Submitted:
25 March 2025
Posted:
26 March 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
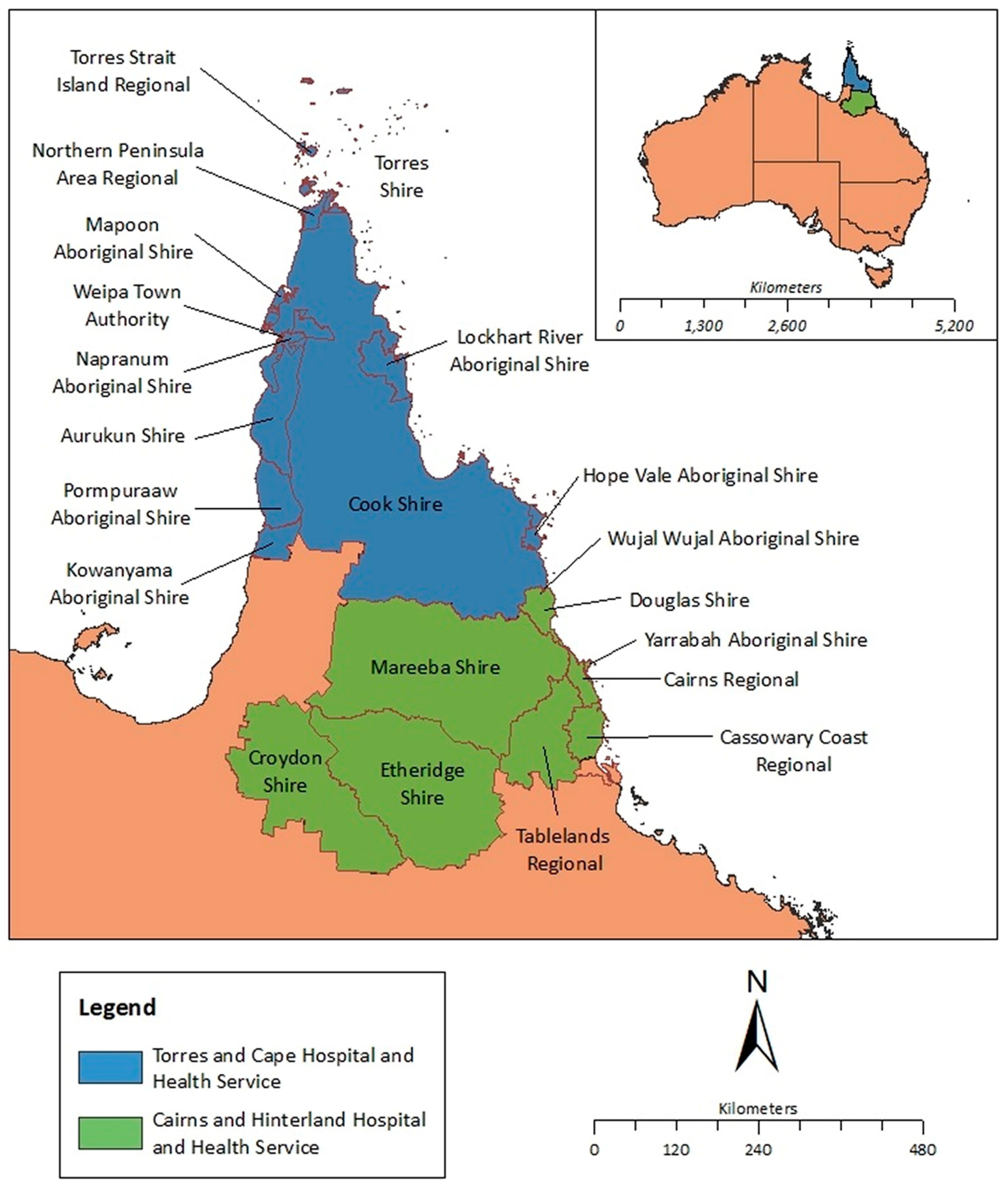
2.1. Study Design and Population
2.2. Identification of Individuals with a Positive Skin Scraping in the FNQ Region Between 2000 and 2023
2.3. The Association Between a Positive Skin Scraping and Subsequent Diagnosis of ARF/RHD or CKD
2.4. Assessment of Individuals Presenting to the Cairns Hospital Emergency Department with a Diagnosis of Scabies
2.5. Statistical Analysis
2.6. Ethics Statement
3. Results
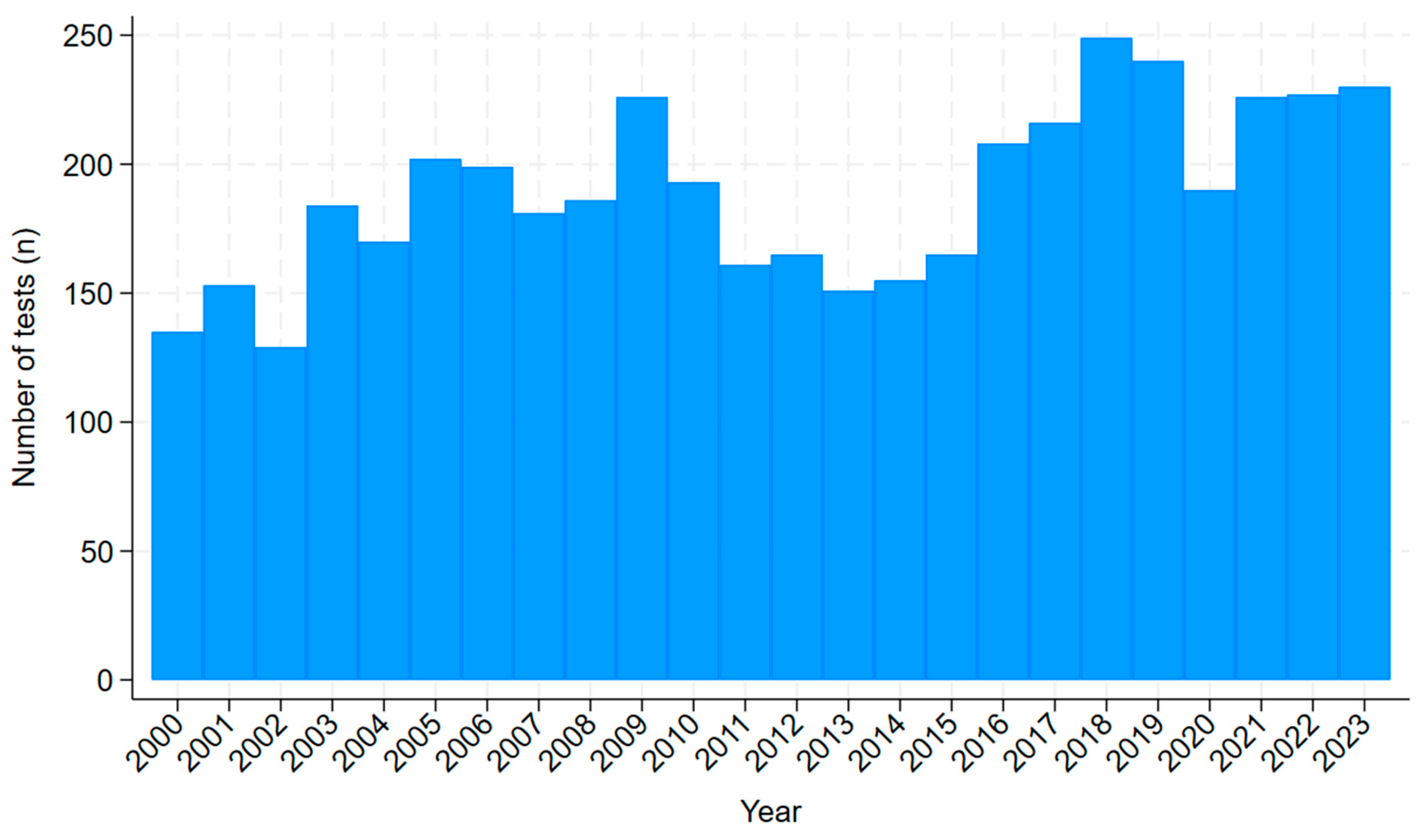
3.1. Skin Scrapings
3.2. Characteristics of the Individuals Who Were Tested
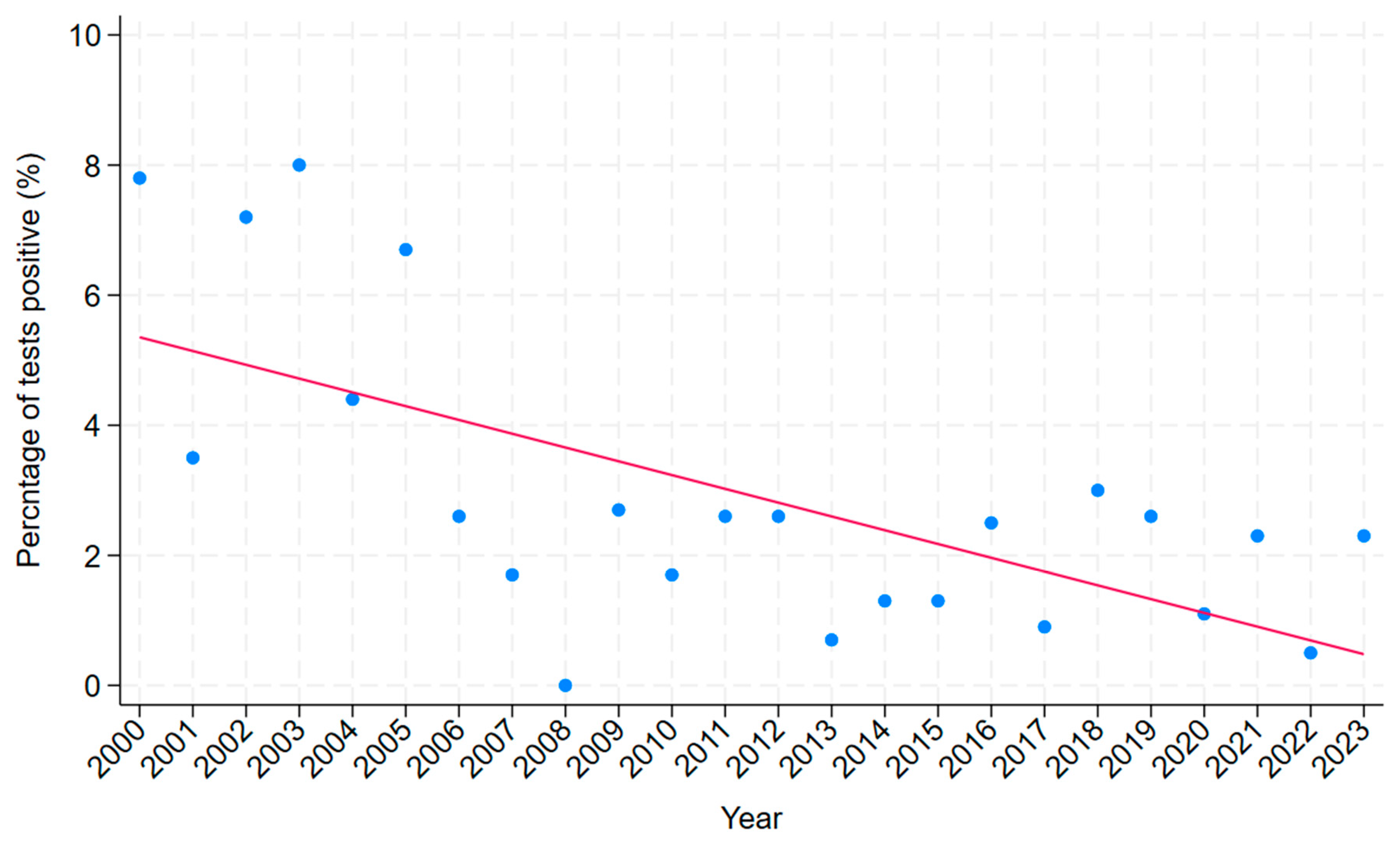
3.3. Number of Positive Tests and Trend Over Time
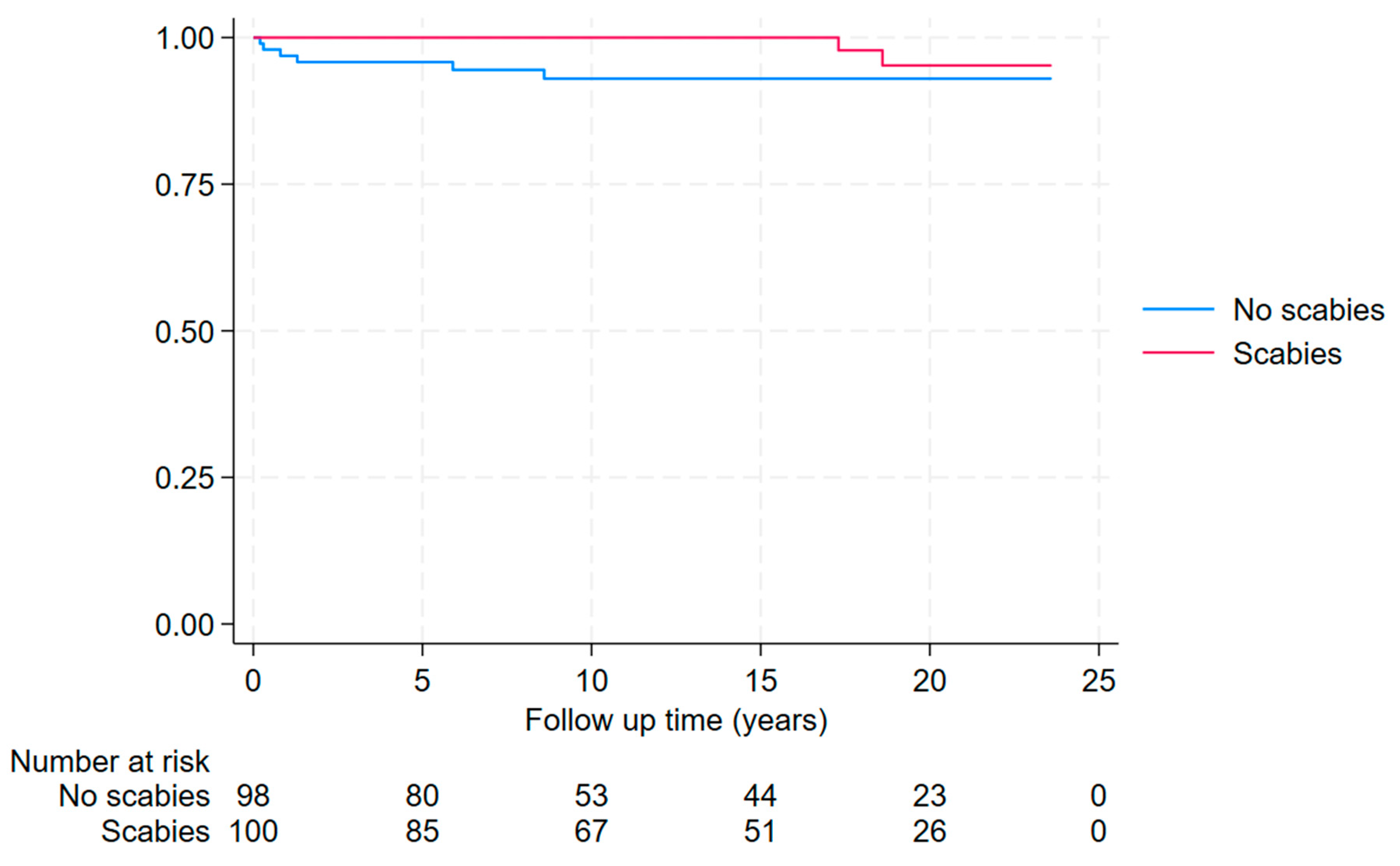
