K, Hooker B. Batch-dependent safety of the BNT162b2 mRNA COVID-19 vaccine in the United States. Science, Public Health Policy and the Law 2019, v5.2019-2024.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).