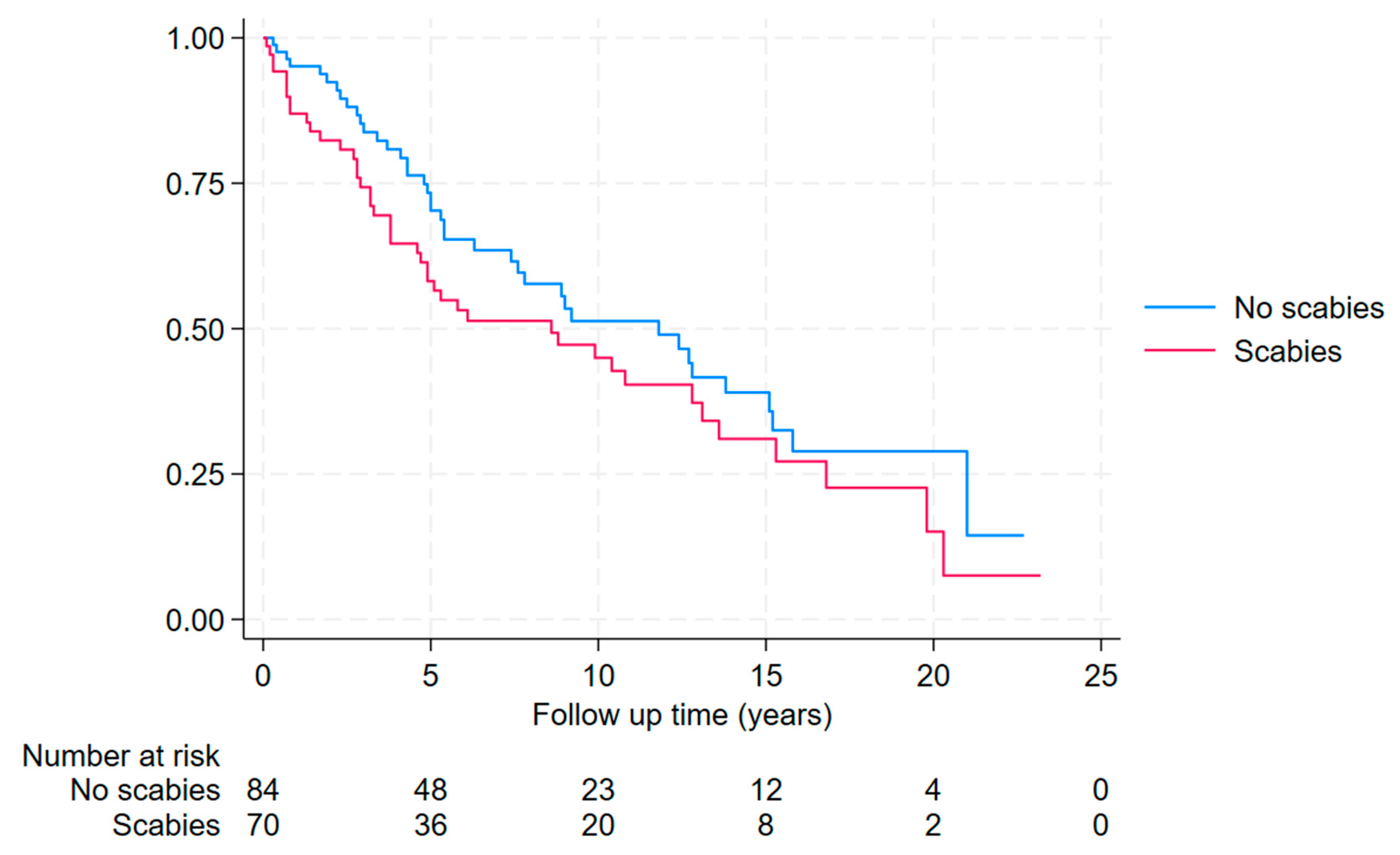
3.4. Association of Microbiologically Diagnosed Scabies with a Subsequent Diagnosis of ARF/RHD or CKD
3.5. Assessment of Individuals Presenting to the Cairns Hospital Emergency Department with Clinically Suspected Scabies
3.5.1. Classic Scabies
3.5.2. Crusted Scabies
4. Discussion
5. Conclusions
Supplementary Materials
References
- Walton SF, Currie BJ. Problems in diagnosing scabies, a global disease in human and animal populations. Clinical microbiology reviews. 2007;20(2):268-79. [CrossRef]
- Romani L, Steer AC, Whitfeld MJ, Kaldor JM. Prevalence of scabies and impetigo worldwide: A systematic review. The Lancet Infectious Diseases. 2015;15(8):960-7. [CrossRef]
- Scabies Geneva: World Heath Organization; 2023 [updated 31 May 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/scabies.
- Li J, Liu Z, Xia X. The disability-adjusted life years (DALYs), prevalence and incidence of scabies, 1990–2021: A systematic analysis from the Global Burden of Disease Study 2021. PLOS Neglected Tropical Diseases. 2024;18(12):e0012775.
- Davidson L, Knight J, Bowen AC. Skin infections in Australian Aboriginal children: a narrative review. The Medical journal of Australia. 2020;212(5):231-7. [CrossRef]
- Lake SJ, Engelman D, Sokana O, Nasi T, Boara D, Marks M, et al. Health-related quality of life impact of scabies in the Solomon Islands. Trans R Soc Trop Med Hyg. 2022;116(2):148-56. [CrossRef]
- Collinson S, Timothy J, Zayzay SK, Kollie KK, Lebas E, Candy N, et al. The prevalence of scabies in Monrovia, Liberia: A population-based survey. PLoS neglected tropical diseases. 2020;14(12):e0008943. [CrossRef]
- Nair PA, Vora RV, Jivani NB, Gandhi SS. A Study of Clinical Profile and Quality of Life in Patients with Scabies at a Rural Tertiary Care Centre. J Clin Diagn Res. 2016;10(10):Wc01-wc5.
- Steer AC, Jenney AWJ, Kado J, Batzloff MR, La Vincente S, Waqatakirewa L, et al. High burden of impetigo and scabies in a tropical country. PLoS Neglected Tropical Diseases. 2009;3(6). [CrossRef]
- Tong SY, Davis JS, Eichenberger E, Holland TL, Fowler VG, Jr. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev. 2015;28(3):603-61.
- Parks T, Smeesters PR, Steer AC. Streptococcal skin infection and rheumatic heart disease. Curr Opin Infect Dis. 2012;25(2):145-53. [CrossRef]
- Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group A streptococcal diseases. Lancet Infect Dis. 2005;5(11):685-94.
- Dowler J, Wilson A. Acute post-streptococcal glomerulonephritis in Central Australia. The Australian journal of rural health. 2020;28(1):74-80. [CrossRef]
- Acute rheumatic fever and rheumatic heart disease in Australia, 2022. Canberra: AIHW; 2024.
- Hoy WE, White AV, Dowling A, Sharma SK, Bloomfield H, Tipiloura BT, et al. Post-streptococcal glomerulonephritis is a strong risk factor for chronic kidney disease in later life. Kidney international. 2012;81(10):1026-32. [CrossRef]
- Pinto SWL, Sesso R, Vasconcelos E, Watanabe YJ, Pansute AM. Follow-up of patients with epidemic poststreptococcal glomerulonephritis. American journal of kidney diseases. 2001;38(2):249-55. [CrossRef]
- Chronic kidney disease in Aboriginal and Torres Strait Islander people. Canberra: AIHW; 2011.
- Fernando DD, Mounsey KE, Bernigaud C, Surve N, Estrada Chávez GE, Hay RJ, et al. Scabies. Nature Reviews Disease Primers. 2024;10(1):74.
- Cinotti E, Perrot JL, Labeille B, Vercherin P, Chol C, Besson E, et al. Reflectance confocal microscopy for quantification of Sarcoptes scabiei in Norwegian scabies. Journal of the European Academy of Dermatology and Venereology. 2013;27(2):e176-e8. [CrossRef]
- Hasan T, Krause VL, James C, Currie BJ. Crusted scabies; a 2-year prospective study from the Northern Territory of Australia. PLoS neglected tropical diseases. 2020;14(12):e0008994. [CrossRef]
- Lynar S, Currie BJ, Baird R. Scabies and mortality. The Lancet Infectious diseases. 2017;17(12):1234.
- The 2020 Australian guideline for prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease. 2020 March 2022.
- Andrews RM, Kearns T, Connors C, Parker C, Carville K, Currie BJ, et al. A regional initiative to reduce skin infections amongst aboriginal children living in remote communities of the Northern Territory, Australia. PLoS neglected tropical diseases. 2009;3(11):e554. [CrossRef]
- Jones M, Thomas H, Snelling T, Bowen A, Marsh J. The SToP (See, Treat, Prevent) Skin Sores and Scabies Trial - a stepped wedge cluster randomised trial for skin disease control in remote Western Australia: Statistical analysis plan. 2023.
- Gardner K, Van Gool K, Van der Linden N, Agostino J, Campbell M, Dickinson H, et al. Evaluation of the one disease crusted scabies elimination project. Canberra: Public Service Research Group, Business School, University of New South Wales. 2018.
- Rosumeck S, Nast A, Dressler C. Ivermectin and permethrin for treating scabies. Cochrane Database Syst Rev. 2018;4(4):CD012994. [CrossRef]
- Lokuge B, Kopczynski A, Woltmann A, Alvoen F, Connors C, Guyula T, et al. Crusted scabies in remote Australia, a new way forward: lessons and outcomes from the East Arnhem Scabies Control Program. The Medical journal of Australia. 2014;200(11):644-8. [CrossRef]
- Kearns TM, Speare R, Cheng AC, McCarthy J, Carapetis JR, Holt DC, et al. Impact of an Ivermectin Mass Drug Administration on Scabies Prevalence in a Remote Australian Aboriginal Community. PLoS neglected tropical diseases. 2015;9(10):e0004151.
- Simple, Complicated and Crusted Scabies NT Health Guideline. 2024.
- Public Health Management of Crusted Scabies. NT Health. Northern Territory Government; 2023.
- 2021 Australian Census Canberra. Australian Bureau of Statistics; 2021.
- Fox H, Hempenstall A, Pilot P, Callander E, Smith S, McDonald MI, et al. Significant healthcare resource utilisation in the management of skin and soft tissue infections in the Torres Strait, Australia. Rural and remote health. 2024. [CrossRef]
- Kang K, Chau KW, Howell E, Anderson M, Smith S, Davis TJ, et al. The temporospatial epidemiology of rheumatic heart disease in Far North Queensland, tropical Australia 1997–2017; impact of socioeconomic status on disease burden, severity and access to care. PLOS Neglected Tropical Diseases. 2021;15(1):e0008990. [CrossRef]
- Vos L, Baer R, McDonald M. Addressing chronic kidney disease in F ar N orth Q ueensland: gains and opportunities. Australian Journal of Rural Health. 2013;21(6):313-8.
- Socio-Economic Indexes for Areas (SEIFA), Australia. Australian Bureau of Statistics; 2021.
- Coffey PM, Ralph AP, Krause VL. The role of social determinants of health in the risk and prevention of group A streptococcal infection, acute rheumatic fever and rheumatic heart disease: a systematic review. PLoS neglected tropical diseases. 2018;12(6):e0006577. [CrossRef]
- Stevens PE, Ahmed SB, Carrero JJ, Foster B, Francis A, Hall RK, et al. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney international. 2024;105(4):S117-S314. [CrossRef]
- Engelman D, Yoshizumi J, Hay RJ, Osti M, Micali G, Norton S, et al. The 2020 International Alliance for the Control of Scabies Consensus Criteria for the Diagnosis of Scabies. The British journal of dermatology. 2020;183(5):808-20. [CrossRef]
- Davis JS, McGloughlin S, Tong SY, Walton SF, Currie BJ. A novel clinical grading scale to guide the management of crusted scabies. PLoS neglected tropical diseases. 2013;7(9):e2387. [CrossRef]
- NT Health Guideline: Simple, Complicated and Crusted Scabies. . Infectious Diseases Department, Royal Darwin Hospital. NT Health; 2024.
- Gramp P, Gramp D. Scabies in remote Aboriginal and Torres Strait Islander populations in Australia: A narrative review. PLoS neglected tropical diseases. 2021;15(9):e0009751. [CrossRef]
- Paltridge M, Smith S, Traves A, McDermott R, Fang X, Blake C, et al. Rapid Progress toward Elimination of Strongyloidiasis in North Queensland, Tropical Australia, 2000–2018. The American journal of tropical medicine and hygiene. 2020;102(2):339. [CrossRef]
- Elston DM. Confirmation bias in medical decision-making. Journal of the American Academy of Dermatology. 2020;82(3):572. [CrossRef]
- Karimkhani C, Colombara DV, Drucker AM, Norton SA, Hay R, Engelman D, et al. The global burden of scabies: a cross-sectional analysis from the Global Burden of Disease Study 2015. The Lancet Infectious diseases. 2017;17(12):1247-54. [CrossRef]
- Leung V, Miller M. Detection of scabies: A systematic review of diagnostic methods. Canadian Journal of Infectious Diseases and Medical Microbiology. 2011;22(4):143-6.
- Osti MH, Sokana O, Gorae C, Whitfeld MJ, Steer AC, Engelman D. The diagnosis of scabies by non-expert examiners: A study of diagnostic accuracy. PLoS neglected tropical diseases. 2019;13(8):e0007635. [CrossRef]
- Yeoh DK, Anderson A, Cleland G, Bowen AC. Are scabies and impetigo “normalised”? A cross-sectional comparative study of hospitalised children in northern Australia assessing clinical recognition and treatment of skin infections. PLoS neglected tropical diseases. 2017;11(7):e0005726. [CrossRef]
- Felmingham C, Tilakaratne D. Overdiagnosis of scabies and overprescribing of scabies treatment in a scabies-endemic region. The Australian journal of rural health. 2020;28(4):394-8. [CrossRef]
- Lorenzetti DL, Quan H, Lucyk K, Cunningham C, Hennessy D, Jiang J, et al. Strategies for improving physician documentation in the emergency department: a systematic review. BMC Emergency Medicine. 2018;18(1):36. [CrossRef]
- Public Health Response- Aurukun- November 2021 In: Team TPH, editor.: Torres and Cape Health Service; 2023.
- Taylor G. NT Health Guideline: Public Health Management of Crusted Scabies.: Centre of Disease Control NT Health. NT Health; 2023.
- List of notifiable Conditions Queensland.: Queensland Health. Queensland Government; 2023.
- Bonazzetti C, Pagani G, Giacomelli A, Morena V, Bassoli C, Corbellino M, et al. A case of crusted scabies with a delayed diagnosis and inadequate therapy. Le Infezioni in Medicina. 2020;28(3):436-40.
- Mounsey KE, Murray HC, King M, Oprescu F. Retrospective analysis of institutional scabies outbreaks from 1984 to 2013: lessons learned and moving forward. Epidemiol Infect. 2016;144(11):2462-71. [CrossRef]
- Currie BJ, Maguire GP, Wood YK. Ivermectin and crusted (Norwegian) scabies. Medical Journal of Australia. 1995;163(10):559-60. [CrossRef]
- Hoy WE, Wang Z, Zhang J, Diwan V, Cameron A, Venuthurupalli SK, et al. Chronic kidney disease in public renal practices in Queensland, Australia, 2011–2018. Nephrology. 2022;27(12):934-44. [CrossRef]
- Kidney disease, Aboriginal and Torres Strait Islander Health Performance Framework website. Australian Institute of Health Welfare. National Indigenous Australians Agency.; 2023.
- The Health of Queenslanders. Report of the Chief Health Officer Queensland. Chronic diseases. Brisbane: Queensland Health; 2024.
- Wyber R, Noonan K, Halkon C, Enkel S, Cannon J, Haynes E, et al. Ending rheumatic heart disease in Australia: the evidence for a new approach. Medical Journal of Australia. 2020;213:S3-S31. [CrossRef]
- Shoukat Q, Rizvi A, Wahood W, Coetzee S, Wrench A. Sight the mite: a meta-analysis on the diagnosis of scabies. Cureus. 2023;15(1). [CrossRef]
- Walter B, Heukelbach J, Fengler G, Worth C, Hengge U, Feldmeier H. Comparison of dermoscopy, skin scraping, and the adhesive tape test for the diagnosis of scabies in a resource-poor setting. Arch Dermatol. 2011;147(4):468-73. [CrossRef]
- Romani L, Marks M, Sokana O, Nasi T, Kamoriki B, Cordell B, et al. Efficacy of mass drug administration with ivermectin for control of scabies and impetigo, with coadministration of azithromycin: a single-arm community intervention trial. The Lancet Infectious Diseases. 2019;19(5):510-8. [CrossRef]
- Marks M, Toloka H, Baker C, Kositz C, Asugeni J, Puiahi E, et al. Randomized Trial of Community Treatment With Azithromycin and Ivermectin Mass Drug Administration for Control of Scabies and Impetigo. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2019;68(6):927-33. [CrossRef]
- Shepheard J. Clinical coding and the quality and integrity of health data. Health Information Management Journal. 2020;49(1):3-4. [CrossRef]
- O’Malley KJ, Cook KF, Price MD, Wildes KR, Hurdle JF, Ashton CM. Measuring diagnoses: ICD code accuracy. Health Serv Res. 2005;40(5 Pt 2):1620-39. [CrossRef]
- Park JH, Kim CW, Kim SS. The diagnostic accuracy of dermoscopy for scabies. Ann Dermatol. 2012;24(2):194-9. [CrossRef]
- Bae M, Kim JY, Jung J, Cha HH, Jeon N-Y, Lee H-J, et al. Diagnostic value of the molecular detection of Sarcoptes scabiei from a skin scraping in patients with suspected scabies. PLoS Neglected Tropical Diseases. 2020;14(4):e0008229. [CrossRef]
- Hendrickx D, Bowen AC, Marsh JA, Carapetis JR, Walker R. Ascertaining infectious disease burden through primary care clinic attendance among young Aboriginal children living in four remote communities in Western Australia. PloS one. 2018;13(9):e0203684. [CrossRef]
- Amgarth-Duff I, Hendrickx D, Bowen A, Carapetis J, Chibawe R, Samson M, et al. Talking skin: attitudes and practices around skin infections, treatment options, and their clinical management in a remote region in Western Australia. Rural and remote health. 2019;19(3):5227. [CrossRef]
| Variable | Total a | Positive | Negative | Odds ratio b (95% CI) | p b | Odds ratio c (95% CI) | p c |
|---|---|---|---|---|---|---|---|
| Tested in Cairns | 945/4342 (22%) | 67/120 (55%) | 878/4222 (20%) | 4.72 (3.28-6.81) | <0.001 | 6.18 (4.24-9.02) | <0.001 |
| First Nations Australian | 2706/4313 (63%) | 110/120 (92%) | 2596/4193 (61%) | 6.76 (3.53–12.96) | <0.001 | 10.54 (5.43-20.45) | <0.001 |
| Adult (age >16) | 3555/4345 (82%) | 116/121 (96%) | 3439/4224 (79%) | 5.30 (2.16–13.01) | <0.001 | 5.94 (2.40-14.69) | <0.001 |
| Female sex | 2174/4344 (50%) | 70/121 (58%) | 2104/4223 (48%) | 1.38 (0.96–1.99) | 0.08 | 1.13 (0.77-1.65) | 0.53 |
| Classic scabies a (n=271) |
Crusted scabies a (n=21) |
Total (n= 292) |
|
|---|---|---|---|
| First Nations Australian | 197 (73%) | 19 (91%) | 216 (74.0%) |
| Male sex | 140 (52%) | 9 (43%) | 149 (51.0%) |
| Child (<16 years) | 150 (55%) | 8 (38%) | 158 (54.1%) |
| Scrapings performed | 9 (3%) | 5 (24%) | 14 (4.8%) |
| Positive skin scrapings | 0 | 1 (5%) | 1 (0.3%) |
| Infectious disease or dermatology service involvement | 7 (3%) | 6 (29%) | 13 (4.5%) |
| Complete documentation of IACS criteria b | 11 (4%) | 4 (19%) | 15 (5.1%) |
| Adequate documentation for clinical scabies diagnosis b | 115 (42%) | 11 (52%) | 126 (43.2%) |
| Satisfied IACS criteria for confirmed scabies b | 0 | 1 (5%) | 1/292 (0.3%) |
| Satisfied IACS for clinical scabies b | 88 (33%) | 13 (62%) | 101 (34.6 %) |
| Documented crusted scabies severity grading | Not Applicable | 2 (10%) d | Not Applicable |
| Followed all NT guidelines for crusted scabies c | Not Applicable | 1 (5%) | Not Applicable |
| Admitted to hospital from the Emergency Department | 60 (22%) | 16 (76%) | 76 (26.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





